Abstract
Background: There are limited national population-based epidemiological data on acute myocardial infarction (AMI) in England, making the current burden of disease, and clinical prognosis, difficult to quantify. The aim of this study was to provide national estimates of incidence and 30-day case fatality rate (CFR) for first and recurrent AMI in England. Methods: Population-based study using person-linked routine hospital and mortality data on 79 896 individuals of any age, who were admitted to hospital for AMI or who died suddenly from AMI in 2010. Results: Of 82 252 AMI events in 2010, 83% were first. Age-standardized incidence of first AMI per 100 000 population was 130 (95% CI 129–131) in men and 55.9 (95% CI 55.3–56.6) in women. Age-standardized 30-day overall CFRs including sudden AMI deaths for men and women, respectively, were 32.4% (95% CI 32.0–32.9) and 30.3% (95% CI 29.8–30.9) for first AMI and 29.7% (95% CI 28.7–30.7) and 26.7% (95% CI 25.5–27.9) for recurrent AMI. Age-standardized hospitalized 30-day CFR was 12.0% (95% CI 11.6–12.3) for men and 12.3% (95% CI 11.9–12.7) for women. Conclusions: While the majority of AMIs are not fatal, of those that are, two-thirds occur as sudden AMI deaths. About one in six of all AMIs are recurrent events. These findings reinforce the importance of primary and secondary prevention in reducing AMI morbidity and mortality.
Introduction
Acute myocardial infarction (AMI) is a major public health concern. It is the cause of approximately three-quarters of all coronary heart disease (CHD) deaths and accounts for about a half of all CHD hospital admissions.1,2 Yet there are few recent population-based UK studies of AMI that reported incidence estimates.3–7 These studies were local rather than national (three come from Oxfordshire), did not necessarily include all age groups or distinguish between first AMI and reinfarction, and dated to the 1990s and early 2000s. As such, there are limited published comprehensive national population-based data on AMI incidence and case fatality in England, making the current burden of disease, and clinical prognosis, difficult to quantify.
To profile AMI on a national level from routine hospital and mortality statistics, data linkage is necessary to enable systematic analysis of person-based disease occurrence to be undertaken. Since 1998, it has been possible to link routinely collected hospital and deaths data for the entire population of England. We used a national-linked hospital and mortality data set to study the occurrence and outcomes of AMI in England. The principle aim of this article is to report the rates of AMI occurrence and 30-day case fatality, distinguishing first, recurrent and all AMI. The second aim of the article is to demonstrate the value of record linkage in administrative data sets for epidemiological research.
Methods
Data sources
Data were obtained from two data sets, Hospital Episode Statistics (HES) and mortality statistics, which were linked together by the Oxford Record Linkage Study team. Both data sets cover all of England and include information on all hospital admissions and deaths. The HES data set provides information on all patients admitted to hospital and whose care is funded by the English National Health Service (NHS). The mortality data are collected by the Office for National Statistics (ONS) and include all deaths that occur in England, whether in hospital or outside. The data sets are linked using probability matching of the following variables: sex, date of birth, postal code of residence, NHS number and HES ID number. The methods of matching and linkage are based on principles and methods used in the Oxford record linkage study.8
Study population
Residents of England were included in the study if they experienced an AMI event between 1 January 2010 and 31 December 2010. An AMI event was defined as an emergency hospital admission with a main discharge diagnosis of AMI (ICD-10 codes I21 or I22) and a length of stay of at least 1 day for someone discharged alive, or a death with AMI coded as the underlying cause of death on the death certificate. The 1-day criterion for hospital stay was applied to avoid counting suspected AMIs in patients who were discharged home when AMI was not confirmed. Any hospital or death records that occurred with 30 days of an AMI event were assumed to relate to the same AMI. Records with invalid dates, missing age or missing sex were excluded from the analysis (<0.1% of records).
For each person, the first occurrence of a hospital admission for AMI or a death due to AMI in 2010 was recorded as the index AMI event on the date of admission or death, as applicable. In order to classify the index AMI event in 2010 as a first event or as a recurrent event (also termed reinfarction), we used a 12-year clinical history (defined as a previous hospital record with AMI as primary or secondary diagnosis) from the English national-linked file.8 If the index AMI event in 2010 occurred in individuals with no clinical history of AMI during the previous 12 years, it was categorized as a first AMI, as a proxy for true first AMI. Otherwise, the index event was categorized as recurrent AMI.
Fatal AMIs were defined as sudden AMI deaths or hospitalized AMI that had a death record within 30 days of a hospital admission for AMI, irrespective of the cause or place of death. For the purposes of this article, we used the term ‘sudden AMI death’ to mean a death record with AMI coded as the underlying cause of death and with no linked hospital admission for AMI in the previous 30 days.
Statistical analyses
Incidence and recurrence were defined as the rates of occurrence of first and recurrent AMI, respectively. The event rate was defined as the rate of occurrence of all AMI. All rates of occurrence were calculated per 100 000 population of England by age group and sex, using the mid-year population estimates published by the ONS. Rates were directly age standardized to the European Standard Population. Recurrence rates were also calculated per 1000 individuals with a prior AMI, standardized to the age distribution of all the individuals who have had an AMI between 1998 and 2010. The 95% confidence intervals were estimated assuming that the observed number of events followed a Poisson distribution.
Hospitalized 30-day case fatality was calculated using the total number of hospitalized AMIs as the denominator, and the number of fatal hospitalized AMIs as the numerator. Overall 30-day case fatality was calculated using the total number of all AMI events as the denominator, and all fatal AMI events as the numerator. Rates were directly age standardized using 5-year age groups and the age distribution of the whole 12-year AMI event cohort as the standard population. Multiple logistic regression analysis was used to quantify the effects of sex, age, deprivation category and history of previous AMI on case fatality. These variables were included because they were available for both hospital as well as mortality records, thus allowing for development of directly comparable models for hospitalized and overall case fatality.
The Index of Multiple Deprivation (IMD) score, a weighted composite measure of overall socio-economic deprivation derived from a model of multiple deprivation domains describing particular geographic areas,9 was used as a proxy measure of socio-economic status. The IMD scores of the 12-year study cohort were grouped into deprivation quintiles.
Differences in the distributions of key variables were examined using t-tests of statistical significance for continuous variables and χ2 tests for categorical variables. Significance was accepted at P < 0.05 level; all tests were two-tailed. All analyses were performed using STATA version 11 (Stata Corporation, College Station, Texas, USA).
Results
Total study cohort in 2010
Between 1 January and 31 December 2010, a total of 82 252 AMI events occurred among 79 896 individuals. Table 1 shows the characteristics of all AMI events in 2010 by first and recurrent events. Of all the events, 83% were first AMIs; 61% occurred in men; 32% were fatal; and 73% occurred in people aged ≥65 years. Among recurrent AMI events in 2010, 23% had experienced a prior AMI in 2010, 13% 1 year before, 6.7% 5 years before and only 1.2% 12 years before. Thus, the percentage of ‘false positive’ first AMIs, i.e. people identified as ‘first’ who actually did have an AMI 13 years or more before 2010 (and therefore unknown to us), is likely to be very small.
Table 1.
Characteristics of all, first and recurrent AMI events, England, 2010
| Characteristics | All AMI | First AMI |
Recurrent AMI |
||||
|---|---|---|---|---|---|---|---|
| n | All | Fatal |
All | Fatal |
|||
| n | n | All cases (%) | n | n | All cases (%) | ||
| Total | 82 252 | 68 422 | 21 715 | 31.7 | 13 830 | 4334 | 31.3 |
| Type of event | |||||||
| Hospital admission | 63 864 | 52 965 | 6258 | 11.8 | 10 899 | 1403 | 12.9 |
| Sudden AMI death | 18 388 | 15 457 | 15 457 | 100 | 2931 | 2931 | 100 |
| Sex | |||||||
| Male | 50 071 | 41 689 | 12 387 | 29.7 | 8382 | 2593 | 30.9 |
| Female | 32 181 | 26 733 | 9328 | 34.9 | 5448 | 1741 | 32.0 |
| Age | |||||||
| Mean | 72.9 | 72.2 | 77.4 | – | 76.6 | 80.1 | – |
| Median | 75 | 74 | 80 | – | 79 | 82 | – |
| Age group (years) | |||||||
| 0–29 | 147 | 144 | 30 | 20.8 | 3 | 1 | 33.3 |
| 30–54 | 9678 | 8787 | 1251 | 14.2 | 891 | 109 | 12.2 |
| 55–64 | 12 527 | 11 019 | 2109 | 19.1 | 1508 | 271 | 18.0 |
| 65–74 | 17 154 | 14 491 | 3948 | 27.2 | 2663 | 701 | 26.3 |
| 75–84 | 23 711 | 19 092 | 7214 | 37.8 | 4619 | 1557 | 33.7 |
| ≥85 | 19 035 | 14 889 | 7163 | 48.1 | 4146 | 1695 | 40.9 |
| Deprivation | |||||||
| Least deprived, 1 | 17 048 | 14 522 | 4594 | 31.6 | 2526 | 822 | 32.5 |
| 2 | 16 604 | 13 950 | 4355 | 31.2 | 2654 | 851 | 32.1 |
| 3 | 16 265 | 13 467 | 4322 | 32.1 | 2798 | 882 | 31.5 |
| 4 | 16 146 | 13 293 | 4279 | 32.2 | 2853 | 877 | 30.7 |
| Most deprived, 5 | 16 189 | 13 190 | 4165 | 31.6 | 2999 | 902 | 30.1 |
The percentage of all events that were sudden AMI deaths was similar in first and recurrent AMI (23 and 21%, respectively, P < 0.001). The mean ages at first and recurrent AMI were 72 and 77 years, respectively (P < 0.001). The percentage of all AMIs that were reinfarctions was similar between men (16.7%) and women (16.9%). It increased with age in both sexes, from 9% in the age group 30–54 years to 22% in the age group of 85 years and over (test for trend P < 0.001).
Rates of occurrence of AMI events
First AMI
In 2010, there were 68 422 first AMI events in England. Table 2 shows incidence rates of first AMI by age and sex. The incidence of first AMI increased with older age in both men and women. The overall age-standardized incidence of first AMI per 100 000 population was 130 (95% CI 129–131) in men and 55.9 (95% CI 55.3–56.6) in women.
Table 2.
Population-based incidence rates of first acute myocardial infarction (AMI) by sex and age, England, 2010
| Sex | Age (years) | First AMIs, n |
Incidence rate per 100 000 |
||||
|---|---|---|---|---|---|---|---|
| Hospital admissions | Sudden deaths | Total first AMIs | Hospital admissions | Sudden deaths | Overall | ||
| Men | 0–29 | 86 | 19 | 105 | 0.0 | 0.2 | 1.0 |
| 30–34 | 106 | 17 | 123 | 0.5 | 1.0 | 7.4 | |
| 35–39 | 409 | 53 | 462 | 1.8 | 2.9 | 26 | |
| 40–44 | 1009 | 136 | 1145 | 5.1 | 6.7 | 59 | |
| 45–49 | 1917 | 282 | 2199 | 12.2 | 14.2 | 116 | |
| 50–54 | 2700 | 406 | 3106 | 22.4 | 23.5 | 190 | |
| 55–59 | 3112 | 535 | 3647 | 34.2 | 33.7 | 250 | |
| 60–64 | 3961 | 838 | 4799 | 45.3 | 50.8 | 313 | |
| 65–69 | 3633 | 967 | 4600 | 64.1 | 73.9 | 392 | |
| 70–74 | 3940 | 1134 | 5074 | 111 | 103 | 524 | |
| 75–79 | 3939 | 1387 | 5326 | 172 | 162 | 711 | |
| 80–84 | 3632 | 1493 | 5125 | 292 | 245 | 998 | |
| 85–89 | 2741 | 1291 | 4032 | 442 | 384 | 1450 | |
| 90+ | 1305 | 641 | 1946 | 525 | 457 | 1692 | |
| All ages | 32 490 | 9199 | 41 689 | 24.2 | 23.8 | 130 | |
| Women | 0–29 | 37 | 2 | 38 | 0.0 | 0.0 | 0.4 |
| 30–34 | 37 | 6 | 43 | 0.2 | 0.4 | 2.6 | |
| 35–39 | 84 | 13 | 97 | 0.3 | 0.6 | 5.4 | |
| 40–44 | 264 | 31 | 295 | 0.8 | 1.5 | 15 | |
| 45–49 | 498 | 59 | 557 | 3.1 | 2.8 | 29 | |
| 50–54 | 679 | 81 | 760 | 4.1 | 4.4 | 45 | |
| 55–59 | 889 | 112 | 1001 | 7.6 | 6.7 | 66 | |
| 60–64 | 1342 | 230 | 1572 | 12.4 | 12.6 | 98 | |
| 65–69 | 1690 | 355 | 2045 | 24.4 | 24.0 | 162 | |
| 70–74 | 2237 | 535 | 2772 | 48.4 | 43.0 | 256 | |
| 75–79 | 2946 | 879 | 3825 | 83.1 | 78.8 | 416 | |
| 80–84 | 3578 | 1238 | 4816 | 145 | 139 | 651 | |
| 85–89 | 3531 | 1514 | 5045 | 257 | 241 | 982 | |
| 90+ | 2663 | 1203 | 3866 | 341 | 323 | 1329 | |
| All ages | 20 475 | 6258 | 26 733 | 10.1 | 9.6 | 55.9 | |
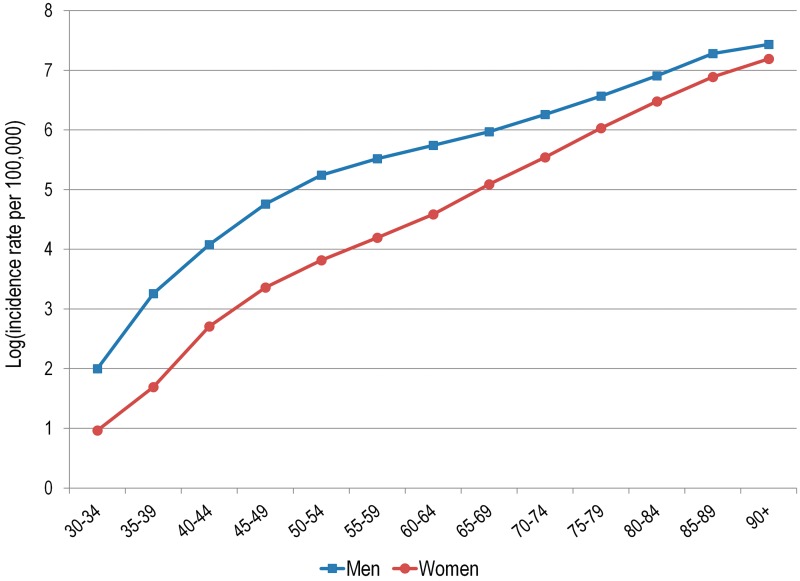
In all age groups, the incidence rate was higher in men than in women, including the very elderly. However, the difference between sexes in their age-specific rates decreased markedly with increasingly older age. Figure 1 illustrates the closing gap in AMI incidence rates between increasingly older men and women. The incidence rate ratio (RR) of first AMI in men compared with women was highest in the 35–39 years age group (RR = 4.80, 95% CI 3.86–5.98) and declined to its lowest in the age group of ≥90 years (RR = 1.27, 95% CI 1.21–1.34).
Figure 1.
Age-specific population-based incidence rates of first AMI on a logarithmic scale by sex, England, 2010
Recurrent AMI
The annual age-standardized AMI recurrence rate per 100 000 population was 24.2 (95% CI 23.7–24.9) in men and 10.1 (95% CI 9.8–10.4) in women. The recurrence rate per 1000 individuals with history of a prior AMI was 34.0 (95% CI 33.3–34.7) in men and 34.3 (95% CI 33.4–35.2) in women.
All AMI
The annual age-standardized event rate of all AMI (first and recurrent) per 100 000 population was 174 (95% CI 173–176) in men and 73.7 (95% CI 72.9–74.5) in women.
Overall 30-day case fatality
All AMI
Of 26 049 fatal AMIs in 2010, 71% were sudden AMI deaths. The percentage of sudden AMI deaths was higher in men than women (74 vs. 67%; P < 0.001) and higher for first AMIs than reinfarctions (71 vs. 68%; P < 0.001). Individuals who died suddenly from AMI without hospitalization for AMI were, on average, 5 years older than hospitalized AMI patients (77 vs. 72 years; P < 0.001).
For both men and women, and for both first and recurrent AMI, the overall case fatality was lowest in the middle ages and increased with older age. The age-adjusted overall 30-day CFRs for men and women, respectively, were 32.4% (95% CI 32.0–32.9) and 30.3% (95% CI 29.8–30.9) for first AMI and 29.7% (95% CI 28.7–30.7) and 26.7% (95% CI 25.5–27.9) for reinfarctions.
For all AMI, multivariate logistic regression was used to investigate the effects of age, sex, deprivation category and history of a previous AMI event on overall 30-day case fatality (Table 3, first column). Age was the strongest predictor of death within 30 days of an AMI event (e.g. comparing the age group >85 years with the age group of 30–54 years: OR = 5.91, 95% CI 5.53–6.32). Men fared slightly worse than women (OR = 1.12, 95% CI 1.09–1.16). A history of previous AMI was a significant factor with a small protective effect (OR = 0.82, 95% CI 0.79–0.85). Individuals in the most deprived quintile were at higher risk than those in the least deprived quintile (OR = 1.21, 95% CI 1.16–1.27).
Table 3.
Overall 30-day case fatality for all, first and recurrent AMI events, and hospitalized 30-day case fatality for all AMI events: results of logistic regression analysis, England, 2010
| Factors | Overall case fatality, all AMI (n = 82 252) | Overall case fatality, first AMI (n = 68 422) | Overall case fatality, recurrent AMI (n = 13 830) | Hospitalized case fatality, all AMI (n = 63 864) |
|---|---|---|---|---|
| ORa (95% CI) | ORa (95% CI) | ORa (95% CI) | ORa (95% CI) | |
| Age | ||||
| 30–54 | Ref. | Ref. | Ref. | Ref. |
| 55–64 | 1.47 (1.36–1.58) | 1.45 (1.35–1.57) | 1.59 (1.25–2.02) | 2.04 (1.71–2.43) |
| 65–74 | 2.38 (2.23–2.55) | 2.34 (2.18–2.51) | 2.65 (2.13–3.30) | 4.34 (3.70–5.09) |
| 75–84 | 3.87 (3.63–4.12) | 3.86 (3.61–4.13) | 3.84 (3.11–4.74) | 8.48 (7.27–9.89) |
| ≥85 | 5.91 (5.53–6.32) | 6.05 (5.64–6.48) | 5.40 (4.36–6.69) | 14.56 (12.5–17.0) |
| Sex | ||||
| Women | Ref. | Ref. | Ref. | Ref. |
| Men | 1.12 (1.09–1.16) | 1.11 (1.07–1.15) | 1.20 (1.11–1.30) | 0.97 (0.92–1.02) |
| Deprivation | ||||
| Least deprived, 1 | Ref. | Ref. | Ref. | Ref. |
| 2 | 1.00 (0.95–1.05) | 1.00 (0.95–1.05) | 0.98 (0.87–1.11) | 1.04 (0.96–1.12) |
| 3 | 1.06 (1.01–1.12) | 1.08 (1.02–1.13) | 1.00 (0.89–1.12) | 1.04 (0.96–1.12) |
| 4 | 1.12 (1.07–1.18) | 1.15 (1.09–1.21) | 1.01 (0.89–1.13) | 1.08 (1.00–1.16) |
| Most deprived, 5 | 1.21 (1.16–1.27) | 1.25 (1.18–1.31) | 1.06 (0.94–1.20) | 1.21 (1.12–1.31) |
| History | ||||
| No history of AMI | Ref. | – | – | Ref. |
| Previous AMI event | 0.82 (0.79–0.85) | – | – | 0.87 (0.82–0.93) |
a: OR = odds ratio; adjusted for all other factors shown
First AMI
Multivariate logistic regression analysis of only first events yielded similar results to the analysis of all events (Table 3, comparing second column with first column).
Recurrent AMI
The analysis of only recurrent AMI events showed a stronger effect of male sex than analysis of all events (Table 3, comparing third column with first column). Deprivation was no longer a significant predictor of 30-day case fatality.
Thirty-day case fatality for hospitalized patients
All AMI
The last column in Table 3 shows the results of multivariate logistic regression analysis for 30-day case fatality in hospital admissions for AMI only, i.e. sudden AMI deaths were excluded. Age was a very strong predictor of death (e.g. comparing the age group >85 years with the age group 30–54 years: OR = 14.6, 95% CI 12.5–17.0). Male sex was no longer a significant factor for the risk of dying within 30 days of AMI (OR = 0.97, 95% CI 0.92–1.02). The effects of deprivation and history of previous AMI were similar to those found for the overall case fatality (Table 3, comparing last column with first column).
Within each age group, hospitalized CFRs were less than half of the overall rates. The age-standardized hospitalized 30-day CFR was 12.0% (95% CI 11.6–12.3) for men and 12.3% (95% CI 11.9–12.7) for women.
Discussion
This study provides a comprehensive account of national population-based statistics on the rate of occurrence of first, recurrent and all AMI events in England, with complete enumeration of 30-day case fatality. The results show that three-quarters of all AMIs occur in individuals aged ≥65 years. About one in six AMIs are reinfarctions in both men and women, and this proportion increases with older age. About a third of all AMIs are fatal, with about two-thirds of fatalities manifesting as sudden AMI deaths. CFRs in hospitalized individuals are about half the overall CFRs that include sudden AMI deaths.
Incidence of first AMI
The results show that about 82 000 AMI events occurred in England in 2010. We confirmed the established patterns of a higher incidence in men than women, at all ages including the very elderly and a steep age gradient in both sexes. However, the difference between men and women in age-specific incidence rates decreased with increasingly older age. The findings that around a quarter of all first events were sudden deaths falls within the internationally reported figures.10–13 This large proportion of AMIs that manifest as sudden deaths reinforces the importance of primary coronary prevention.
The age-standardized incidence rates found in this study are lower than previously reported estimates from the MONICA centres in Glasgow and Belfast1 in the 1980s and the Oxford Myocardial Infarction Incidence Study (OXMIS)4 in the 1990s. The results for incidence of first AMI are also lower than the more recent Oxford Vascular Study (OXVASC) rates per 100 000 population of 162 in men and 92 in women in 2002–05.5 The Health Information Network (THIN), a primary care database comprising patient data from general practices across the UK, estimated that in 2005, the incidence of first AMI in England was 230 and 130/100 000 population for men and women, respectively.14 The generalizability and representativeness of results from both OXVASC and THIN can be questioned. OXVASC data comes from an area with lower deprivation than the national average5 and lower CHD prevalence and mortality rates than the rest of England,15 while THIN relies on voluntary participation of general practices and represents only 3% of the UK population.14 Overall, direct comparisons between the results presented in this article and the studies mentioned above are difficult because of differences in methodology and case ascertainment. Furthermore, these published estimates are based on data much earlier than 2010, and the differences are no doubt attributable at least in part to the declining trends in CHD incidence in the UK (and other developed countries), driven by the reductions in coronary risk factors, and, to a lesser extent, improvements in treatment.14,16–21
Case fatality
Our 30-day overall and hospitalized CFRs for AMI in this study were lower than the rates in the 1980s and 1990s reported previously by others,3,4,22,23 but similar to the more recent estimates from OXVASC.5 Our results are in line with the declining trend in AMI CFR in the UK.14,16–18,23 In agreement with previous studies,4,7 we found that two-thirds of fatal AMIs occur as sudden deaths without a record of hospital care for AMI. This finding underscores the importance of both primary and secondary coronary prevention.
It has been shown previously that the effect of sex on short-term case fatality from AMI varies by whether or not sudden out-of-hospital deaths are included. In general, while 30-day CFRs that include sudden out-of-hospital deaths are higher in men than women, CFRs in those who survive long enough to be admitted to hospital are higher in women than men.12,24–29 Our findings confirm this. Our data showed that men have a slightly higher risk than women in overall 30-day case fatality that includes sudden AMI deaths, after adjusting for age, history of a previous event and deprivation. However, women had a slightly higher 30-day hospitalized case fatality. This sex difference has been explained by the fact that, of those who are destined to die soon after AMI, a higher percentage of women than men survive long enough to reach hospital alive, but die shortly afterwards.24
Study strengths and limitations
Strengths of this study include its large size, population-level representation and complete national coverage. The main limitation is the reliance upon the accuracy and validity of routine data. A systematic review of studies comparing routine hospital discharge statistics with medical records done in England, Wales and Scotland reported, on average, high coding accuracy rates.30 In addition, the quality of hospital data varies by condition, and common diagnoses like AMI are less likely to be subject to miscoding than rare ones.31,32 Linked Scottish Morbidity Record Database and Patient Episode Database for Wales, counterparts to English HES in Scotland and Wales, respectively, were reported to have high accuracy rates for the diagnosis of AMI.33,34
Further limitations include the absence of clinical information, making it impossible to adjust for coronary risk factors and infarct severity, or to report on the diagnostic criteria used in making the clinical diagnosis of AMI. Information on previous episodes of AMI was limited to 12 years of prior history and, inevitably, a small proportion of events that were classified as ‘first’ were in fact recurrent. However, a 12-year history is the best that can be done within the current limits of the English national record linkage data set. Some deaths coded with non-AMI CHD as the underlying cause of death—not included in this study—could have been true cases of AMI. It is also possible that some events identified as recurrent might represent admissions for AMI, after our 30-day cut-off, that were in fact still related to the earlier AMI event. Some AMI hospital admissions with a length of stay of 1 day and live discharge or with only a secondary diagnosis of AMI—excluded from this analysis—could have been true instances of AMI. Notwithstanding the limitations, the presented results are in line with earlier British estimates and are likely to reflect the current situation in England well.
Conclusions
Our study provides recent information about AMI incidence and short-term prognosis in England, distinguishing between first and recurrent events. In particular, it indicates that individuals aged ≥65 years bear most of the population burden of AMI; reinfarctions are relatively common; and overall 30-day CFRs that include sudden AMI deaths are more than twice as high as hospitalized rates, indicating that the clinical prognosis for those who survive long enough to be admitted to hospital is much better than overall prognosis. Our findings reinforce the importance of primary and secondary prevention in reducing AMI morbidity and mortality. More generally, national statistics such as those presented in this article, based on record linkage, can be produced as a routine for a wide range of diseases. Nowadays, the data exist, the data processing technologies are cheap and reliable and comparable information about population health and health care can become readily available.
Funding
The Rhodes Trust (to K.S.); the Medical Research Council (to L.W.); the British Heart Foundation (to M.R.); the National Institute for Health Research (to M.G., partial).
Conflict of interest: None declared.
Key points.
This study provides a comprehensive account of national population-based statistics on the rate of occurrence of first, recurrent and all AMI in England, with complete enumeration of 30-day hospitalized and overall case fatality.
The findings show that around 82 000 AMI events occurred in England in 2010, and that around one in six was a reinfarction rather than a first AMI.
Overall CFRs, which include sudden AMI deaths, are more than double the rates in analyses confined to patients hospitalized for AMI.
The results reinforce the importance of primary and secondary prevention in reducing AMI morbidity and mortality.
Acknowledgements
Leicester Gill and Matt Davidson from the Unit of Health-Care Epidemiology built the linked file and performed the extraction of data for analysis.
References
- 1.Tunstall-Pedoe H, Kuulasmaa K, Mähönen M, et al. Contribution of trends in survival and coronary event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA Project populations. Lancet. 1999;353:1547–57. doi: 10.1016/s0140-6736(99)04021-0. [DOI] [PubMed] [Google Scholar]
- 2.Thygesen K, Alpert JS, White HD, Force EAAWT. Universal definition of myocardial infarction. Circulation. 2007;116:2634–53. doi: 10.1161/CIRCULATIONAHA.107.187397. [DOI] [PubMed] [Google Scholar]
- 3.Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, et al. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90:583–612. doi: 10.1161/01.cir.90.1.583. [DOI] [PubMed] [Google Scholar]
- 4.Volmink JA, Newton JN, Hicks NR, et al. Coronary event and case fatality rates in an English population: results of the Oxford myocardial infarction incidence study. Heart. 1998;80:40–4. doi: 10.1136/hrt.80.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rothwell P, Coull A, Silver L, et al. Population-based study of event rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study) Lancet. 2005;366:1773–83. doi: 10.1016/S0140-6736(05)67702-1. [DOI] [PubMed] [Google Scholar]
- 6.Morris R, Whincup P, Lampe F, et al. Geographic variation in incidence of coronary heart disease in Britain: the contribution of established risk factors. Heart. 2001;86:277–83. doi: 10.1136/heart.86.3.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Norris R. Fatality outside hospital from acute coronary events in three British health districts, 1994–5. BMJ. 1998;316:1065–70. [PMC free article] [PubMed] [Google Scholar]
- 8.Gill L, Goldacre M. Oxford: National Centre for Health Outcomes Development, Unit of Health-Care Epidemiology, University of Oxford; 2003. English National Record Linkage of Hospital Episode Statistics and Death Registration Records. [Google Scholar]
- 9.Office of the Deputy Prime Minister. London: Office of the Deputy Prime Minister; 2004. The English Indices of Deprivation 2004: Summary (revised) [Google Scholar]
- 10.Marshall RJ, Milne RJ, Lynn R, Jackson R. Quantifying the effect of age on short-term and long-term case fatality in 14 000 patients with incident cases of cardiovascular disease. Eur J Cardiovasc Prev Rehabil. 2008;15:179–84. doi: 10.1097/HJR.0b013e3282f14a7f. [DOI] [PubMed] [Google Scholar]
- 11.Salomaa V, Miettinen H, Kuulasmaa K, et al. Decline of coronary heart disease mortality in Finland during 1983 to 1992: roles of incidence, recurrence, and case-fatality: the FINMONICA MI Register Study. Circulation. 1996;94:3130–7. doi: 10.1161/01.cir.94.12.3130. [DOI] [PubMed] [Google Scholar]
- 12.Rosengren A, Spetz CL, Koster M, et al. Sex differences in survival after myocardial infarction in Sweden - data from the Swedish National Acute Myocardial Infarction Register. Eur Heart J. 2001;22:314–22. doi: 10.1053/euhj.2000.2368. [DOI] [PubMed] [Google Scholar]
- 13.Adnet F, Renault R, Jabre P, et al. Incidence of acute myocardial infarction resulting in sudden death outside the hospital. Emerg Med J. 2010;10:884–6. doi: 10.1136/emj.2010.095885. [DOI] [PubMed] [Google Scholar]
- 14.Davies A, Grundy E, Nitsch D, Smeeth L. Constituent country inequalities in myocardial infarction incidence and case fatality in men and women in the United Kingdom, 1996–2005. J Public Health. 2011;33:131–8. doi: 10.1093/pubmed/fdq049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scarborough P, Allender S, Peto V, Rayner M. London: British Heart Foundation; 2008. Regional and Social Differences in Coronary Heart Disease. [Google Scholar]
- 16.Lampe F, Morris R, Walker M, et al. Trends in rates of different forms of diagnosed coronary heart disease, 1978 to 2000: prospective, population based study of British men. BMJ. 2005;330:1046–51. doi: 10.1136/bmj.330.7499.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davies A, Smeeth L, Grundy E. Contribution of changes in incidence and mortality to trends in the prevalence of coronary heart disease in the UK: 1996–2005. Eur Heart J. 2007;28:2142–7. doi: 10.1093/eurheartj/ehm272. [DOI] [PubMed] [Google Scholar]
- 18.Goldacre M, Roberts S. Report to the Department of Health; 2001. Myocardial infarction: an investigation of measures of mortality, incidence and case fatality. Available at: http://www.uhce.ox.ac.uk/hessepho/reports/MIReport.2001%28a%29.pdf (1 July 2011, date last accessed) [Google Scholar]
- 19.Koek H, De Bruin A, Gast A, et al. Decline in incidence of hospitalisation for acute myocardial infarction in the Netherlands from 1995 to 2000. BMJ. 2006;92:162–5. doi: 10.1136/hrt.2004.054486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuulasmaa K, Tunstall-Pedoe H, Dobson A, et al. Estimation of contribution of changes in classic risk factors to trends in coronary-event rates across the WHO MONICA Project populations. Lancet. 2000;355:675–87. doi: 10.1016/s0140-6736(99)11180-2. [DOI] [PubMed] [Google Scholar]
- 21.Rosen M, Alfredsson L, Hammar N, et al. Attack rate, mortality and case fatality for acute myocardial infarction in Sweden during 1987-95. Results from the national AMI register in Sweden. J Intern Med. 2000;248:159–64. doi: 10.1046/j.1365-2796.2000.00716.x. [DOI] [PubMed] [Google Scholar]
- 22.Chambless L, Keil U, Dobson A, et al. Population versus clinical view of case fatality from acute coronary heart disease: results from the WHO MONICA Project 1985–1990. Circulation. 1997;96:3849–59. doi: 10.1161/01.cir.96.11.3849. [DOI] [PubMed] [Google Scholar]
- 23.Capewell S, Livingston BM, MacIntyre K, et al. Trends in case-fatality in 117 718 patients admitted with acute myocardial infarction in Scotland. Eur Heart J. 2000;21:1833–40. doi: 10.1053/euhj.2000.2318. [DOI] [PubMed] [Google Scholar]
- 24.Tunstall-Pedoe H, Morrison C, Woodward M, et al. Sex differences in myocardial infarction and coronary deaths in the Scottish MONICA population of Glasgow 1985 to 1991 - presentation, diagnosis, treatment, and 28-day case fatality of 3991 events in men and 1551 events in women. Circulation. 1996;93:1981–92. doi: 10.1161/01.cir.93.11.1981. [DOI] [PubMed] [Google Scholar]
- 25.Vaccarino V, Parsons L, Every NR, et al. Sex-based differences in early mortality after myocardial infarction. N Engl J Med. 1999;341:217–25. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- 26.Hanratty B, Lawlor DA, Robinson MB, et al. Sex differences in risk factors, treatment and mortality after acute myocardial infarction: an observational study. JECH. 2000;54:912–6. doi: 10.1136/jech.54.12.912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.MacIntyre K, Stewart S, Capewell S, et al. Gender and survival: a population-based study of 201,114 men and women following a first acute myocardial infarction. J Am Coll Cardiol. 2001;38:729–35. doi: 10.1016/s0735-1097(01)01465-6. [DOI] [PubMed] [Google Scholar]
- 28.Tu JV, Austin PC, Filate WA, et al. Outcomes of acute myocardial infarction in Canada. Can J Cardiol. 2003;19:893–901. [PubMed] [Google Scholar]
- 29.Milcent C, Dormont B, Durand-Zaleski I, Steg PG. Gender differences in hospital mortality and use of percutaneous coronary intervention in acute myocardial infarction - microsimulation analysis of the 1999 nationwide French hospitals database. Circulation. 2007;115:833–9. doi: 10.1161/CIRCULATIONAHA.106.664979. [DOI] [PubMed] [Google Scholar]
- 30.Campbell SE, Campbell MK, Grimshaw JM, Walker AE. A systematic review of discharge coding accuracy. J Public Health Med. 2001;23:205–11. doi: 10.1093/pubmed/23.3.205. [DOI] [PubMed] [Google Scholar]
- 31.Dixon J, Sanderson C, Elliott P, et al. Assessment of the reproducibility of clinical coding in routinely collected hospital activity data: a study in two hospitals. J Public Health Med. 1998;20:63–9. doi: 10.1093/oxfordjournals.pubmed.a024721. [DOI] [PubMed] [Google Scholar]
- 32.Aylin P, Lees T, Baker S, et al. Descriptive study comparing routine hospital administrative data with the vascular society of Great Britain and Ireland's National Vascular Database. Eur J Vasc Endovasc Surg. 2007;33:461–5. doi: 10.1016/j.ejvs.2006.10.033. [DOI] [PubMed] [Google Scholar]
- 33.Harley K, Jones C. Quality of Scottish Morbidity Record (SMR) data. Health Bull. 1996;54:410–7. [PubMed] [Google Scholar]
- 34.Brophy S, Cooksey R, Gravenor M, et al. Population based absolute and relative survival to 1 year of people with diabetes following a myocardial infarction: a cohort study using hospital admissions data. BMC Public Health. 2010;10:338–45. doi: 10.1186/1471-2458-10-338. [DOI] [PMC free article] [PubMed] [Google Scholar]