Abstract
Objective
To determine the effect of intention to breastfeed on short-term breastfeeding outcomes in women delivering term and preterm infants
Design
Data from the CDC Pregnancy Risk Assessment Monitoring System (PRAMS) for three states, Ohio, Michigan and Arkansas during 2000–2003 were analyzed. SAS 9.1.3 and SUDAAN 10 were used for analyses.
Results
16839 subjects were included, 9.7% delivered preterm. 52.5% expressed definite intention to breastfeed, 16.8% tentative intention, 4.3% were uncertain, 26.8% had no intention to breastfeed. 65.2% initiated breastfeeding, 45.2% breastfed ≥ 4weeks, 30% breastfed ≥ 10 weeks. Women with definite intention were more likely to initiate (OR 24.3, 95% CI 18.4, 32.1), to breastfeed ≥ 4 weeks (OR 7.12, 95% CI 5.95, 8.51), and to breastfeed ≥ 10 weeks (OR 2.75, 95% CI 2.2, 3.45) compared to tentative intention. Levels of intention did not differ between women delivering preterm and term. Women delivering at < 34 weeks were more likely to initiate breastfeeding (OR 2.24, 95% CI 1.64, 3.06), and to breastfeed ≥ 4 weeks (OR 2.58, 95% CI 1.96, 3.41), but less likely to breastfeed ≥ 10 weeks (OR 0.55, 95% CI 0.44, 0.68) compared to term. Women delivering between 34 and 36 weeks were less likely to breastfeed ≥ 10 weeks than those delivering at term (OR 0.63, 95% CI 0.49, 0.81).
Conclusions
Prenatal intention to breastfeed is a powerful predictor of short-term breastfeeding outcomes in women delivering both at term and prematurely.
Keywords: breastfeeding, preterm infant, breastfeeding outcomes, breastfeeding intention
Introduction
Breastfeeding is an important public health practice that provides health benefits for both the breastfed infant and the breastfeeding mother. Despite the advantages of breastfeeding for mothers, infants, and population level health, breastfeeding rates in the United States continue to fall below WHO recommendations and the United States Healthy People 2020 goals1, 2. Similar discrepancy between goals for optimal breastfeeding and breastfeeding behavior are reported in Canadian, European, and Australian populations as well 3, despite the resource availability in these countries. Efforts to improve breastfeeding outcomes in developed countries must include research to elucidate the causes of suboptimal breastfeeding practices, at both the individual and societal levels.
Maternal prenatal beliefs and intentions about breastfeeding impact breastfeeding behaviors and outcomes. A series of small studies, including non-population based samples of as many as 450 patients, show a positive association of prenatal intention to breastfeed with breastfeeding initiation 4–9. A larger recent study of a prospectively enrolled representative UK cohort of mothers delivering term infants confirms this finding, and notes that intention was a stronger predictor than all other predictors combined 10.
Preterm birth, defined as birth before 37 completed weeks of gestation, is a significant public health problem in the United States, where rates have increased 20% from 1990 through 2007, from 10.6% to 12.7% 11. The benefits of breastfeeding for preterm infants are even greater than those experienced by term infants 12–14, however studies demonstrate consistently lower rates of breastfeeding initiation and shorter breastfeeding duration among mothers of preterm infants 15–18. Breastfeeding intention in mothers of premature infants has been studied in a few convenience samples 19–22, but the impact of intention on breastfeeding outcomes has not been investigated in this population, particularly not compared with a healthy term cohort.
We undertook an analysis of participants in the CDC’s Pregnancy Risk Assessment Monitoring System (PRAMS) for the period 2000–2003, to determine the impact of prenatal breastfeeding intention on breastfeeding initiation and continuation to at least four and ten weeks after delivery. We hypothesized that intention to breastfeed would powerfully predict breastfeeding success, after adjustment for multiple other factors associated with breastfeeding outcomes. We also chose to study the effect of prenatal intention on breastfeeding outcomes in mothers of preterm infants compared to mothers of term infants, given the high rate of preterm births.
Patients and Methods
The Pregnancy Risk Assessment Monitoring System (PRAMS) is a multi-state surveillance project conducted by the US Centers for Disease Control and Prevention (CDC) and participating state health departments. The PRAMS survey instrument is used to collect population-based information from women who had a recent live birth regarding their experiences, behaviors, and attitudes before, during, and immediately after delivery. A total of 32 states and New York City participated in PRAMS between 2000 and 2003. The primary means of data collection is a self-administered mailed questionnaire. The PRAMS sample, drawn from live birth certificate registries in each state, is a validated, stratified, multistate random sample of all births. PRAMS data are statistically weighted to adjust for the complex survey design, non-coverage, and non-response. A detailed explanation of PRAMS methodology may be found at: http://www.cdc.gov/prams/methodology.htm.
We analyzed the effect of prenatal intention to breastfeed on breastfeeding initiation and continuation among respondents from the three states (AR, MI, OH) who were asked to respond to the following supplemental question to the PRAMS standard instrument: “During your most recent pregnancy, what did you think about breastfeeding your new infant?”. Potential responses were: a) I knew I would breastfeed (definite intention), b) I thought I might breastfeed (tentative intention), c) I knew I would not breastfeed (no intention), and d) I didn’t know what to do about breastfeeding (uncertain). This supplemental breastfeeding intention question was asked in only these three states during these years.
To assess breastfeeding initiation, we analyzed the PRAMS question, “Did you ever breastfeed or pump breast milk for your baby after delivery?”. We chose two definitions of breastfeeding continuation: 1) breastfeeding at least four weeks, and 2) breastfeeding at least ten weeks. We chose four weeks to be consistent with the definition used in a previous report, to allow for comparison 23, and because breastfeeding through four weeks predicts continued success 24–26. Breastfeeding duration of greater than ten weeks was also modeled because 95% of mothers completed the survey when the infant was ten weeks old or older, allowing us to maximize our sample size for breastfeeding continuation. Breastfeeding duration was generated from responses to two PRAMS questions: “Are you still breastfeeding or feeding pumped milk to your baby?”, and “How many weeks or months did you breastfeed or pump milk to feed your baby?”
Demographic variables associated with breastfeeding initiation and continuation in our previous study of this PRAMS cohort 16 were modeled as potential confounders of the relationship between breastfeeding behavior and recalled prenatal intention to breastfeed, including infant gestational age, maternal age, race, education, mode of delivery, and Medicaid coverage in pregnancy. We also explored the relationship between parity and breastfeeding behavior, as the breastfeeding behavior of multiparous mothers is influenced by their prior parenting experience 27.
Statistical Analysis
SAS version 9.2 (SAS Institute, Research Triangle Park, NC) was used for data manipulation and to conduct preliminary analyses. SUDAAN version 10 (RTI, Research Triangle Park, NC) was used to compute the accurate standard errors for final weighted analyses and statistical tests to account for the complex survey design.
Preliminary univariate analyses
We examined the relationship between three breastfeeding outcome variables and breastfeeding intention, as well as factors previously associated with breastfeeding in this population 16. Weighted univariate logistic regression analysis was used to estimate the association of these variables with each outcome variable.
Weighted multivariate analyses
To determine the independent relationship between breastfeeding intention and breastfeeding behavior, we constructed a separate multivariable logistic model for each of the three study outcomes, retaining variables associated with breastfeeding outcomes in the preliminary analyses. Subjects who initiated breastfeeding were included in the four week continuation analysis, and those who breastfed for at least four weeks were included in the ten week continuation analysis. We performed a weighted stratified Cochrane Mantel-Haenszel analysis of the relationship of breastfeeding intention with each of the three breastfeeding outcomes, adjusting for preterm delivery (yes, no).
Results
Descriptive Analyses
The 16 838 survey responses included 7317 from Arkansas, 3748 from Michigan, and 5774 from Ohio. Surveys were completed a median of 74 days after the birth of the index baby. Table 1 shows the unadjusted numbers and weighted percentages for characteristics of the population. 9.7% of sampled mothers delivered prematurely, and 41% were primiparous. 65.2% initiated breastfeeding. 45.2% breastfed for at least four weeks, and 30% breastfed for at least ten weeks.
Table 1.
Population Characteristics of Subjects: PRAMS Arkansas, Michigan, and Ohio 2000–2003 Sample n 16838, weighted count 1007194
| Variable | n (unweighted) | Percent (weighted) |
|---|---|---|
| Breastfeeding Intention | ||
| Definite | 7698 | 52.2 |
| Tentative | 3204 | 16.8 |
| Uncertain | 809 | 4.3 |
| No intention | 4625 | 26.8 |
| Gestational Age | ||
| < 34 weeks | 1890 | 2.2 |
| 34–36 weeks | 2834 | 7.5 |
| ≥ 37 weeks | 12 115 | 90.3 |
| Primiparous | 7144 | 41 |
| Maternal Age, yrs | ||
| ≤19 | 2378 | 11.5 |
| 20–24 | 5029 | 25.9 |
| 25–29 | 4471 | 28.5 |
| 30–34 | 3230 | 22.9 |
| ≥35 | 1731 | 11.3 |
| Maternal Education, yrs | ||
| <12 years | 3220 | 16.6 |
| 12 years | 6313 | 33.6 |
| >12 years | 7157 | 48.8 |
| Maternal Race | ||
| White | 12161 | 81.5 |
| Black | 4268 | 15.7 |
| Other | 410 | 2.8 |
| Medicaid | ||
| Medicaid | 7807 | 35.9 |
| Not Medicaid | 9025 | 64.1 |
| Mode of Delivery | ||
| Cesarean section | 5130 | 23.6 |
| Vaginal | 11681 | 64.4 |
| Initiated Breastfeeding | 10 117 | 65.2 |
| Breastfeeding At 4 Weeks, | ||
| % of Entire Population | 7625 | 52 |
| % of Those Who Initiated | 7625 | 79.2 |
| Breastfeeding At 10 Weeks, | ||
| % of Entire Population | 5057 | 30.8 |
| % of Those Who Initiated | 5057 | 73 |
| State | ||
| Arkansas | 7317 | 13.4 |
| Michigan | 3748 | 30.1 |
| Ohio | 5774 | 56.5 |
Overall, 52.2 % of mothers expressed definite intention to breastfeed, 16.8% expressed tentative intention, 4.3% were uncertain, and 26.8% expressed no intention to breastfeed. Primiparous and multiparous mothers were equally likely to express definite intention to breastfeed (52%), but primiparous mothers were more likely to express tentative intention than those with prior children (21% v. 13%, p <0.0001); multiparous mothers were in turn more likely to express no intention to breastfeed (31% vs. 21%, p<0.0001).
Preliminary analyses of breastfeeding intention and duration
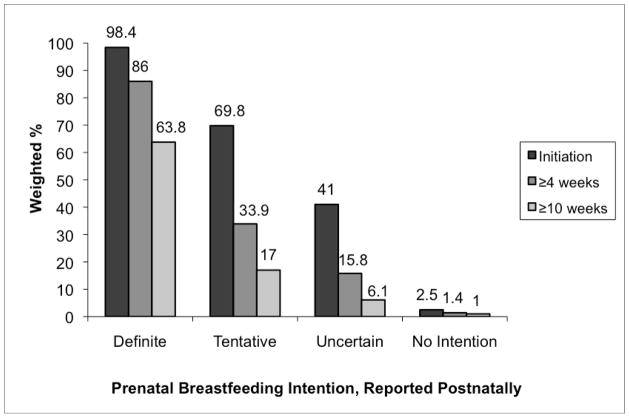
Definite breastfeeding intention was associated with factors known to be predictive of breastfeeding initiation, including older maternal age, higher level of maternal education, non-Black race, and non-Medicaid insurance (all p values <0.0001). 98.4% of women with definite intention to breastfeed initiated breastfeeding, 84.4 % breastfed for at least four weeks, and 58.5% breastfed for ten weeks. In contrast, 69.8% of women who tentatively thought they might breastfeed initiated, 32.9% breastfed for at least four weeks, and only 13.9% breastfed for ten weeks (p<0.0001) (Figure).
FIGURE 1.
Weighted Breastfeeding Outcomes by Level of Prenatal Breastfeeding Intention, PRAMS Arkansas, Michigan, and Ohio, 2000–2003.
As expected, when all other intention levels were compared with no intention to breastfeed, a strong and significant dose-response effect was noted for breastfeeding initiation (p <0.0001).
We analyzed the relationship of breastfeeding intention with each of the three breastfeeding outcomes, adjusting for preterm delivery (yes, no). The association of intention with all three breastfeeding outcomes was similar among both preterm and term respondents (data not shown) and statistically significant for both the preterm and term subgroups, as well as the population as a whole, (p < 0.001 for all).
Breastfeeding intention and breastfeeding initiation
Breastfeeding intention was the strongest predictor of breastfeeding initiation both in univariate analyses, and after adjusting for other significant predictors (Table 2). Women who expressed definite intention were 26.6 times more likely to initiate breastfeeding than those with tentative intention before adjustment, and the magnitude of this association remained stable after adjustment, with an odds ratio of 24.3. This effect size is 10 times larger than the next most significant predictor, premature birth.
Table 2.
Breastfeeding Intention and Other Predictors of Breastfeeding Initiation: PRAMS AR, MI, OH PRAMS 2000–2003
| Predictor | Breastfeeding Initiation | |||
|---|---|---|---|---|
| Crude OR | 95% CI | Adjusted OR† | 95% CI | |
| Breastfeeding Intention | ||||
| Definite | 26.6* | 20.3, 34.8 | 24.3* | 18.4, 32.1 |
| Tentative | 1 | referent | 1 | referent |
| Uncertain | 0.29* | 0.23, 0.38 | 0.30* | 0.23, 0.39 |
| No intention | 0.01* | 0.01, 0.01 | 0.01* | 0.01, 0.01 |
| Gestational Age, wks | ||||
| <34 | 1.22* | 1.05, 1.43 | 2.24* | 1.64, 3.06 |
| 34–36 | 0.92 | 0.78, 1.08 | 0.87 | 0.65, 1.17 |
| ≥ 37 | 1 | referent | 1 | referent |
| Primiparous | 1.38* | 1.24, 1.53 | 1.38* | 1.1, 1.71 |
| Maternal Age, yrs | ||||
| ≤19 | 0.37* | 0.31, 0.44 | 0.72 | 0.48, 1.07 |
| 20–24 | 0.50* | 0.43, 0.58 | 0.69* | 0.51, 0.95 |
| 25–29 | 0.77* | 0.67, 0.89 | 0.86 | 0.64, 1.16 |
| 30–34 | 1 | referent | 1 | referent |
| ≥35 | 0.92 | 0.76, 1.11 | 0.75 | 0.53, 1.07 |
| Maternal Education, yrs | ||||
| <12 | 0.70* | 0.61, 0.81 | 0.98 | 0.75, 1.28 |
| 12 | 1 | referent | 1 | referent |
| >12 | 3.08* | 2.75, 3.44 | 1.67* | 1.32, 2.11 |
| Maternal Race | ||||
| White | 1 | referent | 1 | referent |
| Black | 0.51* | 0.46, 0.57 | 0.94 | 0.75, 1.19 |
| Other | 2.66* | 1.79, 3.94 | 1.13 | 0.58, 2.20 |
| Medicaid | 0.39 | 0.35, 0.43 | 0.60 | 0.47, 0.75 |
| Cesarean section | 0.94 | 0.84, 1.05 | NA | NA |
| State | ||||
| Arkansas | 0.73* | 0.66, 0.81 | 0.92 | 0.74, 1.14 |
| Michigan | 1 | referent | 1 | referent |
| Ohio | 0.78* | 0.70, 0.87 | 0.93 | 0.75, 1.16 |
p <0.01; OR of 1 indicates referent group; all analyses are weighted
final model contained intention, gestational age, parity, maternal age, maternal education, maternal race, Medicaid status, and state of residence
Women giving birth before 34 weeks were 2.24 times more likely to initiate breastfeeding than those delivering term infants. There was a trend towards lower breastfeeding initiation among mothers of infants born between 34 and 36 weeks’ gestation compared to mothers of term infants.
Other predictors of breastfeeding initiation that remained significant after multivariable adjustment included parity, maternal age, maternal education, and Medicaid status. Primiparous women were more likely to initiate breastfeeding than were those with previous births (OR 1.38. 95% CI 1.1, 1.71). Women aged 20–24 years were less likely to initiate breastfeeding than were those aged 30–34 years. College education was associated with a 67% greater likelihood of breastfeeding initiation compared to completion of high school. Medicaid insurance status was associated with 60% lower likelihood of breastfeeding initiation compared with private insurance. The covariates of gestational age, parity, maternal age and education level, race, Medicaid insurance, and state of residence were included in the adjusted model of intention and breastfeeding initiation because they were significant predictors in univariate analysis.
Breastfeeding intention and breastfeeding continuation for at least four weeks
Breastfeeding intention was the strongest predictor of breastfeeding continuation to at least four weeks (Table 3). Women who expressed definite intention to breastfeed were 7.53 times more likely to breastfeed for at least four weeks, compared with those who expressed tentative intention (OR 7.53, 95% CI 6.37, 8.91), and the magnitude of this association changed little with adjustment.
Table 3.
Breastfeeding Intention and Other Predictors of Continued Breastfeeding at 4 weeks: PRAMS AR, MI, OH 2000–2003
| Predictor | Breastfeeding for at least 4 weeks | |||
|---|---|---|---|---|
| Crude OR | 95% CI | Adjusted OR† | 95% CI | |
| Breastfeeding Intention | ||||
| Definite | 7.53* | 6.37, 8.91 | 7.12* | 5.95, 8.51 |
| Tentative | 1 | referent | 1 | referent |
| Uncertain | 0.71* | 0.49, 1.04 | 0.66 | 0.37, 1.18 |
| No intention | 0.87* | 0.39, 1.17 | 0.83 | 0.55, 1.25 |
| Gestational Age, wks | ||||
| <34 | 1.24 | 0.97, 1.59 | 2.58* | 1.96, 3.41 |
| 34–36 | 0.84 | 0.66, 1.06 | 0.98 | 0.74, 1.29 |
| ≥37 | 1 | referent | 1 | referent |
| Primiparous | 0.57* | 0.50, 0.66 | 0.75* | 0.63, 0.90 |
| Maternal Age, yrs | ||||
| 19 | 0.23* | 0.18, 0.30 | 0.55* | 0.38, 0.78 |
| 20–24 | 0.40* | 0.33, 0.49 | 0.65* | 0.51, 0.84 |
| 25–29 | 0.74* | 0.60, 0.91 | 0.86 | 0.68, 1.09 |
| 30–34 | 1 | referent | 1 | referent |
| ≥35 | 1.25 | 0.92, 1.69 | 1.18 | 0.86, 1.63 |
| Maternal Education, yrs | ||||
| <12 | 0.84 | 0.68, 1.05 | 1.11 | 0.85, 1.46 |
| 12 | 1 | referent | 1 | referent |
| >12 | 2.37* | 2.02, 2.77 | 1.55* | 1.27, 1.88 |
| Maternal Race | ||||
| White | 1 | referent | 1 | referent |
| Black | 0.67* | 0.57, 0.80 | 1.1 | 0.89, 1.37 |
| Other | 1.38 | 0.90, 2.14 | 1.09 | 0.68, 1.74 |
| Medicaid | 0.43* | 0.37. 0.49 | 0.64* | 0.52, 0.78 |
| Cesarean section | 0.92 | 0.79, 1.08 | NA | NA |
| State | ||||
| Arkansas | 0.74* | 0.66, 0.81 | 0.86 | 0.72, 1.02 |
| Michigan | 1 | referent | 1 | referent |
| Ohio | 1.05 | 0.90, 1.23 | 1.05 | 0.88, 1.26 |
p <0.01; OR of 1 indicates referent group; all analyses are weighted
final model contained intention, gestational age, parity, maternal age, maternal education, maternal race, Medicaid status, and state of residence
Infant gestational age of less than 34 weeks was a significant predictor of breastfeeding for at least four weeks after adjustment; mothers delivering prior to 34 weeks were 2.58 times more likely to continue for four weeks than those delivering at term (OR 2.58, 95% CI 1.96, 3.41). There was no difference in the odds of breastfeeding for at least four weeks among mothers of late preterm infants compared with mothers of term infants.
Other significant predictors of breastfeeding continuation to at least four weeks included parity, maternal age, maternal education, and Medicaid status. In contrast to breastfeeding initiation, where primiparity was associated with increased odds of initiation, primiparous women were significantly less likely to continue to breastfeed for four weeks than were women with previous births (OR 0.75, 95% CI 0.63, 0.90). Women younger than 24 years were less likely to breastfeed for four weeks than those 30 to 34 years. Women with some college education were more likely to breastfeed for four weeks compared with those who completed high school. Medicaid insurance status, compared with private insurance, was associated with lower odds of breastfeeding for at least four weeks. The covariates of gestational age, parity, maternal age and education level, race, Medicaid insurance, and state of residence were included in the adjusted model of intention and breastfeeding continuation to at least four weeks because they were significant predictors in univariate analysis.
Breastfeeding intention and breastfeeding continuation for at least ten weeks
Definite prenatal intention to breastfeed was the strongest predictor of breastfeeding continuation for at least ten weeks, after adjustment for all other significant predictors. Women with definite intention to breastfeed were 2.75 times more likely to breastfeed for at least ten weeks compared with those with tentative intention. (Table 4).
Table 4.
Breastfeeding Intention and Other Predictors of Continued Breastfeeding at 10 weeks: PRAMS AR, MI, OH 2000–2003
| Predictor | Breastfeeding for at least 10 weeks | |||
|---|---|---|---|---|
| Crude OR | 95% CI | Adjusted OR† | 95% CI | |
| Breastfeeding Intention | ||||
| Definite | 2.98* | 2.41, 3.68 | 2.75* | 2.20, 3.45 |
| Tentative | 1 | referent | 1 | referent |
| Uncertain | 0.64 | 0.36, 1.13 | 0.77 | 0.42, 1.42 |
| No intention | 0.98 | 0.42, 2.26 | 1.08 | 0.47, 2.52 |
| Gestational Age, wks | ||||
| <34 | 0.40* | 0.33, 0.49 | 0.55* | 0.44, 0.68 |
| 34–36 | 0.58* | 0.46, 0.74 | 0.63* | 0.49, 0.81 |
| ≥37 | 1 | referent | 1 | referent |
| Primiparous | 0.76* | 0.65, 0.88 | 1.00 | 0.85, 1.18 |
| Maternal Age, yrs | ||||
| ≤19 | 0.26* | 0.18, 0.30 | 0.39* | 0.27, 0.57 |
| 20–24 | 0.42* | 0.33, 0.49 | 0.55* | 0.43, 0.70 |
| 25–29 | 0.67* | 0.60, 0.91 | 0.71* | 0.58, 0.87 |
| 30–34 | 1 | referent | 1 | referent |
| ≥35 | 1.18 | 0.92, 1.69 | 1.24 | 0.93, 1.64 |
| Maternal Education, yrs | ||||
| <12 | 0.96 | 0.68, 1.05 | 1.21 | 0.91, 1.61 |
| 12 | 1 | referent | 1 | referent |
| >12 | 2.07* | 1.76, 2.44 | 1.43* | 1.18, 1.73 |
| Maternal Race | ||||
| White | 1 | referent | 1 | referent |
| Black | 0.72* | 0.60, 0.86 | 1.01 | 0.81, 1.26 |
| Other | 1.29 | 0.86, 1.92 | 1.16 | 0.75, 1.80 |
| Medicaid | 0.48* | 0.41, 0.56 | 0.75* | 0.62, 0.92 |
| Cesarean section | 0.78* | 0.66, 0.92 | 0.76* | 0.63, 0.90 |
| State | ||||
| Arkansas | 0.63* | 0.54, 0.74 | 0.76* | 0.64, 0.89 |
| Michigan | 1 | referent | 1 | referent |
| Ohio | 0.93* | 0.79, 1.09 | 0.95 | 0.80, 1.13 |
p <0.01; OR of 1 indicates referent group; all analyses are weighted
final model contained intention, gestational age, parity, maternal age, maternal education, maternal race, Medicaid status, mode of delivery, and state of residence
Women delivering premature infants, both those born before 34 weeks and those born between 34 and 36 weeks, were less likely to breastfeed for at least ten weeks than were mothers delivering term infants. Relative to mothers of term infants, mothers of very preterm infants were only 55% as likely to breastfeed for at least ten weeks, and mothers of late preterm infants were only 63% as likely.
Other significant predictors of breastfeeding continuation to at least ten weeks included, maternal college education, private insurance status, and vaginal delivery. Maternal age less than 30 years was negatively associated with breastfeeding continuation to ten weeks in the adjusted analysis. The covariates of gestational age, parity, maternal age and education level, race, Medicaid insurance, cesarean delivery, and state of residence were included in the adjusted model of intention and breastfeeding continuation to at least ten weeks because they were significant predictors in univariate analysis.
Discussion
In this large population-based and representative sample of newly delivered mothers from three US states, we found that prenatal intention to breastfeed is strongly and directly predictive of breastfeeding initiation and continuation. Women who reported definite intention to breastfeed were highly likely to succeed in doing so, as 98.4% initiated breastfeeding, while women with tentative intention were less successful, as only 69.8% initiated, and those who were uncertain were less successful still, as only 39.7% initiated. Compared with women who expressed tentative intention, women expressing definite intention to breastfeed were 26.6 times more likely to initiate breastfeeding, 7.1 times more likely to breastfeed for at least four weeks, and 2.8 times more likely to breastfeed for at least ten weeks. Older maternal age, higher maternal education, and higher socioeconomic status (as indicated by insurance type) were also significant predictors of breastfeeding initiation and duration.
We found an important adjusted relationship of infant gestational age with breastfeeding outcomes. Mothers of preterm infants less than or equal to 34 weeks were more than two times more likely to initiate and continue breastfeeding for at least four weeks than were mothers of term infants. However, these mothers were only 55% as likely as mothers of term infants to continue breastfeeding for at least ten weeks. Given that the hospital stay for infants in this gestational age range is typically 6–20 weeks, this finding suggests that educational efforts in the NICU to encourage breastmilk expression and feeding were successful, but that support for continued breastfeeding at home was lacking. Mothers of late preterm infants (34–36 weeks) were significantly less likely to breastfeed for ten weeks as were mothers of term infants. Our results echo those of Donath and Amir, who found that Australian women delivering at 35–36 weeks gestation were less likely than those delivering at term to initiate breastfeeding (88.2% vs. 92–93.9%), and that by six months of age, mothers of these late preterm infants were over twice as likely to have ceased breastfeeding as those delivering at term 28. The Australian results and ours suggest that late preterm infants, who represent two-thirds of the preterm infants born in the US 11, were a group at high risk for breastfeeding failure.
Other authors have looked at the impact of prematurity on breastfeeding decisions in small convenience samples using primarily qualitative methods. Sweet studied a group of 44 mothers of VLBW infants in Australia in 2008, reporting that breastfeeding intention was developed early in pregnancy, and that preterm birth did not change this intention22. Lucas and Cole reported that intention to breastfeed was more common in mothers of preterm infants (mean BW 1370 g) who were older, married, and delivered male infants, but that infant gestational age played no role 21. Kaufman and Hall and Jaeger and colleagues reported that breastfeeding intention (or lack therof) is established at the time of delivery of a preterm or sick infant, but that some women do change their mind and breastfeed when they initially planned to feed formula 19, 20. Social support from family, peers, and medical providers can influence these decisions, and can influence breastfeeding duration 20. However, none of these studies looked at breastfeeding duration as a function of prematurity systematically and specifically, with a comparison to term infants, as we have done in our study.
Because of these findings, we conducted a stratified analysis of breastfeeding intention on all three breastfeeding outcomes adjusting for gestational age alone, and demonstrated that levels of intention did not differ by gestational age category, reinforcing the importance of infant gestational age in breastfeeding success. Based on our findings, mothers of preterm infants in all gestational age categories represent a group at risk for poor long-term breastfeeding outcomes.
Our study of a large representative sample of women from three US states reinforces findings found in recent smaller studies in other countries. In a cross-sectional sample of 450 pregnant Irish women who delivered term infants, positive intention to breastfeed was associated with an OR of 244 for breastfeeding initiation, compared with no intention 8. A study of 341 Dutch mothers who delivered term infants also found prenatal intention to be associated with an OR of 405.8 for breastfeeding intention. The investigators described the factors involved in formation of a positive intention to breastfeed, including positive personal attitudes toward breastfeeding, negative personal attitudes toward formula feeding, positive social norms for breastfeeding at home and work, social support for breastfeeding at home and work, and high self efficacy for breastfeeding. In fact, when these factors were included in models to predict breastfeeding initiation, no demographic variable remained a significant predictor, suggesting that breastfeeding behavior depends mostly on factors related to social support and womens’ own self-efficacy and attitudes 9.
Several other large-scale studies have also found a strong relationship between breastfeeding intention and behavior. DiGirolamo and colleagues 29 used the 1993–94 Infant Feeding Practices Survey to assess the impact of prenatal breastfeeding intention and breastfeeding behavior in a sample of 1665 primarily White, well-educated US women, recruited in the third trimester of pregnancy. The investigators assessed breastfeeding behavior for 12 months after delivery, comparing the prenatal predicted of duration of breastfeeding to the actual duration. They demonstrated that prenatal intention to breastfeed impacts breastfeeding behavior. Women with no intention of breastfeeding were 405 times less likely to initiate breastfeeding than those who intended to breastfeed for 12 months, and women who planned to stop before two months were 48 times more likely to have breastfed for fewer than ten weeks than were those who intended to breastfeed for at least 12 months 29. Donath and Amir 10 analyzed a large population-based sample of 10548 women from the Avon Longitudinal Study of Pregnancy and Childhood, a prospective cohort study of women and children from the UK. At 32 weeks’ gestation, women were asked to predict their duration of breastfeeding, and breastfeeding outcomes were monitored for 12 months after delivery. They found that anticipated breastfeeding duration was strongly predictive of breastfeeding behavior. Women who intended to breastfeed longer, suggestive of greater commitment to breastfeeding, had higher rates of breastfeeding initiation: 96.6% of women who intended to breastfeed for at least four months initiated breastfeeding, while only 74.7% of those who intended to breastfeed for less than four weeks initiated 10.
Although the PRAMS instrument does not allow us to match intended duration of breastfeeding to actual breastfeeding duration, if the responses to the PRAMS breastfeeding intention question are considered in an ordinal fashion, with a spectrum of definite intention, tentative intention, uncertain intention, and no intention, our analysis also demonstrates that level of intention is important in predicting behavior. Tentative and uncertain intention were associated with greater likelihood of breastfeeding initiation than no intention, but not of continuation at either four or ten weeks, suggesting that a stronger degree of commitment resulted in longer term breastfeeding success, similar to the results reported in the US by DiGirolamo et al 29 and in the UK by Donath and Amir 10.
The major strength of our study lies in the robust sampling methods employed by PRAMS, which allowed us to evaluate the impact of breastfeeding intention on breastfeeding outcomes in a population representative of all live births in three US states over three years. In contrast to other studies of breastfeeding intention and subsequent breastfeeding behavior, our sample was larger than all, and was one of only two studies utilizing a population-based sample. Our results are generalizable to much of the US population. Importantly, the PRAMS data allowed us to determine the impact of prematurity on breastfeeding outcomes, adjusting for breastfeeding intention, while previous studies have excluded premature infants, particularly those born before 34 weeks, by design.
Our study is subject to some limitations. PRAMS subjects are sampled only once, typically when the index infant is between 6 weeks and 6 months of age. As 95% of respondents in our sample returned the survey when their infants were 10 weeks or older, we were able to examine breastfeeding continuation to only 10 weeks. Additionally, breastfeeding intention information was collected postnatally, and remote from the delivery of the infant. This may have created recall bias, as women may have tended to report their actual behavior as their “intention”. We were also unable to determine the effect of predicted breastfeeding duration on actual duration, as these questions are not part of the PRAMS instrument.
The determinants of breastfeeding behavior are clearly multiple, and include factors both intrinsic and extrinsic to mothers themselves. Our study adds to the body of knowledge regarding breastfeeding intention and subsequent breastfeeding behavior. Our study provides a novel report of the impact of breastfeeding intention on breastfeeding outcomes in mothers delivering prematurely. We have demonstrated that intention to breastfeed, as reported postnatally, is an extremely powerful predictor of breastfeeding initiation, with an impact almost 12-fold greater than the next most significant factor, prematurity, and that intention strongly affects continuation to at least four weeks and at least ten weeks. Large population-based prospective studies of prenatally-reported intention to breastfeed are needed to verify the strength of this predictor of breastfeeding outcomes. Further research is needed into the factors influencing maternal intention to breastfeed, with the aim to develop interventions to promote development of positive intention to breastfeed prior to pregnancy or delivery.
Acknowledgments
The PRAMS Working Group
PRAMS Working Group: Alabama—Albert Woolbright, PhD; Alaska—Kathy Perham-Hester, MS, MPH; Arkansas—Mary McGehee, PhD; Colorado—Alyson Shupe, PhD; Delaware—George Yocher, MS; Florida—Marie Bailey, MA, MSW, MPH; Georgia—Carol Hoban, Ph.D, MS,.MPH; Hawaii— Mark Eshima, MA; Illinois—Theresa Sandidge, MA; Louisiana—Joan Wightkin; Maine—Tom Patenaude; Maryland—Diana Cheng, MD; Massachusetts—Hafsatou Diop, MD, MPH; Michigan— Violanda Grigorescu, MD, MSPH; Minnesota—Judy Punyko, PhD, MPH; Mississippi—Marilyn Jones, M.Ed; Missouri—Venkata Garikapaty, MSc, MS, PhD, MPH; Montana—JoAnn Dotson; Nebraska—Brenda Coufal; New Jersey—Lakota Kruse, MD; New Mexico—Eirian Coronado, MPH; New York State—Anne Radigan-Garcia; New York City—Candace Mulready-Ward, MPH; North Carolina—Paul Buescher, PhD; North Dakota—Sandra Anseth; Ohio—Connie Geidenberger; Oklahoma—Alicia Lincoln, MSW, MSPH; Oregon—Kenneth Rosenberg, MD; Pennsylvania—Tony Norwood; Rhode Island—Sam Viner-Brown, PhD; South Carolina—Mike Smith; South Dakota Tribal—Christine Rinki, MPH; Texas—Kate Sullivan, PhD; Tennessee—David Law, PhD; Utah— Laurie Baksh; Vermont—Peggy Brozicevic; Virginia—Marilyn Wenner; Washington—Linda Lohdefinck; West Virginia—Melissa Baker, MA; Wisconsin—Katherine Kvale, PhD; Wyoming— Angi Crotsenberg; CDC PRAMS Team, Applied Sciences Branch, Division of Reproductive Health
Contributor Information
Tarah T. Colaizy, University of Iowa, Dept of Pediatrics, Iowa City, IA
Audrey F. Saftlas, University of Iowa College of Public Health, Dept of Epidemiology, Iowa City, IA
Frank H. Morriss, Jr., University of Iowa, Dept of Pediatrics, Iowa City, IA
References
- 1.MICH HP2020-12. Developing Healthy Poeople 2020: Proposed HP2020 Objectives, Maternal, Infant, and Child Health. 2010. [Google Scholar]
- 2.Organization WH; Organization WH. WHA55 A55/15. Geneva, Switzerlanded: 2002. Global strategy on infant and young child feeding. [Google Scholar]
- 3.Callen P. Incidence and duration of breastfeeding for term infants in Canada, United States, Europe, and Australia: a literature review. Birth. 2004;31:285–92. doi: 10.1111/j.0730-7659.2004.00321.x. [DOI] [PubMed] [Google Scholar]
- 4.Coreil J, Murphy JE. Maternal commitment, lactation practices, and breastfeeding duration. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 1988;17:273–8. [Google Scholar]
- 5.Cronenwett L, Stukel T, Kearney M, Barrett J, Covington C, Del Monte K, et al. Single daily bottle use in the early weeks postpartum and breast-feeding outcomes. Pediatrics. 1992;90:760–6. [PubMed] [Google Scholar]
- 6.Lawson K, Tulloch MI. Breastfeeding duration: prenatal intentions and postnatal practices. J Adv Nurs. 1995;22:841–9. doi: 10.1111/j.1365-2648.1995.tb02633.x. [DOI] [PubMed] [Google Scholar]
- 7.O’Campo P, Faden RR, Gielen AC, Wang MC. Prenatal factors associated with breastfeeding duration: recommendations for prenatal interventions. Birth. 1992;19:195–201. doi: 10.1111/j.1523-536x.1992.tb00402.x. [DOI] [PubMed] [Google Scholar]
- 8.Tarrant RC, Younger KM, Sheridan-Pereira M, White MJ, Kearney JM. The prevalence and determinants of breast-feeding initiation and duration in a sample of women in Ireland. Public Health Nutr. 2010;13:760–70. doi: 10.1017/S1368980009991522. [DOI] [PubMed] [Google Scholar]
- 9.Kools EJ, Thijs C, de Vries H. The behavioral determinants of breast-feeding in The Netherlands: predictors for the initiation of breast-feeding. Health Educ Behav. 2005;32:809–24. doi: 10.1177/1090198105277327. [DOI] [PubMed] [Google Scholar]
- 10.Donath SM, Amir LH. Relationship between prenatal infant feeding intention and initiation and duration of breastfeeding: a cohort study. Acta Paediatr. 2003;92:352–6. [PubMed] [Google Scholar]
- 11.March of Dimes PeriStats: Your online source for perinatal statistics, at. ( http://www.marchofdimes.com/peristats/). ed, April 20, 2010.
- 12.Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep) 2007:1–186. [PMC free article] [PubMed] [Google Scholar]
- 13.Schanler RJ, Hurst NM, Lau C. The use of human milk and breastfeeding in premature infants. Clinics in Perinatology. 1999;26:379–98. vii. [PubMed] [Google Scholar]
- 14.Schanler RJ. The use of human milk for premature infants. The Pediatric clinics of North America. 2001;48:207–19. doi: 10.1016/s0031-3955(05)70295-9. [DOI] [PubMed] [Google Scholar]
- 15.Ahluwalia IB, Morrow B, Hsia J, Grummer-Strawn LM. Who is breast-feeding? Recent trends from the pregnancy risk assessment and monitoring system. J Pediatr. 2003;142:486–91. doi: 10.1067/mpd.2003.199. [DOI] [PubMed] [Google Scholar]
- 16.Colaizy TT, Morriss FH. Positive effect of NICU admission on breastfeeding of preterm US infants in 2000 to 2003. J Perinatol. 2008;28:505–10. doi: 10.1038/jp.2008.32. [DOI] [PubMed] [Google Scholar]
- 17.Furman L, Minich NM, Hack M. Breastfeeding of very low birth weight infants. J Hum Lact. 1998;14:29–34. doi: 10.1177/089033449801400112. [DOI] [PubMed] [Google Scholar]
- 18.Ryan AS, Wenjun Z, Acosta A. Breastfeeding continues to increase into the new millennium. Pediatrics. 2002;110:1103–9. doi: 10.1542/peds.110.6.1103. [DOI] [PubMed] [Google Scholar]
- 19.Jaeger MC, Lawson M, Filteau S. The impact of prematurity and neonatal illness on the decision to breast-feed. J Adv Nurs. 1997;25:729–37. doi: 10.1046/j.1365-2648.1997.1997025729.x. [DOI] [PubMed] [Google Scholar]
- 20.Kaufman KJ, Hall LA. Influences of the social network on choice and duration of breast-feeding in mothers of preterm infants. Res Nurs Health. 1989;12:149–59. doi: 10.1002/nur.4770120305. [DOI] [PubMed] [Google Scholar]
- 21.Lucas A, Cole TJ, Morley R, Lucas PJ, Davis JA, Bamford MF, et al. Factors associated with maternal choice to provide breast milk for low birthweight infants. Arch Dis Child. 1988;63:48–52. doi: 10.1136/adc.63.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sweet L. Birth of a very low birth weight preterm infant and the intention to breastfeed ‘naturally’. Women Birth. 2008;21:13–20. doi: 10.1016/j.wombi.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 23.Ahluwalia IB, Morrow B, Hsia J. Why do women stop breastfeeding? Findings from the Pregnancy Risk Assessment and Monitoring System. Pediatrics. 2005;116:1408–12. doi: 10.1542/peds.2005-0013. [DOI] [PubMed] [Google Scholar]
- 24.Taveras EM, Capra AM, Braveman PA, Jensvold NG, Escobar GJ, Lieu TA. Clinician support and psychosocial risk factors associated with breastfeeding discontinuation. Pediatrics. 2003;112:108–15. doi: 10.1542/peds.112.1.108. [DOI] [PubMed] [Google Scholar]
- 25.Baxter J, Cooklin AR, Smith J. Which mothers wean their babies prematurely from full breastfeeding? An Australian cohort study. Acta Paediatr. 2009;98:1274–7. doi: 10.1111/j.1651-2227.2009.01335.x. [DOI] [PubMed] [Google Scholar]
- 26.Dubois L, Girard M. Social determinants of initiation, duration and exclusivity of breastfeeding at the population level: the results of the Longitudinal Study of Child Development in Quebec (ELDEQ 1998–2002) Can J Public Health. 2003;94:300–5. doi: 10.1007/BF03403610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li R, Ogden C, Ballew C, Gillespie C, Grummer-Strawn L. Prevalence of exclusive breastfeeding among US infants: the Third National Health and Nutrition Examination Survey (Phase II, 1991–1994) Am J Public Health. 2002;92:1107–10. doi: 10.2105/ajph.92.7.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Donath SM, Amir LH. Effect of gestation on initiation and duration of breastfeeding. Arch Dis Child Fetal Neonatal Ed. 2008;93:F448–50. doi: 10.1136/adc.2007.133215. [DOI] [PubMed] [Google Scholar]
- 29.DiGirolamo A, Thompson N, Martorell R, Fein S, Grummer-Strawn L. Intention or experience? Predictors of continued breastfeeding. Health Educ Behav. 2005;32:208–26. doi: 10.1177/1090198104271971. [DOI] [PubMed] [Google Scholar]