The rise of antimicrobial resistance was placed firmly on the world map with the publication of the World Health Organization (WHO) report in March of this year and there have been other calls for international action.1 GPs are well aware of the problem of resistance but don’t really take ownership, attributing resistance to prescribing by other organisations or sectors.2 However, 80% of antibiotics are prescribed in primary care3 and there is ample evidence of the link between outpatient prescribing and antibiotic resistance.4
THE IMPORTANCE OF EUROPEAN ANTIBIOTIC AWARENESS DAY
The fourth in the series of the now annual European Antibiotic Awareness Day (EAAD) was held on the 18 November 2012. The day endeavoured to increase the profile of initiatives designed to improve antibiotic use across Europe aimed at the general public and professionals in both community and hospital settings. Rates of antibiotic resistance are still increasing across Europe, and as resistance is related to use, campaigns have been aimed at encouraging more appropriate prescribing to control the emergence and spread of new resistant bacteria.5 The antibiotic campaign in England, following the publication of the 1998 Standing Medical Advisory Committee report, The Path of Least Resistance,3 led to a fall in community antibiotic prescriptions, but between 2005 and 2011 total antibiotic items prescribed have risen by about 8%.6 Despite this overall increase in antibiotic prescribing there have been some successes associated with improved awareness of the importance of appropriate antibiotic prescribing. Hospital initiatives aimed at controlling methicillin-resistant Staphylococcus aureus and Clostridium difficile have led to a fall in both infections from these organisms and cephalosporin and quinolone usage, which were considered one of the main drivers of these infections. However there has been a steady rise in extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli and Klebsiella spp in both the hospital and community setting over the past few years.7 Therefore the ideals of EAAD are still relevant and worth promoting.
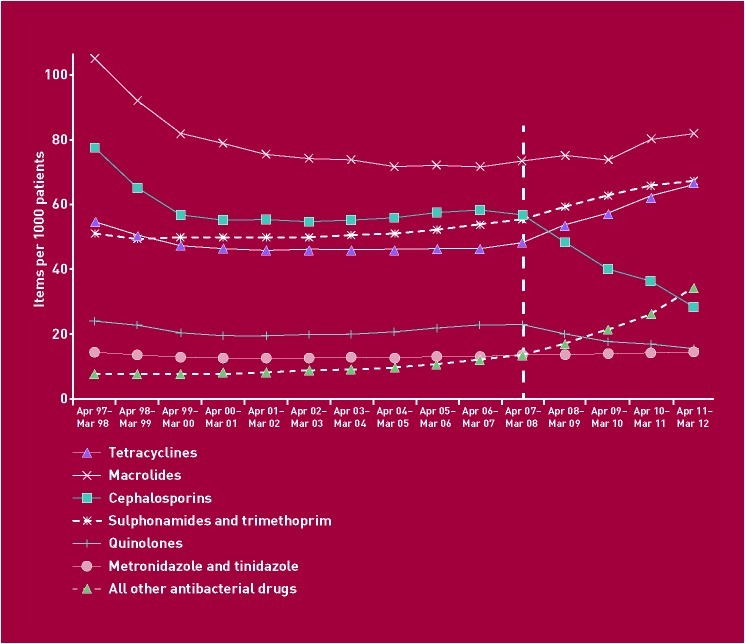
Recent changes in hospital prescribing have been mirrored in community antibiotic prescriptions. The number of community prescription items for cephalosporins in the past 4 years has fallen by 49% and that of quinolones by 35% (Figure 1).6 In contrast the number of prescriptions for tetracyclines, macrolides, trimethoprim, and Macrodantin® (Mercury), which are the first-line antibiotics recommended by national guidance,8,9 have increased,6 resulting in an overall rise in antibiotic prescribing in the community. Cross-European comparisons show that the UK has some way to go before prescribing rates match those of other north European countries. It comes down to further action being taken in the community setting.
Figure 1.
Trends in prescribing antibacterial items (excluding penicillins) in English general practices, with change since 2007/2008.6
GENERAL PRACTICE AND EAAD
EAAD 2012 encourages GPs across the UK to make antimicrobial stewardship a clinical priority, through the launch of a new toolkit: ‘Treat Antibiotics Responsibly, Guidance, Education, Tools’ (TARGET Antibiotics), which will be available on the Royal College of General Practitioners (RCGP) website.10 The TARGET Antibiotic resources have been developed for use in primary care, to highlight the importance of antimicrobial resistance and responsible use, through resources aimed at the clinicians themselves and for them to share with the patients during consultations (Table 1). The resources have been developed by the RCGP and members of Antimicrobial Stewardship In Primary Care Group (ASPIC), a multiprofessional group including GPs, nurses, microbiologists, pharmacists, and patients.11
Table 1.
Resources on the RCGP TARGET Antibiotics website
| TARGET resources | For clinicians | For patients |
|---|---|---|
| Guidance | • Antibiotic guidance for local adaptation • Antibiotic App |
• Guidance for GPs on how to optimise use of the patient materials |
| Education | • PowerPoint presentation template for local adaptation • Links to clinical modules covering antimicrobial use (for example respiratory or urinary tract infections on the RCGP and other websites |
• Materials to share with the patient during the consultation • Life channel antibiotic videos to run in the waiting room • Links to e-Bug educational activities |
| Tools | • Self-assessment tool to assess locality and GP surgery antimicrobial stewardship programmes, guidance, education and audit | • Patient leaflet to be used within consultation • Audit materials to evaluate GP surgery antimicrobial use • Links to other leaflets and tools to use with patients |
It is the turn of primary care to embrace EAAD, and to utilise the available resources of both the TARGET Antibiotics website and EAAD. The resources can all be accessed via the Department of Health website (www.dh.gov.uk) or by searching Google with the terms ‘EAAD’, ‘2012’, and ‘England’.
Acknowledgments
Many thanks to all the members of the Antimicrobial Stewardship in Primary Care Group who gave advice on development of the TARGET resources: Louise Brown, Jonathan Cooke, Barry Cookson, Mike Cooper, Tracey Cooper, Peter Davey, Harpal Dhillon, Matthew Fitzpatrick, Naomi Fleming, Linda Forrester, Nick Francis, Carole Fry, Rose Gallagher, Emma Gilgunn-Jones, Christopher Gush, Gail Haddock, Kieran Hand, Gwyn Harris, Philip Howard, Alison Holmes, Steve Holmes, Robin Howe, Simon Hurding, Hiral Khoda, Donna Lecky, Paula Mansell, Sinead McElroy, Cliodna McNulty, Michael Moore, John Morrison, Neal Patel, Margaret Peycke, Imran Rafi, Mike Sharland, Chris Sherlaw-Johnson, Jacqueline Sneddon, Naomi Stanton, Jane Stockley, Jonathan Underhill, Sally Wellsteed, Lorna Willocks and Debbie Wright.
Provenance
Commissioned; not externally peer reviewed.
Competing interests
Michael Moore is the RCGP clinical champion for antimicrobial stewardship.
REFERENCES
- 1.Carlet J, Jarlier V, Harbarth S, et al. Ready for a world without antibiotics? The Pensières Antibiotic Resistance Call to Action. Antimicrob Resist Infect Control. 2012;1(1):11. doi: 10.1186/2047-2994-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wood F, Phillips C, Brookes-Howell L, et al. Primary care clinicians’ perceptions of antibiotic resistance: a multi-country qualitative interview study. J Antimicrob Chemother. (2012) doi: 10.1093/jac/dks338. DOI: 10.1093/jac/dks338. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health. The path of least resistance. Main report of the Standing Medical Advisory Committee, Sub-Group on Antimicrobial Resistance. Report No: 152. London: DoH; 1998. [Google Scholar]
- 4.Goossens H, Ferech M, Vander SR, Elseviers M. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365(9459):579–587. doi: 10.1016/S0140-6736(05)17907-0. [DOI] [PubMed] [Google Scholar]
- 5.British Society of Antimicrobial Chemotherapy. Antibiotic action — the arms race. Birmingham: British Society for Antimicrobial Chemotherapy; 2011. http://antibiotic-action.com (accessed 1 Nov 2012) [Google Scholar]
- 6.NHS Prescription Services. Antibiotics National Charts. NHSBSA; 2011. http://www.nhsbsa.nhs.uk/PrescriptionServices/Documents/PPDPrescribingAnalysisCharts/Antibiotics_Jun_11_-_National.pdf (accessed 1 Nov 2012) [Google Scholar]
- 7.Enoch DA, Brown F, Sismey AW, et al. Epidemiology of extended-spectrum beta-lactamase-producing Enterobacteriaceae in a UK district hospital; an observational study. J Hosp Infect. 2012;81(4):270–277. doi: 10.1016/j.jhin.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 8.Department of Health Guidance. Antimicrobial stewardship: start smart — then focus. London: DoH; 2011. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_131062 (accessed 1 Nov 2012) [Google Scholar]
- 9.Health Protection Agency. Management of infection guidance for primary care for consultation and local adaptation. London: HPA; 2000. http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1279888711402 (accessed 1 Nov 2012) [Google Scholar]
- 10.RCGP and members of Antimicrobial Stewardship in Primary Care Group. TARGET antibiotics. London: RCGP; 2012. http://www.RCGP.org.uk/TARGETantibiotics/ (accessed 13 Nov 2012) [Google Scholar]
- 11.McNulty CAM, Francis NA. Optimizing antibiotic prescribing in primary care settings in the UK: findings of a BSAC multi-disciplinary workshop 2009. J Antimicrob Chemother. 2010;65(11):1–7. doi: 10.1093/jac/dkq361. [DOI] [PubMed] [Google Scholar]