Abstract
Anorexia/cachexia is a common and currently mostly untreatable complication of advanced cancer. It is also a feature of a number of chronic diseases and can also occur as part of the normal ageing process. Over recent years, two different, but sometimes overlapping, processes have been identified to mediate anorexia/cachexia: those that act primarily on muscle reducing its mass and function, and processes that decrease nutrition leading to loss of both fat and muscle. In the case of at least some cancers, the latter process is sometimes driven by marked overexpression of macrophage inhibitory cytokine-1/growth differentiation factor 15 (MIC-1/GDF15). MIC-1/GDF15 is a transforming growth factor beta (TGF-β) family cytokine that is found in the serum of all normal individuals at an average concentration of about 0.6 ng/ml. Its increased expression in both cancers and other diseases can result in 10–100-fold or more elevation of its serum levels. In experimental animals, serum MIC-1/GDF15 levels at the lower end of this range induce anorexia by direct actions of the circulating cytokine on feeding centres in the brain. Mice with tumours overexpressing MIC-1/GDF15 display decreased food intake, loss of lean and fat mass and cachexia. That this process also mediates anorexia/cachexia in humans is suggested by the fact that there is a direct correlation between the degree of serum MIC-1/GDF15 elevation and the amount of cancer-related weight loss, the first such relationship demonstrated. Further, in experimental animals, weight loss can be reversed by neutralisation of tumour-produced MIC-1/GDF15 with a specific monoclonal antibody, suggesting the possibility of effective therapy of patients with the devastating complication of anorexia/cachexia.
Keywords: MIC-1/GDF15, Macrophage inhibitory cytokine 1, Anorexia, Cachexia, TGF-β, Appetite regulation
Introduction
Worldwide, anorexia/cachexia is a common problem due to inadequate nutrition or as a complication of a number of chronic disease states and ageing. In the developing world, inadequate nutrition causes cachexia [1] and eventually death in many individuals. In the developed world, undernutrition and consequent cachexia is usually seen as part of a disease process. Examples include coeliac disease, leading to reduced nutrient absorption and anorexia nervosa, where reduced intake leads to loss of fat and lean mass and often cachexia [2, 3]. However in some diseases, most notably advanced cancers, mediators produced directly or indirectly by the tumour may cause anorexia and eventually cachexia. Cancer anorexia/cachexia shortens life, causes great morbidity, limits therapy and is responsible for about one quarter of cancer deaths. The aetiological factors contributing to the development of the anorexia/cachexia syndrome fall into two broad and sometimes overlapping groups: factors that greatly decreased energy availability and/or those that primarily lead to loss of muscle mass. Whilst the latter has been most closely investigated, in more recent times, it has become clear that anorexia, driving loss of muscle mass, is also an important aetiological factor, especially in cancer anorexia/cachexia. This review will focus on the role of decreased energy intake in the aetiology of this syndrome and in particular on the role of the transforming growth factor beta (TGF-β) superfamily cytokine, macrophage inhibitory cytokine-1/growth differentiation factor 15 (MIC-1/GDF15), in mediating this process.
Overview of appetite regulation
Mammals have evolved a complex system to regulate food intake and maintain appropriate energy stores, dominantly in the form of fat and carbohydrates. Meal size is controlled by short-term hormonal and neural signals that are derived from the gut or pancreas, such as ghrelin, which initiates meals [4], and cholecystokinin, glucagon-like peptide-1, amylin and peptide YY [5, 6], which are satiety factors. Many of these act via the area postrema (AP) and nucleus tractus solitarus in the brainstem, as well as via the hypothalamus. Whilst circulating mediators are excluded from the majority of the CNS because of the specialised tight junctions of the blood–brain barrier, they do access a limited number of circumventricular organs that lack these tight junctions. These circumventricular organs can be found in the median eminence, which is immediately adjacent to the arcuate nucleus (Arc) of the hypothalamus and the AP. Thus, systemic hormones like insulin and leptin, together with circulating nutrients, can act on these areas to modulate multiple CNS pathways that then converge on the hypothalamus to influence food intake [7] and regulate long-term energy stores. For example, energy deficiency activates powerful hypothalamic pathways involving increased expression and secretion of neuropeptide Y (NPY) that increase appetite and decrease energy expenditure [8]. Energy deficit also leads to decreased brain levels of alpha-melanocyte-stimulating hormone (α-MSH, a cleavage product of proopiomelanocortin (POMC)) and cocaine–amphetamine-related transcript, which oppose NPY actions [9].
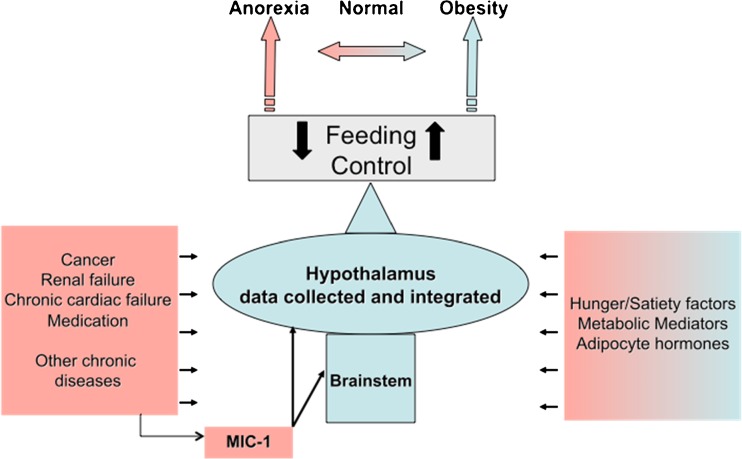
Regulation of energy homeostasis is a complex and tightly controlled process. However, it can also be modulated by food availability and disease processes leading to either obesity or severe weight loss and cachexia (Fig. 1). One molecule that is both overexpressed in disease and capable of modulating appetite is the TGF-β superfamily cytokine, MIC-1/GDF15 [10].
Fig. 1.
Overview of systemic physiological and disease-related factors regulating appetite and body mass
MIC-1/GDF15 in appetite regulation and anorexia/cachexia
MIC-1/GDF15 is a 25-kDa disulphide-linked dimeric stress response protein [11] that is present in the circulation of all individuals with a normal range of 150–1,150 pg/ml [12, 13]. Whilst its major site of synthesis is probably the liver, it is also expressed in small amounts in the lungs, kidneys and adipose tissue. In addition to this basal production, its expression is increased in most cells and tissues by inflammation, injury and malignancy [14]. Many cancers secrete large amounts of MIC-1/GDF15 [15, 16], and biological, genetic and in vitro data implicate it in cancer progression and outcome [14, 16, 17]. For example, metastatic tumours of the prostate, breast and colon markedly overexpress MIC-1/GDF15, resulting in large increases in its serum levels, sometimes to over 100,000 pg/ml [15]. Additionally, there are diagnostically useful relationships between serum MIC-1/GDF15 levels and many cancers, including those of the colon [18], prostate gland [19–21] and pancreas [22, 23]. Further, MIC-1/GDF15 can modify tumour behaviour in vivo and in vitro (reviewed in [14, 16, 17]). Our studies also indicate that elevated serum MIC-1/GDF15, at least in some cases, directly causes cancer anorexia/cachexia, as outlined below.
Experimental data from animal models
We discovered that mice xenografted with tumours overexpressing MIC-1/GDF15 became cachectic [10], with the degree of weight loss proportional to the elevation of serum MIC-1/GDF15 levels. Further, this weight loss could be completely reversed by monoclonal antibodies to MIC-1/GDF15 and reproduced by direct injection of recombinant MIC-1/GDF15 subcutaneously. In these mice, the minimum MIC-1/GDF15 serum concentrations associated with weight loss was about 5 ng/ml, well within the serum level range seen in patients with advanced cancer. Consistent with these findings, transgenic mice overexpressing MIC-1/GDF15 weigh less than [10, 24, 25], and MIC-1/GDF15 germline gene deleted mice weigh more, than their syngeneic controls [26].
In cancer models, and when recombinant MIC-1/GDF15 was administered, weight loss was due to decreased food intake rather than to altered metabolism, as indicated by pair-feeding experiments involving restricting the food intake of a cohort of normal mice to that of syngeneic mice treated with MIC-1/GDF15 [10]. Pair-feeding of normal mice resulted in similar weight loss, with similar changes in both fat and lean mass, as that produced by recombinant MIC-1/GDF15 administration [10]. This experiment demonstrates that similar changes in body weight and muscle mass occur when the food intake of normal mice is reduced to that of MIC-1/GDF15 treated mice. Thus, the loss of muscle mass in MIC-1/GDF15-treated mice can be fully accounted for by reduced food intake, without incriminating a direct action of MIC-1/GDF15 on muscle. Additionally, overexpression of MIC-1/GDF15 in mice did not result in any reduction in energy expenditure as determined by indirect calorimetry [10], further highlighting the importance of reduced food intake to the associated reduction in body weight, adiposity and muscle mass. However, mice bearing tumours overexpressing MIC-1/GDF15 also displayed a number of other metabolic alterations; all of which were consistent with reduced food intake. These included reductions in serum levels of glucose, free fatty acids and triglycerides, leptin and IGF-1 [10]. Even in the face of reduced leptin levels, reflecting reduced fat mass and associated increased drive to eat, MIC-1/GDF15 was still able to reduce food intake. IGF-1 is an important regulator of lean mass whose serum levels are reduced by MIC-1/GDF15 tumour expression as well as by energy restriction [27–30]. IGF-1 is known to be low in cancer anorexia/cachexia, and a reduction in serum IGF-1 levels with energy deficit is likely to be one of the mechanisms mediating reduction in muscle mass under these circumstances.
Consistent with its anorexigenic actions, systemic administration of MIC-1/GDF15 activated neurons in three brain regions associated with appetite regulation: the AP, Arc and the hypothalamic paraventricular nucleus [10], two of which have a permeable capillary bed allowing systemic mediators direct access to the otherwise tightly shielded brain. Further, direct Arc injection of adeno-associated virus overexpressing MIC-1/GDF15 also resulted in decreased food intake, body weight and local neuronal activation, similar to the effects of the systemically administered cytokine. To further elucidate the mechanisms of action of MIC-1/GDF15, we have studied its effects on the Arc in more detail. Systemic injection of MIC-1/GDF15 decreased the Arc expression of the major appetite stimulatory factor NPY and increased that of the opposing anorexigenic factor, POMC. Both of these changes could contribute to hypophagia resulting from MIC-1/GDF15 administration. The major anorexigenic cleavage product of POMC is α-MSH, the ligand for the melanocortin 4 receptor, a major pathway also utilised by leptin, one of the most important identified appetite-suppressant molecules. Whilst the TGF-β superfamily receptor complex responsible for mediating the actions of MIC-1/GDF15 has not been definitively identified, our studies, subsequently supported by others, suggested that MIC-1/GDF15 utilises the TGF-β RII receptor [31, 32] and activates both ERK and STAT3 pathways.
Data from humans studies
There are strong experimental data in animals to indicate that, when expressed in amounts comparable to those seen in human malignancies and other chronic diseases, MIC-1/GDF15 is able to suppress appetite and induce cachexia. To obtain direct evidence for the relevance of MIC-1/GDF15 to anorexia/cachexia in human disease, we have studied serum from a number of patient cohorts. We measured serum levels of MIC-1/GDF15 in a cohort of patients with advanced prostate cancer, originally studied to determine the role of TNF, IL-1 and IL6 in anorexia/cachexia [33]. In these patients, the degree of weight loss over a 6-month period was strongly correlated with prospectively collected serum MIC-1/GDF15 levels [10]. There was no such correlation with the other measured cytokines, although serum levels of IL6, TNF-α and IL8 were higher in the cachectic subjects [33]. Whilst these data have also been validated in a second cohort of patients with advanced prostate cancer [20], no relationship of MIC-1/GDF15 serum levels to nutritional status could be identified in patients with oesophago-gastric cancer, perhaps because of the overriding effect of gastrointestinal disruption [34]. However, in end-stage renal failure, a condition in which MIC-1/GDF15 serum levels can rise to up to 25 ng/ml, increasing serum levels of MIC-1/GDF15 were also associated with reduced body mass index (BMI) in 381 patients with end-stage renal failure on dialysis [10]. Further, in a separate cohort of 98 patients with end-stage renal failure, prior to dialysis, serum MIC-1/GDF15 levels were able to identify patients with protein-energy wasting [35]. Another condition in which serum levels of MIC-1/GDF15 can rise substantially is chronic heart failure [36]. In a paper identifying a role for MIC-1/GDF15 as a marker of chronic heart failure severity, we can also see that the group with the highest MIC-1/GDF15 levels have the lowest BMI [36]. Thus, whilst pathogenic mechanisms have not been directly identified in humans, across a number of diseases where serum levels of MIC-1/GDF15 are elevated, there appears to be a consistent correlation between increase in its serum levels and decrease in markers of nutrition.
To the best of our knowledge, MIC-1/GDF15 is the only putative causative agent for cancer anorexia/cachexia for which it has been possible to identify a direct correlation between its increasing serum levels and measures of body mass. In conjunction with strong data in experimental animals indicating anorexigenic actions for MIC-1/GDF15, the elevated serum concentrations of MIC-1/GDF15 seen in certain human diseases suggest that MIC-1/GDF15 is a cause of anorexia/cachexia. It is unlikely however that it is the only cause. Human studies using antibodies to MIC-1/GDF15, targeted to patients with elevated MIC-1/GDF15 serum levels and early cachexia, will be required to both unequivocally prove the role of this molecule in human disease and determine whether targeting this molecule is an effective therapeutic strategy.
Does MIC-1/GDF15 play a role in physiological appetite regulation?
The relationship of elevated serum MIC-1/GDF15 levels to food intake and body mass raises the question as to whether its levels, in the normal physiological range, play a role in regulating food intake, body weight or metabolism. Currently, there is little direct evidence available to allow any conclusions to be drawn, and what little evidence available is difficult to interpret. However, MIC-1/GDF15 gene knockout mice weigh more that syngeneic wild-type mice [26]. In humans, defining any relationship between obesity or BMI and serum MIC-1 concentrations is complicated by a number of other potential modulators of its serum levels. Its serum levels, within the normal range, are higher in obesity perhaps because it is an adipokine or because of its production by inflammatory cells that commonly reside within fat tissues [37, 38]. Further, obesity is associated with insulin resistance, which also raises MIC-1/GDF15 serum levels [37, 38].
Conclusion
The aetiology of anorexia/cachexia of cancer is multifactorial. At the very least, it involves aetiological factors like depression, side effects of cancer therapy and mechanical disruption to the gastrointestinal tract. It is also likely to involve mediators that are secreted by either tumour cells or other cells in the tumour microenvironment. These may include anorexigenic proteins like MIC-1/GDF15, cytokines whose primary action is on the muscle such as myostatin and perhaps some pro-inflammatory cytokines like IL6 and TNF-α. However, despite a rapidly growing understanding of pathways capable of causing anorexia/cachexia in experimental animals, there is very limited evidence as to which pathways are triggered in patients with disease processes associated with this complication. Ideally, whatever the putative mediator, one would expect to be able to demonstrate: (1) similar serum levels in disease to those able to induce anorexia/cachexia in experimental animals and (ii) a correlation, in patients, between its serum levels and parameters of anorexia/cachexia. Ultimately, however, the best test of the importance of the putative mediator will be that its removal or inhibition in human disease will reverse anorexia/cachexia.
Acknowledgments
This work was supported in part by the National Health and Medical Research Council of Australia (NHMRC). DAB is supported by an NHMRC fellowship. The authors of this manuscript certify that they comply with the ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle [39].
Conflict of interest
Prof. Breit and Dr. Brown are inventors on patents owned by St Vincent’s Hospital, which identify a role for MIC-1/GDF15 in therapy of anorexia/cachexia.
Footnotes
David A. Brown and Samuel N. Breit contributed equally to this work.
References
- 1.Barac-Nieto M, Spurr GB, Lotero H, Maksud MG. Body composition in chronic undernutrition. Am J Clin Nutr. 1978;31:23–40. doi: 10.1093/ajcn/31.1.23. [DOI] [PubMed] [Google Scholar]
- 2.Barera G, Mora S, Brambilla P, Ricotti A, Menni L, Beccio S, et al. Body composition in children with celiac disease and the effects of a gluten-free diet: a prospective case–control study. Am J Clin Nutr. 2000;72:71–75. doi: 10.1093/ajcn/72.1.71. [DOI] [PubMed] [Google Scholar]
- 3.Kooh SW, Noriega E, Leslie K, Muller C, Harrison JE. Bone mass and soft tissue composition in adolescents with anorexia nervosa. Bone. 1996;19:181–188. doi: 10.1016/8756-3282(96)00162-7. [DOI] [PubMed] [Google Scholar]
- 4.Yoshihara F, Kojima M, Hosoda H, Nakazato M, Kangawa K. Ghrelin: a novel peptide for growth hormone release and feeding regulation. Curr Opin Clin Nutr Metab Care. 2002;5:391–395. doi: 10.1097/00075197-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Stanley S, Wynne K, McGowan B, Bloom S. Hormonal regulation of food intake. Physiol Rev. 2005;85:1131–1158. doi: 10.1152/physrev.00015.2004. [DOI] [PubMed] [Google Scholar]
- 6.Lutz TA. The role of amylin in the control of energy homeostasis. Am J Physiol Regul Integr Comp Physiol. 2010;298:R1475–R1484. doi: 10.1152/ajpregu.00703.2009. [DOI] [PubMed] [Google Scholar]
- 7.Kishi T, Elmquist JK. Body weight is regulated by the brain: a link between feeding and emotion. Mol Psychiatry. 2005;10:132–146. doi: 10.1038/sj.mp.4001638. [DOI] [PubMed] [Google Scholar]
- 8.Herzog H. Neuropeptide Y and energy homeostasis: insights from Y receptor knockout models. Eur J Pharmacol. 2003;480:21–29. doi: 10.1016/j.ejphar.2003.08.089. [DOI] [PubMed] [Google Scholar]
- 9.Kalra SP, Dube MG, Pu S, Xu B, Horvath TL, Kalra PS. Interacting appetite-regulating pathways in the hypothalamic regulation of body weight. Endocr Rev. 1999;20:68–100. doi: 10.1210/er.20.1.68. [DOI] [PubMed] [Google Scholar]
- 10.Johnen H, Lin S, Kuffner T, Brown DA, Tsai VW, Bauskin AR, et al. Tumor-induced anorexia and weight loss are mediated by the TGF-beta superfamily cytokine MIC-1. Nat Med. 2007;13:1333–1340. doi: 10.1038/nm1677. [DOI] [PubMed] [Google Scholar]
- 11.Bootcov MR, Bauskin AR, Valenzuela SM, Moore AG, Bansal M, He XY, et al. MIC-1, a novel macrophage inhibitory cytokine, is a divergent member of the TGF-beta superfamily. Proc Natl Acad Sci USA. 1997;94:11514–11519. doi: 10.1073/pnas.94.21.11514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown DA, Bauskin AR, Fairlie WD, Smith MD, Liu T, Xu N, et al. Antibody-based approach to high-volume genotyping for MIC-1 polymorphism. Biotechniques. 2002;33:118–120. doi: 10.2144/02331rr03. [DOI] [PubMed] [Google Scholar]
- 13.Brown DA, Breit SN, Buring J, Fairlie WD, Bauskin AR, Liu T, et al. Concentration in plasma of macrophage inhibitory cytokine-1 and risk of cardiovascular events in women: a nested case–control study. Lancet. 2002;359:2159–2163. doi: 10.1016/S0140-6736(02)09093-1. [DOI] [PubMed] [Google Scholar]
- 14.Breit SN, Johnen H, Cook AD, Tsai VW, Mohammad MG, Kuffner T, et al. The TGF-beta superfamily cytokine, MIC-1/GDF15: a pleotrophic cytokine with roles in inflammation, cancer and metabolism. Growth Factors. 2011;29:187–195. doi: 10.3109/08977194.2011.607137. [DOI] [PubMed] [Google Scholar]
- 15.Welsh JB, Sapinoso LM, Kern SG, Brown DA, Liu T, Bauskin AR, et al. Large-scale delineation of secreted protein biomarkers overexpressed in cancer tissue and serum. Proc Natl Acad Sci U S A. 2003;100:3410–3415. doi: 10.1073/pnas.0530278100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bauskin AR, Brown DA, Kuffner T, Johnen H, Luo XW, Hunter M, et al. Role of macrophage inhibitory cytokine-1 in tumorigenesis and diagnosis of cancer. Cancer Res. 2006;66:4983–4986. doi: 10.1158/0008-5472.CAN-05-4067. [DOI] [PubMed] [Google Scholar]
- 17.Brown DA, Bauskin A, Breit SN. MIC-1. In: Schwab, Manfred, editors. Encyclopedia of Cancer. 3rd ed. Berlin: Springer; 2012.
- 18.Brown DA, Ward RL, Buckhaults P, Liu T, Romans KE, Hawkins NJ, et al. MIC-1 serum level and genotype: associations with progress and prognosis of colorectal carcinoma. Clin Cancer Res. 2003;9:2642–2650. [PubMed] [Google Scholar]
- 19.Brown DA, Stephan C, Ward RL, Law M, Hunter M, Bauskin AR, et al. Measurement of serum levels of macrophage inhibitory cytokine 1 combined with prostate-specific antigen improves prostate cancer diagnosis. Clin Cancer Res. 2006;12:89–96. doi: 10.1158/1078-0432.CCR-05-1331. [DOI] [PubMed] [Google Scholar]
- 20.Wakchoure S, Swain TM, Hentunen TA, Bauskin AR, Brown DA, Breit SN, et al. Expression of macrophage inhibitory cytokine-1 in prostate cancer bone metastases induces osteoclast activation and weight loss. Prostate. 2009;69:652–661. doi: 10.1002/pros.20913. [DOI] [PubMed] [Google Scholar]
- 21.Bauskin AR, Brown DA, Junankar S, Rasiah KK, Eggleton S, Hunter M, et al. The propeptide mediates formation of stromal stores of PROMIC-1: role in determining prostate cancer outcome. Cancer Res. 2005;65:2330–2336. doi: 10.1158/0008-5472.CAN-04-3827. [DOI] [PubMed] [Google Scholar]
- 22.Koopmann J, Rosenzweig CN, Zhang Z, Canto MI, Brown DA, Hunter M, et al. Serum markers in patients with resectable pancreatic adenocarcinoma: macrophage inhibitory cytokine 1 versus CA19-9. Clin Cancer Res. 2006;12:442–446. doi: 10.1158/1078-0432.CCR-05-0564. [DOI] [PubMed] [Google Scholar]
- 23.Koopmann J, Buckhaults P, Brown DA, Zahurak ML, Sato N, Fukushima N, et al. Serum macrophage inhibitory cytokine 1 as a marker of pancreatic and other periampullary cancers. Clin Cancer Res. 2004;10:2386–2392. doi: 10.1158/1078-0432.CCR-03-0165. [DOI] [PubMed] [Google Scholar]
- 24.Baek SJ, Okazaki R, Lee SH, Martinez J, Kim JS, Yamaguchi K, et al. Nonsteroidal anti-inflammatory drug-activated gene-1 over expression in transgenic mice suppresses intestinal neoplasia. Gastroenterology. 2006;131:1553–1560. doi: 10.1053/j.gastro.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 25.Macia L, Tsai VW, Nguyen AD, Johnen H, Kuffner T, Shi YC, et al. Macrophage inhibitory cytokine 1 (MIC-1/GDF15) decreases food intake. Body weight and improves glucose tolerance in mice on normal & obesogenic diets. PLoS One. 2012;7:e34868. doi: 10.1371/journal.pone.0034868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Strelau J, Strzelczyk A, Rusu P, Bendner G, Wiese S, Diella F, et al. Progressive postnatal motoneuron loss in mice lacking GDF-15. J Neurosci. 2009;29:13640–13648. doi: 10.1523/JNEUROSCI.1133-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tovar AR, Halhali A, Torres N. Effect of nutritional rehabilitation of undernourished rats on serum insulin-like growth factor (IGF)-I and IGF-binding proteins. Rev Invest Clin. 1999;51:99–106. [PubMed] [Google Scholar]
- 28.De Pergola G, Zamboni M, Pannacciulli N, Turcato E, Giorgino F, Armellini F, et al. Divergent effects of short-term, very-low-calorie diet on insulin-like growth factor-I and insulin-like growth factor binding protein-3 serum concentrations in premenopausal women with obesity. Obes Res. 1998;6:408–415. doi: 10.1002/j.1550-8528.1998.tb00372.x. [DOI] [PubMed] [Google Scholar]
- 29.Smith WJ, Underwood LE, Clemmons DR. Effects of caloric or protein restriction on insulin-like growth factor-I (IGF-I) and IGF-binding proteins in children and adults. J Clin Endocrinol Metab. 1995;80:443–449. doi: 10.1210/jc.80.2.443. [DOI] [PubMed] [Google Scholar]
- 30.Fontana L, Weiss EP, Villareal DT, Klein S, Holloszy JO. Long-term effects of calorie or protein restriction on serum IGF-1 and IGFBP-3 concentration in humans. Aging Cell. 2008;7:681–687. doi: 10.1111/j.1474-9726.2008.00417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kempf T, Zarbock A, Widera C, Butz S, Stadtmann A, Rossaint J, et al. GDF-15 is an inhibitor of leukocyte integrin activation required for survival after myocardial infarction in mice. Nat Med. 2011;17:581–588. doi: 10.1038/nm.2354. [DOI] [PubMed] [Google Scholar]
- 32.de Jager SC, Bermudez B, Bot I, Koenen RR, Bot M, Kavelaars A, et al. Growth differentiation factor 15 deficiency protects against atherosclerosis by attenuating CCR2-mediated macrophage chemotaxis. J Exp Med. 2011;208:217–225. doi: 10.1084/jem.20100370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pfitzenmaier J, Vessella R, Higano CS, Noteboom JL, Wallace DJ, Corey E. Elevation of cytokine levels in cachectic patients with prostate carcinoma. Cancer. 2003;97:1211–1216. doi: 10.1002/cncr.11178. [DOI] [PubMed] [Google Scholar]
- 34.Skipworth RJ, Deans DA, Tan BH, Sangster K, Paterson-Brown S, Brown DA, et al. Plasma MIC-1 correlates with systemic inflammation but is not an independent determinant of nutritional status or survival in oesophago-gastric cancer. Br J Cancer. 2010;102:665–672. doi: 10.1038/sj.bjc.6605532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Breit SN, Carrero JJ, Tsai VW, Yagoutifam N, Luo W, Kuffner T, et al. Macrophage inhibitory cytokine-1 (MIC-1/GDF15) and mortality in end-stage renal disease. Nephrol Dial Transplant. 2012;27:70–75. doi: 10.1093/ndt/gfr575. [DOI] [PubMed] [Google Scholar]
- 36.Kempf T, von Haehling S, Peter T, Allhoff T, Cicoira M, Doehner W, et al. Prognostic utility of growth differentiation factor-15 in patients with chronic heart failure. J Am Coll Cardiol. 2007;50:1054–1060. doi: 10.1016/j.jacc.2007.04.091. [DOI] [PubMed] [Google Scholar]
- 37.Vila G, Riedl M, Anderwald C, Resl M, Handisurya A, Clodi M, et al. The relationship between insulin resistance and the cardiovascular biomarker growth differentiation factor-15 in obese patients. Clin Chem. 2011;57:309–316. doi: 10.1373/clinchem.2010.153726. [DOI] [PubMed] [Google Scholar]
- 38.Dostalova I, Roubicek T, Bartlova M, Mraz M, Lacinova Z, Haluzikova D, et al. Increased serum concentrations of macrophage inhibitory cytokine-1 in patients with obesity and type 2 diabetes mellitus: the influence of very low calorie diet. Eur J Endocrinol. 2009;161:397–404. doi: 10.1530/EJE-09-0417. [DOI] [PubMed] [Google Scholar]
- 39.von Haehling S, Morley JE, Coats AJS, Anker SD. Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle. J Cachexia Sarcopenia Muscle. 2010;1:7–8. [DOI] [PMC free article] [PubMed]