Abstract
The outcomes of a prospective consecutive study aimed at evaluating the visual and refractive benefit after cataract surgery with the implantation of the aspheric diffractive multifocal intraocular lens (IOL) Tecnis ZMB00 (Abbott Medical Optics) are reported. A total of 31 eyes of 19 patients (age range, 40 to 81 years) underwent phacoemulsification surgery with implantation of this aspheric multifocal IOL. At 6 months after surgery, postoperative spherical equivalent was within ±1.00 D in 96.8% of eyes, with 94.7% of patients presenting a postoperative binocular far LogMAR uncorrected visual acuity (UCVA) of 0.1 or better. Far best-corrected distance VA improved significantly (p < 0.01), with postoperative values of 0.1 or better in 96.8% of eyes. Postoperative near UCVA was 0.10 (equivalent to J1) or better in 93.55% of eyes. Furthermore, the IOL power was found to be very poorly correlated with the postoperative far LogMAR (r = 0.13) and near UCVA (r = 0.13). In conclusion, the aspheric diffractive multifocal IOL Tecnis ZMB00 provides a restoration of the far and near visual function after phacoemulsification surgery for cataract removal or presbyopia correction, which is predictable and independent from the optical power of the implanted IOL.
Key words: Diffractive intraocular lens, Multifocal intraocular lens, Tecnis, Spherical aberration
Multifocal Diffractive Technology
In the last years, sophisticated intraocular lens (IOL) designs, such as the multifocal and accommodating IOLs, with the ability of restoring distance, intermediate and near vision have been introduced in clinical practice [1]. The designs of multifocal IOLs are based on a number of optical concepts that are used to create multiple foci and therefore to generate simultaneous vision. Multizonal refractive, refractive rotationally asymmetric, diffractive and hybrid IOLs (the combination of refractive and diffractive elements) are the currently available options. The latest models of these types of IOLs have been shown to provide good distance and near functional vision without the patient having to wear corrective lenses [2, 3]. However, some optical side effects have been reported with some models of multifocal IOLs such as decreased contrast sensitivity, glare disability or halos [4, 5].
Multifocal diffractive technology uses a platform based on concentric rings in the posterior surface that form 2 primary focal points independent of pupil size, allowing a functional distance and near vision, respectively [6]. It has been shown that this multifocal design results in some optical contrast reduction that may explain some of the photic phenomena reported with some diffractive multifocal IOLs, but this situation can be avoided by minimizing the postoperative level of primary spherical aberration [7]. For this reason, aspheric diffractive multifocal IOLs were developed, which have been shown to provide excellent visual and refractive outcomes as well as a good postoperative optical and visual quality [2, 8]. We have recently conducted a study aimed at evaluating the visual and refractive benefit after cataract surgery with the implantation of one of the latest models of aspheric diffractive multifocal IOL, the Tecnis ZMB00 (Abbott Medical Optics). The outcome of this study is presented in the current report.
Tecnis ZMB00: Combination of Presbyopia and Spherical Aberration Correction
The aspheric multifocal IOL Tecnis ZMB00 (Abbott Medical Optics) is a single-piece IOL with a 6.0-mm full-aperture diffractive optic and an overall length of 13.0 mm. It has an anterior aspheric surface designed according to the average cornea eye model to compensate for the spherical aberration of the cornea with −0.27 µm [9]. The IOL also incorporates a posterior diffractive multifocal optic pattern designed to provide both near and distance vision and thereby reduce spectacle dependency, with a near power representing a +4 D addition. The light distribution between the distance and near focus is approximately 50/50. The Tecnis ZMB00 IOL is available in powers ranging from +5.0 to +34.0 D in 0.5 D increments. The manufacturer's A-constant of this IOL is 118.8, and the surgeon factor 1.68. The optimized SRK/T constant is currently 119.5, the optimized surgeon factor is 2.15 (ULIB).
The Tecnis ZMB00 IOL is made of a soft foldable hydrophobic acrylic material, similar to the Sensar AR40 material (Abbott Medical Optics) with a covalently bound ultraviolet (UV) absorber. UV-blocking protection with full transmission of the entire visible light spectrum is achieved, which promotes a minimization of the contrast sensitivity loss. The haptics of this last-generation IOL have a modified C shape with TriFix design, which allows 3 points of capsular bag fixation to provide long-term stability and centration. It should be considered that minimal decentrations of the optic of a diffractive multifocal IOL can have a significant negative impact on the patients’ visual outcome [10]. The posterior edge of the optic has a 360°-squared design to provide uninterrupted contact at the haptic-optic junction and limit lens epithelial cell migration. Furthermore, a frosted design has been added to the edge of the optic to reduce potential edge glare effects.
Experimental Methodology of Our Research with the Tecnis ZMB00
We conducted a prospective consecutive study including a total of 31 eyes of 19 patients with ages ranging between 40 and 81 years, and undergoing phacoemulsification surgery with the implantation of the aspheric multifocal IOL Tecnis ZMB00. Patients 40 years or older with a visually significant cataract or presbyopia demanding surgical correction, corneal astigmatism of less than 1.50 D and without history of glaucoma or retinal detachment, corneal disease, irregular corneal astigmatism, abnormal iris, macular degeneration or retinopathy, neurophthalmic disease, or history of ocular inflammation were included.
During the preoperative consultation, all patients were asked about their professional and leisure activities. Patients were informed about potential side effects of multifocal lenses, such as reduced contrast vision, halos and glare disability. If patients expressed any doubts, they were not enrolled in the study.
Preoperatively, all patients had a complete ophthalmologic examination including the evaluation of the refractive status, far and near LogMAR uncorrected visual acuity (UCVA) and best-corrected VA (BCVA) testing, slit lamp examination, Goldmann applanation tonometry and funduscopy. Postoperatively, patients were evaluated during the follow-up at 1 day, and 1, 3 and 6 months after surgery. At 1 day after surgery, only far and near UCVA, IOP and the integrity of the anterior segment was evaluated. The postoperative examination protocol at 1, 3 and 6 months was identical to the preoperative protocol.
All surgeries were performed by the same experienced surgeon using a standard mini-incision sutureless microcoaxial phacoemulsification technique. In all cases, a corneal incision of 2.4 mm at 90° was planned. After standard capsulorhexis creation and phacoemulsification, the IOL was inserted successfully into the capsular bag using a Platinum injector (Abbott Medical Optics). All surgeries were uneventful, with no intraoperative adverse events or complications. Postoperatively, the same prophylactic treatment was administered to all patients consisting of corticosteroid-antibiotic combination eye drops.
Results and Discussion
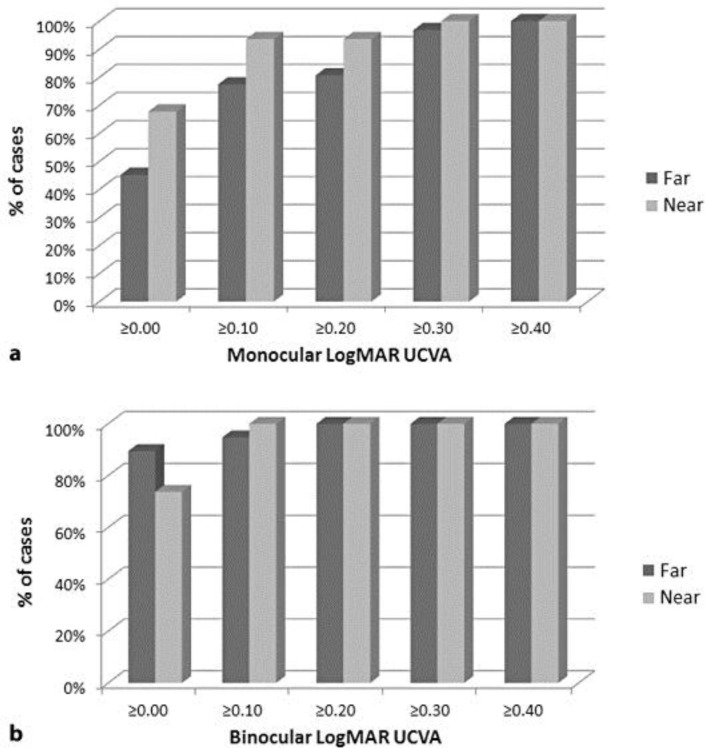
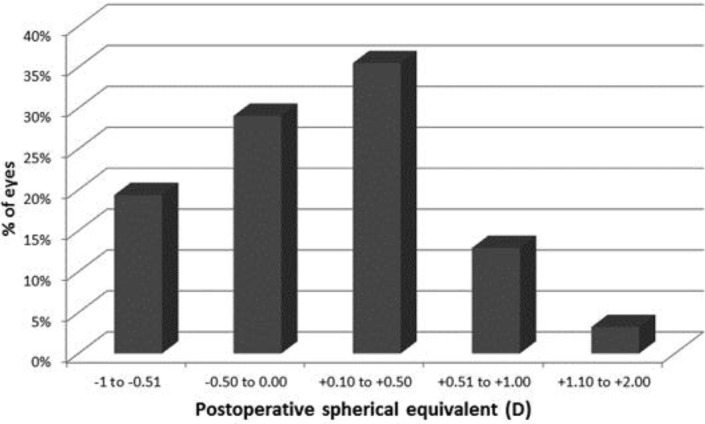
The mean age of patients was 65.0 ± 10.0 years in the analyzed sample, which included a total of 8 males (42.1%) and 11 females (57.9%). Mean IOL power implanted was 22.6 ± 3.6 D, ranging from 12 to 27 D. Table 1 summarizes the far and near visual and refractive outcomes. As shown, a statistically significant improvement was found in far BCVA (p < 0.01), with 96.8% (30 eyes) of eyes having a 6-month monocular postoperative far LogMAR BCVA of 0.1 or better. The replacement of the optically degraded crystalline lens with the optimized optics of the aspheric diffractive multifocal IOL evaluated played the main role in this finding. In addition, postoperative far LogMAR UCVA was 0.1 or better in a great percentage of cases monocularly (24 eyes, 77.4%) (fig. 1a) as well as binocularly (18 patients, 94.7%) (fig. 1b). This was in relation to an excellent predictability of the spherocylindrical correction, as shown in fig. 2. Indeed, almost all eyes (30 eyes, 96.8%) had a postoperative spherical equivalent within ±1.00 D. Similar visual and refractive results were obtained by Bautista et al. [11] using the same modality of diffractive IOL and by other authors [2, 3, 4] using other types of diffractive multifocal IOLs. Specifically, Bautista et al. [11] found in a sample of 70 eyes of 70 patients a mean far LogMAR UCVA of 0.194 ± 0.054, 0.119 ± 0.026, and 0.076 ± 0.014 at 15, 30, and 60 days after surgery, respectively. In addition, these authors found that 74.3% of eyes had a far UCVA of 0.1 LogMAR or better at 60 days after surgery [11]. Alió et al. [2] obtained in a sample of 40 eyes of 20 patients implanted with the aspheric diffractive IOL Acri.LISA 366D (Zeiss) similar distance visual outcomes compared to ours. However, these same authors reported a slightly poorer visual result with a diffractive apodized multifocal IOL, the AcrySof ReSTOR SN6AD3 (Alcon), in an additional sample of 40 eyes of 20 patients [2]. It should be considered that these 2 IOLs, the Acri.LISA 366D and AcrySof ReSTOR SN6AD3, are not designed to compensate for the average corneal spherical aberration. All this previous scientific evidence on the visual and in vivo intraocular optical performance with different multifocal IOL designs and the Tecnis platform is consistent and further supported by the outcomes of objective optical-bench experiences, which has been very useful for checking the real working principle of the currently available multifocal IOLs [12].
Table 1.
Summary of the far and near visual and refractive outcomes in our study with the Tecnis ZMB00
| Before surgery | –6 Months after surgery | p value | |
|---|---|---|---|
| Monocular far LogMAR UCVA | – | 0.08±0.11 (0.00 to 0.40) | – |
| Binocular far LogMAR UCVA | – | 0.01±0.08 (−0.08 to 0.22) | – |
| Manifest sphere, D | +0.27±2.88 (–7.00 to +4.50) | +0.34±0.64 (−0.75 to +2.25) | 0.91 |
| Manifest cylinder, D | −0.60±0.71 (–3.50 to 0.00) | −0.57±0.38 (–1.50 to 0.00) | 0.82 |
| Spherical equivalent, D | −0.03±2.84 (–7.13 to +4.38) | +0.05±0.55 (–1.00 to +1.63) | 0.88 |
| Far LogMAR BCVA | −0.41±0.32 (0.05 to 1.52) | 0.03±0.05 (0.00 to 0.15) | <0.01 |
| Monocular near LogMAR UCVA | – | 0.03±0.09 (−0.10 to 0.30) | – |
| Binocular near LogMAR UCVA | – | 0.00±0.08 (−0.10 to 0.10) | – |
Data are mean ± SD (range).
Fig. 1.
Distribution of far and near UCVA. a Monocular. b Binocular.
Fig. 2.
Distribution of the postoperative spherical equivalent in the sample of eyes evaluated in the current study.
Regarding the near visual outcome obtained in our sample, 67.7% of eyes (21 eyes) and 93.55% of eyes (29 eyes) achieved a postoperative near LogMAR UCVA of 0.00 (equivalent to J1+ in Jaeger notation) and 0.10 (equivalent to J1) or better, respectively. This was comparable to the levels of near VA provided by other aspheric diffractive IOLs [2] and better than those provided by refractive multifocal IOLs [4, 13]. As in the Bautista et al. series [11], most eyes (78.57%) could read Jaeger J1 (0.1 LogMAR) or smaller letters without correction at 6 months postoperatively and none of the eyes presented a near UCVA of J4 (0.4 LogMAR) or worse. This confirms the excellent ability of the Tecnis ZMB00 IOL to provide a near functional vision, and therefore its excellent performance as a presbyopia-correcting IOL.
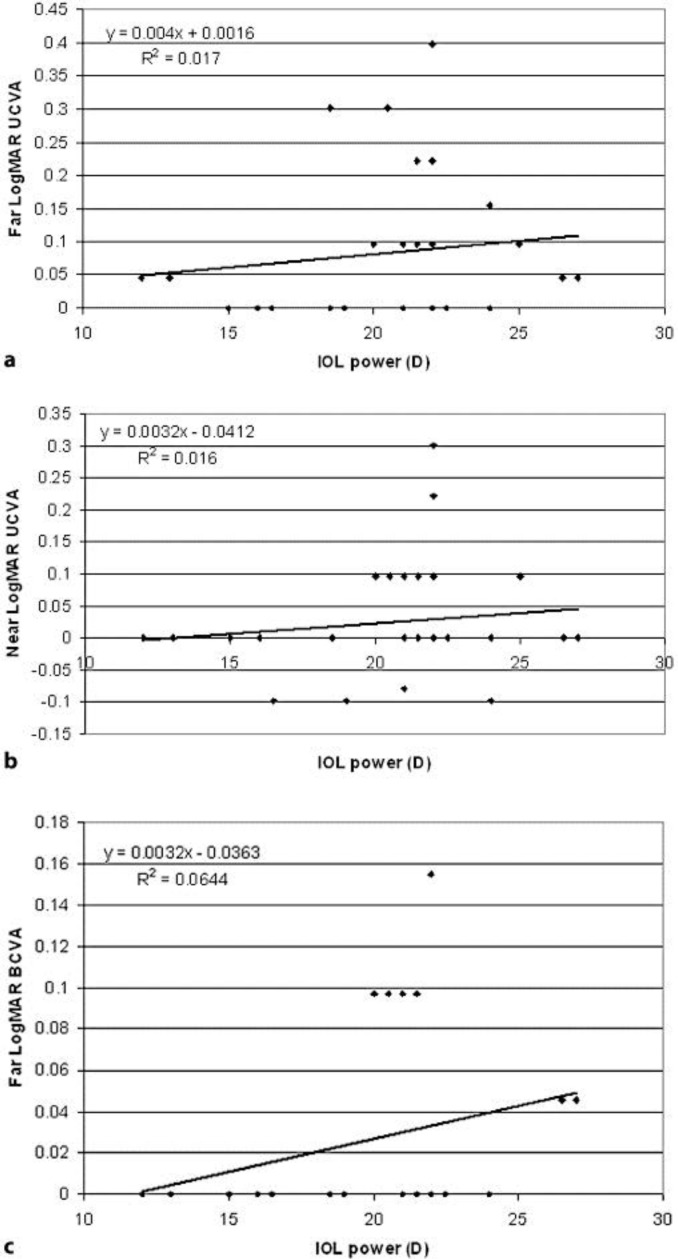
Finally, we evaluated the level of correlation between the IOL power implanted and the postoperative far and near VA. Specifically, the IOL power was found to be very poorly correlated with the postoperative far LogMAR (r = 0.13, fig. 3a) and near UCVA (r = 0.13, fig. 3b). This confirms that the predictability of the refractive correction achieved with the implant was not limited by its optical power. Furthermore, a poor correlation was found between IOL power and far LogMAR BCVA (r = 0.25, fig. 3c), which shows the minimal impact of higher order aberrations on VA in those eyes implanted with the Tecnis ZMB00 IOL. This is in agreement with the excellent contrast sensitivity outcomes obtained by Bautista et al. [11] for this same IOL. It should be remembered that the Tecnis ZMB00 IOL provides compensation for the corneal spherical aberration with −0.27 µm, potentially minimizing the global ocular magnitude of this high-order aberration. This result contrasts with the limitation imposed on the final visual outcome and optical quality by the IOL power of apodized diffractive multifocal IOLs [14], potentially attributable to the aberrometric properties of the IOL as well as to the possibility of foci overlapping [14].
Fig. 3.
Scattergram showing the relationship between the optical power of the IOL implanted and different visual variables. a Postoperative far LogMAR UCVA. b Postoperative near LogMAR UCVA. c Postoperative far LogMAR BCVA.
Conclusions
In conclusion, the aspheric diffractive multifocal IOL Tecnis ZMB00 provides a restoration of the far and near visual function after phacoemulsification surgery for cataract removal or presbyopia correction. The correction provided by the IOL is predictable and independent from the optical power of the IOL implanted. Studies currently in progress are confirming the agreement between this level of visual restoration with patient satisfaction, a minimal perception of photic phenomena, the presence of a postoperative optimized intraocular optics, and an excellent contrast sensitivity outcome, as reported preliminarily by Bautista et al. [11], and Sood and Woodward [15]. The combination of diffractive multifocality and compensation for the corneal spherical aberration is an effective option for cataract surgery and presbyopia correction, allowing an optimized distance and near visual function.
Disclosure Statement
The authors have no proprietary or commercial interest in the medical devices that are involved in this work. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
References
- 1.Auffarth GU, Rabsilber TM, Kohnen T, et al. Design und optische Prinzipien von Multifokallinsen. Ophthalmologe. 2008;105:522–526. doi: 10.1007/s00347-008-1744-9. [DOI] [PubMed] [Google Scholar]
- 2.Alió JL, Piñero DP, Plaza-Puche AB, Amparo F, Jiménez R, Rodríguez-Prats JL, Javaloy J. Visual and optical performance with two different diffractive multifocal intraocular lenses compared to a monofocal lens. J Refract Surg. 2011;27:570–581. doi: 10.3928/1081597X-20101223-01. [DOI] [PubMed] [Google Scholar]
- 3.Kohnen T, Kook D, Auffarth GU, et al. Einsatzmöglichkeiten intraokularer Multifokallinsen und Kriterien der Patientenselektion. Ophthalmologe. 2008;105:527–532. doi: 10.1007/s00347-008-1745-8. [DOI] [PubMed] [Google Scholar]
- 4.Ehmer A, Rabsilber TM, Mannsfeld A, et al. Einfluss verschiedener multifokaler Intraokularlinsenkonzepte auf den Streulichtparameter. Ophthalmologe. 2011;108:952–956. doi: 10.1007/s00347-011-2411-0. [DOI] [PubMed] [Google Scholar]
- 5.Hofman T, Zuberbuhler B, Cervino A, Montés-Micó R, Haefliger E. Retinal straylight and complaint scores 18 months after implantation of the AcrySof monofocal and ReSTOR diffractive intraocular lenses. J Refract Surg. 2009;25:485–492. doi: 10.3928/1081597X-20090512-02. [DOI] [PubMed] [Google Scholar]
- 6.Davison JA, Simpson MJ. History and development of the apodized diffractive intraocular lens. J Cataract Refract Surg. 2006;32:849–858. doi: 10.1016/j.jcrs.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 7.Weeber HA, Piers PA. Theoretical performance of intraocular lenses correcting both spherical and chromatic aberration. J Refract Surg. 2012;28:48–52. doi: 10.3928/1081597X-20111103-01. [DOI] [PubMed] [Google Scholar]
- 8.Packer M, Chu YR, Waltz KL, Donnenfeld ED, Wallace RB, 3rd, Featherstone K, Smith P, Bentow SS, Tarantino N. Evaluation of the aspheric tecnis multifocal intraocular lens: one-year results from the first cohort of the food and drug administration clinical trial. Am J Ophthalmol. 2010;149:577–584. doi: 10.1016/j.ajo.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 9.Terwee T, Weeber H, van der Mooren M, Piers P. Visualization of the retinal image in an eye model with spherical and aspheric, diffractive, and refractive multifocal intraocular lenses. J Refract Surg. 2008;24:223–232. doi: 10.3928/1081597X-20080301-03. [DOI] [PubMed] [Google Scholar]
- 10.Soda M, Yaguchi S. Effect of decentration on the optical performance in multifocal intraocular lenses. Ophthalmologica. 2012;227:197–204. doi: 10.1159/000333820. [DOI] [PubMed] [Google Scholar]
- 11.Bautista CP, González DC, Gómez AC. Evolution of visual performance in 70 eyes implanted with the Tecnis((r)) ZMB00 multifocal intraocular lens. Clin Ophthalmol. 2012;6:403–407. doi: 10.2147/OPTH.S24425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pepose JS, Wang D, Altmann GE. Comparison of through-focus image sharpness across five presbyopia-correcting intraocular lenses. Am J Ophthalmol. 2012;154:20–28. doi: 10.1016/j.ajo.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 13.Pepose JS, Qazi MA, Davies J, Doane JF, Loden JC, Sivalingham V, Mahmoud AM. Visual performance of patients with bilateral vs. combination Crystalens, ReZoom, and ReSTOR intraocular lens implants. Am J Ophthalmol. 2007;144:347–357. doi: 10.1016/j.ajo.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 14.Moreno LJ, Piñero DP, Alió JL, Fimia A, Plaza AB. Double-pass system analysis of the visual outcomes and optical performance of an apodized diffractive multifocal intraocular lens. J Cataract Refract Surg. 2010;36:2048–2055. doi: 10.1016/j.jcrs.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 15.Sood P, Woodward MA. Patient acceptability of the Tecnis multifocal intraocular lens. Clin Ophthalmol. 2011;5:403–410. doi: 10.2147/OPTH.S11126. [DOI] [PMC free article] [PubMed] [Google Scholar]