Abstract
Background
Vancomycin-resistant Enterococcus (VRE) endophthalmitis after penetrating keratoplasty (PKP) is very rare, the management is a challenge due to both the pattern of antibiotic resistance and the aggressive nature of the infectious process. We report the first delayed-onset case of VRE endophthalmitis after PKP.
Materials and Methods
Case report of a 51-year-old female with a 7-week history of PKP who arrived at the emergency room with signs and symptoms of endophthalmitis. Initial visual acuity was light perception, and a posterior pole exam was not possible due to the intense vitreous reaction. Mode B ultrasound was used to assess the posterior pole. The patient underwent pars plana vitrectomy and received intravitreous antibiotics.
Results
Vitreous stains and cultures were positive for Enterococcus faecium resistant to vancomycin. Donor rim cultures and viral PCR were negative. Treatment was carried out by repeated intravitreal antibiotics and systemic linezolid. Clinical improvement was seen after the second dose of intravitreous antibiotics and systemic linezolid, but visual acuity remained at light perception consistent with the ischemic changes observed in the posterior pole.
Conclusion
VRE endophthalmitis might be associated with positive donor rim cultures. Prompt use of systemic linezolid in addition to intravitreous antibiotics is recommendable, but even with prompt treatment, visual prognosis is guarded.
Key words: Delayed-onset endophthalmitis, Penetrating keratoplasty, Vancomycin-resistant Enterococcus, Intravitreal antibiotics, Systemic linezolid
Introduction
Enterococcus is known to be a relatively uncommon cause of endophthalmitis. According to the Endophthalmitis Vitrectomy Study [1], it constitutes only 1.2% of the reported endophthalmitis cases. This Gram-positive bacterium is part of the biota of the gastrointestinal tract [2] and is recognized for its resistance to cephalosporins, penicillinase-resistant penicillins and monobactams [3]. Postoperative vancomycin-sensitive Enterococcus endophthalmitis has been reported after cataract surgery, penetrating keratoplasty (PKP), trabeculectomy and pupilloplasty [4, 5]. However, only 1 case of acute endophthalmitis after PKP caused by vancomycin-resistant Enterococcus (VRE) has been described to date [6]. We report the first case of delayed-onset VRE endophthalmitis after PKP.
Case Report
We report on a 51-year-old female with a 7-week history of PKP in her left eye after treatment of keratoconus. She presented at the emergency room with severe pain, decreased vision and eyelid edema that started 8 h prior to admission. On clinical examination, she had visual acuity of light perception, severe conjuctival chemosis, ciliary injection, marked corneal stromal edema, anterior chamber reaction and hypopyon (fig. 1). Fundus exam was not possible. Mode B ultrasound demonstrated severe dense vitreous opacities and a choroidal thickness of 1.5 mm. A pars plana vitrectomy was performed 24 h after her admittance, and intravitreal ceftazidime (2.25 mg/0.1 ml), vancomycin (1.0 mg/0.1 ml) and dexamethasone (400 µg/0.1 ml) were injected at the end of the procedure. She was treated with topical moxifloxacin 1% and ceftriaxone (50 mg/ml) every hour, oral ciprofloxacin 750 mg twice daily and topical 1% prednisolone acetate every 6 h. Informed consent was obtained from the patient prior the elaboration of this case report.
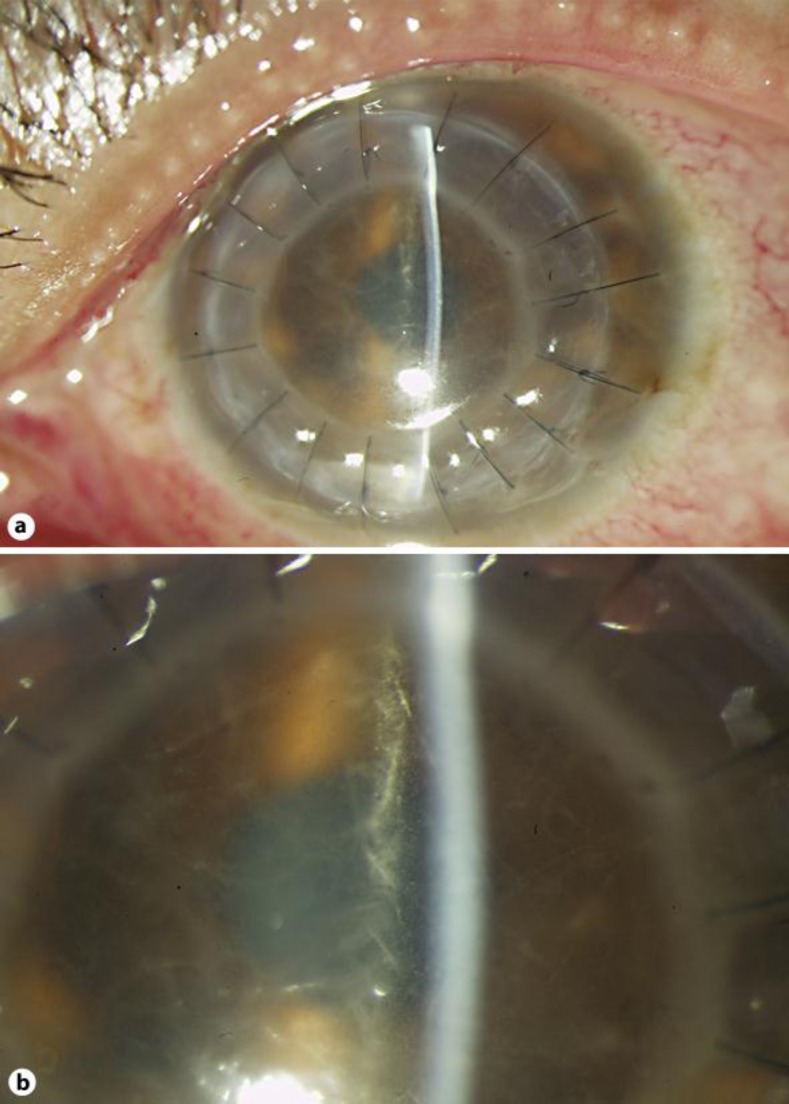
Fig. 1.
a Severe conjuctival chemosis and ciliary injection, marked corneal graft edema, anterior chamber reaction with 3+ cells and hypopyon. b Magnification of the severe anterior chamber reaction and corneal graft edema.
Results
Both Gram stain and the aqueous sample PCR confirmed the presence of Gram-positive bacteria. Cultures and viral PCR from the donor rim were negative. Vitreous culture showed VRE [minimum inhibitory concentration (MIC) >32 µg/dl]. The organism was susceptible to linezolid (MIC 2 µg/dl) and tetracycline (MIC ≤1 µg/dl). Intravitreal antibiotics and dexamethasone were repeated 72 h after her admission. Intravenous linezolid 600 mg twice daily for 1 week was initiated at the same time.
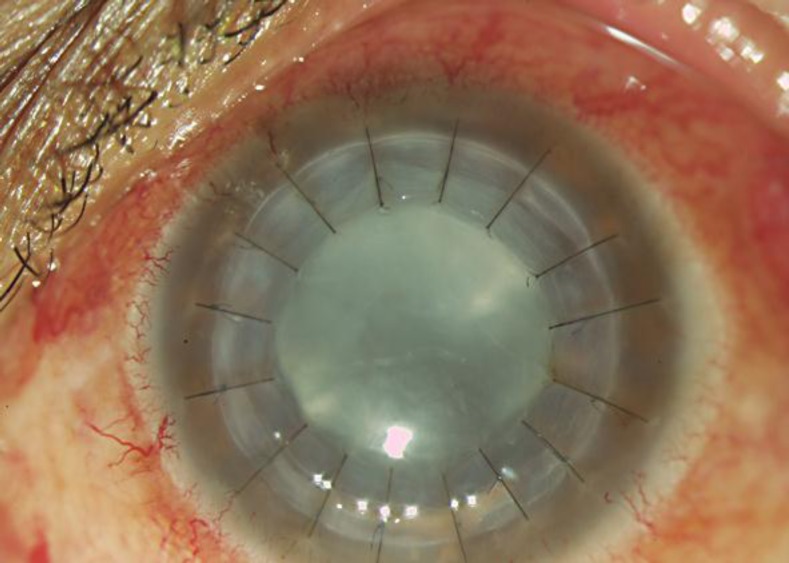
During the next 2 weeks, the pain, chemosis, eyelid and corneal edema improved (fig. 2). However, her visual acuity remained at light perception. The fundus exam revealed ischemic retina, a pale optic nerve with some remaining vitreous opacities and pseudomembranes. Anti-inflammatory topical treatment with prednisolone acetate 1% four times daily was continued.
Fig. 2.
Mild corneal graft edema, no anterior chamber reaction and lens opacity.
Discussion
Enterococcus endophthalmitis after PKP is very rare. In a series of 29 patients with endophthalmitis caused by Enterococcus faecalis, Scott et al. [6] reported only 4 cases of endophthalmitis associated with PKP. They described susceptibility to vancomycin and linezolid in all their patients, but even with a prompt management 48.3% of the 29 cases ended up with a visual acuity of light perception or worse. Cameron et al. [7] described 1 case of Enterococcus endophthalmitis after a revision of 3,000 consecutive PKPs. Later, the same author reported 3 cases of E. faecalis endophthalmitis following PKP; all of them had positive cultures from donor rims for the same microorganism, and antibiogram profiles showed sensitivity to minocycline, bacitracin and gentamicin, and moderate sensitivity to vancomycin [8]. In 2007, Bains et al. [9] reported the first known case of vancomycin-resistant Enterococcus faecium acute endophthalmitis after PKP with positive cultures of the donor rim. To our knowledge, this is the first reported case of a delayed-onset VRE endophthalmitis after PKP; hence the second reported case of VRE endophthalmitis after PKP.
VRE has come to light as a serious health threat, accounting for 28% of the enterococcal infections in intensive care units in the US [9]. Regardless of the increasing incidence of colonization and infection of patients with this microorganism, ophthalmologic infections caused by VRE are still rare. We have to emphasize that in both cases, VRE was resistant not only to vancomycin but to all the routine antibiotics tested in standard in vitro susceptibility tests. The emergence of multi-resistant pathogens suggests the need for new trends in laboratory microbiological research and antibiotic sensitivities.
The clinical response of our case using repeated intravitreal ceftazidime and vancomycin supports the principle that repeated intravitreal antibiotic injection might as well achieve higher than the MICs, therefore reaching a therapeutic response despite of the antibiotic resistance showed in vitro [10, 11]. However, in cases of VRE endophthalmitis the prompt use of systemic linezolid (oral or intravenous) in addition to intravitreal antibiotics is recommendable, since it has shown to achieve aqueous humor and intravitreal concentrations higher than the MIC for 90% of isolates for all Gram-positive bacteria including VRE [12, 13].
Recommendations on the mandatory culture of the sclerocorneal rim after suspected or diagnosed VRE endophthalmitis should be considered, since colonized donor corneal tissue is a potential source of infection, and not every center in developing countries performs it as a routine. Enterococcal endophthalmitis of any type is quite rare, and it is associated with a poor visual prognosis.
Disclosure Statement
The authors have no financial interest relevant to the materials presented in this case report.
References
- 1.Chen KJ, Lai CC, Sun MH, et al. Postcataract endophthalmitis caused by Enterococcus faecalis. Ocul Immunol Inflamm. 2009;17:364–369. doi: 10.3109/09273940903105110. [DOI] [PubMed] [Google Scholar]
- 2.Han DP, Wisniewski SR, Wilson LA, et al. Spectrum and susceptibilities of microbiologic isolates in the Endophthalmitis Vitrectomy Study. Am J Ophthalmol. 1996;122:1–17. doi: 10.1016/s0002-9394(14)71959-2. [DOI] [PubMed] [Google Scholar]
- 3.Jones RN. Enterococcus. [book auth.]; in Schlossberg D: Current Therapy of Infectious Disease. 2nd. St. Louis: Mosby; 2001. pp. 496–499. [Google Scholar]
- 4.Bisno AL. Classification of streptococci. [book auth.] In: Douglas RG Jr, Bennett JE, Mandell GL, editors. Principles and Practice of Infectious Diseases. 3rd ed. New York: Churchill Livingstone; 1990. pp. 1518–1519. [Google Scholar]
- 5.Choi S, Hahn TW, Osterhout G, O'Brien TP. Comparative intravitreal antibiotic therapy for experimental Enterococcus faecalis endophthalmitis. Arch Ophthalmol. 1996;114:61–65. doi: 10.1001/archopht.1996.01100130057009. [DOI] [PubMed] [Google Scholar]
- 6.Scott IU, Loo RH, Flynn HW, et al. Endophthalmitis caused by Enterococcus faecalis: antibiotic selection and treatment outcomes. Ophthalmology. 2003;110:1573–1577. doi: 10.1016/S0161-6420(03)00502-5. [DOI] [PubMed] [Google Scholar]
- 7.Cameron JA, Antonios SR, et al. Endophthalmitis from contaminated donor corneas following penetrating keratoplasty. Arch Ophthalmol. 1991;109:54–59. doi: 10.1001/archopht.1991.01080010056032. [DOI] [PubMed] [Google Scholar]
- 8.Cameron JA, Badr IA, et al. Endophthalmitis cluster form contaminated donor corneas following penetrating keratoplasty. Can J Ophthalmol. 1998;33:8–13. [PubMed] [Google Scholar]
- 9.Bains HS, Weinberg DV, Feder RS, et al. Postoperative vancomycin-resistant Enterococcus faecium endophthalmitis. Arch Ophthalmol. 2007;125:1292–1293. doi: 10.1001/archopht.125.9.1292. [DOI] [PubMed] [Google Scholar]
- 10.Tenover FC, McDonald LC. Vancomycin-resistant staphylococci: epidemiology and control. Curr Opin Infect Dis. 2005;18:300–305. doi: 10.1097/01.qco.0000171923.62699.0c. [DOI] [PubMed] [Google Scholar]
- 11.Fiscella RG, Lai WW, Buerk B, et al. Aqueous and vitreous penetration of linezolid (Zyvox) after oral administration. Ophthalmology. 2004;111:1191–1195. doi: 10.1016/j.ophtha.2003.09.042. [DOI] [PubMed] [Google Scholar]
- 12.Greenwood D. In vitro veritas? Antimicrobial susceptibility tests and their clinical relevance. J Infect Dis. 1981;144:380–385. doi: 10.1093/infdis/144.4.380. [DOI] [PubMed] [Google Scholar]
- 13.Kaye SB, Neal T, Nicholson S, et al. Concentration and bioavailability of ciprofloxacin and teicoplanin in the cornea. Invest Ophthalmol Vis Sci. 2009;50:3176–3184. doi: 10.1167/iovs.08-3201. [DOI] [PubMed] [Google Scholar]