SUMMARY
With our study we wanted to compare the diagnostic accuracy of conventional radiography (orthopanoramic and intraoral radiography) and Cone Beam CT (CBCT) for the diagnosis of periapical lesions on the posterior elements of the upper maxilla endodontically treated.
The images were analyzed by a radiologist and an endodontist whose interpretation of radiological examinations is unique. Were examined 34 molars (23 first molars and 13 second molars) with a total of 102 roots. The CBCT detected a significantly higher number of lesions (43%, p <0.001) compared to conventional radiography. Our results demonstrate that the CBCT can be inserted into the diagnostic routine for the evaluation of all pre-prosthetic posterior elements of the upper jaw endodontically treated in addition to the diagnostic techniques 2D, especially when in the treatment plan is provided the realization of an abutment. The CBCT, which has reduction of cost and absorption of radiation with respect to the conventional CT, is also very useful even when there is a need to perform a surgical treatment-endodontic (apicectomy) of a lesion diagnosed with 2D techniques.
Keywords: periapical lesions, upper molars, periapical radiographs, cone beam CT
Introduction
A cornerstone of the pre-operative diagnostic protocol in case of a prosthetic tooth previously devitalized is a radiographic assessment of the adequacy of the root canal treatment, particularly to exclude the presence of inflammatory periapical lesions of endodontic origin. The presence of periapical lesions requires, in fact, the reprocessing by orthograde or retrograde (apicectomy surgical), especially in case of the realization of a pin-stump.
In fact, the creation of the post-space for housing the pin can facilitate the penetration of bacteria along the endodontic channel and, where the apical seal was incongruous could allow the building of an inflammatory iatrogenic periapical state, and in the case where it was already a chronic symptomatic periapical lesion, could lead to its transformation into an acute infectious form.
The Rx orthopanoramic (OPT) and intraoral radiography are radiological techniques commonly used to determine the presence of a periapical lesion. Already in the historical study by Bender and Seltzer demonstrate, however, the great limitations of these techniques in the study of such lesions (1), even if the use of 2 or more intraoral radiographs, obtained with a correct projection geometry, can improve the accuracy of diagnosis (2, 3).
The display of periapical lesions therefore is not always possible with conventional radiology since with these techniques an object three-dimensional (3D) is inevitably an image compressed in two-dimensional (2D). The main difficulties are found in the study of the upper molar regions because of possible overlap of the walls of the maxillary sinus and the zygomatic process (4, 5). Furthermore, when displayed, the size of periapical lesions is often underestimated in the 2D images (6).
The utility of CT in endodontics has been validated by many scientific studies (7–9) but the traditional method (spiral CT) is expensive and involves the use of a relatively high dose of radiation. These limitations were overcome by the development of new technologies (CBCT) (10) that significantly reduce the dose of radiation (11).
The aim of our study was therefore to evaluate the diagnostic accuracy of CBCT in the study of peri-apical lesions of the posterior teeth of the maxilla endodontically treated.
Materials and methods
Twenty-six patients (14 male/12 female) with a mean age of 56 years (range between 47 and 72 years) were enrolled in our study. All patients were subjected to a preliminary dental examination in the Department of Dentistry of the Policlinico Tor Vergata University of Rome in the period between February 2011 and January 2012. Patients were selected on the basis of the following criteria: 1) Signs or symptoms of periapical periodontitis in a tooth from the posterior elements of the maxilla; 2) All teeth had previously been treated endodontically and needed a prosthetic rehabilitation; 3) The case was investigated by techniques of conventional radiography (OPT and intraoral radiographs) and CBCT.
Were evaluated 34 teeth and a total of 102 roots. The distribution of the evaluated teeth is shown in Table 1.
Table 1.
Number and location of the teeth.
| Tooth | Number | Right | Left |
|---|---|---|---|
| First molar | 21 | 12 | 9 |
| Second molar | 13 | 6 | 7 |
The images were evaluated by a radiologist with decades of experience in dental radiology and by an endodontist. Were assessed before the OPT and intraoral radiographs and later CBCT images (rebuilt in three planes: axial, coronal, and sagittal) with an interval between the two assessments at least a week. Any disagreement in the interpretation of images was solved by comparing the two professionals.
With conventional radiology the periapical lesion was defined as a radiolucency in connection with the apical part of the root, the width of the radiolucency had to measure at least twice the width of the space of the periodontal ligament.
The same criteria were used for the CBCT where the lesion, however, had to be visible on at least two planes.
We evaluated the periapical lesions by dividing into 2 groups: those viewable with both conventional radiology techniques with both the CBCT (Group 1) or only with the CBCT (Group 2). In 9 cases the presence of the periapical lesion was confirmed by subsequent surgical treatment (apicectomy).
For statistical evaluation we used the Fisher exact Test.
Results
Of the 102 analyzed, 48 roots were free of lesions visualized by the methods used.
Then were displayed 54 lesions, 38 located on the first molars and 16 on the second molars.
31 lesions (57%) have been displayed both with the conventional radiology techniques that with the CBCT. A total of 23 lesions (43%) were instead displayed only through the CBCT (p <0.001) (Tab. 2). The visualization of the lesions was influenced by the apical localization of the same and by the type of tooth analyzed (Tab. 2). Lesions located at the level of the second molar are often visible only through the CBCT (first molar vs. second molar: p = 0.14). Also with regard to the lesions in close proximity to the maxillary sinus their visualization by conventional radiology techniques has often been impossible (Fig. 1).
Table 2.
Viewing periapical lesions according to the methods used.
| Methods | Teeth(%) | Total lesions(%) | |
|---|---|---|---|
| First molar | Second molar | ||
| Group 1 | 24 (63) | 7 (44) | 31 (57) |
| Group 2 | 14 (37) | 9 (56) | 23 (43) |
| Total lesions | 38 | 16 | 54 |
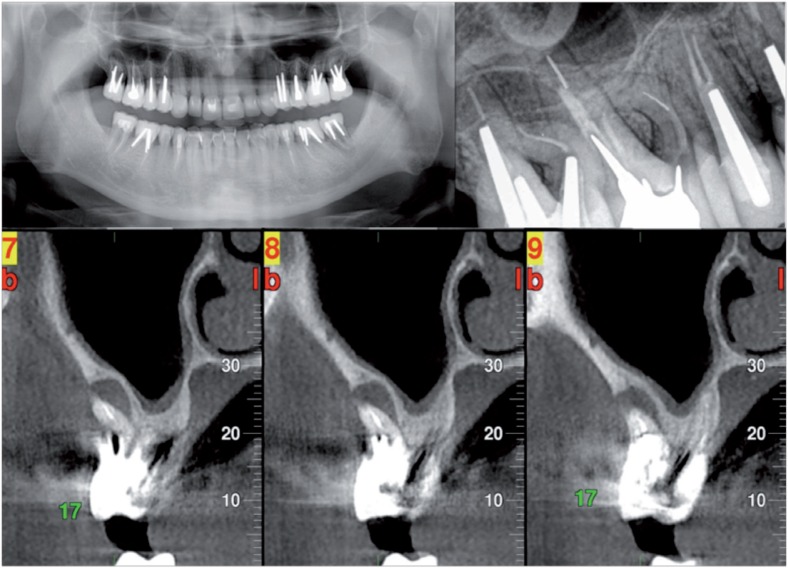
Figure 1.
Rx OPT and intraoral + Reconstructions paraxial CBCT - Periapical lesion in the mesio-buccal root, element 1.7. The overlap of the maxillary sinus floor hinders a correct view of the periapical lesion.
Discussion
The results of our study indicate that the use of CBCT, especially in the study of the posterior elements of the maxilla, is very useful for the proper and safe prosthetic treatment planning. In cases in which are present in the rear quadrants previously endodontically treated teeth, the only use of 2D techniques often is not exhaustive (Fig. 2).
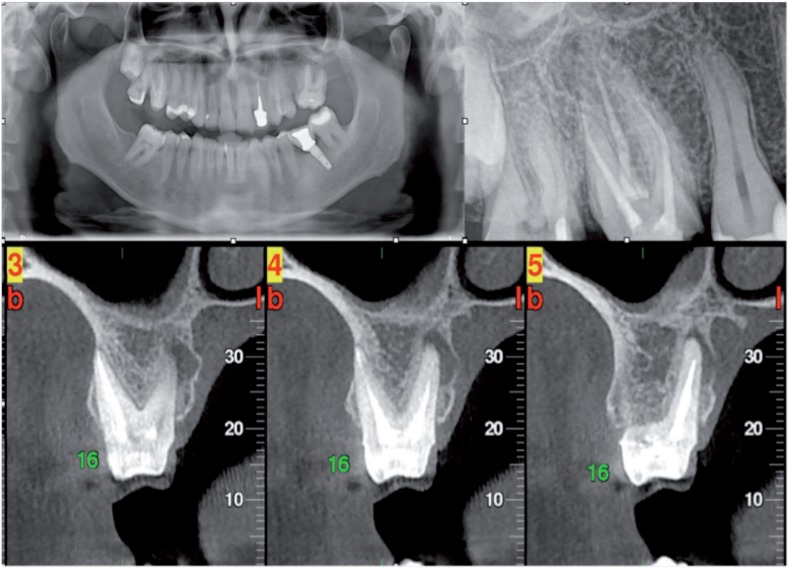
Figure 2.
Rx OPT and intraoral radiography + Reconstructions paraxial CBCT - Periapical lesion in the palatal root, element 1.6. The superimposition of the zygomatic process and the maxillary sinus prevents the proper display of the periapical lesion.
In fact, even using different projection geometries with intraoral radiographs, often can not avoid overlapping structures such as the zygomatic process and especially the maxillary sinus, which may hinder proper display of periapical lesions (12, 13).
Instead, the methods 3D at this level by means of coronal and sagittal slices parallel to the longitudinal axis of the root, and of axial slice perpendicular to them, have a diagnostic accuracy significantly higher. In particular, the CBCT is more appropriate than conventional CT, allowing a reduction of both the dose of radiation absorbed by the patient, both the costs of the examination.
In addition, the exact spatial location and the precise measurement of the size of the lesion allows a correct planning of any surgical solution (apicectomy).
Conclusions
The CBCT can be inserted into the diagnostic routine for the pre-prosthetic evaluation of all posterior elements of the upper jaw endodontically treated (14, 15), in addition to the diagnostic techniques 2D, especially when in the treatment plan is provided for the realization of an pin-stump.
The CBCT, also, it is also very useful when there is a need to perform a surgical treatment-endodontic (apicectomy) of a lesion diagnosed with 2D techniques.
Finally it is important to prefer the use of CBCT compared to conventional CT in relation to the lower dose of radiation absorbed by the patient and to the lower cost of the examination (16).
References
- 1.Bender IB, Seltzer S. Roentgenographic a direct observation of experimental lesions on bone. JADA. 1961 Feb.62:152. [Google Scholar]
- 2.TandlakTidskr S. Roentgenologicperiapical diagnosis. One, two or more roentgenograms? 1970;63:345–50. [Google Scholar]
- 3.Forsberg J, Halse A. Radiographic simulation of a periapical lesion comparing the paralleling and the bisecting-angle techniques. Int Endod J. 1994;27:133–8. doi: 10.1111/j.1365-2591.1994.tb00242.x. [DOI] [PubMed] [Google Scholar]
- 4.Lee S-J, Messer HH. Radiographic appearance of artificially prepared periapical lesions confined to cancellous bone. Int Endod J. 1986;19:64–72. [Google Scholar]
- 5.Wallace JA, Nair MK, Colaco MF, Kapa SF. A comparative evaluation of the diagnostic efficacy of film and digital sensors for detection of simulated periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:93–7. doi: 10.1067/moe.2001.115974. [DOI] [PubMed] [Google Scholar]
- 6.Scarfe WC, Czerniejewski VJ, Farman AG, Avant SL, Molteni R. In vivo accuracy and reliability of color-coded image enhancements for the assessment of periradicular lesion dimensions. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 1999;88:603–11. doi: 10.1016/s1079-2104(99)70093-4. [DOI] [PubMed] [Google Scholar]
- 7.Tachibana H, Matsumoto K. Applicability of x-ray computerized tomography in endodontics. Endod Dent Traumatol. 1990;6:16–20. doi: 10.1111/j.1600-9657.1990.tb00381.x. [DOI] [PubMed] [Google Scholar]
- 8.Marmary Y, Koter T, Heling I. The effect of periapical rarefying osteitis on cortical and cancellous bone. A study comparing conventional radiographs with computed tomography. Dentomaxillofac Radiol. 1999;28:267–271. doi: 10.1038/sj/dmfr/4600453. [DOI] [PubMed] [Google Scholar]
- 9.Velvart P, Hecker H, Tillinger G. Detection of the apical lesion and the mandibular canal in conventional radiography and computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:682–8. doi: 10.1067/moe.2001.118904. [DOI] [PubMed] [Google Scholar]
- 10.Arai Y, Honda K, Iwai K, Shinoda K. Practical model “3DX” of limited cone-beam x-ray CT for dental use. In: Lemke HU, Vannier MW, Inamura K, Farman AG, Doi K, editors. Computer assisted radiology and surgery. Amsterdam: Elsevier; 2001. pp. 713–18. [Google Scholar]
- 11.Lorenzoni DC, Bolognese AM, Garib DG, Guedes FR, Sant’anna EF. Cone-beam computed tomography and radiographs in dentistry: aspects related to radiation dose. Int J Dent. 2012;2012:813768. doi: 10.1155/2012/813768. Epub 2012 Apr 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lofthag-Hansen S, Huumonen S, Gröndahl K, GöranGröndahl H. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Med Oral Pathol Oral Radiol Endod. 2007;103:114–9. doi: 10.1016/j.tripleo.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Phothikhun S, Suphanantachat S, Chuenchompoonut V, Nisapakultorn K. Cone-beam computed tomographic evidence of the association between periodontal bone loss and mucosal thickening of the maxillary sinus. J Periodontol. 2012 May;83(5):557–64. doi: 10.1902/jop.2011.110376. [DOI] [PubMed] [Google Scholar]
- 14.Nakata K, Naitoh M, Izumi M, Inamoto K, Ariji E, Nakamura H. Effectiveness of dental computed tomography in diagnostic imaging of periradicular lesion of each root of a multirooted tooth: a case report. Journal of Endodontics. 2006;32:583–7. doi: 10.1016/j.joen.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Mohan R, Singh A, Mohan Gundappa M. Three-dimensional imaging in periodontal diagnosis – Utilization of cone beam computed tomography. J Indian SocPeriodontol. 2011 Jan-Mar;15(1):11–17. doi: 10.4103/0972-124X.82256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fanucci E, Fiaschetti V, Ottria L, Mataloni M, Acampora V, Lione R, Barlattani A, Simonetti G. Comparison of different dose reduction system in computed tomography for orthodontic applications. ORAL & Implantology. IV(1–2):14–22. [PMC free article] [PubMed] [Google Scholar]