Abstract
PURPOSE
The chronic illness model advocates for psychoeducation within a collaborative care model to enhance outcomes. To inform psychoeducational approaches for attention-deficit/hyperactivity disorder (ADHD), this study describes parent and adolescent knowledge, perceptions and information sources and explores how these vary by sociodemographic characteristics, ADHD risk, and past child mental health service use.
METHODS
Parents and adolescents were assessed 7.7 years after initial school district screening for ADHD risk. The study sample included 374 adolescents (56% high and 44% low ADHD risk), on average 15.4 (SD 1.8) years old, and 36% were African American. Survey questions assessed ADHD knowledge, perceptions, and cues to action, and elicited utilized and preferred information sources. Multiple logistic regression was used to determine potential independent predictors of ADHD knowledge. McNemar's tests compared information source utilization against preference.
RESULTS
Despite relatively high self-rated ADHD familiarity, misperceptions among parents and adolescents were common, including a sugar etiology (25% and 27%, respectively) and medication overuse (85% and 67%). African American respondents expressed lower ADHD awareness and greater belief in sugar etiology than Caucasians. Parents used a wide range of ADHD information sources while adolescents relied on social network members and teachers/school. However, parents and adolescents expressed similar strong preferences for the Internet (49% and 51%) and doctor (40% and 27%) as ADHD information sources.
CONCLUSION
Culturally appropriate psychoeducational strategies are needed that combine doctor-provided ADHD information with reputable Internet sources. Despite time limitations during patient visits, both parents and teens place high priority on receiving information from their doctor.
Keywords: ADHD, adolescence, knowledge, information sources, cultural variation
INTRODUCTION
An estimated two-thirds of children with attention-deficit/hyperactivity disorder (ADHD) remain symptomatic in adolescence and young adulthood [1], placing them at increased risk for adverse outcomes, such as lowered academic and vocational achievements, substance abuse, and involvement with the justice system [2]. In addition, their risk may be accentuated by poor adherence to recommended care because older youth are more likely to discontinue ADHD treatment than their school-age counterparts [3, 4]. Earlier studies suggest that discontinuation of treatment may be related to adolescents' increasing self-determination of health behavior as well as their negative attitudes towards mental health treatment and stigma [4, 5].
Increased adolescent-focused ADHD psychoeducation in the context of a collaborative care paradigm might have the potential to prevent premature treatment discontinuation for this chronic disorder. However, little is known about adolescent knowledge of ADHD, or about culturally sensitive psychoeducation or self-management education [6] for ADHD, despite the fact that such education is considered essential in a chronic illness model [7]. Educational interventions for ADHD are best framed in the context of existing health education models. According to the health belief model (HBM) [8, 9] whether or not treatment is sought depends on knowledge and awareness of a health condition and its treatments, as well as receiving cues to action. The HBM assesses patient perceptions that can be targets of psychoeducational interventions, including perceptions of disorder seriousness, susceptibility, and benefits of interventions [9]. Most studies of ADHD health beliefs indicate significant needs for remedial educational interventions. For example, less than one-half of respondents in a nationally representative adult study could correctly identify ADHD symptoms from a vignette and ADHD symptoms were rated as less serious than depression symptoms [10]. Adult studies also identified misperceptions about etiology [11]), revealed beliefs about overtreatment [12], and documented stigma perceptions surrounding the disorder [10]. In addition, there appears to be significant racial/ethnic variation in adults' ADHD knowledge and explanatory models [13], such that Caucasian parents express greater familiarity with ADHD than parents from minority backgrounds [10, 14]. The first large-scale study of youth beliefs about ADHD causes [15] found that stigmatizing attributional beliefs, such as low effort, inadequate parenting or substance abuse causing ADHD were common. However, this study did not assess general youth ADHD knowledge or perceptions or examine how attitudes about ADHD vary by well established factors that influence seeking care, such as clinical severity and prior mental health service use.
Further, although existing research suggests significant unmet need for ADHD health information among parents and youth [10–12], little is known about their usual information sources and their information gathering preferences. Previous studies reported that parents rate pediatrician-provided information as useful and trustworthy than Internet sources [16]. Internet-based health information merits specific consideration due to general trends towards the Internet as a health information source [17] and increasing Internet use by youth.
Thus, more data on the extent of adolescents' and their parents' ADHD knowledge and perceptions is required to identify target areas for educational and self-management interventions for this group at heightened risk of treatment discontinuation. Guided by the HBM, the objectives of this study are to: 1) describe adolescent and parent ADHD knowledge, perceptions and cues to action and test whether they vary by sociodemographic characteristics, ADHD risk status and lifetime mental health service use; 2) determine adolescent- and parent-reported use of and preference for ADHD information sources and examine variation by ADHD risk status; and 3) among youth at high risk for ADHD, compare utilized and preferred health information sources by adolescents and parents to identify potential gaps that may be addressed by psychoeducation interventions. .
METHODS
Participants and procedures
This research used data from a longitudinal cohort study with six study waves between 1998 and 2008 that assessed detection and access to care for ADHD in a representative school district sample [18]. Data for this report were derived from 374 interviews conducted on average 7.7 years (SD 1.2) after the initial screening in 1998.
To identify students who were at high risk for ADHD, a random sample of children, oversampling girls by a factor of two, was obtained from public school records of 12,009 children (from kindergarten to the fifth grade) from a North Florida school district. Of 1,615 children screened in wave 1, 29.5% (n=476) were deemed at “high risk for ADHD” on enrollment either because they: 1) were diagnosed or treated for ADHD; 2) were considered by parent or teachers to have ADHD; or 3) elicited behavioral concerns and had parent-reported scores of >= 1.5 SD above the normal value on the Swanson-Nolan-and Pelham-IV (SNAP-IV) [19]. The 476 students deemed at high risk were eligible for to up to six subsequent study waves between 1998 and 2008. The remaining 1,139 students were deemed at low risk for ADHD and a subsample, matched to the high risk cohort on age, gender, race and poverty status, was selected for the last study wave to serve as the comparison group. The current research included data from 374 adolescents, 56% (n=209; 79% participation rate) from the high risk and 44% (n=165; 69% participation rate) from the low risk group.. Of the sample, 57% were female (n=213), 36% (n=136) were from African American backgrounds, and 53% (n=197) qualified for free or reduced lunch status. Their average age was 15.4 years (SD 1.8). Over one-half (56%, n=210) had received mental health services in the past.
The study was approved by the University of Florida Institutional Review Board and the school district research office. Informed consent (parents and young adults) and child assent (adolescents) were obtained from all subjects, who received a stipend of $40 (parents) or $30 (adolescents) for their participation. Trained research assistants conducted personal interviews with parents and adolescents in homes, community locations, or at our research center.
Measurement
Predictors
We tested five predictor variables of adolescent and parental ADHD knowledge and health beliefs, based on extant literature, including gender, race, poverty as assessed by school lunch status, ADHD risk status (contrasting high risk and low risk group), and lifetime mental health service use. Demographic information was originally obtained from school registration records and verified during study interviews.
Mental Health Services Use
Receipt of mental health treatment services was assessed using the Child and Adolescent Services Assessment (CASA) [20], a parent-reported measure of mental health service use, with good to excellent agreement between CASA parent reports and medical records for receiving outpatient services [21]. Adolescents were identified as ever having received mental health treatment if their parent reported any lifetime inpatient or outpatient mental health care.
Outcomes
ADHD knowledge, perceptions and cues to action
We used seven survey questions designed to indicate general ADHD familiarity and related health beliefs among general populations [22]. Two questions addressed disease knowledge, namely, whether the respondent has ever heard about “attention deficit disorder, hyperactivity, ADD, or ADHD” (yes; no); and the extent of self-rated knowledge (nothing; little; some; a lot). Two statements addressed perceptions of etiology and overtreatment, namely “attention deficit or hyperactivity is caused by too much sugar in the diet” and “too many children are being given medicines by doctors for attention deficit or hyperactivity” (definitely true; probably true; probably false; definitely false; don't know). Personal experience with ADHD as a potential cue to action was assessed with the questions whether or not the respondent knows a person with ADHD (yes; no). Two questions ascertained the respondent's utilized and preferred ADHD information sources (“where do you get most of your information about attention deficit or hyperactivity” and “if you wanted more information about attention deficit or hyperactivity where would you prefer to get it”). Respondents could list multiple sources. Responses were elicited verbatim and subsequently grouped into four information source categories: “any health professional” (doctor, mental health professional, hospital clinics or public health departments), “any written” (library, medical journals, newspaper or brochures), “any social network” relatives or friends), and “any other” (teacher/school, television or Internet; other).
Statistical analyses
Bivariate analyses assessing the relationship between our five predictors and the knowledge outcomes were performed using the chi-square test of proportions. Comparisons of adolescent and parent total number of information sources was conducted using paired t tests. To simultaneously examine the relationship of our five predictors with outcomes we derived odds ratios through a series of multiple logistic regressions. Tables 1 and 2 provide the results of the bivariate analyses as well as the odds ratios for each potential predictor variable for adolescents and parents, respectively. Tables 3 and 4 document bivariate analyses of utilized and preferred ADHD information sources, respectively, stratified by ADHD risk status. McNemar's tests were conducted to compare the extent to which adolescents and parents from the high risk group reported utilization of ADHD information sources to their expressed preference for these sources, with Figures 1 and 2 depicting the percentage of utilized and preferred ADHD information source categories. All analyses were performed using the UNIVARIATE, MEANS, FREQ and LOGISTIC procedures in SAS software (version 9.2, Cary, NC). For all analyses, p-values less than a level of significance value of 0.05 were considered statistically significant.
Table 1.
Variations in adolescent ADHD knowledge, perceptions and cues to action by ADHD risk status and sociodemographic characteristics
| Ever heard of ADHD | Knows some or lot about ADHD | ADHD caused bv sugar | Too many treated with medications | Knows someone with ADHD | |
|---|---|---|---|---|---|
| Number (%) | Number (%) | Number (%) | Number (%) | Number (%) | |
| ADHD Risk status [X2] | [1.93] | [2.36] | [6.10] * | [0.01] | [4.33] * |
| ADHD/Risk | 177 (91.2%) | 102 (52.6%) | 62 (32.0%) | 130 (67.0%) | 146 (75.3%) |
| Low Risk Match | 153 (95.0%) | 71 (44.4%) | 32 (20.3%) | 105 (66.5%) | 134 (84.3%) |
| AOR (95% CI) | 0.4 (0.1–1.1) | 1.6 (1.0–2.8) | 2.0 (1.1–3.8) | 0.9 (0.5–1.6) | 0.3 (0.2–0.7) |
| Gender [X2] | [0.15] | [0.49] | [0.05] | [0.17] | [0.24] |
| Male | 145 (93.6%) | 79 (51.0%) | 42 (27.3%) | 101 (65.6%) | 124 (80.5%) |
| Female | 185 (92.5%) | 94 (47.2%) | 52 (26.3%) | 134 (67.7%) | 156 (78.4%) |
| AOR (95% CI) | 1.0 (0.4–2.5) | 1.1 (0.7–1.7) | 1.2 (0.7–2.0) | 0.9 (0.6–1.4) | 1.0 (0.6–1.8) |
| Race [X2] | [26.41] *** | [22.75] *** | [23.65] *** | [2.09] | [53.60] *** |
| Caucasian | 222 (98.2%) | 132 (58.4%) | 41 (18.1%) | 157 (69.5%) | 206 (91.2%) |
| African American | 108 (83.7%) | 41 (32.0%) | 53 (42.1%) | 78 (61.9%) | 74 (58.3%) |
| AOR (95% CI) | 6.4 (1.8–22.0) | 2.8 (1.6–4.8) | 0.5 (0.3–0.9) | 1.3 (0.8–2.3) | 5.7 (2.8–11.5) |
| Poverty [X2] | [14.09] ** | [8.78] ** | [24.18] *** | [0.63] | [22.80] *** |
| Non-Poor | 168 (98.3%) | 97 (57.1%) | 25 (14.7%) | 117 (68.8%) | 153 (90.0%) |
| Poor | 162 (88.0%) | 76 (41.3%) | 69 (37.9%) | 118 (64.8%) | 127 (69.4%) |
| AOR (95% CI) | 2.4 (0.6–9.8) | 1.2 (0.7–2.0) | 0.4 (0.2–0.8) | 1.0 (0.6–1.8) | 1.4 (0.7–2.9) |
| Past MH Treatment [X2] | [1.51] | [1.26] | [0.05] | [0.76] | [4.43] * |
| Yes | 187 (94.4%) | 102 (51.5%) | 52 (26.3%) | 136 (68.7%) | 165 (83.3%) |
| No | 143 (91.1%) | 71 (45.5%) | 42 (27.3%) | 99 (64.3%) | 115 (74.2%) |
| AOR (95% CI) | 2.0 (0.7–5.5) | 0.8 (0.5–1.4) | 0.7 (0.4–1.4) | 1.2 (0.7–2.1) | 2.6 (1.3–5.3) |
Note: ADHD = attention deficit/hyperativity disorder; AOR = Adjusted odds ratio based on multiple logistic regression, using ADHD risk group, gender, race, poverty and MH Treatment as predictors; MH = Mental Health; bolded entries indicate statistically significant findings;
p <.05;
p <.01;
p <.001
Table 2.
Variations in parent ADHD knowledge, perceptions and cues to action by adolescent's ADHD risk status and sociodemographic characteristics
| Ever heard of ADHD | Knows some or lot about ADHD | ADHD caused by sugar | Too many treated with medications | Knows someone with ADHD | |
|---|---|---|---|---|---|
| Number (%) | Number (%) | Number (%) | Number (%) | Number (%) | |
| Adolescent Risk status [X2] | [0.15] | [0.01] | [6.56] * | [2.21] | [4.58] * |
| ADHD/Risk | 204 (97.6%) | 163 (78.0%) | 62 (29.7%) | 171 (82.2%) | 193 (92.3%) |
| Low Risk Match | 162 (98.2%) | 128 (77.6%) | 30 (18.2%) | 144 (87.8%) | 141 (85.5%) |
| AOR (95% CI) | 0.3 (0.1–1.4) | 0.7 (0.3–1.3) | 2.4 (1.3–4.5) | 1.0 (0.5–2.0) | 1.2 (0.5–2.7) |
| Gender [X2] | [0.16] | [0.33] | [1.85] | [0.19] | [0.56] |
| Male | 157 (97.5%) | 123 (76.4%) | 34 (21.1%) | 137 (85.6%) | 146 (90.7%) |
| Female | 209 (98.1%) | 168 (78.9%) | 58 (27.2%) | 178 (84.0%) | 188 (88.3%) |
| AOR (95% CI) | 0.6 (0.2–2.6) | 0.7 (0.4–1.2) | 0.8 (0.5–1.3) | 1.2 (0.7–2.1) | 1.0 (0.5–6.1) |
| Race [X2] | [14.31] *** | [51.78] *** | [23.80] *** | [0.98] | [15.87] *** |
| Caucasian | 238 (100%) | 213 (89.5%) | 39 (16.4%) | 204 (86.1%) | 224 (94.1%) |
| African American | 128 (94.1%) | 78 (57.4%) | 53 (39.0%) | 111 (82.2%) | 110 (80.9%) |
| AOR (95% CI) | N/A | 5.4 (2.8–10.4) | 0.5 (0.3–0.9) | 0.3 (0.7–2.1) | 2.6 (1.1–6.1) |
| Poverty [X2] | [7.34] ** | [16.46] *** | [26.83] *** | [1.31] | [7.06] ** |
| Non-Poor | 177 (100%) | 154 (87.0%) | 22 (12.4%) | 153 (86.9%) | 166 (93.8%) |
| Poor | 189 (95.9%) | 137 (69.5%) | 70 (35.5%) | 162 (82.7%) | 168 (85.3%) |
| AOR (95% CI) | N/A | 1.1 (0.6–2.3) | 0.4 (0.2–0.8) | 1.2 (0.6–2.4) | 1.5 (0.6–3.8) |
| Ever MH Treatment [X2] | [3.22] | [11.64] *** | [0.78] | [5.35] * | [17.65] *** |
| Yes | 208 (99.1%) | 177 (84.3%) | 48 (22.9%) | 169 (80.9%) | 200 (95.2%) |
| No | 158 (96.3%) | 114 (69.5%) | 44 (26.8%) | 146 (89.6%) | 134 (81.7%) |
| AOR (95% CI) | 7.5 (1.3–43.7) | 2.6 (1.3–5.0) | 0.6 (0.3–1.1) | 0.5 (0.2–0.96) | 3.6 (1.5–8.6) |
Note: ADHD = attention deficit/hyperativity disorder; AOR = Adjusted odds ratio based on multiple logistic regression, using ADHD risk group, gender, race, poverty and MH Treatment as predictors; MH = Mental Health; N/A = not applicable – race and poverty were not included in logistic regression modeling; bolded entries indicate statistically significant findings;
p <.05;
p <.01;
p <.001
Table 3.
ADHD information source utilization for adolescents and parents, by adolescent's ADHD risk status
| Source type | Adolescents | Parents | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ADHD/Risk | Low Risk Match | ADHD/Risk | Low Risk Match | |||||||
| Number | % | Number | % | X 2 | Number | % | Number | % | X 2 | |
| Health Professional | ||||||||||
| Doctor | 20 | 10.3% | 4 | 2.5% | [8.55] ** | 59 | 28.2% | 28 | 17.0% | [6.55] * |
| MH Professional | 3 | 1.6% | 2 | 1.2% | [0.06] | 27 | 12.9% | 13 | 7.9% | [2.45] |
| Hospital/clinic | 2 | 1.0% | 2 | 1.2% | [0.04] | 7 | 3.4% | 1 | 0.6% | [3.31] |
| Public Health Dpt. | 1 | 0.5% | 0 | 0% | [0.83] | 2 | 1.0% | 2 | 1.2% | [0.06] |
| Social Network | ||||||||||
| Relatives | 48 | 24.7% | 24 | 14.9% | [5.26] * | 15 | 7.2% | 20 | 12.1% | [2.66] |
| Friends | 31 | 16.0% | 48 | 29.8% | [9.73] ** | 30 | 14.4% | 37 | 22.4% | [4.08] * |
| Written | ||||||||||
| Library | 6 | 3.1% | 3 | 1.9% | [0.54] | 17 | 8.1% | 5 | 3.0% | [4.34] * |
| Medical Journal | 2 | 1.0% | 2 | 1.2% | [0.04] | 20 | 9.6% | 15 | 9.1% | [0.02] |
| Newspaper/Magazine | 13 | 6.7% | 16 | 9.9% | [1.23] | 51 | 24.4% | 43 | 26.1% | [0.13] |
| Brochure | 2 | 1.0% | 2 | 1.2% | [0.04] | 28 | 13.9% | 7 | 4.2% | [9.84] ** |
| Other | ||||||||||
| Teacher/School | 41 | 21.1% | 52 | 32.3% | [5.67] * | 17 | 8.1% | 30 | 18.2% | [8.47] ** |
| Internet | 19 | 9.8% | 14 | 8.7% | [0.13] | 72 | 34.5% | 36 | 21.8% | [7.16] ** |
| TV | 21 | 10.8% | 29 | 18.0% | [3.76] | 38 | 18.2% | 41 | 24.9% | [2.46] |
Note: ADHD = attention deficit/hyperativity disorder; bolded entries indicate statistically significant findings;
p <.05;
p <.01;
p <.001
Table 4.
ADHD information source preferences for adolescents and parents, by adolescent's ADHD risk status
| Source type | Adolescents | Parents | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ADHD/Risk | Low Risk Match | ADHD/Risk | Low Risk Match | |||||||
| Number | % | Number | % | X 2 | Number | % | Number | % | X 2 | |
| Health Professional | ||||||||||
| Doctor | 52 | 26.8% | 31 | 19.3% | [2.80] | 83 | 39.7% | 53 | 32.1% | [2.30] |
| MH Professional | 7 | 3.6% | 4 | 2.5% | [0.37] | 28 | 13.4% | 13 | 7.9% | [2.88] |
| Hospital/clinic | 1 | 0.5% | 2 | 1.2% | [0.55] | 10 | 4.8% | 1 | 0.6% | [5.64] * |
| Public Health Dpt. | 2 | 1.0% | 0 | 0.0% | [1.67] | 2 | 1.0% | 0 | 0.0% | [1.59] |
| Social Network | ||||||||||
| Relatives | 14 | 7.2% | 8 | 5.0% | [0.76] | 0 | 0.0% | 2 | 1.2% | [2.55] |
| Friends | 3 | 1.6% | 8 | 5.0% | [3.43] | 2 | 1.0% | 3 | 1.8% | [0.52] |
| Written | ||||||||||
| Library | 17 | 8.8% | 14 | 8.7% | [0.00] | 27 | 12.9% | 15 | 9.1% | [1.36] |
| Medical Journal | 1 | 0.5% | 1 | 0.6% | [0.02] | 10 | 4.8% | 12 | 7.3% | [1.03] |
| Newspaper/Magazine | 5 | 2.6% | 3 | 1.9% | [0.20] | 5 | 2.4% | 4 | 2.4% | [0.00] |
| Brochure | 0 | 0.0% | 2 | 1.2% | [2.42] | 2 | 1.0% | 5 | 3.0% | [2.16] |
| Other | ||||||||||
| Teacher/School | 16 | 8.3% | 14 | 8.7% | [0.02] | 9 | 4.3% | 2 | 1.2% | [3.09] |
| Internet | 99 | 51.0% | 100 | 62.1% | [4.39] * | 103 | 49.3% | 93 | 56.4% | [1.85] |
| Church | 0 | 0 | 0 | 0.0% | 1 | 0.6% | [1.27] | |||
| TV | 2 | 1.0% | 2 | 1.2% | [0.04] | 5 | 2.4% | 3 | 1.8% | [0.15] |
Note: ADHD = attention deficit/hyperativity disorder; bolded entries indicate statistically significant findings;
p <.05;
p <.01;
p <.001
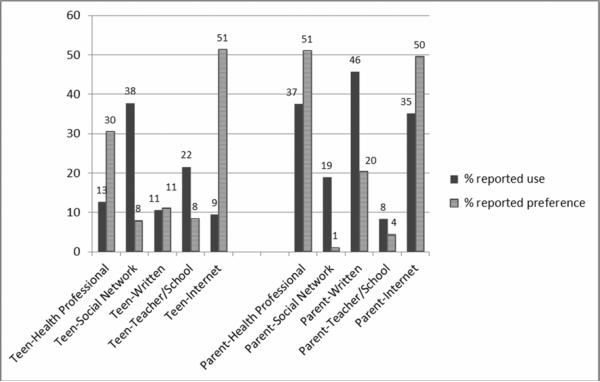
Figure 1.
Adolescents' and parents' reported and preferred use of ADHD information sources
RESULTS
ADHD knowledge, perceptions and cues to action
Almost all adolescents (93%, n=330) had heard of ADHD, nearly one-half (49%, n=173) considered themselves knowledgeable about it, over one-quarter (27%, n=94) considered sugar a cause of ADHD, two-thirds (67%, n=235) expressed concerns about overmedication and most (79%, n=280) knew someone with ADHD. As shown in Table 1, four out of the five adolescent outcome responses were associated with one or more of our predictor variables; only concern about medication overuse was not. Adolescent racial background was the most common predictor. Caucasian adolescents expressed higher knowledge and greater familiarity with ADHD and were less likely to attribute it to sugar than their African American peers. Knowledge, perceptions and cues to action did not vary by gender.
Virtually all parents (98%, n=366) had heard of ADHD, most (78%, n=291) considered themselves knowledgeable about it, one-quarter (25%, n=92) considered sugar a cause of ADHD, and most expressed concerns about overmedication (85%, n=315) or knew someone with ADHD (89%, n=280). As shown in Table 2, all parent outcome responses were associated with one or more of our predictor variables. For parents, their child's past mental health treatment status was the most common predictor, followed by racial background. Parents whose child had past mental health treatment and Caucasian parents expressed greater knowledge and more familiarity with ADHD than those without treatment experience or African American parents, respectively. Like adolescents, Caucasian parents were less likely to attribute ADHD to sugar than their African American peers.
Utilized ADHD information sources
Adolescents used on average 1.2 sources (SD .72, range 0–3) and parents 1.8 sources (SD 1.1, range 0–6) (p<.0001). The most common sources of ADHD information for adolescents were “other” (44.8%; n=159) that comprised teacher/school, Internet and television and “social network” sources (39%, n=139). Use of “written” (11.8%, n=42) and “professional” (9.0%, n=32) sources was relatively rare. Like adolescents, parents reported the most common use of “other” (55.4%, n=207) sources, but parents also relied on “written” (40.6%, n=152), health professional (30.5%, n=114) and “social network” (24.0%, n=90) sources for their ADHD information. As shown in Table 3, ADHD risk status was associated with selected variations in information sources, including doctors, relatives, friends, library, teacher/school and Internet. For both adolescent and parent respondents from the ADHD/Risk group were more likely to use doctors as ADHD information sources, but less likely to obtain information from friends or teachers compared to their low risk peers.
Preferred ADHD information sources
Adolescents voiced preference for on average 1.2 sources (SD .59, range 0–4) and parents 1.3 sources (SD .74, range 0–6) (p<.001). The leading preferred ADHD information source for adolescents and parents was the Internet (56.1%, n=199 and 52.4%, n=196, respectively). Adolescents voiced limited preference for “health professional” (27.0%, n=96), and “written” (12.1%, n=43) sources and were least interested in “social network” sources (8.7%, n=31) for ADHD information. Like adolescents, parents also voiced limited interest in “written” (19.5%, n=73) or “social network” sources (1.9%, n=7); however, parents expressed notable interest in “health professional” (45.2%, n=169) sources. As shown in Table 4, ADHD risk status had only limited associations with information source preferences in adolescents (Internet) and parents (hospital/clinic).
Information source use versus preference in the ADHD/Risk group
For each ADHD information source category we conducted McNemar's test to contrast reported and preferred use. For adolescents we found significant disagreement for the categories “health professional” (χ2(1)=21.4, p<.0001), “social network” (χ2(1)=44.8, p<.0001), “teacher/school” (χ2(1)=15.2, p<.0001) and “Internet” (χ2(1)=66.7, p<.0001), but not for “written” sources (χ2(1)=.18, p=0.7316). As shown in Figure 1, compared to their reported use, youth expressed more preference for information from health professionals and the Internet, and less preference for information from their social network and teacher or school. As shown in Figure 2, parents of adolescents in the ADHD/Risk group exhibited the same pattern as the adolescents, and in addition, expressed less preference for written information than actual use. McNemar's testing results for parents were as follows: “health professional” (χ2(1)=9.1, p=0.0025); “social network” (χ2(1)=35.1, p<.0001);“written”(χ2(1)=36.5, p<.0001); “teacher/school” (χ2(1)=4.6, p=.0325); and “Internet” (χ2(1)=12.2, p=.0005).
DISCUSSION
In this community sample, most adolescents and parents expressed some familiarity with ADHD and the majority indicated they personally knew someone with ADHD. Parents expressed higher self-rated ADHD knowledge than their adolescents; yet, study findings suggest that misperceptions about ADHD and its treatment were considerable despite relatively high self-perceived knowledge. About one-quarter of parents and adolescents endorsed sugar as an etiology for ADHD. Beliefs that excess sugar consumption causes ADHD are longstanding and persist despite older meta-analytic studies showing no association between sugar and behavior or cognitive performance of children [23]. Further, the “sugar hypothesis” of ADHD was thought to be discredited by studies which failed to document effects of sugar in children considered sensitive to sugar by their parents [24]. Of note, newer research proposes that in a subset of patients excessive sugar intake can lead to new onset ADHD via enhanced dopamine release in response to sugar and eventual reduced frontal lobe sensitivity to natural rewards resulting in ADHD behavior and overeating [25]. However, presently these cutting edge hypotheses are unproven. Our study respondents' belief in the sugar etiology therefore most likely reflects old popular beliefs rather than awareness of hypothesized changes in neurocircuitry that may support sugar's causal role. Additionally, while 85% of parents and 67% of adolescents perceived that medication was overused, this assumption is contradicted by scientific facts. Even though the use of ADHD medications has increased over the past decade, particularly in adolescents [26], health services utilization studies indicate that a significant percentage of children with ADHD remain untreated [27] and that among those receiving ADHD interventions through community mental health, less than one-third receive ADHD medications [28].
Race/ethnicity differences in ADHD familiarity
Race/ethnicity, but not poverty, was a key influential factor for ADHD knowledge, attitudes and cues to action, a finding that applied to parents and adolescents. To our knowledge, this is the first study to compare ADHD knowledge and familiarity of African American adolescents to Caucasian peers within a large, community-based sample. Findings suggest lower ADHD awareness and self-reported knowledge and more pervasive beliefs in the ADHD sugar etiology among African American adolescents, similar to patterns found for adults. Our parent findings are consistent with other studies reporting lower ADHD awareness in African American parents [29]. Unaddressed racial/ethnic differences in ADHD concepts may be a central force that perpetuates disparities in ADHD care, including lower use of ADHD medications in racial/ethnic minorities than in Caucasian children [26]. Our findings therefore highlight the importance of devising psychoeducational approaches for ADHD that are culturally sensitive and tailored to improve information exchange between providers, parents and teens.
ADHD Information sources
To our knowledge, no previous studies have sought to identify adolescent ADHD information sources, thus no comparison data are available to set our findings within a broader context. Nevertheless, our results depict a more passive knowledge gathering style for adolescents than adults. Most adolescents received ADHD information in the interpersonal context of their daily routines (attending school and socializing with network members) and adolescents rarely initiated extra steps to access ADHD materials, such as seeking out written or Internet sources. Notably, adolescents showed even less preference for written sources than their actual use, which may indicate relative easy accessibility of materials like magazines or brochures. In contrast, parents took a more active stance and sought out a broad range of ADHD information sources, consistent with the Health Tracking Household Study, which reported that adults pursue a variety of sources about health concerns [30]. Interestingly, an overall decline in adults' health information seeking was noted between 2007 and 2010, particularly in pursuit of print media, without any increase in Internet use despite rapid proliferation of residential broadband during this time period [30], interpreted as potential information overload through conflicting sources. This latter point merits consideration as health care providers devise shared parent-provider ADHD psychoeducation plans because provider information will compete with data gathered from other sources and must be considered trustworthy to be accepted.
Potential ADHD stigma indicators
Our study identified social network members as important de facto ADHD information sources for adolescents and parents, yet neither expressed desire to have relatives or friends serve in this function. We question whether this discrepancy between practice and preference may reflect well-documented stigma associated with mental disorders, including ADHD [4, 15, 31]. The role of social networks in treatment-seeking for youth with mental health problems has been examined in several studies, but remains inconclusive, with some suggestion that supportive parental networks lowers the likelihood of child treatment [32], whereas larger, supportive adolescent social networks may increase use of school mental health services [33].
Internet as ADHD information source
In our study both parents and adolescents expressed preferences for obtaining ADHD information from the Internet. This finding is consistent with general trends towards the web as a health information source [17]. However, increasing reliance on the web for health education poses several problems. Internet access remains inequitable and can reinforce health disparities [34]. Without adequate evaluation skills, web users are also vulnerable to misinformation [17], yet little is known about how to assess and enhance online health literacy [35]. Keeping in mind that both parents' and adolescents' top information preferences were the Internet, followed by the doctor, we conclude that providers should proactively identify reputable websites for their patients and family members. Quality, accountability and credibility of Internet ADHD information are often poor, with low agreement to evidence-based practices [36], and by screening available sites doctors can meet their patients' needs, improve rapport, and decrease the likelihood of misinformation or overload by conflicting sources.
Doctor as desired ADHD information source
Our study findings suggest the need for more effective inclusion of youth in ADHD psychoeducation. Past mental health treatment was associated with higher parental, but not adolescent, ADHD knowledge. We speculate that providers may have preferentially directed ADHD psychoeducation toward parents or did not delivered it in an age-appropriate format to teens. As children with ADHD mature, the balance of information-sharing needs to shift from the provider/parent dyad to the provider/patient dyad [37]. It is encouraging that adolescents rank doctors among their top preferred ADHD information sources. Time for patient-provider communication during an ADHD care visit is an increasingly precious commodity, but is of high priority for both parents and teens. Nevertheless, without more specific guidelines on psychoeducation interventions for adolescents with ADHD, doctors are left to decide how to best utilized limited appointment time to meet adolescents' education needs while supporting teens' developmentally appropriate push for increasing autonomy, to enhance opportunities for effective partnerships in ADHD treatment.
Study limitations
The generalizability of our findings is limited by sampling from one geographic region and the absence of racial/ethnic groups other than Caucasian and African Americans. The assessment of ADHD knowledge also focused on generic aspects rather than details required to develop patient educational modules. Furthermore, the interview did not elicit the perceived usefulness and trustworthiness of information obtained from various sources that could refine prioritizing information sources for a psychoeducation intervention. Lastly, our cross-sectional findings cannot determine whether improving ADHD knowledge will result in improved patient outcomes.
Implications
Further research is needed to more clearly delineate how misperceptions and inaccurate knowledge surrounding ADHD interventions affect utilization and outcomes. Simultaneously, to assist in the development of efficacious educational interventions, more data is needed on current provider practices and how they can be enhanced to meet the culturally diverse needs of adolescent patients and their parents. While awaiting results of such studies, ADHD treatment providers for adolescents should strive to conduct culturally sensitive psychoeducational needs assessments. Study findings can be interpreted to indicate that educational strategies should combine doctor-provided ADHD information with suggested reputable websites and protect time for information exchange with the doctor to align with priorities shared by adolescents and their parents.
Acknowledgements
(The corresponding author affirms that she has listed everyone who contributed significantly to the work in the Acknowledgements):
The authors would like to thank Phillip Porter for his assistance with statistical analyses, and the parents and adolescents whose participation made the study possible.
Source of support: This study was supported by grant RO1MH57399 from the National Institute of Mental Health
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lara C, Fayyad J, de Graaf R, et al. Childhood Predictors of Adult Attention-Deficit/Hyperactivity Disorder: Results from the World Health Organization World Mental Health Survey Initiative. Biol Psychiatry. 2009;65(1):46–54. doi: 10.1016/j.biopsych.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Molina BS, Hinshaw SP, Swanson JM, et al. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry. 2009 May;48(5):484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harpaz-Rotem I, Leslie D, Rosenheck RA. Treatment retention among children entering a new episode of mental health care. Psychiatr Serv. 2004;55(9):1022–1028. doi: 10.1176/appi.ps.55.9.1022. [DOI] [PubMed] [Google Scholar]
- 4.Bussing R, Zima BT, Mason DM, et al. Receiving treatment for attention-deficit hyperactivity disorder: do the perspectives of adolescents matter? J Adolesc Health. 2011 Jul;49(1):7–14. doi: 10.1016/j.jadohealth.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goldston DB, Reboussin BA, Kancler C, et al. Rates and predictors of aftercare services among formerly hospitalized adolescents: A prospective naturalistic study. J Am Acad Child Adolesc Psychiatry. 2003 Jan;42(1):49–56. doi: 10.1097/00004583-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Bodenheimer T, Lorig K, Holman H, et al. Patient self-management of chronic disease in primary care. JAMA. 2002 Nov 20;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 7.Wolraich M, Brown L, Brown RT, et al. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011 Nov;128(5):1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2:328–335. [Google Scholar]
- 9.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984 Spring;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 1.Pescosolido BA, Jensen PS, Martin JK, et al. Public knowledge and assessment of child mental health problems: findings from the National Stigma Study-Children. J Am Acad Child Adolesc Psychiatry. 2008 Mar;47(3):339–349. doi: 10.1097/CHI.0b013e318160e3a0. [DOI] [PubMed] [Google Scholar]
- 11.Bussing R, Gary FA, Mills TL, et al. Cultural variations in parental health beliefs, knowledge, and information sources related to attention-deficit/hyperactivity disorder. J Fam Issues. 2007;28(3):291–318. [Google Scholar]
- 12.Pescosolido BA, Perry BL, Martin JK, et al. Stigmatizing attitudes and beliefs about treatment and psychiatric medications for children with mental illness. Psychiatr Serv. 2007 May;58(5):613–618. doi: 10.1176/ps.2007.58.5.613. [DOI] [PubMed] [Google Scholar]
- 13.Bussing R, Gary FA, Mills TL, et al. Parental explanatory models of ADHD: gender and cultural variations. Soc Psychiatry Psychiatr Epidemiol. 2003 Oct;38(10):563–575. doi: 10.1007/s00127-003-0674-8. [DOI] [PubMed] [Google Scholar]
- 14.dosReis S, Zito JM, Safer DJ, et al. Parental perceptions and satisfaction with stimulant medication for attention-deficit hyperactivity disorder. J Dev Behav Pediatr. 2003 Jun;24(3):155–162. doi: 10.1097/00004703-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Coleman D, Walker JS, Lee J, et al. Children's beliefs about causes of childhood depression and ADHD: A study of stigmatization. Psychiatr Serv. 2009;60(7):950–957. doi: 10.1176/ps.2009.60.7.950. [DOI] [PubMed] [Google Scholar]
- 16.Sciberras E, Iyer S, Efron D, et al. Information needs of parents of children with attention-deficit/hyperactivity disorder. Clin Pediatr (Phila) 2010;49(2):150–157. doi: 10.1177/0009922809346730. [DOI] [PubMed] [Google Scholar]
- 17.Cline RJ, Haynes KM. Consumer health information seeking on the Internet: the state of the art. Health Educ Res. 2001 Dec;16(6):671–692. doi: 10.1093/her/16.6.671. [DOI] [PubMed] [Google Scholar]
- 18.Bussing R, Zima BT, Gary FA, et al. Barriers to detection, help-seeking, and service use for children with ADHD symptoms. J Behav Health Serv Res. 2003;30(2):176–189. doi: 10.1007/BF02289806. [DOI] [PubMed] [Google Scholar]
- 19.Bussing R, Fernandez M, Harwood M, et al. Parent and teacher SNAP-IV ratings of attention deficit hyperactivity disorder symptoms: psychometric properties and normative ratings from a school district sample. Assessment. 2008 Sep;15(3):317–328. doi: 10.1177/1073191107313888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burns BJ, Angold A, Magruder-Habib K, et al. The Child and Adolescent Services Assessment. Duke Medical Center; Durham, N.C.: 1992. [Google Scholar]
- 21.Bussing R, Mason DM, Leon CE, et al. Agreement between CASA parent reports and provider records of children's ADHD services. J Behav Health Serv Res. 2003;30(4):462–469. doi: 10.1007/BF02287433. [DOI] [PubMed] [Google Scholar]
- 22.Bussing R, Schoenberg NE, Perwien AR. Knowledge and information about ADHD: Evidence of cultural differences among African-American and white parents. Soc Sci Med. 1998;46(7):919–928. doi: 10.1016/s0277-9536(97)00219-0. [DOI] [PubMed] [Google Scholar]
- 23.Wolraich ML, Wilson DB, White JW. The effect of sugar on behavior or cognition in children. A meta-analysis. JAMA. 1995;274(20):1617–1621. doi: 10.1001/jama.1995.03530200053037. [DOI] [PubMed] [Google Scholar]
- 24.Wolraich ML, Lindgren SD, Stumbo PJ, et al. Effects of diets high in sucrose or aspartame on the behavior and cognitive performance of children. N Engl J Med. 1994;330(5):301–307. doi: 10.1056/NEJM199402033300501. [DOI] [PubMed] [Google Scholar]
- 25.Johnson RJ, Gold MS, Johnson DR, et al. Attention-deficit/hyperactivity disorder: is it time to reappraise the role of sugar consumption? Postgrad Med. 2011;123(5):39–49. doi: 10.3810/pgm.2011.09.2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zuvekas SH, Vitiello B. Stimulant Medication Use in Children: A 12-Year Perspective. A□ J Psychiatry. 2011 doi: 10.1176/appi.ajp.2011.11030387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cuffe SP, Moore CG, McKeown R. ADHD and Health Services Utilization in the National Health Interview Survey. J Atten Disord. 2009;12(4):330–340. doi: 10.1177/1087054708323248. [DOI] [PubMed] [Google Scholar]
- 28.Zima BT, Bussing R, Tang L, et al. Quality of care for childhood attention-deficit/hyperactivity disorder in a managed care medicaid program. J Am Acad Child Adolesc Psychiatry. 2010;49(12):1225–1237. 1237, e1221–1211. doi: 10.1016/j.jaac.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bailey R, Ali S, Jabeen S, et al. Attention-Deficit/Hyperactivity Disorder in African American Youth. Curr Psychiatry Rep. 2010;12(5):396–402. doi: 10.1007/s11920-010-0144-4. [DOI] [PubMed] [Google Scholar]
- 30.Center for Studying Health System Change . Surprising decline in consumers seeking health information. Tracking Report; Washington, D.C.: 2011. [PubMed] [Google Scholar]
- 31.Gajaria A, Yeung E, Goodale T, et al. Beliefs About Attention-Deficit/Hyperactivity Disorder and Response to Stereotypes: Youth Postings in Facebook Groups. J Adolesc Health. 2011;49(1):15–20. doi: 10.1016/j.jadohealth.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 32.Bussing R, Zima BT, Gary FA, et al. Social networks, caregiver strain, and utilization of mental health services among elementary school students at high risk for ADHD. J Am Acad Child Adolesc Psychiatry. 2003;42(7):842–850. doi: 10.1097/01.CHI.0000046876.27264.BF. [DOI] [PubMed] [Google Scholar]
- 33.Lindsey MA, Barksdale CL, Lambert SF, et al. Social network influences on service use among urban, African American youth with mental health problems. J Adolesc Health. 2010;47(4):367–373. doi: 10.1016/j.jadohealth.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen RA, Adams PF. Use of the internet for health information. NCHS Data Brief. 2011;66:1–8. [PubMed] [Google Scholar]
- 35.Car J, Lang B, Colledge A, et al. Interventions for enhancing consumers' online health literacy. Cochrane Database Syst Rev. 2011;(6):CD007092. doi: 10.1002/14651858.CD007092.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kisely S, Ong G, Takyar A. A survey of the quality of web based information on the treatment of schizophrenia and Attention Deficit Hyperactivity Disorder. Aust N Z J Psychiatry. 2003;37(1):85–91. doi: 10.1046/j.1440-1614.2003.01107.x. [DOI] [PubMed] [Google Scholar]
- 37.Albrecht TL, Penner LA, Cline RJ, et al. Studying the process of clinical communication: issues of context, concepts, and research directions. J Health Commun. 2009;14(Suppl 1):47–56. doi: 10.1080/10810730902806794. [DOI] [PubMed] [Google Scholar]