Abstract
Background
Adolescent women have a high risk of unintended pregnancy. Currently, there are little data about their choice to initiate long-acting reversible contraception (LARC).
Study Design
We evaluated the association of age and preference for a LARC vs. a non-LARC method among adolescent participants in the Contraceptive CHOICE Project, comparing those aged 14–17 years to adolescents aged 18–20 years. We then analyzed the association between age and choice of the implant vs. the intrauterine device (IUD) among adolescents.
Results
Of the 5086 women enrolled, 70% (n=3557) of participants chose a LARC method. Among adolescents aged 14–20 years, 69% of 14–17-year-olds chose LARC, while 61% of 18–20-year-olds chose LARC (relative risk 1.16, 95% confidence interval 1.03–1.30). Among adolescents choosing a LARC method, 63% (n=93/148) of the 14–17-year-olds chose the implant, whereas 71% (n=364/510) of the 18–20-year-olds chose the IUD.
Conclusion
Long-acting reversible contraception use is clearly acceptable and common among adolescents enrolled in the Contraceptive CHOICE Project, with the younger group being most interested in the implant.
Keywords: Adolescent contraception, Intrauterine device, Contraceptive implant, Adolescent pregnancy, Contraception
1. Introduction
Long-acting reversible contraception (LARC) does not rely on user adherence for effectiveness. Discontinuation of LARC methods requires consultation with a medical provider, which allows for additional counseling and discussion regarding side effects and contraceptive options. The three LARC methods available in the United States, the copper intrauterine device (Cu-IUD, Paragard®, Teva Women’s Health, Inc, Cincinnati, OH, USA), levonorgestrel intrauterine device (LNG-IUD, Mirena™, Bayer Healthcare Pharmaceuticals, Wayne, NJ, USA) and etonogestrel subdermal implant (Implanon™, Schering Corporation, Kenilworth, NJ, USA), are established as being safe and effective [1].
Prior research found these factors, safety and effectiveness, to be the most important criteria of young women choosing contraception [2,3]. Additionally, both IUDs have been shown to be acceptable to young women [4,5]. However, according to the recent National Survey of Family Growth, the most popular forms of contraception currently used by adolescents are condoms and withdrawal, followed by birth control pills [6]. All of these methods require active user compliance for pregnancy prevention, making them less reliable than LARC methods.
Despite the American Congress of Obstetricians and Gynecologists (ACOG) 2007 Committee Opinion recommending both the Cu-IUD and LNG-IUD for adolescents [7], many medical providers are reluctant to provide IUDs to young women. A study of California providers demonstrated that only 39% considered a teenager to be an appropriate IUD candidate [8]. Furthermore, most of the data concerning the available contraceptive subdermal implant in the United States come from clinical trials, which did not include women under the age of 18 years. Therefore, there is very little information about the use of IUDs and contraceptive implants by adolescents in the United States.
Another barrier to adolescents obtaining a LARC method is cost. Though the overall cost-effectiveness is high, patients are required to pay a high up-front fee in most private offices, and many free or low-cost clinics do not provide these methods.
The Contraceptive CHOICE Project is a longitudinal, observational study of women’s choice, use and continuation of currently available reversible contraception. Participants aged 14–45 years are offered all methods of reversible contraception at no cost to themselves for 3 years. The objective of this analysis was to estimate the association between adolescent age, choice of LARC vs. other contraceptive methods and preference for specific LARC method among the adolescent participants when the barriers of access from provider and cost are removed. Based on our collective clinical experience, we hypothesized that among the adolescent participants aged 14–20 years choosing a LARC method, the younger participants (age<18 years) will be more likely to choose the subdermal implant than participants aged 18–20 years.
2. Materials and methods
The CHOICE protocol was approved by the Washington University in St. Louis School of Medicine Human Research Protection Office prior to initiation of participant recruitment. A more detailed description of the methods of CHOICE has been previously described [9]. In the paragraphs below, we summarize the study design and analyses that are relevant to this specific research question.
The Contraceptive CHOICE Project, located in St. Louis, MO, is a prospective, observational study designed to remove financial barriers to effective contraception, promote the use of long-acting reversible methods of contraception (LARC) and evaluate use, satisfaction and continuation across both LARC and non-LARC methods in a cohort of 10,000 women. The LARC methods include the levonor-gestrel IUD, the copper IUD and the subdermal implant. The non-LARC methods include combined and progestin-only oral contraceptives, the transdermal contraceptive patch, the vaginal contraceptive ring, depot medroxyprogesterone acetate (DMPA) and barrier methods.
Enrollment began on August 1, 2007, and recruitment and follow-up are ongoing. Women interested in participating in CHOICE undergo an eligibility screen by trained staff. Inclusion criteria for CHOICE are as follows: age 14–45 years, residence in the St. Louis City or County or seeking services at designated recruitment sites, willingness to switch or initiate a new contraceptive method, sexual activity with a male partner or plans to become sexually active within 6 months and ability to consent in English or Spanish. Women who were surgically sterile, desired permanent sterilization or desired pregnancy within 1 year were excluded.
Enrollment is conducted in person by trained staff located at the recruitment location. Contraceptive counseling is provided to women prior to study enrollment in CHOICE. After hearing a standardized script regarding the effectiveness of LARC methods, participants are presented with evidence-based information about safety, effectiveness and risks and benefits of all reversible contraceptive methods. Counselors collect clinical information on each participant using a standardized form to identify conditions that may be a contraindication to a particular contraceptive method. Approval for the selected method is obtained from a clinician at the end of contraceptive counseling.
Following contraceptive counseling, study staff obtains written, informed consent for study participation. Assent is obtained for minors under 18 years, and the consent of one parent or legal guardian is obtained. Upon consent, the participant provides detailed contact information and self-collected specimens for sexually transmitted infection (STI) testing, and responds to a staff-administered structured baseline questionnaire. The questionnaire provides information about participant demographics, medical and reproductive history including sexual and obstetrical histories, and initial knowledge about the safety and effectiveness of available contraception methods. The participant receives her contraceptive method at the end of the enrollment session.
We performed a cross-sectional analysis of baseline data obtained during participant enrollment in the Contraceptive CHOICE Project (CHOICE). The data for this analysis were obtained from the baseline questionnaire of the first 5086 participants enrolled from August 1, 2007, through December 31, 2009. The inclusion criteria for our analysis were that the participants be 14–20 years of age. For the purpose of the analysis, they were categorized into two groups: 14–17- year-olds and 18–20-year-olds. Of the 5086 participants, 21% (n=1,054) were aged 14–20 years [4% (n=214) were aged 14–17 years and 17% (n=840) were aged 18–20 years]. Frequencies, percents, means and standard deviations were used to describe demographic characteristics. Univariate analysis was performed using χ2 tests and, when appropriate, Fisher’s Exact Tests for categorical variables as well as Student’s t test for continuous variables. Confounding was defined as either a greater than 10% relative change in the association between age and method choice with or without the covariate of interest in the model or prior evidence from the literature of a confounding effect. Confounders were included in the final multivariable model. Multivariable Poisson regression models with robust error variance were used to estimate relative risk (RR) and 95% confidence intervals (CIs) for the relationship between IUD and subdermal implant choice among the young women. This analytic approach provides an unbiased estimate of the RR when the outcome is common (>10%) [10,11].
p Values and RRs and 95% CIs were used to describe statistical significance. All analyses were performed using SAS 9.2 (SAS Institute, Cary, NC, USA) and STATA 10 (StataCorp LP, College Station, TX, USA).
To test the hypothesis that the young adolescents would choose the subdermal implant over the IUD more frequently than the older adolescents, we divided participants aged 14–20 years who chose a LARC method into two groups: 14–17-year-olds and 18–20-year-olds. Assuming an IUD acceptance rate of 30% in young women and an odds ratio of 1.5 for subdermal implant acceptance (relative to IUD), a sample size of approximately 920 women aged 14–20 years provides >80% power to address the difference in LARC choice in younger women.
3. Results
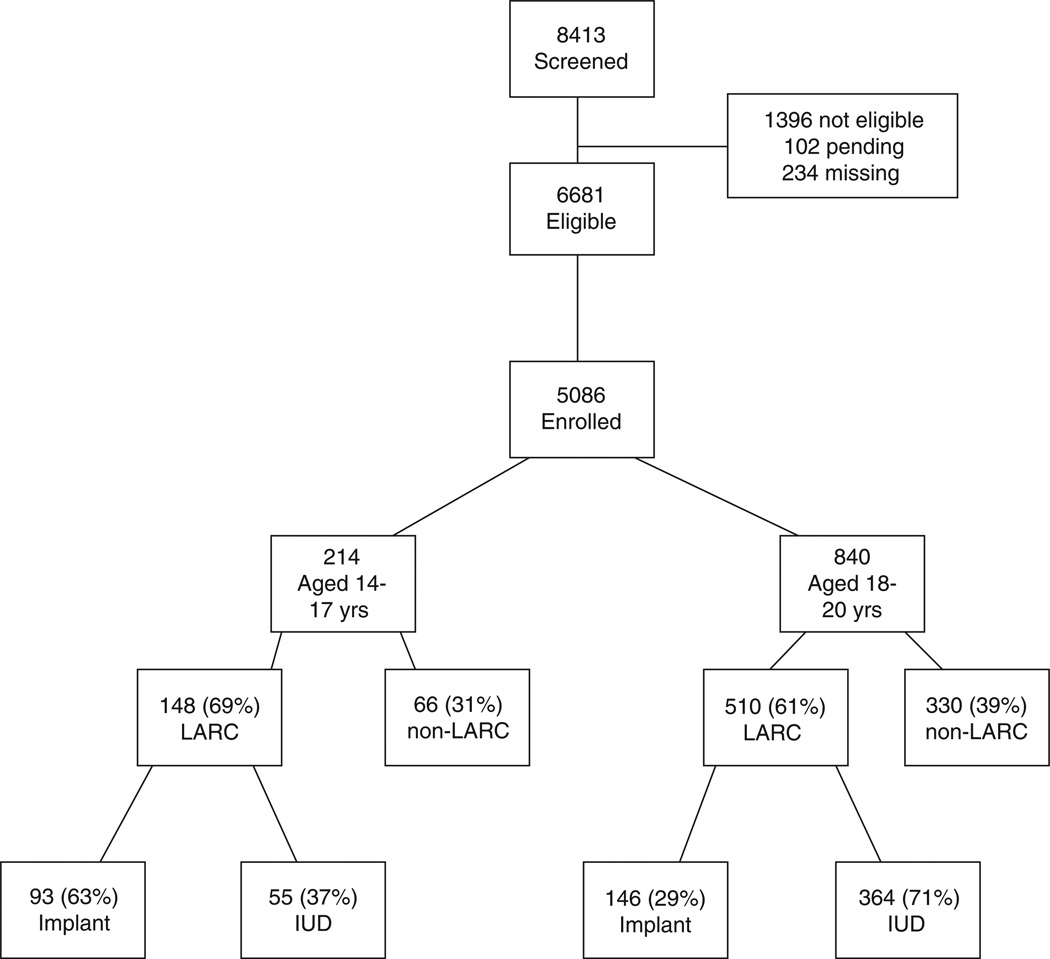
Fig. 1 illustrates participant screening, enrollment and method selection. Of the 5086 enrolled, 70% (n=3557) of participants chose a LARC method, 47.0% LNG-IUD, 11% the copper IUD and 12% the subdermal implant. Among the adolescents aged 14–20 years, 62% (658/1054) chose a LARC method. Of this group, 69% of those aged 14–17 years chose a LARC method, while 61% of those aged 18–20 years chose LARC (unadjusted RR=1.14, 95% CI 1.03–1.26). Other characteristics that varied between adolescents who chose LARC and those who chose a non-LARC method were race, education, receiving government support to meet basic needs, insurance status, history of unintended pregnancy and history of an STI (Table 1). We adjusted for race, education, receiving government support and history of unintended pregnancy in the final model because we considered these covariates clinically relevant. In the adjusted model, the RR that adolescents aged 14–17 years would choose a LARC method when compared to adolescents aged 18–20 years increased slightly to 1.16 (95% CI 1.03–1.30) (Table 2).
Fig. 1.
Enrollment flowchart.
Table 1.
Characteristics of 14–20-year olds choosing LARC vs. non-LARC methods (N=1054)
| LARC (n=658) Mean (SD) |
Non-LARC (n=396) Mean (SD) |
||
|---|---|---|---|
| Age | 18.4 (1.5) | 18.7 (1.4) | |
| Age at first pregnancy | 17.1 (1.7) | 17.5 (1.6) | |
| n (%) | n (%) | Univariate RR (95% CI) |
|
| Age category, years | |||
| 18–20 | 510 (61%) | 330 (39%) | Reference |
| ≤17 | 148 (69%) | 66 (31%) | 1.14 (1.03–1.26) |
| Hispanic | |||
| No | 625 (63%) | 367 (37%) | Reference |
| Yes | 33 (53%) | 29 (47%) | 0.84 (0.67–1.07) |
| Race | |||
| Black | 390 (67%) | 191 (33%) | 1.17 (1.06–1.30) |
| White | 209 (57%) | 156 (43%) | Reference |
| Other | 53 (52%) | 48 (48%) | 0.92 (0.75–1.13) |
| Education | |||
| ≤High school | 436 (69%) | 212 (31%) | Reference |
| ≥Some college | 222 (55%) | 184 (45%) | 0.81 (0.73–0.90) |
| Monthly income | |||
| None | 217 (67%) | 106 (33%) | Reference |
| $1–$800/month | 303 (60%) | 199 (40%) | 0.90 (0.81–1) |
| $800+/month | 124 (68%) | 60 (32%) | 1 (0.88–1.14) |
| Govt. support | |||
| No | 299 (54%) | 251 (46%) | Reference |
| Yes | 359 (71%) | 145 (29%) | 1.31 (1.19–1.44) |
| Insurance | |||
| None | 217 (61%) | 138 (39%) | 1.07 (0.96–1.21) |
| Private/military | 265 (57%) | 201 (43%) | Reference |
| Medicaid/disability | 163 (79%) | 43 (21%) | 1.39 (1.25–1.55) |
| Unintended pregnancy | |||
| 0 | 250 (51%) | 240 (49%) | Reference |
| 1 | 256 (69%) | 111 (31%) | 1.37 (1.22–1.53) |
| 2+ | 152 (78%) | 43 (22%) | 1.53 (1.36–1.71) |
| History of STI | |||
| No | 399 (60%) | 271 (40%) | Reference |
| Yes | 256 (68%) | 121 (32%) | 1.14 (1.04–1.25) |
| Monogamous with current partner | |||
| No | 56 (56%) | 44 (44%) | Reference |
| Yes | 600 (63%) | 352 (37%) | 1.13 (0.94–1.35) |
| Prior abortions | |||
| No | 498 (62%) | 301(38%) | Reference |
| Yes | 160 (63%) | 95(37%) | 1.01 (0.9–1.12) |
Table 2.
Relative risk that 14–20-year-olds will choose a LARC method over a non-LARC method: adjusted analysisa
| LARC vs. non-LARC (95% CI) |
|
|---|---|
| Age, years | |
| 18–20 | Reference |
| 14–17 | 1.16 (1.03–1.30) |
| Race | |
| Black | 1.08 (0.98–1.20) |
| White | Reference |
| Other | 0.95 (0.79–1.15) |
| Education | |
| ≤High school | Reference |
| ≥Some college | 0.92 (0.82–1.02) |
| Government support | |
| No | Reference |
| Yes | 1.20 (1.08–1.32) |
| Unintended pregnancy | |
| 0 | Reference |
| 1 | 1.28 (1.14–1.43) |
| 2+ | 1.43 (1.26–1.61) |
Adjusted for race, education, requires government support to meet basic necessities and history of unintended pregnancy.
Of the 658 adolescent participants who chose a LARC method, 148 were 14–17-year-olds and 510 were 18–20- year-olds. Of the 14–17-year-olds, 63% (n=93) chose the implant, whereas 29% (n=146) of the 18–20-year-olds chose the implant. In addition to age, we identified seven covariates in the univariate analysis that were significantly associated with selection of the implant (Table 3). Only history of an unintended pregnancy and prior oral contraceptive use changed the relationship between age and selection of implant by greater than 10%. When comparing the choice of implant vs. IUD between the two adolescent groups, we controlled for race, education, need of government support, history of unintended pregnancy and prior oral contraceptive use as we considered them clinically relevant. The RR that more adolescents aged 14–17 years would choose the contraceptive implant when compared to adolescents aged 18–20 years remained statistically significant (RRadj=1.67, 95% CI 1.34–2.07) (Table 4). Participants with a history of an unintended pregnancy were less likely to choose the implant, as were participants who had used oral contraceptives in the past. None of the knowledge questions were found to significantly confound the association between age and specific LARC method choice and were not included in the final multivariable model.
Table 3.
Characteristics of 14–20-year olds who chose a LARC method (n=658)
| IUDs n=419 Mean (SD) |
Implant n=239 Mean (SD) |
||
|---|---|---|---|
| Age | 18.8 (1.2) | 17.7 (1.8) | |
| Age at first pregnancy | 17.2 (1.7) | 16.9 (1.7) | |
| n (%) | n (%) | Univariate RR (95% CI) |
|
| Age category, years | |||
| 18–20 | 364 (71%) | 146 (29%) | Reference |
| 14–17 | 55 (37%) | 93 (63%) | 2.20 (1.82–2.64) |
| Hispanic | |||
| No | 398 (64%) | 227 (36%) | Reference |
| Yes | 21 (64%) | 12 (36%) | 1.00 (0.63–1.59) |
| Race | |||
| Black | 237 (61%) | 153 (39%) | 1.24 (0.98–1.57) |
| White | 143 (68%) | 66 (32%) | Reference |
| Other | 36 (68%) | 17 (32%) | 1.02 (0.65–1.58) |
| Education | |||
| ≤High school | 254 (58%) | 182 (42%) | Reference |
| ≥Some college | 165 (74%) | 57 (26%) | 0.62 (0.48–0.79) |
| Monthly income | |||
| None | 120 (55%) | 97 (45%) | Reference |
| $1–$800/month | 198 (65%) | 105 (35%) | 0.78 (0.63–0.96) |
| $801+/month | 90 (73%) | 34 (27%) | 0.61 (0.44–0.85) |
| Government support for basic needs | |||
| No | 185 (62%) | 114 (38%) | Reference |
| Yes | 234 (65%) | 125 (35%) | 0.91 (0.75–1.12) |
| Insurance | |||
| None | 139 (64%) | 78 (36%) | 1.24 (0.95–1.60) |
| Private | 188 (71%) | 77 (29%) | Reference |
| Medicare/disability | 88 (54%) | 75 (46%) | 1.58 (1.23–2.04) |
| Unintended pregnancy | |||
| 0 | 128 (51%) | 122 (49%) | Reference |
| 1 | 160 (62%) | 96 (38%) | 0.77 (0.63–0.94) |
| 2+ | 131 (86%) | 21 (14%) | 0.28 (0.19–0.43) |
| History of STI | |||
| No | 239 (60%) | 160 (40%) | Reference |
| Yes | 178 (70%) | 78 (30%) | 0.76 (0.61–0.95) |
| Monogamous with current partner | |||
| No | 41 (73%) | 15 (27%) | Reference |
| Yes | 376 (63%) | 224 (37%) | 1.39 (0.89–2.18) |
| Prior abortions | |||
| No | 302 (61%) | 196 (39%) | Reference |
| Yes | 117 (73%) | 43 (27%) | 0.68 (0.52–0.9) |
| Period length | |||
| Irregular | 31 (60%) | 21 (40%) | 1.18 (0.83–1.68) |
| Regular | 368 (66%) | 191 (34%) | Reference |
| Period heaviness | |||
| Light | 59 (68%) | 28 (32%) | 0.86 (0.62–1.20) |
| Moderate | 242 (63%) | 145 (37%) | Reference |
| Heavy | 93 (70%) | 40 (30%) | 0.80 (0.60–1.07) |
| Most recent method use | |||
| DMPA | |||
| No | 316 (66%) | 164 (34%) | Reference |
| Yes | 103 (58%) | 75 (42%) | 1.23 (1–1.53) |
| Oral contraceptives | |||
| No | 147 (54%) | 127 (46%) | Reference |
| Yes | 272 (71%) | 112 (29%) | 0.63 (0.51–0.77) |
| Patch | |||
| No | 346 (62%) | 210 (38%) | Reference |
| Yes | 73 (72%) | 29 (28%) | 0.75 (0.54–1.04) |
| Vaginal ring | |||
| No | 342 (61%) | 222 (39%) | Reference |
| Yes | 77 (82%) | 17 (18%) | 0.46 (0.30– 0.72) |
| Condom | |||
| No | 178 (64%) | 101 (36%) | Reference |
| Yes | 241 (64%) | 138 (36%) | 1.01 (0.82– 1.23) |
Table 4.
Relative risk that more 14–17 year olds will choose the implant than 18–20 year olds: adjusted analysis*
| Implant vs. IUD (95% CI) |
|
|---|---|
| Age, years | |
| 18–20 | Reference |
| 14–17 | 1.67 (1.34– 2.07) |
| Race | |
| Black | 1.14 (0.91– 1.42) |
| White | Reference |
| Other | 1.08 (0.69– 1.68) |
| Education | |
| ≤High school | Reference |
| ≥Some college | 0.77–(0.58– 1.01) |
| Government support | |
| No | Reference |
| Yes | 1.17 (0.97– 1.42) |
| Unintended pregnancy | |
| 0 | Reference |
| 1 | 0.74 (0.61– 0.91) |
| 2+ | 0.31 (0.20– 0.48) |
| Prior use of oral contraceptives | |
| No | Reference |
| Yes | 0.81 (0.66– 0.99) |
Adjusted for: race, education, requires government support to meet basic necessities, history of unintended pregnancy, and prior use of oral contraceptives.
4. Discussion
Adolescent participants in this study preferentially chose LARC methods over non-LARC methods when offered LARC methods and cost was removed as a barrier. Sixty-one percent to 69% of the adolescent women chose a LARC method. Whitaker et al. [12] found similar results when they studied young women’s attitudes toward IUDs; 51% of participants aged 14–18 years positively viewed IUDs after a brief educational session. Our findings provide evidence that adolescent women are interested in safe, effective contraception and have a high acceptance of LARC methods when offered when the barrier of cost is removed. By distinguishing between IUDs and the subdermal implant, our study demonstrates that younger women aged 14–17 years preferred the implant over the IUD.
Unfortunately, not all clinicians are comfortable providing IUD and implants to their adolescent patients. Many clinicians are not trained to insert the implant, which means that their adolescent patients will not have access to one of the safest and most effective contraceptive methods. Additionally, a recent survey of St. Louis providers, predominately physicians, indicated that only 31% of providers consider an IUD appropriate for teenagers, 50% would insert one for a 17- year-old with one child, and only 19% would insert one for a 17-year-old without any pregnancies [13]. Regardless of ACOG’s statement encouraging IUD use by teen women, even nulliparous ones, many physicians remain reluctant to recommend or insert IUDs in their adolescent patients.
Currently, the most popular forms of contraception used by adolescents are condoms and withdrawal, followed by birth control pills. The rhythm method also increased in popularity since 2002, with 17% using it in 2006–2008 [6]. Only 3.6% of women aged 15–19 years used the IUD, and the implant was not included as a separate method [14]. The use of less reliable methods likely contributes to the 80% unintended pregnancy rate of adolescent women aged 15–19 years [15].
Our participants are a convenience sample. They chose to be part of this research study and were motivated to prevent pregnancy. Therefore, our results may not be true for all young women. However, most clinicians have adolescent patients who are motivated to prevent pregnancy and appreciate a thorough discussion and provision of all available contraceptive methods, especially the most effective methods. Long-acting reversible contraception methods should be considered first-line contraceptive options and offered to adolescents.
Prior research has found IUDs to be the most cost-effective reversible contraceptive method [16]. The single rod implant was not included in previous contraception cost-effectiveness studies as it was not yet available in the United States. Unfortunately, the high up-front cost of LARC methods often prevents young women without insurance coverage from choosing these methods despite their cost-effectiveness over the life cycle of the method when compared to non-LARC methods.
After a steady decline in the past 15 years, the US adolescent pregnancy rate rose for the first time in 2006, increasing by 3% over the 2005 rate in women aged 15–19 years [17]. Part of this can be attributed to the fact that the most popular forms of contraception used by adolescents rely on correct use for effectiveness. Adolescent women want safe, effective contraception, but find barriers to access, both from their medical providers and the high up-front cost of the method. They rely on their clinician to give them complete and accurate information about all their options. Contraceptive counseling should include discussion of IUDs and the contraceptive implant for adolescents as these methods are acceptable, safe, and very effective.
Acknowledgments
This research was supported in part by (a) an anonymous foundation; (b) Midcareer Investigator Award in Women’s Health Research (K24 HD01298); (c) Clinical and Translational Science Awards (UL1RR024992) and (d) grant numbers KL2RR024994 and K3054628 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
References
- 1.Hatcher RA, Trussell J, Nelson AL, Cates W, Stewart FH, Kowal D, editors. Contraceptive technology. 19th ed. New York: Ardent Media, Inc; 2007. [Google Scholar]
- 2.Stanwood NL, Bradley KA. Young pregnant women’s knowledge of modern intrauterine devices. Obstet Gynecol. 2006;108:1417–1422. doi: 10.1097/01.AOG.0000245447.56585.a0. [DOI] [PubMed] [Google Scholar]
- 3.Grady WR, Klepinger DH, Nelson-Wally A. Contraceptive characteristics: the perceptions and priorities of men and women. Fam Plan Perspect. 1999;31:168–175. [PubMed] [Google Scholar]
- 4.Li CFI, Lee SSN, Pun TC. A pilot study on the acceptability of levonorgestrel-releasing intrauterine device by young, single, nullip-arous Chinese females following surgical abortion. Contraception. 2004;69:247–250. doi: 10.1016/j.contraception.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 5.Toma A, Jamieson MA. Revisiting the intrauterine contraceptive device in adolescents. J Pediat Adolesc Gynecol. 2006;19:291–296. doi: 10.1016/j.jpag.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Abma JC, Martinez GM, Copen CE. Teenagers in the United States: sexual activity, contraceptive use, and childbearing, National Survey of Family Growth 2006–2008. National Center for Health Statistics. [Accessed on June 11, 2010];Vital Health Stat. 2010 23(30) at http://www.cdc.gov/nchs/data/series/sr_23/sr23_030.pdf. [PubMed] [Google Scholar]
- 7.ACOG Committee opinion number 392. Obstet Gynecol. 2007;110:1493–1495. doi: 10.1097/01.AOG.0000291575.93944.1a. [DOI] [PubMed] [Google Scholar]
- 8.Harper C, Blum M, Thiel de Bocanegra H, et al. Challenges in translating evidence to practice: the provision of intrauterine contraception. Obstet Gynecol. 2008;111:1359–1369. doi: 10.1097/AOG.0b013e318173fd83. [DOI] [PubMed] [Google Scholar]
- 9.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203:115e1–115e7. doi: 10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mcnutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 11.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 12.Whitaker A, Johnson L, Harwood B, Chiappetta L, Crenin M, Gold M. Adolescent and young adult women’s knowledge of and attitudes toward the intrauterine device. Contraception. 2008;78:211–217. doi: 10.1016/j.contraception.2008.04.119. [DOI] [PubMed] [Google Scholar]
- 13.Madden T, Allsworth JE, Hladky KJ, Secura GM, Peipert JF. Intrauterine contraception in St. Louis: a survey of obstetrician and gynecologists’ knowledge and attitudes. Contraception. 2010;81:112–116. doi: 10.1016/j.contraception.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mosher WD, Jones J. Use of contraception in the United States: 1982–2008. National Center for Health Statistics. [Accessed on June 11, 2010];Vital Health Stat. 2010 23(29) at http://www.cdc.gov/nchs/data/series/sr_23/sr23_029.pdf. [PubMed] [Google Scholar]
- 15.Henshaw SK. Unintended pregnancy in the United States. Fam Plan Perspect. 1998;30:24–29. [PubMed] [Google Scholar]
- 16.Chiou CF, Trussell J, Reyes E, Knight K, et al. Economic analysis of contraceptives for women. Contraception. 2003;68:3–10. doi: 10.1016/s0010-7824(03)00078-7. [DOI] [PubMed] [Google Scholar]
- 17.Guttmacher Institute. U.S. teenage pregnancies, births, and abortions: national and state trends and trends by race and ethnicity. [Accessed on April 14, 2010]; at http://www.guttmacher.org/pubs/USTPtrends.pdf. [Google Scholar]