We found that mild or moderate iliac vein compression was not associated with an elevated risk of left-sided deep venous thrombosis, while greater than 70% compression may be associated with an elevated risk of left deep venous thrombosis.
Abstract
Purpose:
To determine if compression of the left common iliac vein (LCIV) by the right common iliac artery is associated with left-sided deep venous thrombosis (DVT).
Materials and Methods:
This institutional review board–approved case-control study was performed in a cohort of 230 consecutive patients (94 men, 136 women; mean age, 57.5 years; range, 10–94 years) at one institution who had undergone contrast material–enhanced computed tomography of the pelvis prior to a diagnosis of unilateral DVT. Demographic data and information on risk factors were collected. Two board-certified radiologists determined iliac vein compression by using quantitative measures of percentage compression {[1 minus (LCIV diameter at point of maximal compression/distal right common iliac vein diameter)] times 100%}, as well as qualitative measures (none, mild, moderate, severe), with estimates of measurement variability. Logistic regression analysis was performed (independent variable, left vs right DVT; dependent variable, iliac vein compression). Cutpoints of relevant compression were evaluated by using splines. Means (with 95% confidence intervals [CIs]) and odds ratios (ORs) (and 95% CIs) of left DVT per 1% increase in percentage compression were calculated.
Results:
Patients with right DVT were more likely than those with left DVT to have a history of pulmonary embolism. Overall, in all study patients, mean percentage compression was 36.6%, 66 (29.7%) of 222 had greater than 50% compression, and 16 (7.2%) had greater than 70% compression. At most levels of compression, increasing compression was not associated with left DVT (adjusted ORs, 1.00, 0.99, 1.02) but above 70%, LCIV compression may be associated with left DVT (adjusted ORs, 3.03, 0.91, 10.15).
Conclusion:
Increasing levels of percentage compression were not associated with left-sided DVT up to 70%; however, greater than 70% compression may be associated with left DVT.
©RSNA, 2012
Supplemental material: http://radiology.rsna.org/lookup/suppl/doi:10.1148/radiol.12111580/-/DC1
Introduction
Deep venous thrombosis (DVT) has been noted to occur as much as 60% more frequently in the left lower extremity than in the right lower extremity (1). Investigators since Virchow have suggested that this disparity may be related to compression of the left common iliac vein (LCIV) by the right common iliac artery (2). In the 1950s, May and Thurner (3) found pathologic changes (venous spurs) at the point where the right common iliac artery crosses over the LCIV. They proposed a causal mechanism by which chronic pulsations of the right common iliac artery resulted in venous spur formation in the LCIV, predisposing patients to DVT at this location. Preliminary studies comparing limbs with left DVT to limbs without left DVT have suggested that iliac vein compression may be associated with a higher percentage of left-sided DVT (4) and a lower percentage of symptomatic pulmonary embolism (PE) (5). However, Kibbe et al (6) also found a high prevalence of iliac vein compression in patients without DVT, suggesting that iliac vein compression may represent a normal variation without pathologic consequences. In addition, prior studies have been limited by small sample sizes and a lack of control groups. The purpose of our study was therefore to determine (a) if greater than 70% LCIV compression is a risk factor for left-sided DVT and (b) whether increasing percentage LCIV compression is associated with increased odds of left-sided DVT below 70% compression.
Materials and Methods
Subjects
An institutional review board exemption was obtained for the review of deidentified existing data, and the requirement for informed consent was waived as the study presented minimal harm to subjects. The study was based at Johns Hopkins Hospital (Baltimore, Md).
Patients with a diagnosis of left- or right-sided DVT who also had undergone abdominal and/or pelvic computed tomographic (CT) studies with contrast material since 2004 were identified. DVTs were characterized by side and location. Compared with iliofemoral or popliteal DVT, calf DVT has a lower probability of propagation to the lungs; hence, we limited our study to popliteal and iliofemoral DVT (7). Cases were defined as patients with left-sided DVT, while control subjects were patients with right-sided DVT. Control subjects with right-sided DVT were selected because they, unlike patients without DVT, would be expected to have distributions of potential confounders similar to those of patients with left-sided DVT. Patients with bilateral DVT or a history of bilateral DVT and those with unilateral risk factors (eg, trauma, tumors, lymphadenopathy, surgical clips) were excluded.
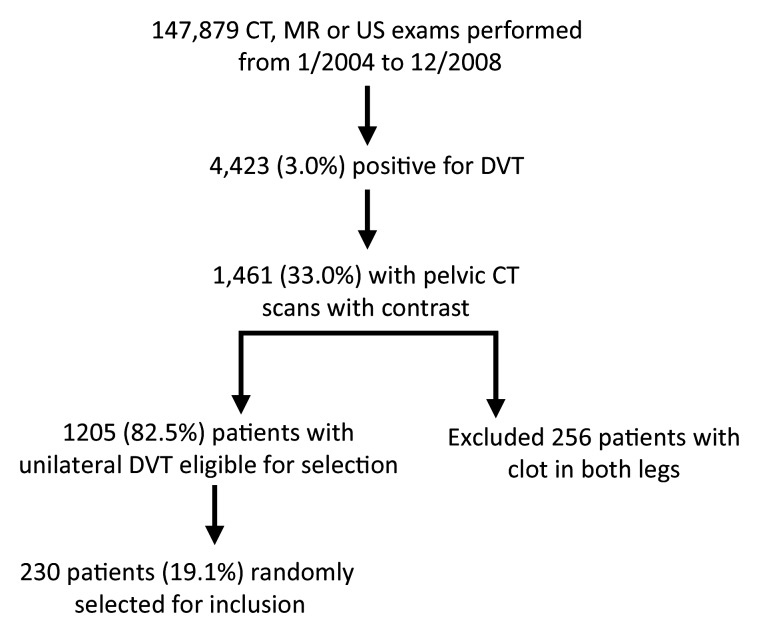
To ascertain patients, 147 879 ultrasonography (US), venography, CT, and magnetic resonance (MR) imaging reports from January 1, 2004, through December 31, 2008, were acquired from the Hospital Radiology Information Systems and imported into an MS Access Database. DVT cases were ascertained by performing automated text searches of these reports (Appendix E1 [online]). The remaining reports were read by the primary author (A.K.N.) to yield 4423 cases of DVT (3.0%) (Fig 1). Of these, 1461 were noted to have been observed at pelvic CT examinations performed with contrast material. We selected CT studies performed prior to the diagnosis of DVT but used concurrent or subsequent CT studies when prior CT studies were not available. After excluding patients with current or historical bilateral involvement, we randomly selected 230 patients, ending up with 127 patients with left DVT and 103 patients with right DVT. Of these 230 patients, 70 did not have any symptoms of DVT, 126 had undergone CT to evaluate malignancy (diagnosis or follow-up), and 33 had undergone CT for abdominal pain. Data were controlled by A.N. and J.C.
Figure 1:
Patient flow diagram.
CT Parameters
Studies were performed with a 64-detector CT scanner (Somatom Sensation 64; Siemens Medical Solutions, Malvern, Pa) (detector thickness, 0.6 mm; section thickness, 0.75 mm; reconstruction interval, 0.5 mm; 120 kVp; 120–200 mAs). Contrast material (100–120 mL of Iohexol 350 [milligrams of iron per milliliter] or Iodixanol 320 [milligrams of iron per milliliter]; GE Healthcare, Princeton, NJ) was injected intravenously (at 4 mL/sec). Patients underwent either single-phase (after 60–80 seconds) or dual-phase (arterial, after 25–30 seconds; venous, after 25–35 additional seconds) acquisitions.
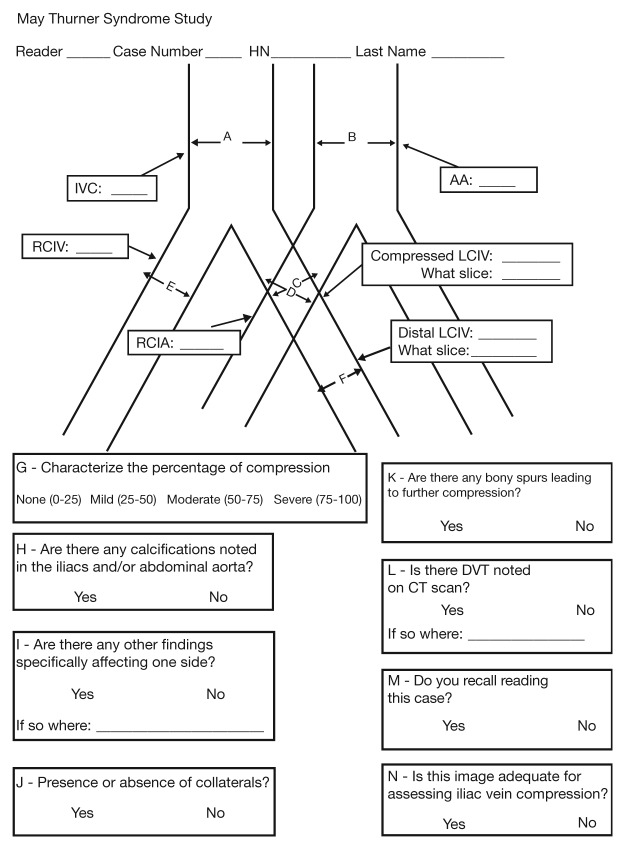
Development of Measurement Instrument
A pilot study was conducted with two board-certified radiologists (K.H., M.A.) to develop an instrument to measure iliac vein compression and other potentially causally relevant variables (Fig 2). Iliac vein compression was defined by using qualitative and quantitative measures. Quantitative measures include the minor diameter of the LCIV at the point of maximal compression and percentage compression, which can be defined as the minor diameter of the LCIV at maximal compression divided by the minor diameter of the LCIV prior to the bifurcation of the LCIV or the minor diameter of the LCIV at the point of maximal compression divided by the minor diameter of the right common iliac vein (RCIV) prior to the bifurcation of the RCIV. As the diameter of the LCIV may be influenced by the presence or absence of clot, we used the measure of percentage compression in which the distal RCIV was the reference denominator as the primary measure of our exposure of interest. A qualitative estimate of iliac vein compression was estimated by asking radiologists to rate the level of LCIV compression (none [0%–25%], mild [>25%–50%], moderate [>50%–75%], or severe [>75%]). Detailed information regarding the measurement of iliac vein compression and other related measurements are provided in Appendix E2 (online).
Figure 2:
Data entry form. AA = abdominal aorta.
All of the cases were read in duplicate by two board-certified radiologists during (S.M.) and 1 year after (L.C.) interventional radiology fellowship, with assessments of interreader variability. Intrareader variability was assessed by asking radiologists to reread 30 randomly selected cases (sample size based on convenience). Intrapatient variability was assessed by identifying patients who had undergone repeat CT for routine screening purposes (typically patients with cancer) or patients who had undergone repeat CT for reasons not related to the iliac vein anatomy. By using the continuous outcome of the compressed LCIV diameters, intraclass correlation coefficients were determined and Bland-Altman plots were generated.
Study radiologists who are aware of the link between iliac vein compression and left-sided DVT might be more likely to report higher levels of iliac vein compression if they observe left-sided DVT. A masking substudy of 25 patients was performed to provide a quantitative estimate of the potential bias associated with unmasked readings (Appendix E3 [online]).
Statistical Analysis
Baseline demographic variables in patients with left-sided DVT and those with right-sided DVT were described by using means for continuous variables and proportions for categoric variables. Statistical significance was tested by using t tests for continuous variables and χ2 tests for categoric variables (P < .05).
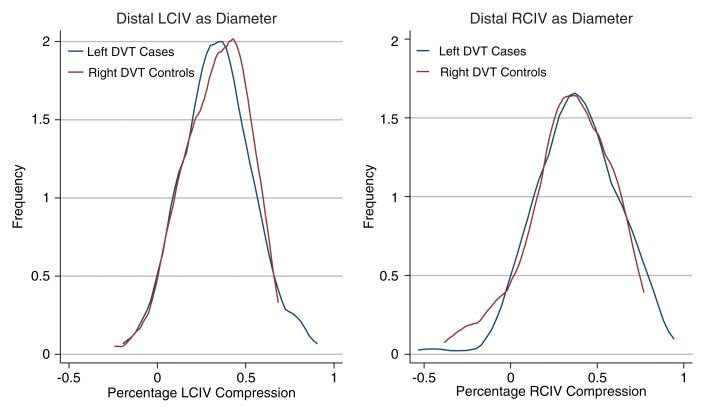
The main exposure (iliac vein compression) was evaluated by creating density plots of compressed LCIV diameters, distal LCIV diameters, RCIV diameters, and subjective compression ratings separately according to the side of DVT.
Logistic regression analysis was performed with the outcome as the log odds of being a left-sided DVT case and with the exposures as the different measures of iliac vein compression. First, we evaluated the hypothesis that a binary threshold for iliac vein compression is associated with left-sided DVT. A priori we did not have a strong prior belief about any particular threshold or cutpoint; however, one study suggested 70% as a cutpoint for iliac vein compression (8). Hence, for our primary analysis, we used a logistic regression model in which percentage compression (using the distal RCIV as the reference diameter) was modeled as a binary risk factor (yes or no) with 70% used as the cutpoint. To assess the sensitivity of our results to the choice of the threshold, we ran logistic regression models by using different thresholds for percentage compression, using the distal RCIV and LCIV as reference diameter.
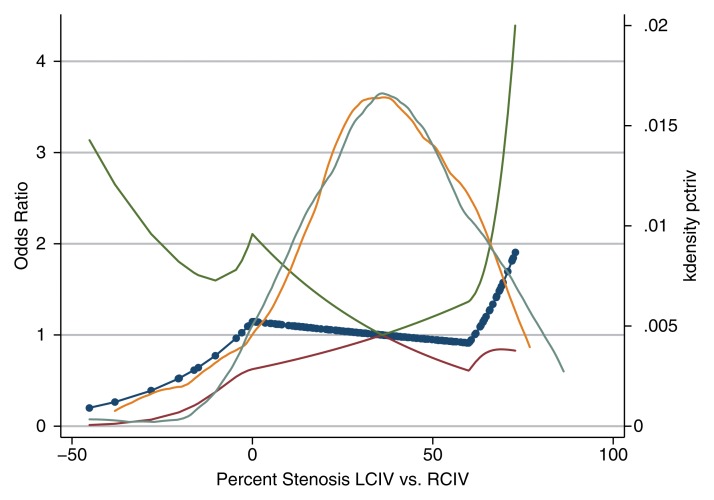
To determine if greater percentage compression levels were associated with increasingly greater odds of left DVT, we used logistic regression with splines. Lowess plots were generated for exploratory analysis. Given the prior suggestion that 70% compression may be clinically relevant, the 70% percentage compression threshold was evaluated as a spline knot for the primary analysis. Different combinations of spline knots were investigated to assess the sensitivity of our findings.
Various risk factors for DVT were collected, including recent surgery, cancer, oral contraceptive usage, trauma, short-term immobility, long-term immobility, hypercoagulable states, previous or concurrent DVT or PE, obesity, and pregnancy. However, we did not expect any of these risk factors to be confounders in our study (Appendix E4 [online]). Primary analyses were unadjusted and adjusted only for demographic variables (age, sex, ethnicity). We also conducted more customary analyses to determine if measured covariates met statistical criteria for confounders as long as they were not hypothesized to act through venous compression (Appendix E5 [online]).
In terms of effect modifiers, the left-sidedness of DVT has been noted to be more pronounced (9) in certain types of patient groups. We performed stratified analyses to identify possible effect modification by location, chronicity, and extent of DVT (iliofemoral vs popliteal) (10), mode of diagnosis, sex, ethnicity, indication, and timing of the CT studies. Tests of heterogeneity were performed, with P < .01 used as a cutoff for identification of effect modifiers.
Summary estimates were produced with 95% confidence intervals (CIs), and statistical significance was assessed by using Wald tests (P < .05). Sensitivity analyses were performed, excluding potentially influential observations and cases with atypical anatomy in which the right common iliac artery overlies the RCIV.
Sample Size and Power
Prior case series suggested a difference in proportions of 18%–26% between patients with left-sided and those with right-sided DVT (ie, proportion on the left of 59%–63%) (4). On the basis of these estimates, a sample size of 216 patients would be required to detect a difference of 17% with 80% power (11).
Results
Demographic Data
Patients with left- and those with right-leg DVT were comparable in terms of baseline demographic data and risk factors for DVT (Table 1). Although patients with right- and those with left-leg DVT were equally likely to have PE at presentation, patients with left-leg DVT were less likely to have a history of PE (P = .015). Patients with left DVT were more likely to have involvement of the profunda femoris (P = .003) and common femoral vein (P < .001) segments (Table 2) at presentation.
Table 1.
Baseline Clinical Characteristics of Patients with Left- and Those with Right-Leg DVT
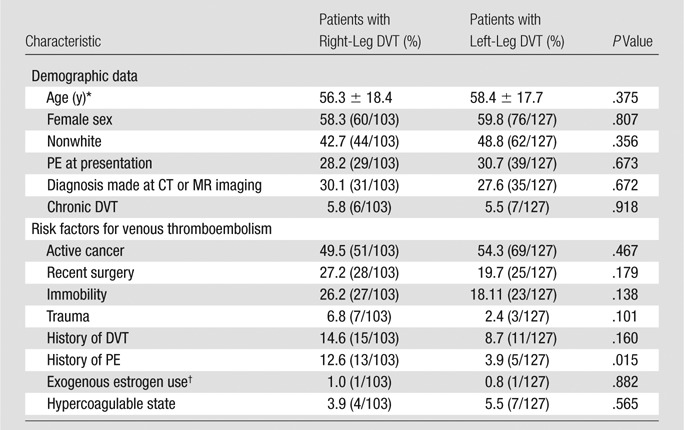
Note.—Unless otherwise specified, data are percentages of patients, with raw data in parentheses.
Data are means ± standard deviations.
Hormone replacement therapy or oral contraceptives.
Table 2.
Distribution of DVT Locations according to Side of DVT
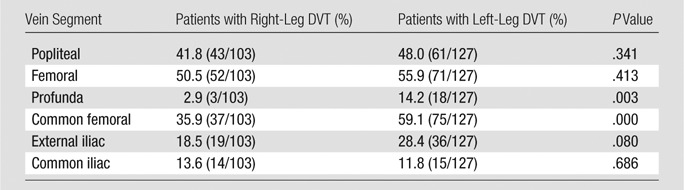
Note.—Data are percentages of patients, with raw data in parentheses (eg, 41.8% of patients with DVT in their right leg were noted to have clot in their popliteal vein). Multiple segments of the vein could be involved; hence, column totals do not add up to 100%.
Measurement of Iliac Vein Compression
Average values were determined for each of the measurements obtained in our study, along with summary estimates of interreader, intrareader, and intrapatient correlations (Tables 3, 4). For the main quantitative measures used to determine iliac vein compression, intraclass correlation coefficients ranged from 0.560 to 0.957. In our masking substudy, the intraclass correlation coefficient for comparison of masked and unmasked readings was noted to be 0.942 for both radiologists combined. According to graphic inspection, increasingly severe degrees of iliac vein compression (qualitative measure of iliac vein compression) were associated with higher mean percentages of percentage LCIV compression using both measures of percentage compression (Appendix E3 [online]).
Table 3.
Results of CT Readings: Intraclass Correlation Coefficients for Continuous Measurements
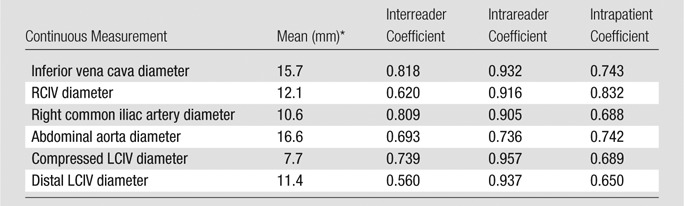
Data represent the average of two radiologists’ readings.
Table 4.
Results of CT Readings: Intraclass Correlation Coefficients for Ordinal or Binary Measurements
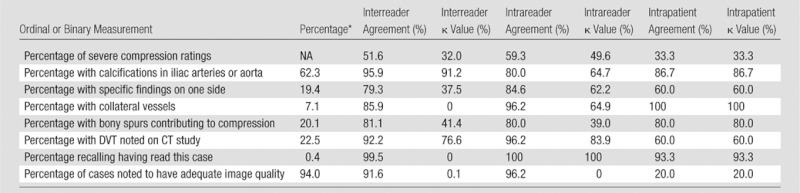
Note.—NA = not applicable.
Mean percentage, averaged between the two radiologists’ readings.
Percentage Compression
The distributions of the measures of iliac vein compression according to DVT side are displayed in Figures 3 and 4. By using the primary measure of iliac vein compression and the distal RCIV as the denominator for the calculation of percentage compression, mean percentage compression was 36.6% (95% CI: 33.4, 39.7). In terms of percentage compression categories, 74.8% (166 of 222) of patients were noted to have greater than 25% compression, 33.3% had greater than 50% compression, and 7.2% had greater than 70% compression. Twelve (9.8%) of 123 patients with left DVT were noted to have greater than 70% compression, compared with four (4.0%) of 99 patients with right DVT.
Figure 3:
Density plots of compressed LCIV diameter according to side of DVT.
Figure 4:
Density plots of percentage LCIV compression values according to side of DVT and reference used in the denominator to define compression. Left: LCIV as the reference. Right: RCIV as the reference.
Iliac Vein Compression as a Risk Factor for Left DVT
First, we tested our hypothesis that iliac vein compression greater than 70% (yes or no) would be associated with greater odds of left DVT. Using logistic regression analysis adjusted for demographic variables (age, sex, ethnicity), we found that iliac vein compression greater than 70% (yes or no) was associated with increased odds of left DVT (odds ratio [OR]: 3.03; 95% CI: 0.91, 10.15) (Table 5). Results were similar for other measures of compression and with different thresholds for iliac vein compression. Results were also similar after adjusting for various risk factors for DVT. Tests for interaction for age, sex, presence of unilateral findings, ethnicity, presence of lower extremity or pulmonary symptoms, mode of DVT detection, location and extent of DVT, timing and indication for CT examination, presence of collateral vessels, and history of PE were not statistically significant (P > .01) (Table 6).
Table 5.
Outcomes of Logistic Regression Analysis with Left versus Right DVT as Outcome and Measures of LCIV Compression as Exposure
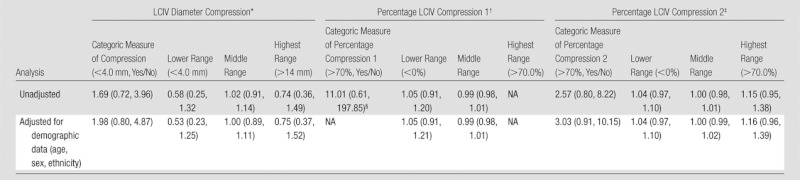
Note.—Data are ORs, with 95% CIs in parentheses. NA = not applicable.
For the range values, ORs are those for left DVT for a 1-mm increase in compressed LCIV diameter for each range of compressed iliac vein diameter (>4.0 mm, 4–14 mm, and >14 mm).
Percentage LCIV Compression 1 is that calculated by using the distal LCIV as the reference denominator. For the range values, ORs are spline ORs for left DVT for a 1% increase in percentage compression for each region of percentage compression (<0%, 0%–70%, and >70%).
Percentage LCIV Compression 2 is that calculated by using the distal RCIV as the reference denominator. For the range values, ORs are spline ORs for left DVT for a 1% increase in percentage compression for each region of percentage compression (<0%, 0%–70%, and >70%).
This OR was estimated—six of six patients with compression > 70% had left DVT, compared with 117 of 216 patients with < 70% compression. The OR was estimated by adding 0.5 to each cell.
Table 6.
Results of Effect Modification Analyses
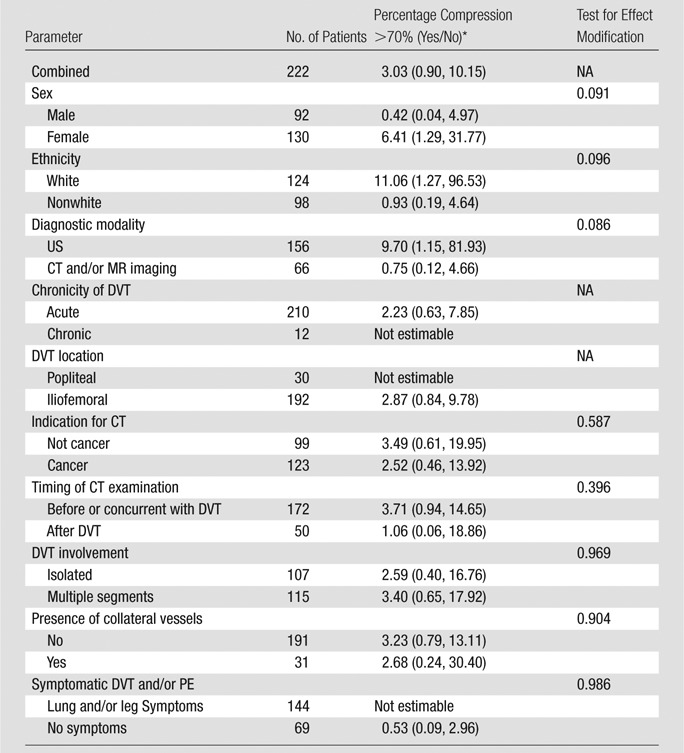
Note.—NA = not applicable.
Data are ORs, with 95% CIs in parentheses.
Given that iliac vein compression greater than 70% may be associated with left DVT, we then sought to determine if greater levels of percentage compression were associated with greater odds of left DVT. Lowess plots were created to explore the relationship between percentage compression and left DVT. Splines were used in logistic regression, with left DVT as the outcome and percentage LCIV compression as the exposure, with knots set at 0.0% and 70% (Fig 5). At levels of compression of less than 70%, greater percentage compression was not found to be associated with increasing odds of left DVT per 1% increase in percentage compression (ORs: 1.00, 0.99, 1.02) (adjusted for demographic data) (Table 5). These results were consistent using unadjusted and adjusted logistic regression models, as well as in logistic regression models using other spline knots and measures of percentage compression.
Figure 5:
Odds of left DVT versus percentage LCIV compression (using distal RCIV as reference denominator) is modeled by using logistic regression with splines (solid line with dots) with 95% confidence limits (upper and lower lines). Knots are set at 0% and 70% with reference at 36.6%. Density plot with distributions of percentage compression values by side of DVT is overlaid on top of regression lines (blue line = patients with left-sided DVT, orange line = patients with right-sided DVT). kdensity = Frequency of patients with left-sided DVT or right-sided DVT with a given level of percentage stenosis.
Discussion
The results of our study suggest that mild or moderate levels of iliac vein compression were not associated with left DVT; however, iliac vein compression greater than 70% was associated with substantially greater odds for left DVT. We also noted that greater than 70% iliac vein compression occurred in 9.8% of patients with left DVT (12 of 123) and 4.0% of patients with right DVT (four of 99).
The results of our study are consistent with those of previous smaller studies on iliac vein compression. Fraser et al (4) found evidence of at least 50% iliac vein compression in 11 of 36 patients (31%) with left-sided DVT compared with two of 20 patients (10%) with right-sided DVT and four of 28 control patients (14.3%). Oguzkurt et al (8) compared 34 patients with left-sided DVT and 34 age-and sex-matched control subjects without DVT and found that percentage compression in patients with left-sided DVT was significantly higher in patients with left-sided DVT (74% vs 28%, P < .001). The results of our study suggest that iliac vein compression (>70%) may be associated with an elevated risk of left-sided DVT.
Although the data are limited, we found a higher prevalence of severe iliac vein compression in our study compared with prior studies. In a sample of 50 emergency room patients undergoing pelvic CT, Kibbe et al (6) found evidence of greater than 50% iliac vein compression in 24% of patients (12 of 50); however, only 2% of patients were noted to have iliac vein compression greater than 70% (one of 50), compared with 7.2% of patients in our study. The higher percentages noted in our study may also be attributable to measurement error or selection biases in which our sample of patients may have been enriched for causes of DVT that required percutaneous management at a tertiary care center.
In our study, we also noted that patients with right DVT were more likely to have a history of PE than patients with left DVT. In a study of 75 patients with unilateral DVT, Chan et al (5) found that LCIV compression (compressed diameter, <4 mm) was associated with decreased odds of symptomatic PE. These results provide some support for the hypothesis that LCIV compression may impede clot progression to the lungs. Additional studies of the natural history of left versus right DVT are required to evaluate this hypothesis.
In our subgroup analyses, we did not find any statistically significant differences in the effects of iliac vein compression in different subgroups; however, we did note large differences in some of the subgroups (women vs men, white vs nonwhite patients, timing and mode of DVT diagnosis). Although these differences were not statistically significant, these subgroup comparisons may have been underpowered and represent findings for future investigations.
Limitations of our study included retrospective data collection, the lack of an established reference standard measurement, a lack of comprehensive evaluation of the deep veins, and a small number of patients with high levels of compression. We noticed a lower ratio of left:right DVT in patients with DVT and pelvic CT compared with all patients with DVT, suggesting that our selection criteria may have decreased the overall proportion of patients with iliac vein compression. Although this may limit the generalizability of our findings, we did not find any statistically significant differences when we stratified according to indication for CT. In addition, the use of patients with right-sided DVT as a control group limits confounding in our data set.
The lack of an established reference standard measurement of iliac vein compression prevents us from fully evaluating pelvic CT as a method of diagnosing iliac vein compression. Prior investigators have described the use of intravascular US to characterize not only percentage compression but also venous webs and spurs (12). Although this method may be used to detect more cases of iliac vein compression, it may not be feasible in a population-based study. Although these data were not available, three-dimensional reconstructions would have provided precise determinations of the cross-sectional area of the compressed iliac vein. In the absence of a comparison with a reference standard measurement, we collected and compared different measures of iliac vein compression to provide us with indirect assessments of iliac vein compression. High intrareader (0.91–0.94) intraclass correlation coefficients were noted, while moderate interreader (0.56–0.74) and intrapatient (0.65–0.83) intraclass correlation coefficients were noted. Overall, similar results were noted by using quantitative and qualitative measures of iliac vein compression. Finally, comprehensive evaluation of the deep veins was not performed, as patients with DVT diagnosed at pelvic CT may have had undiagnosed popliteal DVT. However, the percentage of cases and control subjects in whom the diagnosis was made with CT and/or MR imaging was similar, suggesting a source of error that biases the study toward the null (13).
In conclusion, we found that mild or moderate iliac vein compression was not associated with an elevated risk of left-sided DVT, while greater than 70% compression may be associated with an elevated risk of left-sided DVT. Further studies are needed to better characterize the risk and outcomes of patients with high levels of LCIV compression.
Advances in Knowledge.
• Mild or moderate levels of left common iliac vein compression noted at pelvic CT were not associated with left deep venous thrombosis (DVT).
• Iliac vein compression greater than 70% may be associated with an elevated risk of left DVT.
• Iliac vein compression greater than 70% occurred in 7.2% (16 of 222) of all patients in our study.
Implication for Patient Care.
• Greater than 70% iliac vein compression noted at pelvic CT may be associated with left-sided DVT, but mild or moderate levels of iliac vein compression at pelvic CT were not associated with left-sided DVT.
Disclosures of Conflicts of Interest: A.N. No relevant conflicts of interest to disclose. J.E. No relevant conflicts of interest to disclose. L.C. No relevant conflicts of interest to disclose. S.M. No relevant conflicts of interest to disclose. M.A. No relevant conflicts of interest to disclose. A.R.S. No relevant conflicts of interest to disclose. M.S. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: is a consultant for Sanofi-Aventis, Daiichi-Sankyo, Eisai, and Janssen Healthcare; has given expert testimony for Anderson Daniel; Chason, Rosner, Leary and Marshall; and Sands Anderson; institution has grants or grants pending with Bristol Myers Squibb; is on the speakers bureaus of Sanofi-Aventis and Ortho-McNeil; has received payment for development of educational presentations from Ortho-McNeil. Other relationships: none to disclose. J.C. No relevant conflicts of interest to disclose. N.P. No relevant conflicts of interest to disclose. K.H. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: none to disclose.
Supplementary Material
Received August 10, 2011; revision requested September 22; revision received February 2, 2012; accepted March 2; final version accepted June 5.
From the 2010 RSNA Annual Meeting.
Funding: This research was supported by the National Institutes of Health (grant 5F30HL094095).
Abbreviations:
- CI
- confidence interval
- DVT
- deep venous thrombosis
- LCIV
- left common iliac vein
- OR
- odds ratio
- PE
- pulmonary embolism
- RCIV
- right common iliac vein
References
- 1.Fazel R, Froehlich JB, Williams DM, Saint S, Nallamothu BK. Clinical problem-solving: a sinister development—a 35-year-old woman presented to the emergency department with a 2-day history of progressive swelling and pain in her left leg, without antecedent trauma. N Engl J Med 2007;357(1):53–59 . [DOI] [PubMed] [Google Scholar]
- 2.Virchow R. Uber die erweiterung kleiner gefasse [About the expansion of small vessels]. Arch Path Anat 1851;3:427 [Google Scholar]
- 3.May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology 1957;8(5):419–427 [DOI] [PubMed] [Google Scholar]
- 4.Fraser DG, Moody AR, Martel A, Morgan PS. Re-evaluation of iliac compression syndrome using magnetic resonance imaging in patients with acute deep venous thromboses. J Vasc Surg 2004;40(4):604–611 [DOI] [PubMed] [Google Scholar]
- 5.Chan KT, Popat RA, Sze DY, et al. Common iliac vein stenosis and risk of symptomatic pulmonary embolism: an inverse correlation. J Vasc Interv Radiol 2011;22(2):133–141 [DOI] [PubMed] [Google Scholar]
- 6.Kibbe MR, Ujiki M, Goodwin AL, Eskandari M, Yao J, Matsumura J. Iliac vein compression in an asymptomatic patient population. J Vasc Surg 2004;39(5):937–943 [DOI] [PubMed] [Google Scholar]
- 7.Kearon C. Natural history of venous thromboembolism. Circulation 2003;107(23 Suppl 1):I22–I30 [DOI] [PubMed] [Google Scholar]
- 8.Oguzkurt L, Ozkan U, Ulusan S, Koc Z, Tercan F. Compression of the left common iliac vein in asymptomatic subjects and patients with left iliofemoral deep vein thrombosis. J Vasc Interv Radiol 2008;19(3):366–370; quiz 371 . [DOI] [PubMed] [Google Scholar]
- 9.Ouriel K, Green RM, Greenberg RK, Clair DG. The anatomy of deep venous thrombosis of the lower extremity. J Vasc Surg 2000;31(5):895–900 . [DOI] [PubMed] [Google Scholar]
- 10.Chung JW, Yoon CJ, Jung SI, et al. Acute iliofemoral deep vein thrombosis: evaluation of underlying anatomic abnormalities by spiral CT venography. J Vasc Interv Radiol 2004;15(3):249–256 [DOI] [PubMed] [Google Scholar]
- 11.Eng J. Sample size estimation: how many individuals should be studied? Radiology 2003;227(2):309–313 [DOI] [PubMed] [Google Scholar]
- 12.Raju S, Neglen P. High prevalence of nonthrombotic iliac vein lesions in chronic venous disease: a permissive role in pathogenicity. J Vasc Surg 2006;44(1):136–143; discussion 144 [DOI] [PubMed] [Google Scholar]
- 13.Grimes DA, Schulz KF. Bias and causal associations in observational research. Lancet 2002;359(9302):248–252 [DOI] [PubMed] [Google Scholar]
- 14.Hernán MA, Hernández-Díaz S, Werler MM, Mitchell AA. Causal knowledge as a prerequisite for confounding evaluation: an application to birth defects epidemiology. Am J Epidemiol 2002;155(2):176–184 [DOI] [PubMed] [Google Scholar]
- 15.Greenland S, Robins JM. Identifiability, exchangeability, and epidemiological confounding. Int J Epidemiol 1986;15(3):413–419 [DOI] [PubMed] [Google Scholar]
- 16.James AH, Tapson VF, Goldhaber SZ. Thrombosis during pregnancy and the postpartum period. Am J Obstet Gynecol 2005;193(1):216–219 [DOI] [PubMed] [Google Scholar]
- 17.Marik PE, Plante LA. Venous thromboembolic disease and pregnancy. N Engl J Med 2008;359(19):2025–2033 [DOI] [PubMed] [Google Scholar]
- 18.Moreland NC, Ujiki M, Matsumura JS, et al. Decreased incidence of left common iliac vein compression in patients with abdominal aortic aneurysms. J Vasc Surg 2006;44(3):595–600 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.