Abstract
Unemployment and underemployment have adverse mental and physical health consequences, such as increased stress and depression. Health damaging behaviors like unhealthy eating, smoking, and alcohol use may be used to cope, contributing to chronic disease risk. In this adverse economic climate, it is vital to understand the health implications of unemployment and underemployment as well as underlying mechanisms. A randomized household survey of adults in six low resource communities was conducted in New Haven, Connecticut in 2009, yielding a sample of 1205 (73% participation) racially diverse adults (61% Black, 20% Latino, 12% White) ages 18–65 (61% women). We used ANOVA to test group differences and structural equation modeling to test mediation. 14.5% were unemployed and looking for work, 18.4% worked part-time, 38.2% worked full-time. Those employed full-time reported the least damaging psychological factors and health behaviors: lowest levels of stress and depression, most healthy and least unhealthy eating, most physical activity, and lowest levels of smoking and drinking. Those employed part-time fell in the middle, and those unemployed fell on the unhealthy end of all psychological and behavioral factors. Stress significantly mediated the associations of full-time employment with frequency of unhealthy eating and physical activity, and amount of cigarette smoking and alcohol consumption. Depression significantly mediated the association of full-time employment with frequency of healthy eating. Compared to <10% nationwide, rates of unemployment in this sample were high. Both those unemployed and employed part-time reported adverse health behaviors as compared to those employed full-time, partially mediated by heightened stress and depression. It is vital for the health and well-being of the nation to increase not simply employment, but specifically full-time employment. Provision of mental health services to those unemployed and underemployed should be a priority to promote healthier lifestyles and prevent costly future chronic disease.
Keywords: USA, Alcohol, Depression, Diet, Exercise, Employment, Smoking, Stress, Unemployment
Introduction
Rates of unemployment in the U.S. are as high as they have been in two decades. Rates of poverty are rising, and the disparity in income between rich and poor is increasing, with Black and Latino Americans hit hardest (DeNavas-Walt, Proctor, & Smith, 2011). Although the connection between unemployment and negative health outcomes is well-established (Kasl & Jones, 2007), there is a call for contemporary research to understand health implications of unemployment due to the current economic recession (Bambra, 2010; Bartley & Ferrie, 2010). Because of changes and cuts to social welfare services, decreases in the number of secure, full-time jobs, and general changes in the workforce over the past several years, it is important to re-examine the associations of employment status with mental and physical health, as they may differ from past decades (Bambra, 2010). Given current tough economic times, understanding the health implications of unemployment and underemployment as well as the mechanisms involved is vital.
Job loss or unemployment leads to increased anxiety and depressive symptoms, among other psychiatric symptoms (Dooley, Catalano, & Wilson, 1994; Hammarström & Janlert, 2002). Communities with high rates of unemployment have higher rates of suicide and mental hospitalization (Dooley & Catalano, 1986). Unemployment leads to increases in smoking and alcohol use (Hammarström, 1994; Hammarström & Janlert, 2002; Mossakowski, 2008), somatic symptoms or ailments (Grayson, 1989; Hammarström & Janlert, 2002), hospitalization (Eliason & Storrie, 2009), and risk of early death (Lundin, Lundberg, Hallsten, Ottosson, & Hemmingsson, 2010; Roelfs, Shor, Davidson, & Schwartz, 2011).
There has been increasing interest not only in unemployment, but in the continuum of employment, including those who are underemployed (e.g., working part-time involuntarily) or experience job insecurity (Dooley, 2003; Kasl & Jones, 2007). Inadequate or underemployment is associated with increased depression and alcohol use, lowered self-concept and functional health, and increased chronic disease (Dooley, Prause, & Ham-Rowbottom, 2000; Friedland & Price, 2003). Given these findings and high rates of underemployment in the current economic climate, the comparison of full-time employment to both unemployment and underemployment is crucial.
Understanding the mechanisms through which employment status affects health outcomes is important to knowing how best to intervene. Some evidence suggests that economic insecurity or poverty, stress, and lowered self-esteem or self-concept are mediators of the relationship between employment status and health outcomes (Bambra, 2010; Bartley, 1994; Kasl & Jones, 2007), although the mechanisms involved have not been as well studied. Other research suggests that negative health behaviors (e.g., binge eating, smoking, drinking) may be used as coping mechanisms for stress, anxiety, and depression (Harrington et al., 2006; Witkiewitz et al., 2011). Taken together, stress and depression may be important mediators of the relationship between employment status and health behaviors.
This investigation includes survey data from a racially diverse, low-income, urban U.S. sample within the context of high neighborhood unemployment. This study aims to: (1) explore associations of employment status with mental health (stress, depressive symptoms) and health behaviors (healthy and unhealthy eating, physical activity, cigarette smoking, alcohol consumption); and (2) test whether stress and depressive symptoms mediate the relationships between employment status and health behaviors.
Methods
A randomized household health survey was conducted in six low-income neighborhoods (42% of children and 34% of the general population living in poverty based on American Community Survey 5-year estimates, 2005–2009) in New Haven, Connecticut from October 12th to November 23rd, 2009, at the height of the economic recession. Institutional Review Board approval was obtained in advance from Yale University Human Subjects Committee.
Procedure
The survey was interviewer-administered in English and Spanish. Households were randomized from a complete list of addresses in each neighborhood provided by city government, and each was approached three times until: (1) an eligible resident answered and consented; (2) an eligible resident answered and refused; or (3) no one answered and another address was randomly selected. Trained surveyors from the community conducted interviews and collected data via handheld computers. Participants received a $10 grocery store voucher and were entered into a $500 raffle.
Participants
Of 3980 households randomized, for 1651 a resident was reached within three attempts, and 73% of those chose to participate. Thus, 1205 interviews were conducted with racially/ethnically diverse adults (61% Black, 20% Latino, 12% White, 3% Multi-racial, 1% Asian or Pacific Islander, 1% American Indian or Alaska Native, 1% refused to report) aged 18–65 years, 61% being women. Of 1205 participants, 14.5% (n = 175) reported being unemployed and looking for work, 18.4% (n = 222) reported working part-time, 38.2% (n = 460) reported working full-time. The final analytic sample included these 857 participants. Participants who reported not working in the past 30 days but not looking for work (e.g., students, homemakers, retired, unable to work) were excluded from analyses. Compared with the analytic sample, excluded participants were more likely to be women (67%), have a High School diploma/GED or less (62%), be older (mean age = 45), and report more chronic conditions (mean = 2), but there were no differences in race/ethnicity (61% Black, 20% Latino).
Measures
Employment status
Participants reported whether they had a paid job in the past 30 days. If “Yes,” participants reported if it was full-time or part-time. If “No,” participants indicated whether they were currently looking for work or not working for other reasons.
Stress
Participants were asked “Have you been feeling tense, stressed, or under a lot of pressure during the past month?” (WHO, 1995). They responded from 1 (Not at all) to 4 (Yes, my life is almost unbearable).
Depressive symptoms
Participants were asked during the last month if they have often been bothered by… “feeling down, depressed, or hopeless?” and “little interest or pleasure in doing things?” (Whooley, Avins, Miranda, & Browner, 1997). A sum of depressive symptoms was created, with resulting scale range from 0 to 2 (no/yes to each question).
Healthy eating
Participants indicated how many days per week they had the following: vegetables, fruits, beans or nuts, whole grains (Duffany et al., 2011). A mean was calculated to create a composite score of frequency of healthy eating.
Unhealthy eating
Participants indicated how many days per week they had the following: sweets, foods high in fat and salt, sugar-sweetened beverages (Duffany et al., 2011). A mean was calculated to create a composite score of frequency of unhealthy eating.
Exercise
Participants reported how many days during the past week and minutes per day they did vigorous and moderate physical activity. Following U.S. Department of Health and Human Services guidelines for physical activity (HHS, 2008), with every minute of vigorous physical activity counting for twice the minutes of moderate physical activity, we created a composite measure of minutes of physical activity in the past week by adding weekly moderate activity minutes with twice the weekly vigorous activity minutes.
Cigarette smoking
Participants indicated whether they smoke cigarettes daily. If “Yes,” participants reported how many cigarettes they smoke daily on average (WHO, 2008). Participants answering “No” were coded as smoking 0 cigarettes daily.
Alcohol consumption
Participants reported how many alcoholic drinks they have on average in one day when they drink (WHO, 2008). Participants reporting not drinking were coded as consuming 0 drinks.
Participant characteristics
Participants reported gender, race/ethnicity, age, education level, and diagnosed chronic conditions.
Data analyses
For Aim 1, we used ANOVA and post-hoc analyses (with SPSS) to compare those employed full-time, employed part-time, and unemployed in self-reported mental health (stress, depressive symptoms) and health behaviors (healthy and unhealthy eating, physical activity, cigarette smoking, alcohol consumption). Participant characteristics were used as control variables, and we tested gender and race/ethnicity as moderators. For Aim 2, we used structural equation modeling (with AMOS) to test whether stress and depressive symptoms were mediators of the associations that employment status had with health behaviors.
Results
Differences by employment status
Means and standard deviations or percentages for demographics and study variables by employment status and for the total sample are in Table 1. ANOVAs comparing those employed full-time, those employed part-time, and those unemployed revealed significant differences for stress F(2, 854) = 4.07, p = .017, depressive symptoms F(2, 854) = 9.91, p < .001, healthy eating F(2, 854) = 8.19, p < .001, unhealthy eating F(2, 854) = 8.84, p < .001, physical activity F(2, 850) = 5.32, p = .005, and cigarette smoking F(2, 854) = 10.76, p < .001, and marginally significant for alcohol consumption F(2, 850) = 2.43, p = .089. Controlling for age, gender, race, education level, or number of chronic conditions did not change results. Those employed full-time reported the best, and those unemployed the worst mental health and health behaviors. Those employed part-time fell in the middle of the other two groups. Additionally, we conducted follow-up 3-way ANOVAs testing whether gender and race/ethnicity (including two largest groups: Blacks and Latinos) moderated the relationships of employment status with any of the mental and physical health variables, or whether there were any 3-way interactions among gender, race/ethnicity, and employment status. All interactions were nonsignificant.
Table 1.
Means (and standard deviations) or percentages by employment status and for total analytic sample.
| Unemployed (n = 175) | Employed part-time (n = 222) | Employed Full-time (n = 460) | Total sample (n = 857) | |
|---|---|---|---|---|
| % Female | 55.4% | 65.8% | 56.5% | 58.7% |
| % Black | 54.9% | 62.2% | 62.6% | 60.9% |
| % Latino | 26.3% | 13.5% | 20.7% | 20.0% |
| % High school diploma/GED certificate or less | 71.3% | 54.8% | 47.1% | 54.1% |
| Age | 37.26 (12.67) | 35.85 (14.24) 40.16 (12.20) 38.45 (12.98) | ||
| Chronic conditions | 1.07 (1.17) | 1.11 (1.23) | 1.10 (1.30) | 1.10 (1.26) |
| Stress | 1.94 (.94)a | 1.90 (.88)a | 1.75 (.78)b | 1.83 (.84) |
| Depressive symptoms | .66 (.85)a | .53 (.76)a | .38 (.67)b | .48 (.74) |
| Healthy eating | 3.52 (1.54)a | 3.68 (1.59)a | 4.02 (1.49)b | 3.83 (1.54) |
| Unhealthy eating | 4.27 (1.96)a | 3.66 (2.02)b | 3.56 (1.87)b | 3.73 (1.95) |
| Physical activity | 605.15 (935.26)a | 811.62 (1366.66)ab | 1029.95 (1749.51)b | 885.97 (1525.26) |
| Cigarette smoking | 4.92 (7.35)a | 3.47 (6.65)b | 2.41 (5.38)c | 3.20 (6.24) |
| Alcohol consumption | 2.18 (3.26)a | 1.90 (3.05)ab | 1.64 (2.51)b | 1.82 (2.83) |
Note: Results of ANOVA post-hoc tests for mental and physical health outcomes are shown with subscripts. Means not statistically significantly different at p < .05 share a letter; those that are statistically significantly different do not share a letter.
Post-hoc tests (least-squared difference) comparing differences among all three groups revealed that those working full-time reported significantly lower stress and depressive symptoms, and more frequent healthy eating than both those working part-time and those unemployed (no significant differences between the latter two groups). Both those working full-time and those working part-time reported significantly less frequent unhealthy eating than those unemployed. Those working full-time reported significantly more physical activity than those unemployed. All three groups differed significantly from each other for amount of cigarette smoking. Those working full-time reported less alcohol consumption than those unemployed.
These results suggest that differences specifically between those working full-time and both of the other groups (part-time and unemployed) were driving many of the overall group differences found in the ANOVAs, indicating a significant health benefit of working full-time. Based on these results and past research suggesting underemployment has similar negative health consequences as unemployment (Dooley et al., 2000; Friedland & Price, 2003), we conducted remaining analyses with a combined group of those working part-time and unemployed (397) compared to working full-time (460).
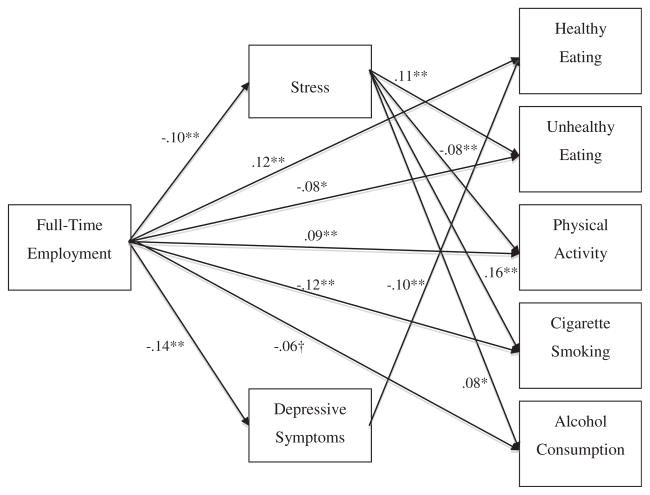
Testing mediation
We used structural equation modeling to test the hypothesis that stress and depressive symptoms mediate the relationships of full-time employment with healthy and unhealthy eating, physical activity, cigarette smoking, and alcohol consumption. Bivariate correlations are in Table 2. Missing data points were imputed using AMOS regression imputation. We began with a fully saturated model, with full-time employment predicting both hypothesized mediators and all five hypothesized outcomes, and both hypothesized mediators predicting all five hypothesized outcomes. The mediators’ error terms were correlated and the outcomes’ error terms were correlated, given connections among these variables. We removed nonsignificant paths (p > .10; Kline, 2011) one by one, with the highest p values first, resulting in the model in Fig. 1. Model fit statistics indicated a good fitting model: χ2(5) = 4.41, p = .492; RMSEA = .000, CI = .000–.045; AIC = 66.41.
Table 2.
Bivariate correlations.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Full-time employment | – | ||||||
| 2. Stress | −.10** | – | |||||
| 3. Depressive symptoms | −.14** | .53** | – | ||||
| 4. Healthy eating | .13** | −.05 | −.11** | – | |||
| 5. Unhealthy eating | −.10** | .12** | .11** | −.15** | – | ||
| 6. Physical activity | .10** | −.09** | −.01 | .07* | .03 | – | |
| 7. Cigarette smoking | −.14** | .17** | .11** | −.14** | .16** | .05 | – |
| 8. Alcohol consumption | −.07** | .09** | .08* | .03 | .12** | .10** | .17** |
p < .05;
p < .01.
Fig. 1.
Structural equation model results. Coefficients shown are standardized betas. †p < .10; *p < .05; **p < .01.
Paths remaining in the model are significant (ps < .05) and in the expected directions (Fig. 1), except for the marginally significant direct path from full-time employment to alcohol consumption (p = .074). Full-time employment has significant direct effects on healthy and unhealthy eating, physical activity, and cigarette smoking. Stress has significant direct effects on unhealthy eating, physical activity, cigarette smoking, and alcohol consumption. Depressive symptoms have a direct effect on healthy eating. Using bootstrapping methods we obtained p values for each of the indirect effects from full-time employment to outcome variables, and these indirect effects were all significant (ps < .05). Results suggest that stress partially mediates the association of full-time employment with unhealthy eating, physical activity, cigarette smoking, and alcohol consumption, and that depressive symptoms partially mediate the association of full-time employment with healthy eating.
Because of some evidence that health behaviors can affect employment over time (e.g., Jusot, Khlat, Rochereau, & Sermet, 2008), we also tested the reverse model, with the five health behaviors as main predictors, stress and depression as mediators, and full-time employment as the outcome. This model did not fit the data as well as the original model: χ2 (5) = 17.73, p = .003; RMSEA = .055, CI = .028–.083; AIC = 79.73.
Discussion
We examined the relationship of employment status with mental health outcomes and physical health behaviors among a mostly Black and Latino sample of adults living in six low-income neighborhoods in New Haven, Connecticut. Compared to <10% nationwide (based on U.S. Bureau of Labor Statistics), rates of unemployment in this sample were high (20.4% of labor force).
Being employed full-time was associated with lower levels of stress and depressive symptoms, more frequent healthy eating, less frequent unhealthy eating, more physical activity, less cigarette smoking, and less alcohol consumption, compared with being unemployed or working part-time. Results suggest the importance of full-time employment (not just any employment) for health and well-being. We found that stress is a mechanism through which full-time employment relates to unhealthy eating behaviors, physical activity, cigarette smoking, and alcohol consumption, and that depressive symptoms are a mechanism through which full-time employment relates to healthy eating behaviors. Unemployment and underemployment may be associated with unhealthy coping strategies because of the increases in stress and depression. More work is documenting the negative effects of the economic climate on mental health (e.g., Sargent-Cox, Butterworth, & Anstey, 2011), and worldwide economic trends may lead to increases in unhealthy coping strategies with potential increases in chronic disease to follow. This is especially true for low-income people of color in the U.S. living in urban neighborhoods disproportionately burdened by job loss.
The effects of employment status did not vary by gender or race/ ethnicity in this sample. With increasing numbers of women in the workforce, results suggest employment status is just as important to mental health and health behaviors for women as for men. However, these findings may vary by health outcome and social context and should continue to be explored.
Because the survey was short to minimize participant burden and maximize participation, there are some weaknesses of measures. Stress was assessed with one item and depressive symptoms were assessed with two items. However, these are established measures of mental health and were found to be important mediators between employment status and health behaviors. There also was no true measure of underemployment because participants reporting working part-time did not indicate whether they preferred to work full-time. Still, we found that those employed part-time showed increased levels of adverse mental health outcomes and health behaviors compared to those employed full-time. If anything, this study underestimates the negative effects of underemployment, as some adults may be have been working part-time by choice. The study was cross-sectional, therefore providing correlational evidence of relationships examined, not a causal test. However, although past work suggests these effects may be bi-directional, our comparison of a reverse model suggests the hypothesized direction of results provides the best fitting model. Longitudinal research must examine continued and longer-term effects of changes in employment status and the poor economic times. Future research should also examine potential buffers of the impact of un- or underemployment on mental and physical health outcomes, such as social support networks and economic resources.
Importantly, these data come from a large, randomized household survey in New Haven, Connecticut, and survey respondents were racially/ethnically diverse, allowing us to test demographic moderators and find that the relationships of employment status with mental and physical health did not vary by gender or race. This study was conducted at the height of the recession in 2009, with a highly vulnerable, understudied, and underserved population, highlighting the importance and uniqueness of the findings to the broader literature on employment and health. The study also contributes to our understanding of psychological mechanisms involved in the relationship between employment status and health and the direction of effects by its use of structural equation modeling.
This study supports past work suggesting it is vital for the health and well-being of all people to increase not simply employment, but specifically full-time employment. The number of secure, full-time jobs has been decreasing, which findings suggest may have adverse effects on mental health, health behaviors, and chronic disease. These effects will be detrimental to already suffering national economies, as the cost of treating mental and physical health problems will increase. Findings also suggest that free mental health services should be provided to the underemployed and unemployed, who may be at heightened risk of stress, depression, and unhealthy coping behaviors.
Acknowledgments
Funding for this study came from the Patrick and Catherine Weldon Donaghue Medical Research Foundation; Kresge Foundation, Emerging and Promising Practices; CTSA Grant Number UL1 RR024139 from the National Center for Research Resource; and The Aetna Foundation, which funded Dr. Rosenthal’s effort. Its contents are solely the responsibility of the authors. Research was conducted in affiliation with Community Interventions for Health, Oxford Health Alliance, Oxford England.
Footnotes
There is no known conflict of interest.
References
- Bambra C. Yesterday once more? Unemployment and health in the 21st century. Journal of Epidemiology and Community Health. 2010;64:213–215. doi: 10.1136/jech.2009.090621. [DOI] [PubMed] [Google Scholar]
- Bartley M. Unemployment and ill health: understanding the relationship. Journal of Epidemiology and Community Health. 1994;48:333–337. doi: 10.1136/jech.48.4.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartley M, Ferrie J. Do we need to worry about the health effects of unemployment? Journal of Epidemiology and Community Health. 2010;64:5–6. doi: 10.1136/jech.2009.089797. [DOI] [PubMed] [Google Scholar]
- DeNavas-Walt C, Proctor BD, Smith JC. U.S. Census Bureau, Current Population Reports. Washington, DC: U.S. Government Printing Office; 2011. Income, poverty, and health insurance coverage in the United States: 2010. [Google Scholar]
- Dooley D. Unemployment, underemployment, and mental health: conceptualizing employment status as a continuum. American Journal of Community Psychology. 2003;32:9–20. doi: 10.1023/a:1025634504740. [DOI] [PubMed] [Google Scholar]
- Dooley D, Catalano R. Do economic variables generate psychological problems? Different methods, different answers. In: MacFadyen AJ, MacFadyen HW, editors. Economic psychology: Intersections in theory and application. Amsterdam: North Holland; 1986. pp. 503–546. [Google Scholar]
- Dooley D, Catalano R, Wilson G. Depression and unemployment: panel findings from the epidemiologic catchment area study. American Journal of Community Psychology. 1994;22:745–765. doi: 10.1007/BF02521557. [DOI] [PubMed] [Google Scholar]
- Dooley D, Prause J, Ham-Rowbottom KA. Underemployment and depression: longitudinal relationships. Journal of Health and Social Behavior. 2000;41:421–436. [PubMed] [Google Scholar]
- Duffany KO, Finegood DT, Matthews D, McKee M, Naraya KMV, Puska P, et al. Community Interventions for Health (CIH): a novel approach to tackling the worldwide epidemic of chronic diseases. CVD Prevention and Control. 2011;6:47–56. [Google Scholar]
- Eliason M, Storrie D. Job loss is bad for your health – Swedish evidence on cause specific hospitalization following involuntary job loss. Social Science & Medicine. 2009;68:1396–1406. doi: 10.1016/j.socscimed.2009.01.021. [DOI] [PubMed] [Google Scholar]
- Friedland DS, Price RH. Underemployment: consequences for the health and well being of workers. American Journal of Community Psychology. 2003;32:33–45. doi: 10.1023/a:1025638705649. [DOI] [PubMed] [Google Scholar]
- Grayson JP. Reported illness after CGE closure. Canadian Journal of Public Health. 1989;80:16–19. [PubMed] [Google Scholar]
- Hammarström A. Health consequences of youth unemployment. Public Health. 1994;108:403–412. doi: 10.1016/s0033-3506(94)80097-9. [DOI] [PubMed] [Google Scholar]
- Hammarström A, Janlert U. Early unemployment can contribute to adult health problems: results from a longitudinal study of school leavers. Journal of Epidemiology and Community Health. 2002;56:624–630. doi: 10.1136/jech.56.8.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington EF, Crowther JH, Henrickson HCP, Mickelson KD. The relationships among trauma, stress, ethnicity, and binge eating. Cultural Diversity and Ethnic Minority Psychology. 2006;12:212–229. doi: 10.1037/1099-9809.12.2.212. [DOI] [PubMed] [Google Scholar]
- Jusot F, Khlat M, Rochereau T, Sermet C. Job loss from poor health, smoking and obesity: a national prospective survey in France. Journal of Epidemiology and Community Health. 2008;62:332–337. doi: 10.1136/jech.2007.060772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasl SV, Jones BA. Unemployment and health. In: Ayers S, Baum A, McManus C, Newman S, Wallston K, Weinman J, et al., editors. Cambridge handbook of psychology, health and medicine. 2. Cambridge UK: Cambridge University Press; 2007. [Google Scholar]
- Kline R. Principles and practice of structural equation modeling. 3. New York: Guilford Press; 2011. [Google Scholar]
- Lundin A, Lundberg I, Hallsten L, Ottosson J, Hemmingsson T. Unemployment and mortality – a longitudinal prospective study on selection and causation in 49321 Swedish middle aged men. Journal of Epidemiology and Community Health. 2010;64:22–28. doi: 10.1136/jech.2008.079269. [DOI] [PubMed] [Google Scholar]
- Mossakowski KN. Is the duration of poverty and unemployment a risk factor for heavy drinking? Social Science & Medicine. 2008;67:947–955. doi: 10.1016/j.socscimed.2008.05.019. [DOI] [PubMed] [Google Scholar]
- Roelfs DJ, Shor E, Davidson KW, Schwartz JE. Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality. Social Science & Medicine. 2011;72:840–854. doi: 10.1016/j.socscimed.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sargent-Cox K, Butterworth P, Anstey KJ. The global financial crisis and psychological health in a sample of Australian older adults: a longitudinal study. Social Science & Medicine. 2011;73:1105–1112. doi: 10.1016/j.socscimed.2011.06.063. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (HHS) 2008 Physical activity guidelines for Americans. 2008 Available from http://www.health.gov/paguidelines/
- Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instrument for depression: two questions are as good as many. Journal of General Internal Medicine. 1997;12:439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Desai SA, Steckler G, Jackson KM, Bowen S, Leigh BC, et al. Concurrent drinking and smoking among college students: an event-level analysis. Psychology of Addictive Behaviors. 2011 doi: 10.1037/a0025363. http://dx.doi.org/10.1037/a002536, Online First Publication. [DOI] [PMC free article] [PubMed]
- World Health Organization (WHO) Countrywide integrated noncommunicable diseases intervention programme. Copenhagen: WHO Regional Office for Europe; 1995. [Google Scholar]
- World Health Organization (WHO) WHO STEPS surveillance manual. Geneva, Switzerland: 2008. Available from www.who.int/ncd_surveillance/en/stepsinstrumentcore_exp_v1.4.pdf. [Google Scholar]