INTRODUCTION
The impact of alcohol, tobacco, and illicit drug use has been identified as an area of concern for many American Indian (AI) individuals and communities (Johnson, et. al. 2010; SAMHSA, 2010a; Young & Joe, 2009; National Highway Traffic Safety Administration, 2009; Tann et.al., 2007; US Department of Health and Human Services Indian Health Service (DHHS-IHS), 2009; Jones-Saumty et. al., 2003; Gray & Nye, 2001; Mail & Johnson, 1993). Recent estimates of substance use rates in the United States indicate that AIs have a higher incidence of tobacco and overall illicit drug use than any other race or ethnic group. Additionally, although rates of alcohol use are lower for AIs than for other groups, those AIs who drink are more likely to drink heavily and more likely to need treatment for alcohol-related problems (CDC, 2011a, 2011b, 2011c; SAMHSA, 2010b).
Because few data exist on alcohol and other drug use in AI communities, NIDA’s National Drug Abuse Treatment Clinical Trials Network (CTN) funded several projects in order to develop collaborative research partnerships with AI communities. The CTN framework consists of thirteen nodes, comprised of university-based Regional Research and Training Centers (RRTCs) linked with Community-based Treatment programs (CTPs). This framework provides the opportunity to perform collaborative research with a variety of CTPs and patient populations throughout the country. The Methamphetamine and Other Drug project (MOD) was an exploratory project that was developed and implemented by five CTN nodes in partnership with AI Tribal and community entities in regions that were associated with a node and in an Indian Health Service (IHS) catchment area. As part of this larger project, the Ohio Valley Node (OVN) partnered with entities serving tribes within the Aberdeen IHS service area, which encompasses tribes located in four Northern Plains states - Iowa, Nebraska, North Dakota, and South Dakota. When assessing regional differences for rates of health disparities, the Aberdeen Area leads all other IHS service areas in disease severity in several areas of health, including age-adjusted rate of alcohol-related death, and deaths caused from tobacco smoking (as of 1999, the mortality rate among AIs in the Aberdeen areas due to tobacco use was twice that of the US population as a whole [Indian Health Service (IHS), 2000]). The Aberdeen Area has a life expectancy of 66.8 years (males 63.0, females 70.6), which is 10.1 years less than the U.S. figure. In addition, the 2000 Census indicated that Aberdeen Area AI females were more than 6 times more likely to be unemployed than females in the U.S. overall, and 44.1% of AI people residing in the Aberdeen Area were below poverty level as compared to 29.2% of all IHS area AI residents and 12.4% of the U.S. population overall (DHHS-IHS, 2008). Anecdotal evidence (Orwa, 2008; South Dakota Dept of Health, 2007) and some preliminary study findings point to problematic use of alcohol, tobacco, and drugs in the region. Several epidemiological studies of AIs living on or near reservations in the north central U.S. have indicated higher rates of cigarette smoking (Holm, et. al., 2010; Nez-Henderson, et. al., 2005; May & Gossage, 2001), alcohol binge episodes (Holm, et. al., 2010; May & Gossage, 2001), and marijuana use (May & Gossage, 2001) than the U.S. averages. Further, Dickerson, et. al., 2009 conducted a secondary analysis of epidemiological data from AI male veterans in the region which revealed higher rates of nicotine dependence, alcohol use disorder, and lifetime drug use disorder than those reported for the U.S. population age 12 and older. Less is known about the characteristics of northern plains AIs who present for treatment for substance-related problems. In a fetal-alcohol prevention project across four northern plains reservation communities, May, et. al. (2008) examined substance use patterns of women at high risk for drinking during pregnancy. Participants in this study, on average, started drinking at age 14, and 24% had binged on alcohol in the previous week. Overall, rates of use for specific substances and characteristics of AI clients in substance abuse treatment in the Aberdeen area are severely lacking, particularly for those receiving treatment in urban facilities.
A community-based participatory research (CBPR; Burhansstipanov, et. al., 2005; Caldwell, et. al., 2005) approach was used to design, develop, and implement the MOD study in the Aberdeen Area. The project was a joint effort of the CTN’s OVN at the University of Cincinnati, the Northern Plains Tribal Epidemiology Center (NPTEC) of the Great Plains Tribal Chairmen’s Health Board (GPTCHB), and the City/County Alcohol and Drug Programs (CCADP) in Rapid City, SD. Ongoing guidance was provided by a Community Advisory Board, which consisted of tribal members involved in substance abuse treatment and/or prevention on three area reservations and by a consultant from the Prairielands Addiction Technology Transfer Center (PATTC), who was also an enrolled member of a Northern Plains tribe. Throughout this process, researchers met with a number of substance abuse treatment providers in both tribal, urban Indian Health, and non-tribal programs, as well as with representatives from state agencies, to discuss areas of concern including substance abuse trends and barriers to treatment for AIs in the Great Plains. Collaborators in this process also participated in two major meetings aimed at exploring research efforts with American Indian communities: 1) representatives from the Community Advisory Board and collaborating researchers presented at a NIDA-sponsored workshop on conducting research with American Indian communities; 2) both the director of NIDA and the director of the NIDA Center for the Clinical Trials Network attended a joint meeting with representatives from the GPTCHB, tribal substance-abuse treatment providers, tribal college health program representatives, urban treatment programs serving AIs, Single State Agency Directors, the Indian Health Service, and the study research team to discuss the current state of substance abuse and other behavioral health concerns among Northern Plains Tribes, and to identify potential areas for intervention and research.
The study aims were endorsed through formal resolution by the Great Plains Tribal Chairmen, followed by development of the protocol through face-to-face meetings and teleconferences between the collaborating researchers and the Community Advisory Board. The protocol aims and procedures were presented to the Aberdeen Area Alcohol Directors Association for feedback, which was incorporated prior to protocol finalization. The result was a two-phase project, in which descriptive data were gathered on AI clients being treated for substance abuse problems in an urban setting (CCADP), followed by a series of focus groups to explore local perceptions of substance use patterns and associated issues in several Aberdeen Area tribal reservation communities. Approval was received from the University of Cincinnati Institutional Review Board – Social and Behavioral Sciences (UC IRB-S). The authors certify responsibility for this manuscript, and there are no known conflicts of interest.
The present paper reports the results from the first phase of the project, which was completed at CCADP over a 9-month period in 2008–2009. CCADP is located in the second-largest urban area of the state and is accredited by the South Dakota Division of Alcohol and Drug Abuse to provide chemical dependency services including substance use assessments, social-setting detoxification, outpatient treatment, residential treatment, family counseling, specialized methamphetamine/opiate day treatment, low-intensity transitional care, and street case management services. Most referrals to CCADP come through the criminal justice system, although many clients are self-referred as well. The majority of their clients are urban-dwelling AIs. In 2008, the total number of clients served was 2,199, of which 1213 were AI (55.2%). In 2009, the total number of clients served was 2,145, of which 1226 were AI (57.2%). These totals represent clients across the entire range of services and may involve multiple admissions. Although CCADP makes provisions for AI clients to access some community cultural resources, the treatment provided at CCADP is not specific to AI cultural or healing practices. The present paper aims to help fill the knowledge gap around AI clients in urban substance abuse treatment programs in the Aberdeen Area and to provide information that could be used to improve treatment outcomes for these clients.
METHODS
Participants for this study were recruited from the population of clients already admitted to treatment services at CCADP who self-identified as AI and were within 2 weeks of entry into services for the current treatment episode. Clients meeting this description were advised of the study using an IRB-approved flyer and, if interested, were referred to the study staff by the CCADP counselors. Seventy-nine clients meeting this description were approached for study participation, 77 of whom expressed willingness to participate. These 77 clients were given a thorough explanation of the study; they signed the study informed consent document that was approved by the University of Cincinnati IRB. The study measure was the Addiction Severity Index-Native American Version (ASI-NAV; Carise & McLellan, 1999), which is a cultural adaptation of the Addiction Severity Index (ASI; McLellan, et. al., 1992). The ASI is widely used in both research and clinical practice and shows good reliability and validity among different populations (McLellan, et. al., 2006). Information regarding the psychometric properties of this adaptation of the ASI, however, is unavailable. The ASI-NAV was developed based on information gained during a pilot process in the Northern Plains, and incorporates culturally-relevant modifications in a number of areas. Specifically, questions relevant to AIs were added to the existing 7 ASI areas, such as tribal affiliation, years of education in AI-specific settings, utilization of traditional healing practices, and the extent to which the client has lived in a reservation setting. An eighth area devoted to the assessment of cultural and spiritual practices was added to the ASI-NAV. In-depth information regarding the development of the ASI-NAV is available in a SAMHSA special report by Carise and McLellan (1999). In the current study, the ASI-NAV was administered by trained interviewers who were members of tribes in the Aberdeen Area.
Information from the ASI-NAV was first analyzed using descriptive statistics for selected variables. Substance abuse information for the past 30 days was not included in the analysis due to the disproportionate number of clients (80.5%) who had been in a controlled environment during part of that time frame (average 14 days). Next, participants were partitioned into three groups according to lifetime substance use patterns: 1) participants who had only ever used alcohol (ETOH-only); 2) participants who had only ever used both alcohol and marijuana (ETOH + MJ); and 3) participants who had used alcohol and at least one drug other than marijuana, although marijuana may have been used as well (ETOH + Other Drug). A number of participant characteristics were then tested for between-group differences. Specifically, differences were analyzed for gender, current living arrangements, history of abuse victimization, psychiatric problems, and engagement in cultural activities. In addition, between-group differences were analyzed for age of first use. A Kruskal-Wallis (KW) procedure was used to analyze those characteristics coded numerically, and categorical characteristics were analyzed using Pearson Chi-Square (P) with a Fisher’s Exact test for analyses with small participant counts. In order to explore possible relationships between the age of first use of any substance and other participant characteristics, we utilized a Wilcoxon (W) procedure, substituting a Student’s T (T) when a Folded F statistic indicated a between-category difference in variance. We also explored the relationships between age of initial multiple substance use and these same other participant characteristics. These relationships were tested the same manner as described above.
RESULTS
Client Characteristics
Eleven different tribes were represented in the study sample. Gender composition of the sample was 62.3% male and 37.7% females. On average, clients were 38 years old (range 18 to 63), living off-reservation (88.3%), and were enrolled members of a Northern Plains Tribe (90.9%). Education and employment patterns for the clients are shown in Table 1. As noted above, a large percentage had been in a controlled environment for part of the past 30 days; most of these had been in other inpatient/residential substance abuse treatment services (69.4%), while the remainder had been in jail or prison (30.6%). One-fourth (25.8%) of those in a controlled environment had been there the entire previous 30 days. About half of the clients (54.5%) had never been married, 11.7% were currently married, and the remainder were either separated/divorced (32.5%) or widowed (1.3%).
Table 1.
Education and Employment for AI Clients in Treatment
| AI Clients in Treatment (n=77) | |
|---|---|
| Education (Years) | 11.9 (1.6) |
| - % Receiving AI-specific education | 67.5% |
| - # years AI-specific education | 8.5 (3.4) |
| Vocational training (months) | 14.2 (11.7) |
| Employment pattern past 3 years: | |
| 1. Full Time | 36.0% |
| 2. Part Time Regular | 18.7% |
| 3. Part Time Irregular | 16.0% |
| 6. Disability / Pension | 6.7% |
| 7. Unemployed | 16.0% |
| 8. Controlled Environment | 6.7% |
| Worked past 30 daysa | 31.2% |
| Total income past 30 days | $312.6 (441.1) |
| -Total income past 30 days - Pts w/income only | $617.2 (442.9) |
Note:
Represents percentage who worked at least one day out of the past 30 days
Substance Use Factors
Table 2 provides information on substance use patterns and treatment history for the participating clients. Alcohol was the primary substance used across their lifetimes, followed by marijuana, amphetamines, and cocaine. Twenty-six of the clients were classified as ETOH-Only, 22 were ETOH + MJ, and 29 were ETOH + Other Drug (23 of which also had lifetime marijuana use). Over half (58. 4%) identified themselves as tobacco smokers. Slightly more than half (50.7%) of participants reported that their current treatment episode was prompted by the criminal justice system. Over half (55.8%) of the participants reported that traditional practices were helpful in achieving and/or maintaining abstinence in the past.
Table 2.
Substance Use and Prior Treatment Episodes for AI Clients in Treatment
| AI Clients in Treatment (N=77) | ||||
|---|---|---|---|---|
| Substance | n | Regular Usea % | Years Used | Age of 1st Use |
| Alcohol - any use | 74 | 96.1% | 15.9 (10.1) | 14.5 (3.4) |
| Alcohol - to Intoxication | 73 | 94.8% | 13.4 (9.8) | 16.8 (5.0) |
| Heroin | 2 | 2.6% | 1.5 (0.7) | 24.5 (10.6) |
| Prescription Opioids | 6 | 7.8% | 5.8 (4.3) | 21.2 (14.0) |
| Sedatives | 4 | 5.2% | 6.5 (6.5) | 23.3 (12.1) |
| Cocaine | 14 | 18.2% | 4.4 (5.2) | 23.9 (8.7) |
| Amphetamines | 14 | 18.2% | 4.1 (3.0) | 20.9 (6.9) |
| Marijuana | 45 | 58.4% | 14.2 (8.4) | 14.7 (4.7) |
| Hallucinogens | 2 | 2.6% | 1.0 (0.0) | 21.0 (0.0) |
| Inhalants | 1 | 1.3% | 2.0 (0.0) | 11.0 (0.0) |
| More than 1 substance per day | 33 | 42.9% | 12.2 (6.8) | 16.4 (6.2) |
| Tobacco (Smoked) | 45 | 58.4% | not assessed | not assessed |
| Prior Treatment (Tx) | n | % | # Episodes | # Detox only |
| Alcohol Tx | 70 | 90.9% | 14.4 (22.4) | 0.7 (2.4) |
| - with AI focus | 43 | 61.4% | ||
| - with AI Tx staff | 45 | 64.3% | ||
| - provided on reservation | 22 | 31.4% | ||
| Drug Tx | 18 | 23.4% | 2.6 (1.0) | 0.0 (0.1) |
| - with AI focus | 7 | 38.9% | ||
| - with AI Tx staff | 10 | 55.6% | ||
| - provided on reservation | 2 | 11.1% |
Note:
Regular Use is defined as ≥3 uses per week, regular binges, or non-regular problematic use; Where not specifically indicated, numbers represent means (standard deviations).
In comparing ETOH-Only clients with ETOH + MJ clients and ETOH + Other Drug clients, significant between-group differences were found for age of 1st use of any substance (KW=10.0; df=2.0; p<.01). These relationships are shown in Figure 1. The average age of first use for ETOH-Only clients was 15.6 years, compared to 13.9 years for ETOH + MJ and 13.0 years for ETOH + Other Drug. A significant between-group difference was also found for lifetime physical abuse victimization (P=7.5; df=2; p<.05), with a trend toward significance for lifetime sexual abuse victimization (P=5.7; df=2; p<.06). On average, ETOH + Other Drug clients were victimized at rates that were nearly double the rate of physical abuse (76.7% vs 42.3%) and more than triple the rate of sexual abuse (40.0% vs 11.5%) experienced by the ETOH-Only clients, with ETOH + MJ falling between those two groups (50.0% physical and 27.3% sexual).
Figure 1.
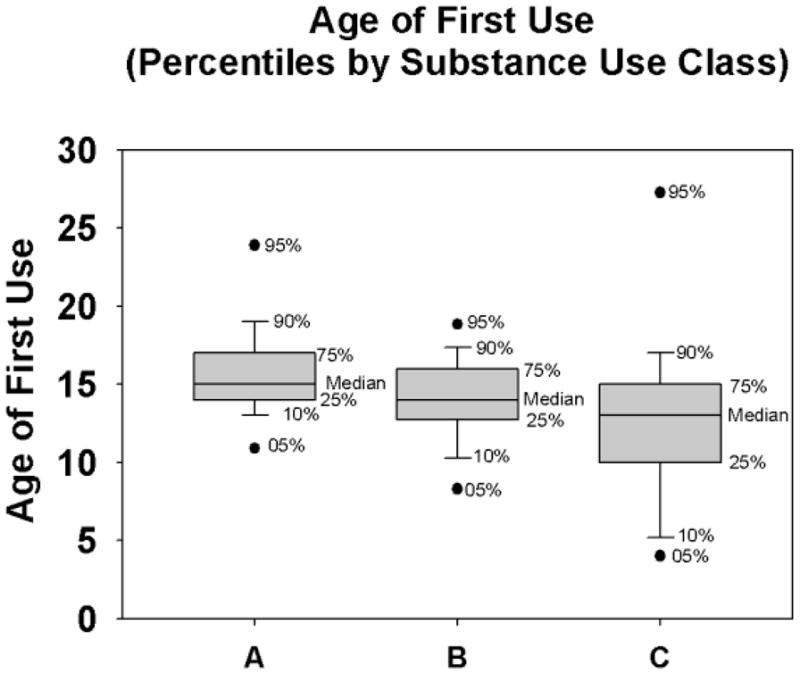
A=ETOH-Only; B=ETOH + MJ; C=ETOH + Other Drug
Psychosocial Factors
Clients reported substantial rates of lifetime abuse and mental health symptoms. Depression and anxiety were the most commonly-reported problems, and about a third (31.6%) of the clients reported having attempted suicide at some time in their lives. Table 3 provides information on the psychosocial factors reported by the participating clients.
Table 3.
Psychosocial Factors for AI Clients in Treatment
| AI Clients in Treatment (N=77) | ||
|---|---|---|
| Living Arrangement past 3 yrs | n | % |
| -Spouse and/or Children | 28 | 36.4% |
| - Family / Friends | 23 | 29.9% |
| - Alone | 15 | 19.5% |
| - Controlled Environment | 8 | 10.4% |
| -No Stable Arrangements | 3 | 3.9% |
| Currently live with someone: | ||
| - with alcohol problem | 14 | 18.2% |
| - with drug problem | 12 | 13.0% |
| - who supports recovery | 47 | 61.8% |
| Lifetime Abuse History | ||
| -Emotional | 46 | 59.7% |
| -Physical | 44 | 57.1% |
| -Sexual | 20 | 26.0% |
| Treatment History - Mental Health/non SUD | ||
| -Hospital | 18 | 23.4% |
| -Outpatient | 25 | 32.5% |
| Emotional/Behavioral Problems (past 30 days/lifetime) | ||
| -Depression 30 | 28 | 36.4% |
| -Depression life | 62 | 80.5% |
| -Anxiety 30 | 36 | 46.8% |
| -Anxiety life | 54 | 70.1% |
| -Hallucinations 30 | 1 | 1.3% |
| -Hallucinations life | 13 | 16.9% |
| -UCRa 30 | 21 | 27.3% |
| -UCRa Life | 38 | 49.4% |
| -Violent behavior 30 | 9 | 11.7% |
| -Violent behavior life | 46 | 59.7% |
| -Suicidal ideation 30 | 4 | 5.2% |
| -Suicidal ideation life | 34 | 44.2% |
| -Suicide Attempt 30 | 1 | 1.3% |
| -Suicide Attempt life | 24 | 31.6% |
Note:
UCR = Problems with understanding, concentrating and remembering
In addition to being correlated with substance use patterns as noted above, a number of psychosocial factors were significantly associated with a younger age of first use. Clients reporting difficulty in understanding, concentrating, and remembering initiated substance use at an average age of 12.7 compared to 15.5 years for clients without such problems (T=3.0; df=67.2; p<.01). On average, clients reporting lifetime sexual abuse victimization initiated substance use at age 12.6, whereas clients without victimization initiated at age 14.7 (T=2.4; df=59.5; p<.05). The age at which clients first used more than one substance on a regular basis was earlier for female clients than for males (14.4 years vs 17.7 years; W=2.7; p<.01), and for clients reporting a history of at least one suicide attempt (13.2 years vs 18.4 years; W=2.2; p<.05).
Cultural Engagement
In assessing cultural practices with the ASI-NAV, 68.8% of the participants indicated regular participation in Native American cultural activities, and 48.1% indicated regular participation in Native American dance activities. Most participants (66.2%) indicated familiarity with their native language, although only a few (9.1%) spoke it as their primary language at home. No correlation was found between cultural engagement and substance use patterns or age of first use.
DISCUSSION
Substance Use
The present sample of AI clients seeking treatment at this urban, non-tribal treatment program indicated that alcohol is the leading substance of abuse, followed by marijuana. While the use of amphetamines, cocaine, and prescription opioids was also reported, alcohol and marijuana by far are used earlier, longer, and by more treatment-seeking clients. This pattern is similar to that reported nationally for AIs in substance abuse treatment(SAMHSA, 2009). The high rate of tobacco smoking reported is in line with results from Nez-Henderson, et. al. (2005), who reported that about half of the AI men and women in the Northern Plains were smokers, and that living off-reservation was associated with higher odds of smoking.
The finding that age of substance use initiation was lower for clients using alcohol plus illicit drugs than for alcohol-only clients helps to inform prevention efforts for AI adolescents in the Aberdeen Area. Based on this finding, it appears that such efforts should start prior to age 13 and should target both alcohol and illicit drug use.
Psychosocial Factors
The clients in this study faced significant challenges in a number of areas, including levels of education lower than those reported for tribes in the Aberdeen Area (DHHS-IHS, 2008), high rates of unemployment, and income that is both below the federal definition of poverty ($10,830 for family of 1; DHHS, 2009) and below the median income reported for AI households in the Aberdeen Area ($23,246; DHHS-IHS, 2009). While the clients’ ability to work and the income received may have been reduced by their time spent in a controlled environment, these findings are in line with information reported by SAMHSA (2010a) that illicit drug use and heavy or binge drinking are correlated with increased unemployment and decreased levels of education. As a result of participating in this study, providers at CCADP were able to identify a number of barriers faced by AI substance users seeking their services. CCADP has responded by instituting intensive case management services to assist AI clients by providing transportation for social service appointments, coordinating more closely with medical and mental health service providers, and directly assisting the client in applying for needed social services. Through its study involvement, the program also recognized the need for greater involvement with the client’s family and with the IHS, despite difficulties faced in such efforts. To increase involvement with the IHS and families, CCADP providers now directly transport clients to IHS appointments and perform home visits with the client and his/her family.
The high rates of abuse victimization reported are consistent with the findings presented by Tjaden & Thoennes (2000) that AI men and women report more violent victimization than do men and women of other racial backgrounds. A few studies have examined mental health disorders in AI populations and have noted the co-morbidity of substance use disorders with other psychiatric disorders (Abbott, 2007; Abbott, 2008) and suicidal behaviors (LeMaster, et. al., 2004). The current findings that substance use onset and patterns are correlated with victimization, cognitive impairment, and suicidal behavior underscore the need to attend to co-morbid psychiatric issues as part of a comprehensive program of recovery from substance abuse. Addressing the issue of mental health for Aberdeen Area AI clients, including substance use, victimization, and suicide, must also take into consideration the impact of disparities in health and resources (Dorgan, 2010; Johnson, 1994) and cultural adeptness (Albright & LaFromboise, 2010; LaFromboise, Albright, & Harris, 2010).
Cultural Engagement
In contrast to the psychosocial challenges they faced, most clients in this study reported receiving support for recovery from both interpersonal and cultural sources. Several authors have suggested cultural identity as a protective factor in preventing or treating substance abuse (Barlow, et. al., 2010; Dickerson & Johnson, 2010; Torres-Stone, et. al., 2006). It was surprising, then, that engagement in cultural practices was not associated with substance use patterns or age of onset. We do not know, however, at what age the clients began these cultural practices nor do we know their level of participation in such activities. Others have suggested that further investigation is needed to determine which groups might benefit most from which cultural elements (Gone, 2004; Hawkins, Cummins, & Marlatt, 2004; Herman-Stahl, Spencer, & Duncan, 2003). Given the lack of correlation between substance use patterns and cultural practices, despite the clients’ subjective experience of the helpfulness of such practices, further exploration is warranted to determine which factors may need to be considered when incorporating cultural elements into Aberdeen Area urban treatment programs.
Limitations
There are several limitations of note in the current study. First, the clients were enrolled in treatment at an urban, non-Native treatment center and may not be representative of AI substance users who would seek treatment in an urban clinic that is based in traditional Native healing practices. Next, because the majority of the clients in this study were not reservation-dwelling, the information gained from them may not represent AI substance users living in reservation communities. In addition, the clients in this study represent a specific geographic area. Findings from the current study should not, therefore, be considered representative of urban-dwelling AI substance use clients in other areas of the U.S. Finally, although the ASI has demonstrated strong psychometric properties, the psychometrics of the ASI-NAV adaptation have not been evaluated. According to its developers, “While there is no evidence that simply adding questions to the instrument would diminish the reliability and validity of the data, comprehensive scientific studies have not been completed comparing the ASI data collected in its original form with ASI data collected when additional questions are added.” (Carise and McLellan, 1999). Despite limitations, the current study assists in filling the current gap in knowledge regarding substance use patterns, associated challenges, and resources for supporting recovery among AI clients accessing urban-based treatment in the Northern Plains.
Acknowledgments
This work was supported by NIDA grant: U10-DA013732 to the University of Cincinnati (Dr. Somoza).
References
- Abbott PJ. Co-Morbid Alcohol/Other Drug Abuse/Dependence and Psychiatric Disorders in Adolescent American Indian and Alaska Natives. Alcoholism Treatment Quarterly. 2007;24(4):3–21. [Google Scholar]
- Abbott PJ. Comorbid alcohol/other drug abuse and psychiatric disorders in adult American Indian and Alaska Natives: A critique. Alcoholism Treatment Quarterly. 2008;26(3):275–293. [Google Scholar]
- Albright K, LaFromboise TD. Hopelessness among White- and Indian-identified American Indian adolescents. Cultural Diversity and Ethnic Minority Psychology. 2010;16(3):437–442. doi: 10.1037/a0019887. [DOI] [PubMed] [Google Scholar]
- Barlow A, Mullany BC, Neault N, Davis Y, Billy T, Hastings R, Coho-Mescal V, Lake K, Powers J, Clouse E, Reid R, Walkup JT. Examining correlates of methamphetamine and other drug use in pregnant American Indian adolescents. American Indian and Alaska Native Mental Health Research: The Journal of the National Center. 2010;17(1):1–24. doi: 10.5820/aian.1701.2010.1. [DOI] [PubMed] [Google Scholar]
- Burhansstipanov L, Christopher S, Schumacher A., Sr Lessons learned from community-based participatory research in Indian Country. Cancer Control. 2005;12(Supplement 2):70–76. doi: 10.1177/1073274805012004s10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell JY, Davis JD, Du Bois B, Echo-Hawk H, Shephard Erickson J, Turner Goins R, Hill C, Hillabrant W, Johnson SR, Kendall E, Keemer K, Manson SM, Marshall CA, Running Wolf P, Santiago RL, Schacht R, Stone JB. Culturally Competent Research with American Indians and Alaska Natives: Findings and Recommendations of the First Symposium of the Work Group on American Indian Research and Program Evaluation Methodology. American Indian and Alaska Native Mental Health Research: The Journal of the National Center. 2005;12(1):1–21. doi: 10.5820/aian.1201.2005.1. [DOI] [PubMed] [Google Scholar]
- Carise D, McLellan AT. Increasing Cultural Sensitivity of the Addiction Severity Index (ASI): An Example with Native Americans in North Dakota. Substance Abuse and Mental Health Services Administration (SAMHSA), Center for Substance Abuse Treatment; 1999. [Google Scholar]
- Centers for Disease Control Prevention CDC. Drug-Induced Deaths - United States 2003 – 2007. MMWR 2011. 2011a;60(Suppl):60–61. [Google Scholar]
- Centers for Disease Control Prevention CDC. Binge Drinking - United States, 2009. MMWR 2011. 2011b;60(Suppl):101–104. [PubMed] [Google Scholar]
- Centers for Disease Control Prevention CDC. Cigarette Smoking - United States, 1965 – 2008. MMWR 2011. 2011c;60(Suppl):109–113. [PubMed] [Google Scholar]
- Dickerson DL, Johnson CL. Mental health and substance abuse characteristics among a clinical sample of urban American Indian Alaska Native youths in a large California metropolitan area: a descriptive study. [Accessed February 3, 2011];Community Mental Health Journal. 2010 doi: 10.1007/s10597-010-9368-3. Published online: December 16, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, O’Malley SS, Canive J, Thuras P, Westermeyer J. Nicotine dependence and psychiatric and substance use comorbidities in a sample of American Indian male veterans. Drug and Alcohol Dependence. 2009;99(1–3):169–175. doi: 10.1016/j.drugalcdep.2008.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorgan Senator BL. The tragedy of Native American youth suicide. Psychological Services. 2010;7(3):213–218. [Google Scholar]
- Gone JP. Mental health services for Native Americans in the 21st century United States. Professional Psychology: Research and Practice. 2004;35(1):10–18. [Google Scholar]
- Gray N, Nye PS. American Indian and Alaska Native substance abuse: Co-morbidity and cultural issues. American Indian and Alaska Native Mental Health Research: The Journal of the National Center. 2001;10(2):67–84. doi: 10.5820/aian.1002.2001.67. [DOI] [PubMed] [Google Scholar]
- Hawkins EH, Cummins LH, Marlatt GA. Preventing substance abuse in American Indian and Alaska Native Youth: Promising strategies for healthier communities. Psychological Bulletin. 2004;130(2):304–323. doi: 10.1037/0033-2909.130.2.304. [DOI] [PubMed] [Google Scholar]
- Herman-Stahl M, Spencer DL, Duncan JE. The implications of cultural orientation for substance use among American Indians. American Indian and Alaska Native Mental Health Research: The Journal of the National Center. 2003;11(1):46–66. doi: 10.5820/aian.1101.2003.46. [DOI] [PubMed] [Google Scholar]
- Holm JE, Vogeltanz-Holm N, Poltavski D, McDonald L. Assessing Health Status, Behavioral Risks, and Health Disparities in American Indians Living on the Northern Plains of the U.S. Public Health Reports. 2010;125:68–78. doi: 10.1177/003335491012500110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indian Health Service. Regional differences in Indian Health 1998–99. Rockville, MD: IHS; 2000. [Accessed March 16, 2009]. Available at http://www.ihs.gov/Publicinfo/Publications/trends98/region98.asp. [Google Scholar]
- Johnson D. Stress, depression, substance abuse, and racism. American Indian and Alaska Native Mental Health Research: The Journal of the National Center. 1994;6(1):29–33. doi: 10.5820/aian.0601.1994.29. [DOI] [PubMed] [Google Scholar]
- Johnson CV, Bartgis J, Worley JA, Hellman CM, Burkhart R. Urban Indian voices: A community-based participatory research health and needs assessment. American Indian and Alaska Native Mental Health Research: The Journal of the National Center. 2010;17(1):49–70. doi: 10.5820/aian.1701.2010.49. [DOI] [PubMed] [Google Scholar]
- Jones-Saumty D, Thomas B, Phillips ME, Tivis R, Nixon SJ. Alcohol and health disparities in nonreservation American Indian communities. Alcoholism: Clinical and Experimental Research. 2003;27(8):1333–1336. doi: 10.1097/01.ALC.0000080343.90121.25. [DOI] [PubMed] [Google Scholar]
- LaFromboise TD, Albright K, Harris A. Patterns of hopelessness among American Indian adolescents: Relationships by levels of acculturation and residence. Cultural Diversity and Ethnic Minority Psychology. 2010;16(1):68–76. doi: 10.1037/a0016181. [DOI] [PubMed] [Google Scholar]
- LeMaster PL, Beals J, Novins DK, Manson SM the AI-SUPERPFP Team. The prevalence of suicidal behaviors among Northern Plains American Indians. Suicide and Life-Threatening Behavior. 2004;34(3):242–254. doi: 10.1521/suli.34.3.242.42780. [DOI] [PubMed] [Google Scholar]
- Mail PD, Johnson S. Boozing, sniffing, and toking: An overview of the past, present, and future of substance use by American Indians. American Indian and Alaska Native Mental Health Research: The Journal of the National Center. 1993;5(2):1–33. doi: 10.5820/aian.0502.1993.1. [DOI] [PubMed] [Google Scholar]
- May PA, Miller JH, Goodhart KA, Maestas OR, Buckley D, Trujillo PM, Gossage JP. Enhanced case management to prevent fetal alcohol spectrum disorders in Northern Plains communities. Maternal and Child Health Journal. 2008;12:747–759. doi: 10.1007/s10995-007-0304-2. [DOI] [PubMed] [Google Scholar]
- May PA, Gossage JP. New data on the epidemiology of adult drinking and substance use among American Indians of the northern states: Male and female data on prevalence, patterns, and consequences. American Indian and Alaska Native Mental Health Research: The Journal of the National Center. 2001;10(2):1–26. doi: 10.5820/aian.1002.2001.1. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Grissom G, Pettinati H, Argerious M. The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Cacciola JS, Alterman AI, Rikoon SH, Carise D. The Addiction Severity Index at 25: origins, contributions and transitions. American Journal of Addiction. 2006;15(2):113–24. doi: 10.1080/10550490500528316. [DOI] [PubMed] [Google Scholar]
- National Highway Traffic Safety Administration. Traffic Safety Facts 2006 Data Race and Ethnicity. NHTSA National Center for Statistics and Analysis, DOT HS 810 995; Washington, D.C: 2009. [Google Scholar]
- Nez-Henderson PN, Jacobsen C, Beals J the AI-SUPERPFP Team. Correlates of Cigarette Smoking Among Selected Southwest and Northern Plains Tribal Groups: The AI-SUPERPFP Study. American Journal of Public Health. 2005;95:867–872. doi: 10.2105/AJPH.2004.050096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orwa MA. AATCHB-NPTEC Alcohol and Drug Abuse Treatment Services Assessment Survey Results. Presentation to the Aberdeen Area Alcohol Directors Association; December 18, 2008; Rapid City, SD. 2008. [Google Scholar]
- South Dakota Department of Health. American Indian Health Status. Zaniya Project report. 2007 May 10;2007 [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Summary of National Findings. I. Office of Applied Studies; Rockville, MD: 2010a. Results from the 2009 National Survey on Drug Use and Health. NSDUH Series H-38A, HHS Publication No. SMA 10-4586 Findings. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2009 National Survey on Drug Use and Health: Detailed Tables. Office of Applied Studies; Rockville, MD: 2010b. [accessed February 2, 2011]. http://oas.samhsa.gov/WebOnly.htm#NSDUHtabs. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies. OAS Series #S-45, HHS Publication No. (SMA) 09-4360. Rockville, MD: 2009. Treatment Episode Data Set (TEDS) Highlights - - 2007 National Admissions to Substance Abuse Treatment Services. [Google Scholar]
- Tann S, Yabiku ST, Okamoto SK, Yanow J. TRIADD: The risk for alcohol abuse, depression, and diabetes multimorbidity in the American Indian and Alaska Native population. American Indian and Alaska Native Mental Health Research. 2007;14(1):1–23. doi: 10.5820/aian.1401.2007.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. Publication NCJ 183781. Rockville, MD: National Institute of Justice; 2000. Full Report of the Prevalence, Incidence, and Consequences of Violence Against Women. [Google Scholar]
- Torres-Stone RA, Whitbeck LB, Chen X, Johnson K, Olson DM. Traditional practices, traditional spirituality, and alcohol cessation among American Indians. Journal of Studies on Alcohol. 2006;67:236–244. doi: 10.15288/jsa.2006.67.236. [DOI] [PubMed] [Google Scholar]
- US Department of Health, Human Services DHHS. Annual Update of the HHS Poverty Guidelines. Federal Register. 2009;74(14):4199–4201. [Google Scholar]
- US Department of Health and Human Services. Indian Health Service. (DHHS-IHS; 2009)Trends in Indian Health, 2002–2003 Edition. Washington: Government Printing Office; Released October 2009. [Google Scholar]
- US Department of Health and Human Services. Indian Health Service. (DHHS-IHS; 2008) Regional Differences in Indian Health 2002–2003 Edition. Washington: Government Printing Office; Released March 2008. [Google Scholar]
- Young RS, Joe JR. ‘Some Thoughts About the Epidemiology of Alcohol and Drug Use Among American Indian/Alaska Native Populations. Journal of Ethnicity in Substance Abuse. 2009;8(3):223–241. doi: 10.1080/15332640903110443. [DOI] [PubMed] [Google Scholar]


