Abstract
Background
Correspondence from occupational physicians to GPs is infrequent, despite evidence that good communication leads to earlier return to work of sick-listed patients and is cost effective.
Aim
To explore the circumstances, content, and preferred method of communication GPs would value from an occupational physician, following an occupational health consultation with one of their patients.
Design and setting
A cross-sectional survey in the UK.
Method
A questionnaire was developed de novo, piloted, and sent to 600 GPs of consecutive employees undergoing occupational physician assessments. Descriptive data were generated using Excel®.
Results
The response rate was 374/600 (62%). Demographic features of GP responders reflected national figures. A total of 372 (99.5%) GPs wanted information from occupational physicians. Most wanted information on diagnosis (303, 81%), clinical assessment (275, 74%), functional assessment (295, 79%), or advice on the timing (308, 82%) and adjustments 290 (78%) of any return-to-work plan. Over 80% wanted information following every occupational physician consultation, and over 90% wanted information on the timing of a return to work, adjustments suggested, or if different medical diagnosis or management was suggested. The preferred method of communication was letter by post 341/374 (92%). Brief, relevant information was valued and considered useful for completing ‘fit notes’.
Conclusion
Occupational physicians should send formal letters, by post, to the patient’s GP following occupational health assessments. This would assist the GP in completing the patient’s ‘fit note’ and ultimately increase the chances of their patient being rehabilitated back to work.
Keywords: communication, cross-sectional survey, general practitioners, occupational health physicians
INTRODUCTION
In contrast to most other clinical specialties, communication between GPs and occupational physicians is generally poor.1–6 The problem arises because referrals are sent by the employer to the occupational physicians and the occupational physicians’ reports are returned to the employers, and because, in contrast to most other specialties, occupational health in the UK is not part of the NHS. Professional guidance recommends that, subject to consent, the occupational physician should inform the GP of work-related facts that may have a bearing on the health of the individual.7–9 The NHS Plan makes a commitment that patients have the right to receive copies of clinicians’ letters about them.10 However, there is evidence that occupational physicians do not routinely communicate with GPs: in a recent audit of depression screening,11 only 20% of occupational physicians communicated with the GP when an employee was diagnosed by occupational health with depression.
Lack of knowledge of, and negative attitudes to, occupational health by GPs have been well documented and shown to be a barrier to vocational rehabilitation of workers absent from work because of ill health.7,12–14 There is evidence that improved communication between occupational physicians and patients’ primary and secondary care providers improves vocational rehabilitation for employees on long-term sick leave, leads to earlier return to work, and is cost effective.15 Dame Carol Black’s review of the health of Britain’s working age population. Working for a Healthier Tomorrow, puts an emphasis on improving the rates of return to work following sickness absence, and increasing occupational health input to facilitate this.16
The aims of the study were to explore the circumstances in which GPs would value communication from an occupational physician following an occupational health consultation with one of their patients; the information GPs would like the communication to contain; and their preferred method of communication. There is no previous research examining these questions.
METHOD
A cross-sectional questionnaire study was undertaken. The sampling frame was all GPs of employees undergoing occupational physician assessments by one national occupational health provider (Nexus Healthcare Limited) between 1 December 2009 and 30 June 2010 inclusive.
How this fits in
Occupational physicians do not routinely communicate with GPs, despite strong evidence that good communication leads to earlier return to work in sick-listed patients, and is cost effective. This study reveals that GPs want more information about their patients from occupational physicians. GPs would value a report, by post, after every consultation, including clinical and functional information, advice on the timing and adjustments of any return-to-work plan, and any alternative medical diagnosis or management suggested. This would increase occupational health knowledge and awareness within general practice and would assist the GP in completing the patient’s ‘fit note’, ultimately increasing the chances of their patient being rehabilitated back to work — a prime goal of Dame Carol Black’s Review of the health of Britain’s working age population: Working for a Healthier Tomorrow.
Before each consultation, patients were asked to complete a standard clinical consent form, which included contact details of their GP. GP details were collated for the research project after the occupational health report had been completed and sent, and separately from any clinical issues, and therefore could not have influenced the clinical assessment or the report to the employer. The questionnaire was developed de novo, it contained both closed and open questions which had face validity; that is, they were deemed to be acceptable measures of the study questions by the researchers and GPs who piloted the questionnaire. The introduction to the questionnaire informed GPs that one of their patients had recently had an occupational physician assessment, and enquired as to what information the GP would like from the occupational physician. The questionnaire was divided thematically into four sections. The first three covered the circumstance, content, and method of communication. The last sought demographic information on the type and size of GP practice, age, sex, and type of GP, and any occupational health qualification held. Additional questions asked how many occupational health reports the GP had received in the last year and whether the GP had heard of Dame Carol Black’s review. The questionnaire was piloted among a 12-member GP group practice with a special interest in occupational health to ensure clarity and ease of use of the questionnaire.
Following the consultation with the occupational physician, the employee’s GP was contacted by facsimile and asked to complete and return the study questionnaire. GPs who did not respond were contacted a second time by facsimile, and if there was still no response an attempt was made to contacted them by telephone. Questionnaires were sent out between 22 April and 20 September 2010. The last questionnaire was received on 22 October 2010.
Data were collated and presented for analysis using an Excel® spreadsheet. All data entered were double checked. Data collection, handling, and storage complied with the Data Protection Act 1998. Descriptive statistical methods were used to present the data; 95% exact binomial confidence intervals were calculated. Demographic data were compared with the latest available national statistics. Free-text comments were analysed and presented thematically.
RESULTS
No changes were made to the questionnaire as a result of the pilot.
During the study period, 691 patients were assessed by occupational health physicians at Nexus Healthcare. Of these, 68 (9.8%) patients did not provide GP details and 23 (3.3%) listed a GP already listed by another patient. GPs of the remaining 600 (86.8%) patients were contacted. A total of 374/600 (62%) completed questionnaires were received: 276 (74%) were returned by facsimile, 28 (7%) were returned by post, and 70 (19%) were completed over the phone.
Demographic features of the GPs who returned questionnaires were compared to the most recent national figures available from the national statistics for NHS staff workforce — GPs, from the NHS Information Centre (2009) (Table 1).17,18 Female GPs were slightly under-represented in the survey. The age distribution of responding GPs reflects closely that of national figures, with a slight under-representation of those aged <35 years (Table 1).
Table 1.
Summary of demographic data of GP responders
| Study sample, n (%) | National statistics, 200917,18 | |
|---|---|---|
| GP partner/principal | 320 (86) | 79.4% |
| Female | 131 (35.1) | 43.7% |
| Age, years | ||
| <35 | 28 (7.5) | 12.6% |
| 35–45 | 110 (29.5) | 30.4% |
| 46–55 | 131 (35.1) | 35.1% |
| >55 | 104 (27.9) | 21.8% |
| List size (mean) | 9235 | 6637 |
| Geographic location | ||
| Rural | 35 (9.4) | 10% |
| In London | 60 (16.0)a | 13% |
| Occupational health qualification | ||
| DipOccMed | 14 (3.8) | 0.2%b |
| Other | 4 (1.1) | — |
DipOccMed = Diploma in Occupational Medicine.
Defined by postcode.
Estimate based on number of DipOccMed holders aged <65 years, data from Faculty of Occupational Medicine.
In this survey, the overwhelming majority of GPs wanted information about their patients from occupational physicians. Only 2/374 (0.5%) GPs wanted no information at all. Most of the GPs desired information on clinical and functional assessment, and advice on the timing and adjustments of any return-to-work plan. More than half wished for information regarding the applicability of disability legislation, which at the time of the study was the Disability Discrimination Act 1995. Only 29% of GPs wanted a copy of the report to the employer, which would not contain clinical information (Table 2).
Table 2.
Content of communication that GP responders would value following an occupational physician assessment of one of their patientsa
| Type of information | n (%) [95% CI], N = 374 |
|---|---|
| 1. None — I would like no communication at all | 2 (0.5) [0.1 to 2] |
| 2. Copy of full report from the occupational physician to the employer (this would not contain full clinical information) | 109 (29) [25 to 34] |
| 3. Brief summary of occupational physician’s working diagnosis | 303 (81) [77 to 85] |
| 4. Brief summary of occupational physician’s clinical findings | 275 (74) [69 to 78] |
| 5. Brief summary of occupational physician’s functional assessment: such as patient’s limitations with regard to activities of daily living/relevant work tasks/specific physical or psychological functional impairments | 295 (79) [74 to 83] |
| 6. Occupational physician’s opinion regarding current fitness for work | 324 (87) [83 to 90] |
| 7. Occupational physician’s opinion regarding applicability of the Disability Discrimination Act 1995 | 197 (53) [47 to 58] |
| 8. Details of suggested adjustments or phased return-to-work plan | 290 (78) [73 to 82] |
| 9. Anticipated return-to-work date (full or phased) | 308 (82) [78 to 86 |
Assuming the patient consents to release of the information). 95% exact binomial CIs were calculated using Stata Statistical Software.
When asked in what circumstances they would value information, over 90% wanted information regarding the timing of a return to work, on adjustments suggested, or if different medical diagnosis or management was suggested by the occupational physician, and over 80% wanted information following every occupational physician consultation (Table 3).
Table 3.
Circumstances in which GP responders would like to receive information from an occupational physician following an independent assessment of one of their patientsa
| nb (%) [95% CI] | ||||||
|---|---|---|---|---|---|---|
| Circumstances | n | Strongly agree | Agree | Neutral | Disagree | Strongly disagree |
| As with all other specialties, following each consultation | 373 | 155 (42) | 149 (40) | 40 (11) | 25 (7) | 4 (1) |
| (82)a [77 to 85) | ||||||
| If occupational physician’s diagnosis or management appears to differ from mine | 369 | 232 (63) | 118 (32) | 17 (5) | 0 (0) | 2 (0.5) |
| (95)a [92 to 97) | ||||||
| If the occupational physician has advised the employer regarding the timing of a full or partial return to work | 369 | 206 (56) | 154 (42) | 7 (2) | 1 (0.3) | 1 (0.3) |
| (98)a [95 to 99] | ||||||
| If the occupational physician has advised the employer regarding adjustments that may facilitate my patient’s return to work (temporary or permanent change in duties or hours, or special equipment, or other support) | 368 | 190 (52) | 152 (41) | 21 (6) | 3 (0.8) | 2 (0.5) |
| (93)a [90 to 95] | ||||||
Assuming the patient consents to release of the information).
Combined percentage for those who ‘Strongly agree’ and ‘Agree’ with 95% CIs. 95% exact binomial CIs were calculated using Stata Statistical Software.
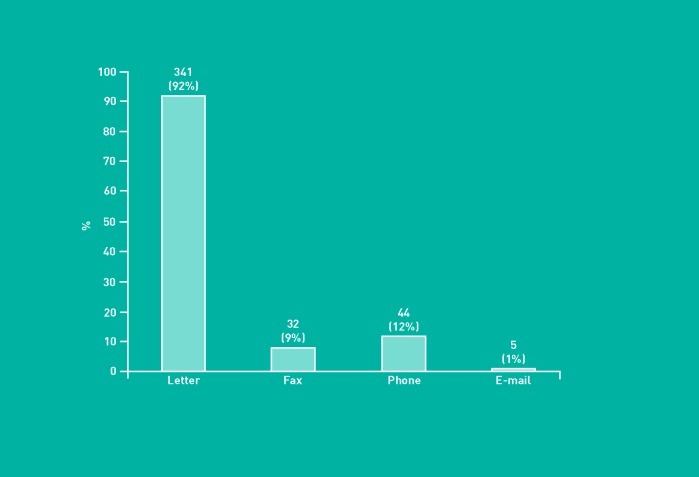
The preferred method of communication from occupational physicians was a letter by post 341 (92%) (Figure 1). A minority of 32 (9%) were happy to receive a letter by facsimile, five (1%) by email, and 44 (12%) via a phone call (categories not exclusive). Several GPs commented that they did not feel email, especially from outside the NHS.net, was sufficiently secure for passing confidential information. In addition, they commented that the volume of emails GPs received was already too high, and that they had systems in place to process data received in letters by post, but not for emails.
Figure 1.
GP responders’ preferred method of receipt of information from the occupational physician, n (%).
With regard to the number of communications actually received in the last year, 337/366 (92%) of GPs stated they received five or fewer; 165/366 (45%) stated that they had received none at all. When asked if they had heard about Dame Carol Black’s review,16 282 (76%) stated not at all; 73 (20%) said yes, a little; and only 17 (4%) were aware of its recommendations.
Several themes emerged from the free-text comments. In total, 32 free-text comments were received regarding circumstances, 26 regarding content, and 11 regarding timing. The main themes were that information from occupational health was valued, and that GPs wanted to know about the occupational health assessment and its outcome and recommendations. GPs indicated that they would like the information to be brief and relevant. A few GPs commented that a report was not necessarily useful after every consultation, especially if there was a series of consultations, and that occupational physicians should exercise discretion in sending reports to GPs. There were several comments that occupational health information would be useful for completing ‘fit notes’. Some examples of free-text comments received are presented in Box 1.
Box 1. Examples of free-text comments received from GPs
Circumstances
Any information is helpful
If occupational physician has anything helpful to suggest
Very helpful to know what the occupational physician is thinking
I think the GP should always receive a copy regardless of circumstances — it forms a vital part of the patient’s health record
It remains very useful to be informed of an occupational physician’s advice to our patient whether our own advice has been similar or not
Tell me anything you feel I need to know
Tell us of any new clinical information we haven’t noticed
Reports and information from occupational physicians are becoming of increasing importance for the very reasons stated in your information sheet. I combined general practice and OH [occupational health] for 25 years and traditionally sadly lacking information
Short report please
Not after each consultation. Summaries, or when points are made
Any other changes to management compared to GP’s current management
New findings
If strongly disagreeing with the GP and if I got it wrong, the reasons why
Content
Diagnosis and reason why patient couldn’t work
Clinical findings if significant
Clinical findings — if relevant. If occupational physician feels any further medical treatment or opinion/referral would be appropriate, for example, CBT [cognitive behavioural therapy]/ physio[therapy]. Especially with regard to occupational diseases.
But needs to be brief
Brief
Anything you feel is relevant
Any new findings
Any info with regard to ill health early retirement if recommended
Any different recommendations
Any other relevant patient information
A full copy with a synopsis of key findings
Method
Any — so long as it comes
No system currently for emailed letters
Unhappy about non-NHS net emails — encryption issues
Facsimile/phone depending on urgency of matter
DISCUSSION
Summary
This survey revealed that most GPs would value a report, by post, after every consultation, with clinical and functional information, and advice on the timing and adjustments of any return-to-work plan, and whether different medical diagnosis or management was suggested by the occupational physician. At present, such communication occurs in a minority of cases.
Strengths and limitations
The study may have been subject to responder bias: those who responded may be more likely to want communication from occupational physicians. In addition, responders may have been more likely to perceive that they should indicate a desire for communication from occupational physicians. However, a high response rate was obtained and the high degree of uniformity of responses suggests that responder bias is likely to be low. Another potential weakness is the lack of a validated or standard questionnaire; questions had to be written de novo for this study. However the questionnaire had face validity and the pilot indicated that it was clearly written.
Nexus Healthcare Limited is a national occupational health provider based in London and therefore there was a risk that London GPs would be over-represented in the study sample. However, this did not appear to be the case, as the differences between the study group and national figures was small (16% versus 13% in London). In addition, the demographic profile of the GPs in the present study was similar to that of UK GPs. Therefore, it is likely that the study findings would be generalisable to other UK-based GPs.
The study took place just after the introduction of the new Med 3 form for medical certification of sickness absence (‘fit note’) in April 2010.19 This may have influenced the results of the study because GPs may have an increased need to obtain occupational health advice in relation to their patients. Few responders had heard of Dame Carol Black’s review16 despite this review resulting in the introduction of the new ‘fit note’. This suggests that GPs may not be fully conversant with the stated reasons for the change in sickness certification: to improve communication between relevant parties and thereby facilitate successful and speedy return to work for employees absent for medical reasons.
A rough estimate of occupational physician assessments carried out each year in the UK comprises 750 specialist occupational physicians (Faculty of Occupational Medicine personal communication, 2011: figures for members and fellows aged <65 years as estimate of those in active practice) each performing 500–1000 reports per year (S Sperber, personal communication, 2011: conservative estimate based on personal experience and that of employers and colleagues). This would equal about 10–20 reports per GP per year. In the present survey, most GPs reported receiving fewer than five reports in the last year and nearly half received none. This suggests that in only a minority of cases are reports currently sent to GPs following occupational physician assessments.
Comparison with existing literature
Faber et al designed and investigated a standardised, mutually agreed form for two-way communication between occupational physicians and orthopaedic surgeons;20 however, the protocol tested did not result in significant improvement in the level of communication in the cases assessed. This would support the present finding of infrequent communication of information from occupational physicians to employees’ treating doctors.
Waddell et al found strong evidence that improved communication between all players in the return-to-work process leads to faster return to work and less sickness absence overall, and is cost effective.15 This emphasises the importance of optimum communication between occupational physicians and GPs.
Implications for practice and research
Results of this study support the introduction of routine written communication from occupational physicians to GPs, provided the patient consents. Occupational physicians should send a formal letter to the GPs of patients following an assessment on behalf of the employer. The letter should be sent in all cases, but at the very least where advice is given regarding the timing of a return to work, the recommended adjustments, or if a different medical diagnosis or management is suggested by the occupational physician. The report should contain information regarding the occupational physician’s clinical and functional assessment, advice on the timing and adjustments of any return-to-work plan, and opinion regarding the applicability of disability legislation.
Ideally, GPs would prefer a brief, relevant tailored report to themselves — not a copy of the report to the employer. Although at first glance this may seem impractical, it is increasingly common for occupational health consultations and reports to be recorded directly onto computers in standardised sections on electronic pro formas. It would be possible therefore, in theory, to produce two separate computer-generated reports, using the appropriate sections of the pro forma, one for the employer and one for the GP. If a separate tailored report to the GP cannot be generated, then a copy of the report to the employer should be sent, unless it is considered that no relevant or new information is contained. The letter should be sent by post, as this is the current preferred method and is seen as the most practical and secure. If appropriate IT systems became available, GPs’ preference may change to electronic transmission in the future.
It must be acknowledged that the majority of patients receiving a Med 3 do not have an assessment by an occupational physician, so the immediate impact of improved communication would only affect a small number of patients. However, in the long run, sending occupational health reports to GPs will increase their awareness of potential workplace adjustments and the availability of occupational health advice.
GPs might feel that the occupational physician’s assessment ‘trumps’ the Med 3 and would determine recommendations to the employer; however, the Med 3 certificate is supplied primarily for purposes of statutory sick pay and is therefore required regardless of any occupational health report. In addition, in cases where there is apparent discrepancy between the advice of the GP and that of the occupational physician, this is usually because one party holds information not available to the other, either medical or work related, including scope for adjustments. Provision of occupational health reports would enhance communication between the GP and occupational physician and facilitate resolution of employment issues to the benefit of the employee.
It is unlikely that access to occupational health reports would ‘bias’ the GP when completing the ‘fit note’; this is not perceived to be the case with other clinical specialties, and evidence suggests that communication between occupational physicians and GPs improves outcomes for patients in terms of employment prospects.15
In addition, the occupational health report provides employment details and occupational key health-related issues, which the GP can enter into their records, as per National Institute for Health and Clinical Excellence recommendations.21
Further research could usefully look at the effects on occupational outcomes of providing tailored occupational physician reports to GPs, including the perspective of employees and employers.
GPs have indicated that they want more information about their patients from occupational physicians. Implementation of these recommendations would increase occupational physician–GP interactions and increase occupational health knowledge and awareness within general practice, thus contributing towards improved vocational rehabilitation and the goals of ‘the Black Review’.16
Acknowledgments
Nigel Smeeton statistician, London Research Design Centre gave statistical advice and Dr Jonathan Peters assisted at the design stage of the project, and he and his colleagues at the Holmwood Health Centre and Morland Surgery, Tadley piloted the project. Steven Sperber and the staff at Nexus Healthcare Limited supported the data collection, Rebecca Fields provided administrative support and data input, and Barbara Smiley provided administrative support.
Funding
The study was funded by NHS Plus, who approved the design of the study. Neither the funder nor the study sponsor, Nexus Healthcare Limited, was involved in the collection, analysis, interpretation of data, writing of the article, or decision to submit it for publication; this ensured the independence of researchers from funders and sponsors. Both authors had access to all of the data and can take responsibility for the integrity of the data and the accuracy of data analysis. Ira Madan received funding support from Guy’s and St Thomas’ NHS Foundation Trust.
Ethical approval
The study was approved by The National Hospital for Neurology and Neurosurgery and Institute of Neurology Joint Research Ethics Committee, study reference number 09/H0716/82.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
Anna F Stern has support from NHS Plus for the submitted work but declares no other competing interests. Ira Madden has declared no competing interests.
Data sharing
The dataset is available from the corresponding author at: anna.stern@nexushealthcare.co.uk. Consent was not obtained but the presented data are anonymised and the risk of identification is low.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Parker G. General practitioners and occupational health services. Br J Gen Pract. 1996;46(406):303–305. [PMC free article] [PubMed] [Google Scholar]
- 2.Parker G. Attitudes of general practitioners to occupational health services. J Soc Occup Med. 1991;41(1):34–36. doi: 10.1093/occmed/41.1.34. [DOI] [PubMed] [Google Scholar]
- 3.Buijs P, van Amstel R, van Dijk F. Dutch occupational physicians and general practitioners wish to improve cooperation. Occup Environ Med. 1999;56(10):709–713. doi: 10.1136/oem.56.10.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anema JR, Jettinghoff K, Houtman I, et al. Medical care of employees long-term sick listed due to mental health problems: a cohort study to describe and compare the care of the occupational physician and the general practitioner. J Occup Rehabil. 2006;16(1):41–52. doi: 10.1007/s10926-005-9001-4. [DOI] [PubMed] [Google Scholar]
- 5.Beaumont DG. The interaction between general practitioners and occupational health professionals in relation to rehabilitation for work: a Delphi study. Occup Med. 2003;53(4):249–253. doi: 10.1093/occmed/kqg066. [DOI] [PubMed] [Google Scholar]
- 6.Anema JR, Van Der Giezen AM, Buijs PC, Van Mechelen W. Ineffective disability management by doctors is an obstacle for return-to-work: a cohort study on low back pain patients sicklisted for 3–4 months. Occup Environ Med. 2002;59(11):729–33. doi: 10.1136/oem.59.11.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The OH at Work Survey on OH practice: part 1: medical confidentiality. Occupational Health (at Work) 2009;5(6):12–20. [Google Scholar]
- 8.The Faculty of Occupational Medicine, Royal College of Physicians of London. Good occupational medical practice. London: Faculty of Occupational Medicine; 2010. http://www.fom.ac.uk/wp-content/uploads/p_gomp2010.pdf (accessed 18 Oct 2012) [Google Scholar]
- 9.Harling K, Hunt S, editors. The Faculty of Occupational Physician’s guidance on ethics for occupational physicians. 6th edn. London: Faculty of Occupational Medicine; 2006. [Google Scholar]
- 10.Department of Health. Copying letters to patients: good practice guidelines. London: Department of Health; 2003. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4086054.pdf (accessed 18 Oct 2012) [Google Scholar]
- 11.Occupational Health Clinical Effectiveness Unit. Depression screening and management of staff on long-term sickness absence: occupational health practice in the NHS in England — a national clinical audit. London: Royal College of Physicians; 2009. [Google Scholar]
- 12.Morgan DR. The general practitioners’ view. Occup Med. 1999;49(6):403–405. doi: 10.1093/occmed/49.6.403. [DOI] [PubMed] [Google Scholar]
- 13.van Weel C, Orbon K, van der Gulden J, et al. Occupational health and general practice: from opportunities lost to opportunities capitalised? Med Lav. 2006;97(2):288–294. [PubMed] [Google Scholar]
- 14.Sawney P, Challenor J. Poor communication between health professionals is a barrier to rehabilitation. (Editorial) Occup Med. 2003;53(4):246–247. doi: 10.1093/occmed/kqg065. [DOI] [PubMed] [Google Scholar]
- 15.Waddell G, Burton AK, Kendall NAS. Vocational rehabilitation: what works, for whom, and when? London: The Stationery Office; 2008. Vocational Rehabilitation Task Group — Industrial Injuries Advisory Council. http://www.dwp.gov.uk/docs/hwwb-vocational-rehabilitation.pdf (accessed 18 Oct 2012) [Google Scholar]
- 16.Dame Carol Black’s Review of the health of Britain’s working age population. Presented to the Secretary of State for Health and the Secretary of State for Work and Pensions 17th March 2008. London: The Stationery Office; Working for a healthier tomorrow. http://www.dwp.gov.uk/docs/hwwb-working-for-a-healthier-tomorrow.pdf (accessed 18 Oct 2012) [Google Scholar]
- 17.The NHS Information Centre. General and personal medical services: detailed results — England. Leeds: The Health and Social Care Information Centre; 2009. Workforce and Facilities. 30 September 2009 http://www.ic.nhs.uk/webfiles/publications/010_Workforce/nhsstaff9909/GP/General Practice Staff 2009. Detailed Result.pdf (accessed 18 Oct 2012) [Google Scholar]
- 18.The NHS Information Centre. General and personal medical services: England — 1999–2009 (second edition) Leeds: The Health and Social Care Information Centre; 2010. Workforce and Facilities. http://www.ic.nhs.uk/webfiles/publications/010_Workforce/nhsstaff9909/GP/General%20Practice%20%20Bulletin%20Tables%201999%20-%202009.pdf (accessed 18 Oct 2012) [Google Scholar]
- 19.Department for Work and Pensions. Statement of fitness for work. http://www.dwp.gov.uk/healthcare-professional/news/statement-of-fitness-for-work.shtml (accessed 18 Oct 2012)
- 20.Faber E, Burdorf A, van Staa AL, et al. Qualitative evaluation of a form for standardized information exchange between orthopedic surgeons and occupational physicians. BMC Health Serv Res. 2006;6:144. doi: 10.1186/1472-6963-6-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Institute for Health and Clinical Excellence. Managing long-term sickness and incapacity for work. Guidance PH19. http://www.nice.org.uk/nicemedia/pdf/PH19Guidance.pdf (accessed 6 Nov 2012)