Abstract
Chronic hepatitis C virus (HCV) infection is highly prevalent among current and former drug users. However, the minority of patients enrolled in drug treatment programs have initiated HCV treatment. New models are needed to overcome barriers to care. In this retrospective study, we describe the implementation and outcomes of 42 patients treated in a Concurrent Group Treatment (CGT) program. Patients participated in weekly provider-led group treatment sessions which included review of side effects; discussion of adherence and side effect management; administration of interferon injections; brief physical exam; and ended with brief meditation. Of the first 27 patients who initiated CGT, 42% achieved a sustained viral response. Additionally, 87% (13/15) of genotype-1 infected patients treated with direct acting antiviral agent achieved an undetectable viral load at 24 weeks. The CGT model may be effective in overcoming barriers to treatment and improving adherence and outcomes among patients enrolled in drug treatment programs.
Introduction
Over 4 million people in the United States are infected with the hepatitis C virus (HCV) (Armstrong, Wasley, Simard, McQuillan, Kuhnert & Alter, 2006; Ly, Xing, Monina Klevens, Jiles, Ward & Holmberg, 2012). HCV related morbidity and mortality are projected to continue to increase through the next decade, peaking by 2020 (Wong, McQuillan, McHutchison, & Poynard, 2000; Armstrong et al 2006; Davis & Rodriguez, 2001). Injection drug users (IDUs) and opiate agonist treatment patients have high rates of HCV infection with antibody positivity between 65% and 90% (Murrill, Weeks, Castrucci, Weinstock, Bell, Spruill, & Gwinn, 2002; Diaz et al., 2001; Patrick et al., 2001 Shepard, Finelli & Alter, 2005), and worldwide, about ten million IDUs may be anti-HCV positive (Nelson, Mathers & Cowie, 2011). Direct acting antiviral medications (DAAs) have been shown to increase successful treatment of HCV but add complexity to treatment regimens with increased pill burden, as well as new and additive side effects when compared to older treatment regimens. Unfortunately, few IDUs receive HCV treatment despite their interest in treatment (Walley, et al., 2005) and guidelines encouraging their evaluation and treatment (National Institues of Health, 2003; Mehta et al, 2006; Mehta et al, 2008; Grebely et al, 2009; Ghany, Strader, Thomas, & Seeff, 2009; European Association for the Study of the Liver, 2011).
Low uptake of HCV treatment among drug users is associated with numerous factors including patient mistrust of the medical system (Merrill, Rhodes, Deyo, Marlatt, & Bradley, 2002), misconceptions regarding HCV disease and treatment, fears of adverse medication effects, mental illness, unstable housing, and lack of psychosocial support (Edlin et al., 2005; Treloar & Holt 2008; Doab, Treloar, & Dore, 2005; Strauss et al., 2007). Physicians often withhold treatment due to anticipation of poor adherence; severe medical, psychiatric and psychosocial co-morbidities; or concerns about substance abuse relapse and reinfection (Edlin et al., 2001; Stephenson, 2001; Stein, Maksad & Clarke, 2001; Falck-Ytter et al., 2002; Bini et al., 2005; Kanwal et al, 2007;. Grebely et al, 2009; Kramer, Kanwal, Richardson, Giordano, Petersen & El-Serag, 2011; Gidding et al, 2012).
Referral to hospital based specialty care has not been a successful strategy for HCV-infected IDUs. IDUs are less likely than non-drug users to receive referrals to hepatology clinics, are less likely to be considered treatment candidates when evaluated by hepatologists, and have poorer outcomes when they do receive treatment (Falck-Ytter et al., 2002; Cullen et al., 2005; Doab et al., 2005; Fishbein, Yungtai, Reinus & Klein, 2004; Feurerstadt et al., 2010; Mehta et al., 2006; Schackman, Teixeira, & Beeder, 2007).
IDUs already engaged in medical treatment have been demonstrated to engage in HCV treatment and to achieve optimal outcomes in multidisciplinary settings where drug treatment, medical care, peer education and psychosocial support are all included (Sylvestre 2005, Clanon, Mueller, & Harank, 2005; Litwin, Soloway, & Gourevitch, 2005; Grebely et al, 2007; Guadagnino et al., 2007; Sylvestre & Zweben, 2007; Litwin et al., 2009; Hellard, Sacks-Davis & Gold, 2009;. Norman et al., 2008; Grebely, et al., 2011). Successful models emphasize HCV support groups throughout all stages of evaluation and treatment, with individualized medical care separate from the group. Despite the success of these models, the high HCV prevalence among current and previous drug users, their low rates of HCV treatment uptake, and poor outcomes in referral-based models suggest that new models of HCV treatment are still needed to bridge the treatment gap.
Group treatment of HCV and addiction are natural allies, as both peer- and provider-led groups are familiar, well-received, and efficient in the substance abuse setting (Leshner, 1997). The 12-step model of mutual aid is used by the majority of adults receiving formal drug treatment in the U.S (Substance Abuse and Mental Health Services Administration, 2004). Group medical visits have been used since the 1990’s as a tool in the management of chronic illness (Noffsinger, 1999; Bronson & Maxwell, 2008; Jaber, Braksmajer, & Trilling, 2006; Meehan et al., 2006). Group medical visits combine provider-led group education and peer interaction with elements of individual patient visits (Jaber et al., 2006). Although group medical visits are different from 12-step groups in how one participates, how they are organized, and the usual settings that they occur, both modalities create healthy communities based on mutual aid and support. In concurrent group treatment of HCV infection, patients initiate and continue treatment together for the entire treatment course experiencing the same milestones together (e.g. 4 week viral load). All elements of individual medical visit (e.g.vital signs, history, and physical) are integrated within the group setting.
Although HCV treatment groups differ from group treatment of chronic diseases in the fact that HCV can be cured, essential benefits of group treatment are still applicable. Among these is the mutual support of peers with similar experience. As the group members form relationships, they develop a sense of responsibility to the group which leads to the aspiration to “do well” in treatment and to see their peers succeed as well. Patients undergoing the same treatment reassure each other about expected but distressing and frightening side effects. Additionally, the partnership of patient and provider in treatment groups adds an ongoing educational component not present in peer-led support groups.
While prior studies have shown improved HCV outcomes when HCV treatment is co-located with substance abuse treatment and/or incorporates peer support, we are not aware of any published evaluations of group HCV treatment. In this study we describe the implementation and early outcomes of a program of concurrent group treatment (CGT) of chronic HCV infection in a methadone maintenance program. We report final virological outcomes for the first 27 patients who initiated CGT of HCV, and preliminary virological outcomes for the first 15 genotype-1 infected patients who initiated CGT of HCV with new direct acting antiviral agents.
Methods
Setting
The Concurrent Group Treatment Program (CGT) was first implemented in March 2009 at a large methadone maintenance treatment center in the Bronx, NY. The center provides pharmacotherapy and related services to approximately 1000 opioid dependent adults. An estimated 65% of patients are anti-HCV positive, and 75% of anti-HCV positive patients have chronic HCV infection. In August 2011, the CGT program was extended to a second site that serves another 1000 opioid dependent adults.
Both centers offer comprehensive substance abuse treatment, as well as medical and psychiatric care. Medical care, including evaluation and treatment for HCV, is provided on-site by internists, family physicians, and physician assistants with expertise in HIV and addiction medicine (Litwin et al., 2005; Litwin et al., 2009). An on-site psychiatrist is also available for consultations. Liver biopsies, when indicated, are performed at an affiliated hospital.
A peer education program focused on HCV has been active since 2002. Peer trainings are conducted at regular intervals for interested patients who have initiated HCV treatment. Peer training includes 6 hour-long sessions led by a hepatitis coordinator who also provided ongoing weekly supervision. Peers participate in various on-site and off-site activities including: co-facilitating HCV support groups and CGT groups; escorting patients to liver biopsy appointments; participation in clinic-wide HCV educational events; participation in off-site task forces and activities; and off-site speaking engagements and trainings (Litwin et al., 2005). In CGT groups, peers co-led HCV-related discussions with patients, answered questions, and provided logistical support (recorded patient weights, distributed weekly surveys and made coffee).
The Concurrent Group Treatment Model
Referral and evaluation
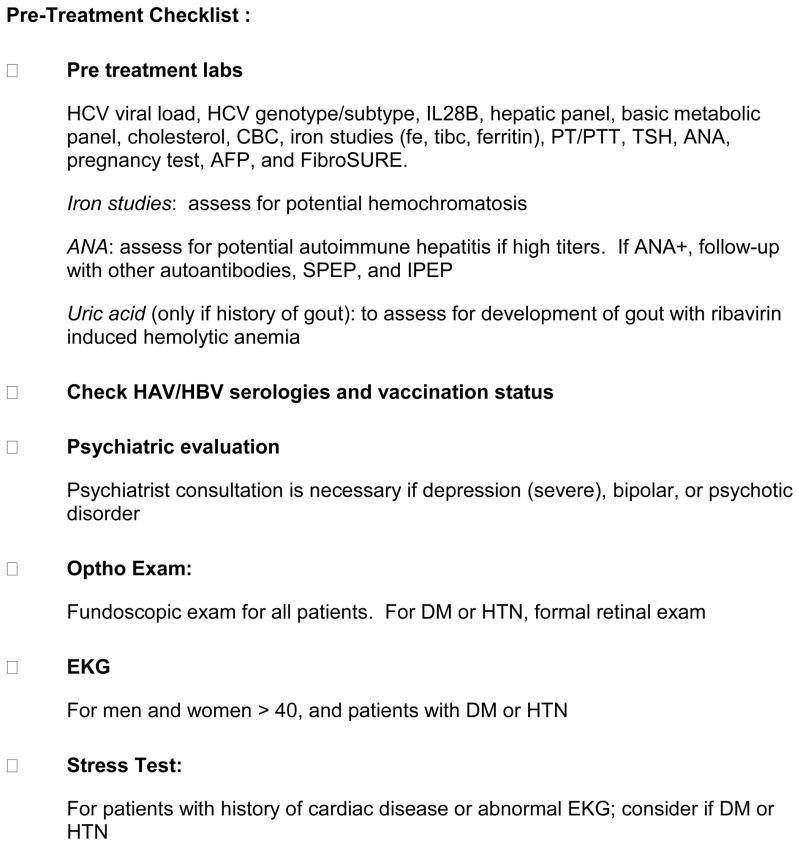
Medical staff referred patients who were appropriate for HCV treatment when they were identified on admission, during annual medical exams, or at routine medical visits. A minimum of four patients was required to start a group. However, individual patient characteristics (e.g. number of coinfected subjects or women) informed group size to maximize group cohesion. The wait to begin group treatment did not exceed three months. Pre-treatment evaluation included laboratory testing, assessment of medical co-morbidities, psychiatric evaluation, and a complete psychosocial evaluation (including social support, housing stability, substance abuse issues and health insurance, detailed in figure 1). All patients received fundoscopic exams on-site. Patients with a history of diabetes or hypertension were referred to an affiliated off-site ophthalmologist. Group treatment was offered as an alternative to individual treatment, and interested patients were invited to a group treatment orientation. Individual treatment with the same providers was available to patients who preferred not to participate in a group, or whose schedules did not allow participation.
Figure 1.
Orientation
Prospective CGT patients participated in two formal orientation meetings. The first provided an opportunity for patients to meet as a group and interact with each other and with the treatment team. Patients introduced themselves and shared their concerns about HCV disease and treatment. Members of the treatment team presented a brief overview of the HCV epidemic and its impact on drug users, the natural history of HCV, risks and benefits of treatment, and expected treatment outcomes. The CGT protocol was discussed in detail, including group format, expectations of attendance and confidentiality, and medications and treatment schedules.
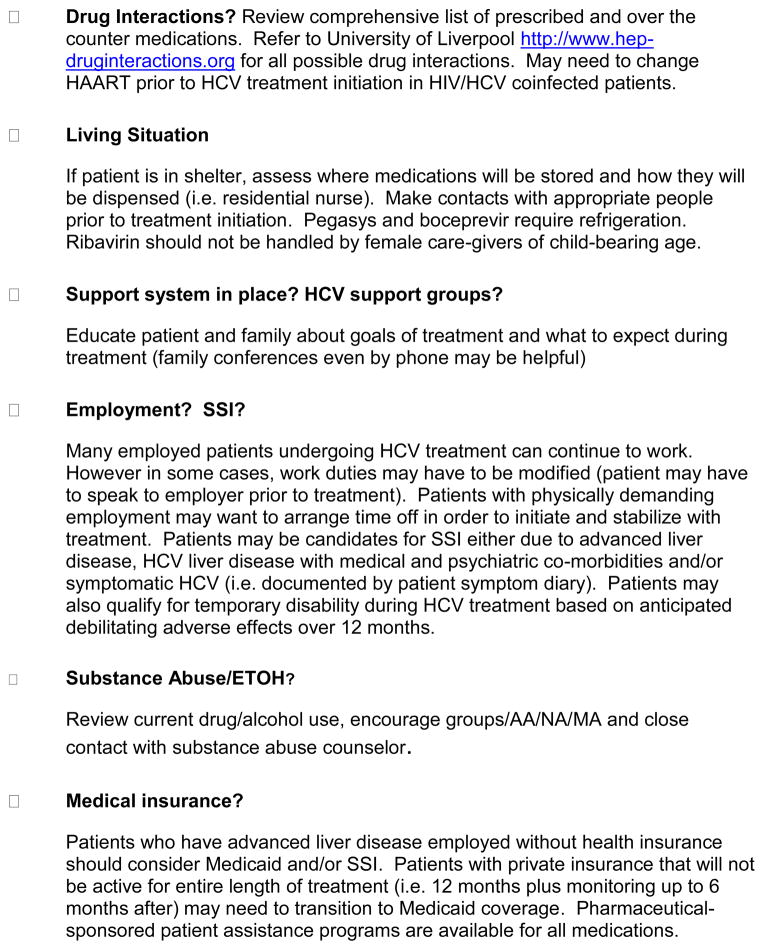
In the second orientation meeting, the CGT protocol and confidentiality issues were reviewed, and a group treatment contract (figure 2) was read aloud by patients and signed. Additionally, medication side effects and general management strategies wre reviewed by providers.
Figure 2.
Group Format
Groups were scheduled for one hour. Prior to each group, one provider reviewed labs and made decisions regarding dose adjustments to interferon and ribavirin as well as initiation or adjustment of adjunct hematologic growth factors. A peer educator was delegated to set up the group room with coffee and snacks. Patients typically began to gather 30 minutes before the official start for refreshments and conversation.
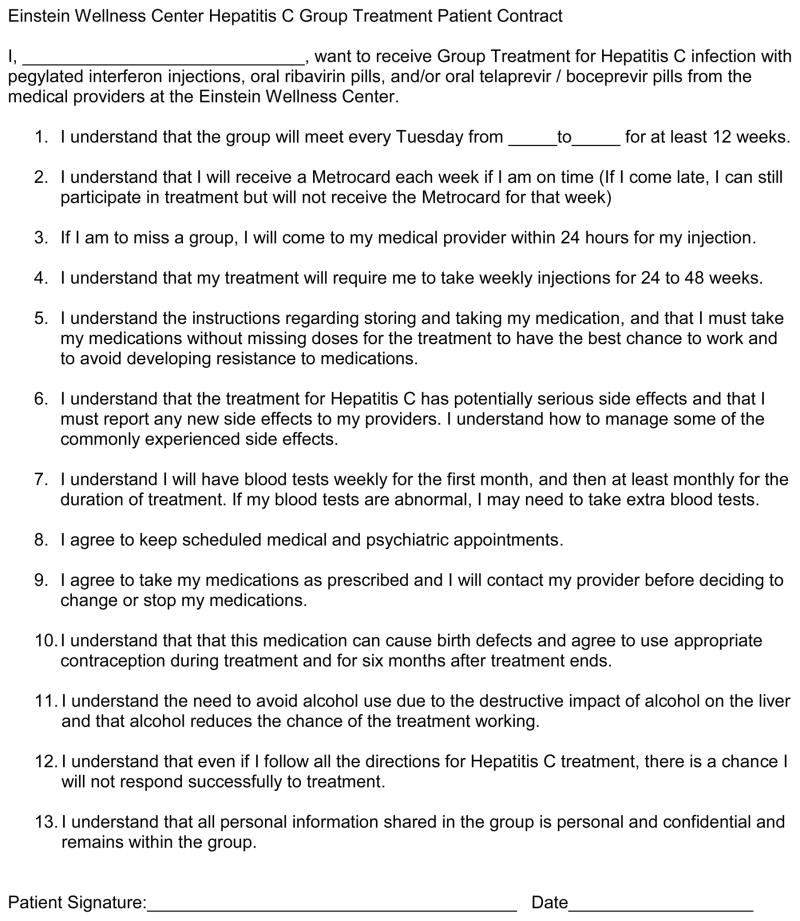
During the first half hour informal group discussion continued as patients completed side effect inventory sheets (figure 3). At the same time, a provider conducted brief “individual visits” in a corner of the conference room. During individual visits, vital signs including weight were reviewed and a brief interview was conducted addressing laboratory values and adherence to medication. Significant or new adverse effects were addressed, interferon and growth factor injections administered, and prescriptions provided. The second half hour was dedicated to a provider-facilitated formal group discussion.
Figure 3.
The facilitated group discussion began with a hand raising survey of how group participants were faring in treatment, with possible responses ranging from “terrible” to “no problem”. Individual experiences of adverse effects were shared, and the group members provided mutual support and practical suggestions for symptom management. Patients who had completed or were further along in their treatment shared their experiences and advice. Discussion topics varied, and have included specific side effect management, HCV facts (such as the difference between of relapse and reinfection), and the stigma associated with HCV. The group concluded with a 5–10 minute guided meditation exercise.
Patients were encouraged to bring their family members and friends to the group for support and education. In addition, the group hosted interested visitors such as prospective patients, substance abuse counselors, medical students, medical residents, and providers from other institutions. Visitors provided an opportunity for the group members to recount their treatment experiences and to take on the roles of mentor and teacher.
Treatment Regimens
During the period of the program to date, all patients have received combination therapy with ribavirin (800–1200 mg PO daily in divided dose, based on weight or genotype) and pegylated interferon alpha 2a (180 mcg injected subcutaneously once a week). For patients treated without direct-acting antiviral agents, treatment duration was 48 weeks for patients infected with genotype 1 and for HIV positive patients, and 24 weeks for HIV negative patients infected with genotypes 2 or 3. Patients discontinued treatment at 12 weeks if an early viral response (EVR) was not achieved.
Interferon injections were administered by providers in the group setting. Patients were either administered ribavirin (and protease inhibitor) as directly observed therapy (DOT) at the methadone medication window, or self administered their oral medications. All patients initiated HCV treatment as part of our standard on-site HCV treatment program, which includes directly-administered weekly interferon injections. All eligible patients were also invited to participate in an ongoing clinical trial which randomized patients initiating HCV treatment to either self-administered oral medications (ribavirin +/− protease inhibitor) or to receiving oral medications at the methadone window. Patients who did not participate in the clinical trial could choose DOT or self administration of oral medications.
In May, 2011, the FDA approved two protease inhibitors, telaprevir and boceprevir, to be used in combination with pegylated interferon and ribavirin for the treatment of genotype-1 infected patients with chronic HCV. Both protease inhibitors add further complexity to HCV treatment as these medications must be taken three times daily, increase daily pill burden (up to 18 pills daily), and are taken with food. Telaprevir must be taken with 20 grams of fat, and is associated with novel side effects (including rash and anal discomfort), and additive side effects (gastrointestinal symptoms and anemia). Boceprevir is associated with dysgeusia and additive anemia, and is started after a 4 week lead-in period with pegylated interferon and ribavirin (Ghany, Nelson, Strader, Thomas, & Seeff, 2012).
Incentives
Patients received weekly metro cards worth $4.50 for the first 12 weeks of treatment as an incentive for on-time arrival to group. Lunch was provided for patients at treatment initiation, and at 4 and 12 weeks. At the completion of treatment (24 or 48 weeks) a ceremony was held and certificates of appreciation were awarded. Incentives were funded in part by a two New York State-funded grant programs and through an unrestricted industry-funded grant.
Group Duration
We originally planned the CGT intervention for the first 12 weeks of HCV treatment, with patients who achieved EVR returning to their individual providers for completion of office based treatment. However, we found that almost all patients who were eligible to continue treatment wanted to continue CGT for the full duration. This change allowed groups to overlap, facilitating interaction between patients at different stages of treatment. In addition, HCV treatment “graduates” are able to return to share experiences and support patients still undergoing treatment.
Collaborative management and charting
Initially, management of group treatment was shared between all clinic providers (MDs and physician assistants). As the program continued, two providers at each site continued to manage the groups on a regular basis. One provider was primarily responsible for reviewing lab work prior to the group and making treatment decisions, with expert HCV mentoring available by experienced internists and hepatologists. A psychiatrist was also available for consultation and for urgent walk in appointments. Peer educators provided social support both during the group and outside of the group in informal settings. Substance abuse counselors met with patients for substance abuse and general counseling sessions at least monthly, and provided additional support and interventions as needed. The clinic medical assistant was instrumental in scheduling and obtaining bloodwork, and often communicated her observations of patients’ mood and overall well-being to the rest of the treatment team. Charting was done using a template designed for HCV group treatment (available upon request).
Evaluation of CGT Program
We conducted a retrospective review of medical charts using a standardized chart review instrument for the first 27 patients initiating CGT for HCV between March 9, 2009 and October 15, 2010. In addition, we reviewed all charts of all 15 genotype-1 infected patients initiating CGT for HCV with triple therapy including direct-acting antiviral agents between August 2, 2011 and January 24, 2012. This study was approved by the Albert Einstein College of Medicine Committee on Clinical Investigations.
Definitions of key outcomes and variables
The main outcome variables were the following. End of treatment response or ETR was defined as undetectable viral load at the end of treatment. Sustained viral response or SVR was defined as undetectable viral load 24 weeks after the end of treatment. For patients initiating treatment with pegylated interferon and ribavirin, early viral response or EVR was defined as undetectable viral load or 2 log decrease in viral load at 12 weeks into treatment. For patients initiating treatment with directing-acting antiviral agents, extended rapid viral response was defined as undetectable viral load at both weeks 4 and 12 (telaprevir) or at both weeks 8 and 24 (boceprevir). Reasons for early treatment discontinuation were evaluated by chart review. Key variables included psychiatric diagnoses, drug use prior to and during HCV treatment. Psychiatric diagnoses were determined through review of admission history and physical, most recent annual history and physical, progress notes and problem list. Recent drug use was defined as at least one positive urine toxicology report (opioid or cocaine) in the 6 months preceding HCV treatment initiation. Active drug use was defined as any positive urine toxicology result within one month of HCV treatment initiation. Drug use during treatment was defined as any positive urine toxicology during the period of HCV treatment.
Results
Pegylated interferon and ribavirin (n=27)
All CGT patients had a history of heroin addiction, and 26 were enrolled in our methadone maintenance treatment program. Patient characteristics are summarized in Table 1. All had Medicaid insurance, 67% were Latino, 62% had current psychiatric illness, 52% were current drug users, and 30% were HIV co-infected.
Table 1.
Characteristics of 42 opioid-dependent patients treated for HCV with concurrent group treatment
| Characteristic | Peg/RBV (n=27) | Peg/RBV/PI (n=15) |
|---|---|---|
| Age, mean (sd) | 49 (5.0) | 48 (8.5) |
| Gender, n (%) | ||
| Male | 16 (59) | 12 (80) |
| Female | 11 (41) | 3 (20) |
| Race/Ethnicity, n (%) | ||
| Latino | 18 (67) | 14 (93) |
| African American | 6 (22) | 1 (7) |
| Caucasian | 3 (11) | 0 (0) |
| Psychiatric illness, n (%)a | ||
| No current psychiatric illness | 10 (37) | 1 (7) |
| Current psychiatric illness | 17 (62) | 14 (93) |
| Depression | 16 (59) | 10 (67) |
| Anxiety | 4 (15) | 4 (27) |
| Psychosis | 8 (30) | 4 (27) |
| Post-traumatic stress disorder | 1 (4) | 1 (7) |
| Bipolar disorder | 1 (4) | 2 (13) |
| Prescribed psychiatric medication (pre-HCV treatment) | 21 (78) | 9 (60) |
| Source of Psychiatric Care | ||
| Psychiatrist | 18 (67) | 10 (67) |
| Primary Care Provider | 4 (15) | 1 (7) |
| No psychiatric care | 5 (19) | 4 (27) |
| Drug use within 180 days of treatment initiation, n (%)b | ||
| Any positive urine toxicology | 15 of 26 (58) | 8 of 15 (53) |
| Opioid positive urine toxicology | 11 of 26 (42) | 7 of 15 (47) |
| Cocaine positive urine toxicology | 11 of 26 (42) | 6 of 15 (40) |
| Opioid and cocaine positive urine toxicology | 7 of 26 (27) | 5 of 15 (33) |
| Drug use within 30 days of treatment initiation, n (%)b | ||
| Any positive urine toxicology | 8 of 25 (32) | 2 of 15 (13) |
| Opioid positive urine toxicology | 4 of 25 (16) | 2 of 15 (13) |
| Cocaine positive urine toxicology | 6 of 25 (24) | 1 of 15 (7) |
| Opioid and cocaine positive urine toxicology | 2 of 25 (8) | 1 of 15 (7) |
| HCV genotype, n (%) | ||
| Genotype 1 | 18 (67) | 15 (100) |
| Genotype 2 or 3 | 9 (33) | 0 (0) |
| HCV Viral Load (IU/ml), n (%) | ||
| ≥800,000 IU/ml | 14 (52) | 8 (53) |
| < 800,000 IU/ml | 13 (48) | 7 (47) |
| HIV status, n (%) | ||
| HIV− | 19 (70) | 15 (100) |
| HIV+ | 8 (30) | 0 (0) |
depression, anxiety disorder, psychotic disorder, post-traumatic stress disorder, and/or bipolar disorder
missing data
Almost all (89%) attended 100% of CGT sessions in the first 12 weeks of treatment. One patient left the group for inpatient drug treatment, but continued his HCV treatment during the inpatient stay, and returned to the group. Only 11% (n=3) discontinued treatment within the first 12 weeks because of adverse events, including anemia, psychiatric instability, and liver decompensation that resolved after treatment was stopped. Two additional patients discontinued treatment early due to virological non-response.
CGT was acceptable to all patients. No patient participating in CGT expressed discomfort with receiving medical care in a group setting, including taking of vital signs, receiving injections, or sharing personal experiences (e.g. side effects of rash, hair loss, fatigue and depression). After the initial twelve weeks, patients were offered the choice of ongoing group treatment or completing treatment with individual office visits, and almost all (26 of 27 patients) chose to continue group treatment.
Final virological data was obtained on the first 27 patients who initiated CGT (Table 2). Overall, 78% of patients achieved EVR, 74% ETR, and 42% SVR. Of patients with genotype-1 infection, 44% achieved SVR. Only 13% (1 of 8) HIV/HCV coinfected patients achieved SVR. One coinfected patient who achieved an ETR died from lymphoma prior to assessment of SVR.
Table 2.
Final Outcomes of 27 opioid-dependent patients treated with pegylated interferon and ribavirin
| Peg/RBV (n=27) | |
|---|---|
| Early viral response (EVR), n (%) | 21 (78) |
| End of treatment response (ETR), n (%) | 20 (74) |
| Sustained viral response (SVR), n (%) | 11 (42) |
| Discontinued treatment early, n (%) | 3 (11) |
Fifteen out of 26 patients (58%) had positive urine toxicologies during antiviral treatment, including 7 (27%) with opiates, 11 (42%) with cocaine, and 3 (12%) with both opiates and cocaine. Urine toxicology data was unavailable for one patient.
Direct Acting Antiviral Agents (n=15)
Preliminary virologic data was obtained for the first 15 genotype-1 patients who initiated treatment with pegylated interferon, ribavirin, and protease inhibitor in the CGT model (Table 3). Fourteen initiated treatment with telaprevir and one with boceprevir (after a 4 week lead-in period). Patient characteristics are summarized in Table 1. Thirteen patients were methadone-maintained and two patients were maintained on buprenorphine. All were monoinfected, 93% were Latino, 93% had a current psychiatric disorder, 62% recently used illicit drugs, and 33% had cirrhosis. None were HIV-coinfected. Thirteen of fifteen patients (87%) had an undetectable viral load at 24 weeks. Four completed 24 weeks of treatment (extended rapid viral response) and all achieved sustained viral response. Three patients completed 48 weeks of treatment, all had an end of treatment response, and are awaiting determination of sustained viral response. One of these three patients discontinued telaprevir due to severe rash. Six patients remain on treatment with undetectable viral load at 24 weeks. Two subjects discontinued treatment for the following reasons: 1) >1000 IU/ml at 4 weeks and 2) incarcerated after 2 weeks.
Table 3.
Preliminary Outcomes of 15 opioid-dependent patients treated with pegylated interferon, ribavirin, and direct-acting antiviral agents
| Peg/RBV/DAA (n=15) | |
|---|---|
| <43 IU/ml viral load at week 4, n (%) | 13 (87) |
| Undetectable viral load (<7.1 IU/ml) at week 4, n (%) | 7 (47) |
| Undetectable viral load at weeks 4 and 12 (eRVR)*, n (%) | 7 (47) |
| Undetectable viral load at week 24, n (%) | 13 (87) |
| Discontinued treatment early, n (%) | 2 (13) |
| End of treatment response (ETR), n (%) | 7 of 9 (78) |
| Sustained viral response (SVR), n (%) | 4 of 6 (67) |
Overall, 8 patients achieved eRVR (including one on boceprevir – undetectable at weeks 8 and 24)
Seven out of 15 patients (47%) had positive urine toxicologies during antiviral treatment, including 5 (33%) with opiates, 5 (33%) with cocaine, and 3 (20%) with both opiates and cocaine.
Discussion
Our results are encouraging, showing that patients had high rates of retention in the group and low rates of treatment discontinuation. Rates of SVR for genotype-1 infected patients treated with pegylated interferon and ribavirin were similar to registration trials, and early virological results are promising for genotype-1 infected patients initiating treatment with direct-acting antiviral agents. This program builds on the results from investigators incorporating peer support groups into HCV treatment (Sylvestre et al., 2007; Grebely et al., 2007; Litwin et al., 2005). It is the first program to our knowledge to use concurrent group treatment (CGT) for HCV, in which patients simultaneously initiate and complete HCV treatment together within a group setting. In addition to the peer support found in our earlier models, CGT includes consistent ongoing patient education and problem solving opportunities through group leadership by healthcare providers. CGT provides patients with the opportunity to share concerns and solutions with patients at the same point in treatment as well as with others who have completed treatment. CGT allows efficient HCV treatment by both patients and providers as all elements of individual patients visits are delivered within the group setting. Patients were willing to receive injections in a group setting and were able to maintain confidentiality.
We learned several important lessons regarding the implementation of CGT among those receiving DAAs compared to those who did not. The group seemed to be even more important to alleviate anxiety and fears of newer treatments with novel and additive side effects (e.g. rash of telaprevir; increased nausea with DAAs). In general, it makes sense for patients to be initiating the same DAA as treatment regimens and algorithm differ significantly between telaprevir and boceprevir. Finally, formally trained peers did not have experience with DAAs, so the collective experience of the group became even more important. Finally, with complex treatment algorithms and frequent blood draws, the improved efficiency for providers became even more compelling.
CGT may enhance motivation and provide positive social support which may result in greater treatment retention. Low discontinuation rates compare favorably with other studies treating current and former drug users in settings that used support groups in multidisciplinary settings (Grebely et al., 2007; Litwin et al., 2009) CGT addresses many patient-related barriers that have contributed to low uptake and poor outcomes in the treatment of IDUs. Social support is built into the treatment model starting in the orientation sessions, as patients who may be socially isolated, mistrustful of medical authority, and/or ambivalent about treatment are reassured by the concurrent participation of their peers. The treatment group incorporates mutual aid, enabling patients to give as well as receive help for the duration of their treatment. Thus, patients take on a dual role of patient and role model, providing each other with motivation to succeed in treatment.
As observed by other investigators, peer support can serve to address and mitigate patients’ fears of negative side effects of treatment.(Sylvestre, 2005; Sylvestre & Zweban, 2007; Grebely et al., 2007; Grebely et al., 2010; Litwin et al., 2009) In facilitated discussions, side effects experienced by individuals are generalized and used as teaching points for effective side effect management. Patients discuss their treatment experiences with the group, receive practical and emotional support, and serve as role models for coping effectively with treatment related problems. Patients observe in their peers that side effects are normal in the context of HCV treatment, and not usually a reason to discontinue treatment.
Misconceptions regarding hepatitis C disease and treatment have been major barriers for IDUs, and educational interventions for HCV targeted to both opiate agonist treatment patients and staff may promote maximal participation and optimal treatment outcomes (Talal et al., 2010). Group treatment provides frequent opportunities for education. Weekly discussions facilitated by medical staff during group treatment sessions provide basic information about HCV to participants and visitors.
The CGT model may be particularly useful in treating IDUs at high risk for psychosocial or psychiatric instability as it allows for frequent contact and close observation of patients during treatment by both providers and members of the group. This facilitates frequent assessment of mood, psychosocial, and addiction issues and allows for rapid intervention when needed. Many patients continued to use drugs during HCV treatment. During recruitment and weekly treatment groups, providers highlighted that patients who were actively using drugs could be successfully treated (Hellard et al., 2009), and emphasized that both HCV and drug abuse or dependence should be addressed simultaneously. Providers also discussed the fact that only a minority of drug users who have been successfully treated are reinfected (Backmund et al., 2004). Group leaders highlighted that the key to successful treatment is adherence to groups, medications, and lab draws. Harm reduction education was also a discussion topic, and included counseling on safer injection strategies. Substance abuse treatment was not provided within the group, but was addressed individually with the medical provider and substance abuse counselor and in additional on-site recovery-oriented groups.
The majority (93%) of our patients were Latino or African American. Studies in real-world populations have shown suboptimal outcomes in these populations (Feurstadt et al., 2010). Thus far, outcomes of patients in CGT approach those seen in registration trials, despite the socioeconomic and ethnic characteristics of the patients. CGT may be a useful tool in helping to reduce disparities in HCV treatment.
Overall, only 31% of patients treated were women. In the first CGT group, a significant proportion of patients were women (5 out of 12; 42%) but in subsequent groups men outnumbered women. However, similar rates of women in treatment (29%) were reported in another study of HCV treatment in the context of a methadone maintenance program (Litwin et al., 2009). It is possible that women may feel less comfortable in treatment groups if there are not enough women, or that they are less likely to be treated for HCV for other reasons. Further work is needed to examine optimal characteristics of groups. It is also possible that the low proportion of women in some groups may be related to our modest sample size.
There were several limitations to our study. The sample size was small and lacked a control group. Consequently, the results obtained with our group treatment model should be verified with larger randomized studies that include relevant control groups. Secondly, the results may not generalize to other drug treatment settings. Most methadone maintenance treatment programs do not have on-site medical treatment, experienced HCV providers, or an established HCV program (Brown et al., 2006). Concurrent enrollment of patients in a clinical trial which measured adherence at monthly intervals may have provided additional social support. Finally, with the increased complexity of triple therapy (Ghany et al., 2011), the CGT model may require further refinement.
Our study demonstrates that a novel program of concurrent group HCV treatment can be acceptable and effective in the context of a multidisciplinary drug treatment center. The CGT model addresses multiple barriers for people in treatment for opioid dependence with high rates of mental illness, ongoing illicit drug use, and low social support by maximizing educational and mutual aid opportunities.
On-site programs that can successfully engage active current and former drug users in HCV treatment and maximize retention and adherence will be increasingly important in the coming decade as new antiviral medications with the potential for resistance are added to the standard regimen of interferon and ribavirin. Concurrent group medical treatment of HCV may help to realize the promise of improved outcomes for complex patients and reduce the projected burden of disease for society. Given the numerous challenges faced in the treatment of HCV in real-world settings (Feurstadt et al., 2010), further investigation of the CGT model in a variety of settings is merited. Future effectiveness studies should investigate the effect of group medical treatment on adherence, treatment completion, resistance, and sustained virological response. Finally, future studies should also investigate the costs and cost-effectiveness of group HCV medical treatment.
Acknowledgments
The Division of Substance Abuse is funded in part by contract C-002464 from the New York State Office of Alcoholism and Substance Abuse Services. The HCV Program has received funding from the New York State Department of Health AIDS Institute – “Expanding the Capacity to Provide Hepatitis C Care and Treatment); the New York State Department of Health and Centers for Disease Control and Prevention grant (CDC U50 CCU22419201); and an unrestricted grant from Genentech – a member of the Roche group. Dr. Litwin is supported by the National Institute on Drug Abuse (NIH K23 022454) and the Robert Wood Johnson Foundation Faculty Scholar Program. This study was also supported by the National Institutes of Health (NIH R25 DA 14551) and a Center for AIDS Research Grant (NIH P30 A151519) awarded to Albert Einstein College of Medicine from the National Institutes of Health. We would like to acknowledge Sarah Church, Lauren Cockerham-Colas, Zenobia Colon, Jennifer Hidalgo, Nydia Lopez, Thomas McQuaid, Nancy Pagan, Kelly Ramsey, Sheila Reynoso, Dina Rodriguez, Brenda Spikes, and HCV Peers for their roles in the program. We would like to thank all DoSA medical providers, staff, and patients who participated in this treatment program. Dr. Litwin has served on the advisory board for Vertex Pharmaceuticals and Merck Pharmaceuticals.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States 1999 through 2002. Annals of Internal Medicine. 2006;138:187–190. doi: 10.7326/0003-4819-144-10-200605160-00004. [DOI] [PubMed] [Google Scholar]
- Backmund M, Meyer K, Edlin B. Infrequent reinfection after successful treatment for hepatitis C virus infection in injection drug users. Clin Infect Dis. 2004;39(10):1540–1543. doi: 10.1086/425361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backus LI, Boothroyd DB, Phillips BR, Mole LA. Predictors of response of U.S. veterans to treatment for the hepatitis C virus. Hepatology. 2007;46:37–47. doi: 10.1002/hep.21662. [DOI] [PubMed] [Google Scholar]
- Bini EJ, Brau N, Currie S, et al. Prospective multicenter study of eligibility for antiviral therapy among 4,084 U.S. veterans with chronic hepatitis C virus infection. Am J Gastroenterol. 2005;100:1772–1779. doi: 10.1111/j.1572-0241.2005.41860.x. [DOI] [PubMed] [Google Scholar]
- Bronson D, Maxwell R. Shared medical appointments: increasing patient access without increasing physician hours. Cleveland Clinic Journal of Medicine. 2008;71:369–377. doi: 10.3949/ccjm.71.5.369. [DOI] [PubMed] [Google Scholar]
- Brown LS, Jr, Kritz SA, Goldsmith RJ, Bini EJ, Rotrosen J, Baker S, Robinson J, McAuliffe P. Characteristics of substance abuse treatment programs providing services for HIV/AIDS, hepatitis C virus infection, and sexually transmitted infections: the National Drug Abuse Treatment Clinical Trials Network. Journal of Substance Abuse Treatment. 2006;30:315–21. doi: 10.1016/j.jsat.2006.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clanon K, Mueller J, Harank M. Integrating treatment for hepatitis C virus infection into an HIV clinic. Clinical Infectious Diseases. 2005;16:S362–S366. doi: 10.1086/427454. [DOI] [PubMed] [Google Scholar]
- Cullen W, Kelly Y, Stanley J, Langton D, Bury G. Experience of hepatitis C among current or former heroin users attending general practice. Irish Medical Journal. 2005;98:73–4. [PubMed] [Google Scholar]
- Davis GL, Rodriguez JR. Treatment of chronic hepatitis C in active drug users. New England Journal of Medicine. 2001;345:215–217. doi: 10.1056/NEJM200107193450312. [DOI] [PubMed] [Google Scholar]
- Diaz T, Des Jarlais DC, Vlahov D, Perlis TE, Edwards V, Friedman SR, Rockwell R, Hoover D, Williams IT, Monterroso ER. Factors associated with prevalent hepatitis C: differences among young adult injection drug users in lower and upper Manhattan, New York City. American Journal of Public Health. 2001;9:23–30. doi: 10.2105/ajph.91.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doab A, Treloar C, Dore GJ. Knowledge and attitudes about treatment for hepatitis C infection and barriers to treatment among current infection drug users in Australia. Clinical Infectious Diseases. 2005;40:2313–S320. doi: 10.1086/427446. [DOI] [PubMed] [Google Scholar]
- EASL Clinical Practice Guidelines. Management of hepatitis C virus infection - European Association for the Study of the Liver. Journal of Hepatology. 2011;55(2):245–264. doi: 10.1016/j.jhep.2011.02.023. [DOI] [PubMed] [Google Scholar]
- Edelman D, Fredrickson S, Weinberger M, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Annals of Internal Medicine. 2010;152:689–696. doi: 10.7326/0003-4819-152-11-201006010-00001. [DOI] [PubMed] [Google Scholar]
- Edlin BR, Seal KH, Lorvick J, Kral AH, Ciccarone DH, Moore LD, et al. Is it justifiable to withhold treatment for hepatitis C from illicit-drug users. New England Journal of Medicine. 2001;345:211–5. doi: 10.1056/NEJM200107193450311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlin B, Kresina T, Cargill V, et al. Overcoming barriers to prevention, care, and treatment of hepatitis C in illicit drug users. Clinical Infectious Diseases. 2005;40:S276–S285. doi: 10.1086/427441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falck-Ytter Y, Kale H, Mullen K, Sarbah S, Sorescu L, McCullough A. Surprisingly small effect of antiviral treatment in patients with hepatitis C. Annals of Internal Medicine. 2002;136:288–292. doi: 10.7326/0003-4819-136-4-200202190-00008. [DOI] [PubMed] [Google Scholar]
- Feuerstadt P, Bunim AL, Garcia H, Karlitz JJ, Massoumi H, Thosani AJ, Pellecchia A, Wolkoff AW, Gaglio PJ, Reinus JF. Effectiveness of hepatitis C treatment with pegylated interferon and ribavirin in urban minority patients. Hepatology. 2010;51:1137–1143. doi: 10.1002/hep.23429. [DOI] [PubMed] [Google Scholar]
- Fishbein D, Yungtai L, Reinus JM, Klein R. Factors associated with successful referral for clinical care of drug users with chronic hepatitis C who have or are at risk for HIV infection. Journal of Acquired Immune Deficiency Syndromes. 2004;37:1367–1375. doi: 10.1097/01.qai.0000131932.21612.49. [DOI] [PubMed] [Google Scholar]
- Ghany MG, Strader DB, Thomas DL, Seeff LB. Diagnosis, management and treatment of hepatitis C, an update. Hepatology. 2009;49:1335–1374. doi: 10.1002/hep.22759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghany MG, Nelson DR, Strader DB, Thomas DL, Seeff LB. An Update on Treatment of Genotype 1 Chronic Hepatitis C Virus Infection: 2011 Practice Guidelines by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:1422–1444. doi: 10.1002/hep.24641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gidding HF, Law MG, Amin J, et al. Hepatitis C treatment outcomes in Australian clinics. Med J Aust. 2012;196(10):633–637. doi: 10.5694/mja12.10014. [DOI] [PubMed] [Google Scholar]
- Grebely J, Raffa J, Tyndall M, et al. Low uptake of treatment for hepatitis C virus infection in a large community-based study of inner city residents. Journal of Viral Hepatitis. 2009;16:352–358. doi: 10.1111/j.1365-2893.2009.01080.x. [DOI] [PubMed] [Google Scholar]
- Grebely J, Genoway K, Khara M, et al. Treatment uptake and outcomes among current and former injection drug users receiving directly observed therapy within a multidisciplinary group model for the treatment of hepatitis C virus infection. International Journal of Drug Policy. 2007;18:437–443. doi: 10.1016/j.drugpo.2007.01.009. [DOI] [PubMed] [Google Scholar]
- Grebely J, Petoumenos K, Matthews G, et al. Factors associated with uptake of treatment for recent hepatitis C virus infection in a predominantly injecting drug user cohort: The ATAHC Study. Drug & Alcohol Dependence. 2010;107:244–249. doi: 10.1016/j.drugalcdep.2009.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grebely J, Knight E, Genoway KA, et al. Optimizing assessment and treatment for hepatitis C virus infection in illicit drug users: a novel model incorporating multidisciplinary care and peer support. Eur J Gastroenterol Hepatol. 2011;22(3):270–277. doi: 10.1097/meg.0b013e32832a8c4c. [DOI] [PubMed] [Google Scholar]
- Guadagnino V, Trotta M, Montesano F, et al. Effectiveness of a multi-disciplinary standardized management model in the treatment of chronic hepatitis C in drug addicts engaged in detoxification programmes. Addiction. 2007;102:423–431. doi: 10.1111/j.1360-0443.2006.01698.x. [DOI] [PubMed] [Google Scholar]
- Jaber R, Braksmajer A, Trilling J. Group visits: a qualitative review of current research. Journal of the American Board of Family Medicine. 2006;19:276–290. doi: 10.3122/jabfm.19.3.276. [DOI] [PubMed] [Google Scholar]
- Hellard M, Sacks-Davis R, Gold J. Hepatitis C treatment for injection drug users: a review of the available evidence. Clin Infect Dis. 2009;49(4):561–573. doi: 10.1086/600304. [DOI] [PubMed] [Google Scholar]
- Kanwal F, Hoang T, Spiegel BM, et al. Predictors of treatment in patients with chronic hepatitis C infection – role of patient versus nonpatient factors. Hepatology. 2007;46(6):1741–1749. doi: 10.1002/hep.21927. [DOI] [PubMed] [Google Scholar]
- Kramer JR, Kanwal F, Richardson P, Giordano TP, Petersen LA, El-Serag HB. Importance of patient, provider, and facility predictors of hepatitis C virus treatment in veterans: a national study. Am J Gastroenterol. 2011;106:483–491. doi: 10.1038/ajg.2010.430. [DOI] [PubMed] [Google Scholar]
- Leshner AI. Introduction to the special issue: The National Institute on Drug Abuse’s (NIDA’s) Drug Abuse Treatment Outcome Study (DATOS) Psychology of Addictive Behaviors. 1997;11:211–215. [Google Scholar]
- Litwin A, Soloway I, Gourevitch M. Integrating services for injection drug users infected with hepatitis C virus with methadone maintenance treatment: challenges and opportunities. Clinical Infectious Diseases. 2005;40:S339–S34. doi: 10.1086/427450. [DOI] [PubMed] [Google Scholar]
- Litwin A, Harris K, Nahvi S, et al. Successful treatment of chronic hepatitis C with pegylated interferon in combination with ribavirin in a methadone maintenance treatment program. Journal of Substance Abuse Treatment. 2009;37:32–40. doi: 10.1016/j.jsat.2008.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ly KN, Xing J, Monina Klevens R, Jiles RB, Ward JW, Holmberg SD. The increasing burden of mortality from viral hepatitis in the United States between 1999 and 2007. Annals Intern Med. 2012;156(4):271–278. doi: 10.7326/0003-4819-156-4-201202210-00004. [DOI] [PubMed] [Google Scholar]
- Magura S. The relationship between substance user treatment and 12-step fellowships: current knowledge and research questions. Substance Use & Misuse. 2007;42:343–360. doi: 10.1080/10826080601142071. [DOI] [PubMed] [Google Scholar]
- Meehan K, Hill J, Root L, Kimtis E, Patchett L, Noffsinger E. Group medical appointments: organization and implementation in the bone marrow transplantation clinic. Supportive Cancer Therapy. 2006;3:84–90. doi: 10.3816/SCT.2006.n.003. [DOI] [PubMed] [Google Scholar]
- Mehta SH, Lucas GM, Mirel LB, Torbenson M, Higgins Y, Moore RD, et al. Limited effectivelness of antiviral treatment for hepatitis C in an urban HIV Clinic. AIDS. 2006;20:2361–2369. doi: 10.1097/QAD.0b013e32801086da. [DOI] [PubMed] [Google Scholar]
- Mehta S, Genberg B, Astemborski J, et al. Limited uptake of hepatitis C treatment among injection drug users. Journal of Community Health. 2008;33:126–133. doi: 10.1007/s10900-007-9083-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill J, Rhodes L, Deyo R, Marlatt G, Bradley K. Mutual mistrust in the medical care of drug users. Journal of General Internal Medicine. 2002;17:327–333. doi: 10.1046/j.1525-1497.2002.10625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos R. Active ingredients of substance use-focused self-help groups. Addiction. 2008;103:387–396. doi: 10.1111/j.1360-0443.2007.02111.x. [DOI] [PubMed] [Google Scholar]
- Murrill C, Weeks H, Castrucci B, Weinstock H, Bell B, Spruill C, Gwinn M. Age-specific seroprevalence of HIV, hepatitis B virus, and hepatitis C virus infection among injection drug users admitted to drug treatment in 6 US cities. American Journal of Public Health. 2002;92:385–387. doi: 10.2105/ajph.92.3.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. Consensus Development Conference Statement Management of Hepatitis C: 2002 June 10–12, 2002. HIV Clinical Trials. 2003;4:55. doi: 10.1310/hct.2003.4.1.008. [DOI] [PubMed] [Google Scholar]
- Nelson PK, Mathers BM, Cowie B, et al. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews. Lancet. 2011;378:571–583. doi: 10.1016/S0140-6736(11)61097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noffsinger EB. Will drop-in medical appointments (DIGMAs) work in practice? Permanente Journal. 1999;3:58–67. [Google Scholar]
- Norman J, Walsh NM, Mugavin J, et al. The acceptability and feasibility of peer worker support role in community based HCV treatment for injecting drug users. Harm Reduction Journal. 2008;5:8. doi: 10.1186/1477-7517-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick DM, Tyndall MW, Cornelisse PG, Li K, Sherlock CH, Rekart ML, Strathdee SA, Currie SL, Schechter MT, O’Shaughnessy MV. Incidence of hepatitis C virus infection among injection drug users during an outbreak of HIV infection. Canadian Medical Association Journal. 2001;165:889–895. [PMC free article] [PubMed] [Google Scholar]
- Schackman BR, Teixeira PA, Beeder AB. Offers of hepatitis C care do not lead to treatment. Journal of Urban Health. 2007;84:455–458. doi: 10.1007/s11524-007-9180-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepard CW, Finelli L, Alter MJ. Global epidemiology of hepatitis C infection. Lancet Infect Dis. 2005;5:558–67. doi: 10.1016/S1473-3099(05)70216-4. [DOI] [PubMed] [Google Scholar]
- Stein MD, Maksad J, Clarke J. Hepatitis C disease among injection drug users: knowledge, percieved risk and willingness to receive treatment. Drug and Alcohol Dependence. 2001;61:211–5. doi: 10.1016/s0376-8716(00)00144-7. [DOI] [PubMed] [Google Scholar]
- Stephenson J. Former addicts face barriers to treatment for HCV. JAMA. 2001;285:1003–5. doi: 10.1001/jama.285.8.1003. [DOI] [PubMed] [Google Scholar]
- Strauss SM, Astone Twerell J, Munoz-Plaza CE, Des Jarlais DC, Gwadz M, Hagan H, Osborne A, Rosenblum A. Drug treatment program patients’ hepatitis C virus (HCV) education needs and their use of available HCV education services. BMC Health Serv Res 2007. 2007 Mar 8;7:39. doi: 10.1186/1472-6963-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMSHA) Results from the 2003 National Survey on Drug Use and Health: National Findings. Office of Applied Studies; Rockville, MD: 2004. [Google Scholar]
- Sylvestre D. Treating hepatitis C virus infection in active substance users. Clinical Infectious Diseases. 2005;40:S321–S324. doi: 10.1086/427447. [DOI] [PubMed] [Google Scholar]
- Sylvestre D, Zweben J. Integrating HCV services for drug users: a model to improve engagement and outcomes. International Journal of Drug Policy. 2007;18:406–410. doi: 10.1016/j.drugpo.2007.01.010. [DOI] [PubMed] [Google Scholar]
- Talal AH, et al. Assessment of hepatitis C virus attitudes towards treatment among methadone maintenance treatment program staff. Poster presented at the 61st Annual Meeting of the American Association for the Study of Liver Diseases; Boston, MA. October 30–November 3, 2010.2010. [Google Scholar]
- Treloar C, Holt M. Drug treatment client’s readiness for hepatitis C treatment: implications for expanding treatment services in drug and alcohol settings. Australian Health Review. 2008;32:570–576. doi: 10.1071/ah080570. [DOI] [PubMed] [Google Scholar]
- Trento M, Passera P, Porta M, et al. Group visits improve metabolic control in type 2 diabetes. Diabetes Care. 2001;24:995. doi: 10.2337/diacare.24.6.995. [DOI] [PubMed] [Google Scholar]
- Walley AY, White MC, Kushel MB, et al. Knowledge of and interest in hepatitis C treatment at a methadone clinic. J Subst Abuse Treat. 2005;28:181–187. doi: 10.1016/j.jsat.2004.12.004. [DOI] [PubMed] [Google Scholar]
- Wong JB, McQuillan GM, McHutchison JG, Poynard T. Estimating future hepatitis C morbidity, mortality and cost in the United States. American Journal of Public Health. 2000;90:1562–1569. doi: 10.2105/ajph.90.10.1562. [DOI] [PMC free article] [PubMed] [Google Scholar]