Abstract
Actinic keratosis is a scaly, cutaneous lesion that is often seen in elderly patients. It is almost never seen in children and young adults. It develops on areas such as the face, ears and dorsa of the hands with chronic sun exposure. Actinic keratosis is a premalignant lesion, since histological changes in the epidermis may progress to squamous cell carcinoma if left untreated. There are roughly 70,000 people with albinism in India. These patients are prone to develop actinic keratosis which may undergo spontaneous remission or develop into invasive squamous cell carcinoma, basal cell carcinoma and malignant melanoma.We present an unusual case of a 35 year old albino who developed actinic keratosis at the age 15 years which progressed to squamous cell carcinoma.
Keywords: Actinic keratosis, albinism, children, squamous cell carcinoma
INTRODUCTION
Albinism is an autosomal recessive disorder characterized by lack of melanin pigment due to which these people are prone to sun damage.[1] Albinism is of two types - ocular and oculocutaneous. The incidence of oculocutaneous albinism is estimated to be one in 20000, in most populations in the world.[1] The prevalence in regions of sub-Saharan Africa is estimated to be much greater than these figures; for example, it is estimated at about 1:4000 in Zimbabwe and in Tanzania it is 1:1429.[2]
Albinism most commonly arises from mutations in genes encoding for proteins involved in the synthesis or transport of melanin by melanocytes. Patients may present with nystagmus, strabismus, photophobia and decreased visual acuity. Patients with oculocutaneous albinism present commonly with cutaneous manifestations of actinic keratosis and are also prone to develop squamous cell carcinoma, basal cell carcinoma, malignant melanoma and dysplastic nevus syndrome.[1,3]
Actinic keratosis is a scaly, cutaneous lesion that is often seen in elderly patients. It is almost never seen in children and young adults. We present an unusual case of a 35 year old albino who developed actinic keratosis at the age 15 years which progressed to squamous cell carcinoma.
CASE REPORT
A 35 year old male presented with a swelling on the right shoulder since two months. He also gave history of tiny growths on trunk and upper limbs, since the age of 15 years. He has past history of photosensitivity and decreased vision since birth. Family history revealed history of photosensitivity and fair skin in other family members.
On physical examination, he had depigmented skin and white hairs. He had photophobia, nystagmus and decreased visual acuity. There were multiple, erythematous, papular lesions of 0.5-2 cm over trunk and upper arms [Figure 1a and b]. An ulceronodular growth on right shoulder was 3×2×2 cm, erythematous, firm and non-tender. Based on these findings, clinical diagnosis of oculocutaneous albinism with multiple actinic keratoses with squamous cell carcinoma was made. Laboratory investigations showed hemoglobin of 10 gm% with normal leukocyte and differential count. His liver and kidney function tests were normal. He was non reactive for HIV and HBsAg.
Figure 1.

(a) Multiple, papular, erythematous lesions of 0.5-2 cm over back, (b) Multiple, papular, erythematous lesions of 0.5-2 cm over upper arm.
Pathological Findings
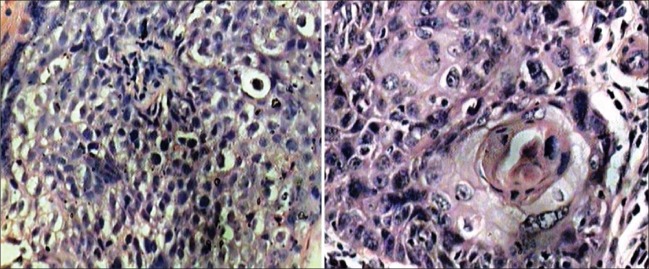
The received specimen of an ulceronodular growth measured 3×2×2 cm [Figure 2a]. Cut surface was grayish white, homogenous, firm without hemorrhage and necrosis [Figure 2b]. Microscopically, the biopsy from erythematous lesion on the back revealed actinic keratosis characterized by dyskeratosis, hyperkeratosis, irregular acanthosis, alteration of polarity of basal cell layer and atypia in kertinocytes but no dermal invasion [Figure 3a]. The sections from the nodular growth revealed squamous cell carcinoma comprised of nests and tongue-like processes of malignant squamous cells with epithelial and keratin pearl formation [Figure 3b].
Figure 2.
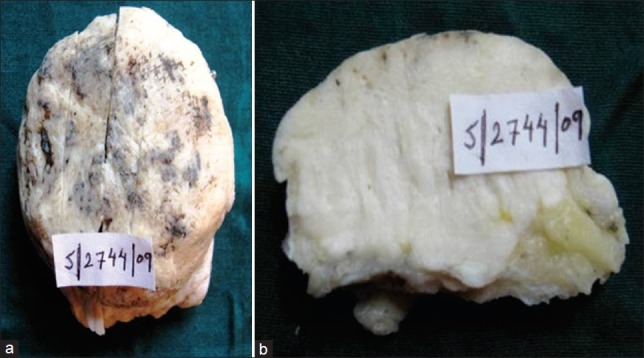
(a) A 3×2×2 cm, ulceronodular grayish white growth, (b) Cut surface showed grayish white, homogenous, firm tumor without hemorrhage and necrosis.
Figure 3.
(a) Actinic keratosis comprised of disorderly arranged atypical keratinocytes with loss of polarity in basal cell layer (H and E, ×200), (b) Squamous cell carcinoma comprised of malignant epithelial cells with epithelial pearl formation (H and E, ×400).
DISCUSSION
Actinic keratosis was first described by Dubreuilh in 1904. The factors implicated in development of actinic keratoses are UV rays, fair skin, blue eyes, blond hair, immmunosuppression and genetic diseases like albinism and xeroderma pigmentosum.[3] Prevalence of actinic keratosis depends upon the skin type and geographical location. Males develop actinic keratosis more frequently than females.[1] It develops on areas such as the face, ears and dorsa of the hands with chronic sun exposure. The rate of development of squamous cell carcinoma from actinic keratosis is estimated to be 0.025 to 16% per year.[3] Among patients with multiple actinic keratoses, the cumulative lifetime risk of having at least one invasive squamous cell carcinoma is substantial, possibly 6-10%.[4] The cumulative risk depends on the number of lesions and the length of time they persist.[5] According to Foote et al,[3] patients with actinic keratoses at highest risk for squamous cell carcinoma are older, male, red haired and have prolonged residence as an adult in a sunny region. Induration, erythema or erosion of actinic keratoses may be indicative of progression to squamous cell carcinoma. It is believed that several years can elapse before this transformation occurs.
The lesions in actinic keratoses can be flat or raised, single or multiple, pigmented or pale and usually less than 1 cm in diameter. Microscopically, actinic keratosis is defined as epidermis having irregular hyperplasia or atrophy with keratinocytes having a disorderly arrangement, accompanied by atypia.[6] Our case was a 35 year old male with oculocutaneous albinism. He developed lesions of actinic keratosis at the age of 15 years, which is uncommon. One of the lesions increased in size to attain the present size of 3×2×2 cm and was diagnosed as squamous cell carcinoma.
There are different treatment options for actinic keratosis; of which curettage and cryotherapy with liquid nitrogen, 5-flourouracil are commonly used options.[1,5] Topical chemotherapeutic agents such as those containing 5-flourouracil are used in patients with multiple lesions,[5] which was also the treatment offered in this case with excision of larger lesions.
Albinism is a disorder that affects individuals and their families, socially and psychologically. Children with albinism have to deal with issues such as photophobia, decreased visual acuity, extreme sun sensitivity, hearing problems and skin cancer. They also face social discrimination as a result of their appearance.[2]
Children with albinism need protection from sun that can be achieved with the use of sunscreens, protective clothing, and indoor activities.[1] They may be clearly well aware of the short-term consequences of sun exposure but may be less informed about the long-term risks of developing skin cancer. The children themselves must be convinced that staying out of the sun is a sensible and worthwhile choice. The involvement of the parents is also crucial to a sustained health intervention plan, if mothers can be educated and informed about albinism they will have more confidence to deal with their child's condition.[7] The Regional Dermatological Training Center (RDTC) in Moshi, Tanzania runs a mobile skin care clinic where a doctor and a nurse regularly visit villages to examine the skin of albinos and provide education on protection from UV light exposure.[8,9] It is very important for children with albinism to be accepted socially so that they can lead a normal life.
CONCLUSION
The high incidence of malignancies among children with albinism suggests that periodic monitoring and treatment are important in these patients.
Footnotes
Source of Support: Nil
Conflict of Interest: No.
REFERENCES
- 1.Ramalingam VS, Sinnakirouchenan R, Thappa DM. Malignant transformation of actinic keratoses to Squamous cell carcinoma in an albino. Indian J Dermatol. 2009;54:46–8. doi: 10.4103/0019-5154.48986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hong ES, Zeeb H, Repacholi MH. Albinism in Africa as a public health issue. BMC Public Health. 2006;6:212. doi: 10.1186/1471-2458-6-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foote JA, Harris RB, Giuliano AR, Roe DJ, Moon TE, Cartmel B, et al. Predictors for cutaneous basal and Squamous cell carcinoma among actinically damaged adults. Int J Cancer. 2001;95:7–11. doi: 10.1002/1097-0215(20010120)95:1<7::aid-ijc1001>3.0.co;2-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alam M, Ratner D. Cutaneous Squamous cell carcinoma. N Engl J Med. 2001;344:975–83. doi: 10.1056/NEJM200103293441306. [DOI] [PubMed] [Google Scholar]
- 5.Salasche SJ. Epidemiology of actinic keratoses and squamous cell carcinoma. J Am Acad Dermatol. 2000;42:4–7. doi: 10.1067/mjd.2000.103342. [DOI] [PubMed] [Google Scholar]
- 6.Dinehart SM, Nelson-Adesokan P, Cockerell C, Russell S, Brown R. Metastatic cutaneous squamous cell carcinoma derived from actinic keratosis. Cancer. 1997;79:920–3. doi: 10.1002/(sici)1097-0142(19970301)79:5<920::aid-cncr8>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 7.Ackerman AB. Solar keratosis is squamous cell carcinoma. Arch Dermatol. 2003;139:1216–7. doi: 10.1001/archderm.139.9.1216. [DOI] [PubMed] [Google Scholar]
- 8.Lund PM, Gaigher RA. A health intervention program for children with albinism at a special school in South Africa. Health Educ Res. 2002;17:365–75. doi: 10.1093/her/17.3.365. [DOI] [PubMed] [Google Scholar]
- 9.Simona B. Albinos in black, Africa: Problems and solutions. Int J Dermatol. 2004;43:616–21. [Google Scholar]