Abstract
Background:
Poisoning and drug overdose (DO) are important health problems in developing countries. These emergencies are associated with high mortality and morbidity. Different factors affect the final outcome of patients. This study aims to review the pattern of poisoning and DO in an urban tertiary care hospital and also the determinants and final outcome of patients with poisoning and DO.
Materials and Methods:
Observational, retrospective hospital records-based study at a tertiary care hospital (15 months). Data on demography, hospitalization, complications, type of poison/drug and outcome of patients with poisoning and DO were collected. Data were analyzed using descriptive statistics, Chi square test and ANOVA. P < 0.05 was considered significant.
Results:
Of the total of 296 records, 213 were included (122 poisoning, 91 DO). Organophosphates (OP) (32.5%), pyrethroids (17.2%) and organocarbamates (12.2%) were the commonly used poisons. Sedatives and antiepileptics (21% each) were the common DOs. Poisoning among men was greater than that among women (P < 0.001). Outcome parameters of hospital stay and ventilator requirement were significant (P < 0.001). The overall case fatality rate was 2.4%.
Conclusions:
OP compounds were the most common among poisons, while sedatives were frequently consumed drugs. Young adults from urban areas were the common victims with suicidal intention. Regulations, educational awareness and poison information centers will help to reduce the growth of this public health problem.
Keywords: Drug overdose, outcomes, poisoning, tertiary care center
Introduction
Deliberate self-harm is a major public health problem in many developing countries including India.[1] Each year, 500,000 deaths occur in rural Asia due to suicide, and 200,000 of these deaths are due to self-organophosphates (OP) poisoning. The medical management of poisoning emergencies is difficult and, till date, there are no clear-cut evidence-based guidelines for the best management of OP poisoning.[2] Drug overdose (DO) is the second most common mode of deliberate self-harm after poisoning with pesticides. Both are associated with a high case fatality rate (CFR). In developing countries, the fatality rate is 15-times higher than in industrialized countries.[3]
This study aims to review the incidence of poisoning and DO in an urban tertiary care hospital and also the determinants and final outcome of patients with poisoning and DO.
Materials and Methods
The study was an observational, retrospective study conducted for a duration of 15 months carried out at a tertiary care center with superspeciality services and bed strength of 1200 well equipped with modern diagnostic and treatment facilities. Data were collected from medical records of all adult patients admitted to the Emergency Medicine Department with a primary diagnosis of poisoning and DO after approval from hospital authorities. Records of patients who got discharged against medical advice were excluded.
Data regarding demographic profile, residence, disease data, clinical assessment, treatment data, comorbid conditions, investigational details, adverse drug reactions and treatment outcome data were collected.
Statistical analysis
Both descriptive and inferential statistics were used to analyze the data. Categorical data of the determinants of treatment and outcome measures were analyzed using the X2 test. Analysis of variance (ANOVA) was used to compare between the drug overdose and the poisoning groups. P <0.05 was considered significant. The Kruskal Wallis test was used to compare the determinants of treatment between the different types of poisoning.
Results
The study profile is shown in Figure 1. A total of 296 records were screened, and 213 were included based on study criteria. There were 122 cases of poisoning and 91 cases of DO.
Figure 1.
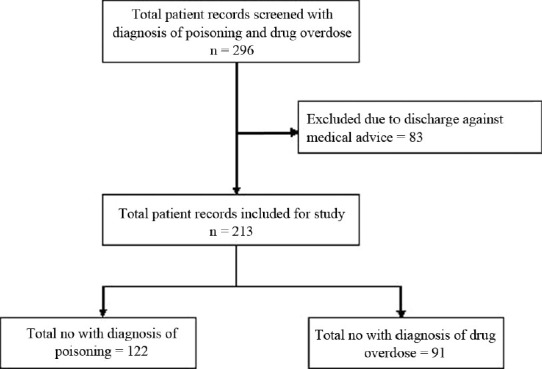
The number of patient records screened and included in the study
Table 1 shows the patient characteristics of both poisoning and DO. The numbers of male patients with poisoning were significantly greater than the number of women with poisoning (χ2 17.3, df = 1, P = 0.0001). Women significantly outnumbered men in the diagnosis of DO. Poisoning (122 cases) was common in the younger age groups between 21 and 30 years (54.9%). The people from the urban areas were significantly higher compared with the rural areas. (χ2 6.45, df = 1, P = 0.009).
Table 1.
Patient characteristics in the study
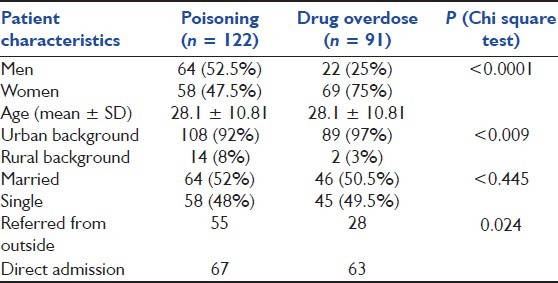
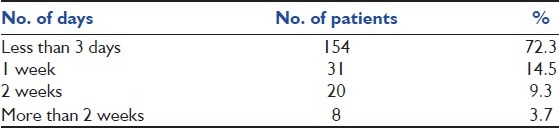
Figure 2 shows the pattern of poisoning in this study, the most common being OP (32.5%), pyrethroids (17.2%), organocarbamates (OC) (12.2%) and corrosives (7.3%). A total of 38.9% of the patients were referred from primary and secondary hospitals. Among them, a significant number were poisoning cases (χ2 4.4, df = 1, P = 0.024). Table 2 shows duration of hospital stay in both poisoning and DO patients. Majority of patients in the study had a shorter stay in the hospital. We found that 66% of patients with poisoning had a shorter stay of less than or equal to 3 days in the hospital, and the median, interquartile range values for duration of stay was 2 (1–4) days.
Figure 2.
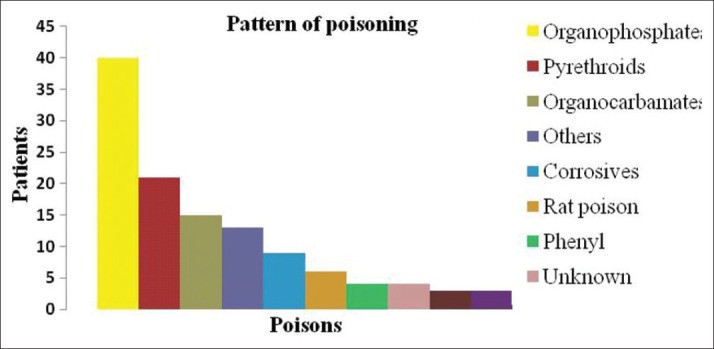
The pattern of poisoning in the study
Table 2.
Duration of hospital stay in patients with poisoning and drug overdose (n = 213)
Among patients with poisoning, 67% required intensive care, and the duration of stay in the Intensive Care Unit (ICU) was 4.43 ± 2.80 days. Of those patients in the ICU, 21.9% needed assisted ventilation for a period of 6.05 ± 3.42 days. The need for ventilation was significantly higher in patients with OP poisoning than in those with the other types of poisoning. (χ2 15.80, df = 3, P = 0.001).
24.5% of the patients had consumed the poison during the late evening hours (6 pm to 12 midnight) We also found that 69.6% of the patients presented to hospital within 12 h of the event, while 23.7% presented within 3 h of the event. It was found that 90.9% of the patients had intentionally used the poisons to induce self-harm. The common route of consumption of poison was oral (97.5%), followed by accidental inhalation.
OP and OC received both specific as well as supportive therapy, and the remaining poisons were managed symptomatically with supportive therapy. Pralidoxime, glycopyrrolate and atropine were the antidotes used. In 62.5% of the OP poisoning patients, the combination of pralidoxime with glycopyrrolate was the commonly used antidote. There was no significant difference between the need of ventilation and the different antidotes used in the treatment of OP poisoning. (χ2 3.18, df = 2, P = 0.20). In 53.3% of the patients, no specific antidote was used.
12.2% of the patients with poisoning developed complications during the stay in hospital. Ventilator-associated pneumonia was the most common complication noted (33.3%), while multiorgan dysfunction syndrome stood as the second most common complication (13.3%). Poisoning due to OP compounds lead to a higher number of complications (53.3%), especially ventilator-associated pneumonia.
Figure 3 shows the pattern of DO. Sedatives and antiepileptic drugs were the most common, with 21% each, followed by antidepressants and paracetamol. The present study showed DO to be 42.7% (91/213) of the study population, of which female patients accounted for 75% of the cases. Young women in the age group of 21–30 years accounted for 39.5% of the DO cases, with nearly 50% being married, and were from an urban background.
Figure 3.
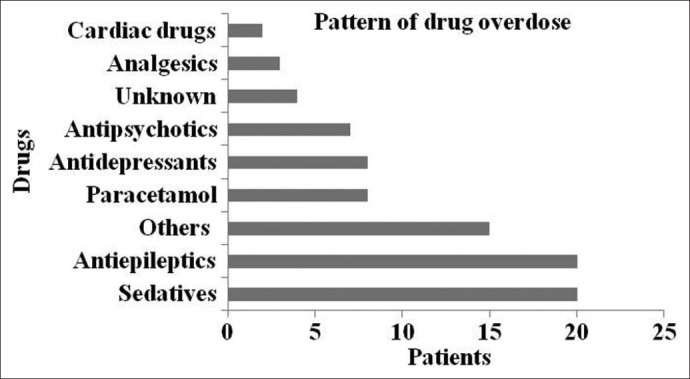
The pattern of drug overdose in the study
Of the total DO cases, 30% were referred from other hospitals. About 43.9% were treated in the ICU for a duration of 3.94 ± 2.36, while only 7% of them received assisted ventilation for 6.53 ± 3.55. We found that nearly 43% of the events occurred between 6 am and 6 pm. Thirty-four percent of the patients presented to the hospital within 6 h of event. In 79% of the patients, there were intentions of self harm; the remaining were accidental.
DOs were managed most often in the general wards symptomatically. A total of 37.5% received ICU care for a duration of 3.25 ± 0.71 days, and none of the patients needed assisted ventilation. Paracetamol was the most common drug with specific antidote used in cases of overdose. N acetyl cysteine (NAC) was the antidote used. Most cases of barbiturate overdose were managed symptomatically. In 17.5% of the patients, the drug levels were elevated, and, in them, forced alkaline diuresis (FAD) as infusion was used effectively for a duration (days) of 2.60 ± 1.51. DO patients (85%) were treated symptomatically, and only one of the patients required use of inotropes.
The important factors influencing outcome in patients with poisoning are severity of poisoning, type of poison, quantity consumed, time of event, time to present at hospital, duration of stay at hospital, stay in ICU, need for ventilation and complications during the stay at hospital. There was a significantly greater need for assisted ventilation in patients with poisoning as compared with DO (χ2 6.03, df = 1, P = 0.014).
A significantly longer stay was found in patients with OP poisoning when analyzed using the Kruskal Walis test (P = 0.0001); however, the duration of stay did not correlate with the mortality.
The overall CFR in our study was 2.4%. There were three mortalities among patients with poisoning. The poisons used were aluminum phosphide (2) and a corrosive. There was no significant difference in the outcomes between men and women (χ2 0.874, df = 1, P = 0.35). All patients with DO improved and no mortality was reported.
Discussion
Of the 500,000 deaths occuring every year, nearly 200,000 deaths are due to self-poisoning with OP compounds in South East Asia.[2] Data from the western part of the globe shows that DO is a common mode of deliberate self-harm. The results of the present study show that poisoning and DO persist to remain a major public health problem.
OP compounds (32.5%) were the most commonly consumed poisons, and their treatment included oximes and glycopyrrolate. Men outnumbered women by 4.6%, and 54.9% of them were in the age group of 21–30 years. These findings correlate with studies conducted in Iran and also other studies performed across our countries, and may be attributed to the fact that pesticides are more accessible to men, as is found in the literature.[1,4–9]
The domicile distribution of patients in our study showed 92% from urban areas comparable to other studies, which have shown predominance of poisoning in rural areas.[10]
Twenty-five percent of the patients had consumed the poison in the evening hours. This pattern of consumption has been shown in other studies, and it has been postulated that people who definitely want to die chose a poisonous compound and most often took it in the evening hours when the rest of the family was less alert.[11]
Only 19% of the patients presented to the hospital within 3 h of poisoning as compared with 57.4% in the literature.[12] This could probably be attributed to the fact that 66% of the poisoning cases were referrals and hence a lot of time could have lapsed during the transport. This again highlights that the outcome in these patients depends on multiple factors.
Of the other poisons in our study, the incidence of Aluminium Phosphide was 3.2%, and this is significantly lower compared with studies in North India.[13–15] Also across Asia, AIP poisoning is very common, with mortality as high as 31% in Iran.[16]
In the present study, deaths were due to aluminum phosphide and corrosive poisoning, and the overall CFR due to self-poisoning was 2.4%. The literature shows that in UK, the self-poisoning CFR is less than 0.5%, in Sri Lanka it is 7% and in India it is 30%. The low mortality in our study could be attributed to the infrastructure and treatment facility available at a tertiary care center.
Duration of hospital stay, ventilator requirement and duration, type of poison and the quantity, comorbid conditions, clinical complications are some of the major determinants of outcomes in patients with poisoning. From our experience, we found that majority of the critically ill patients and poor patients got discharged against medical advice owing to financial reasons. There is thus a dearth of data on the final outcome of patients with poisoning.
As the overall mortality was low (3), the determinants of the outcome using multiple logistic regression test was not feasible in the present study. However, comparing the above-mentioned parameters of patients in our study, those with poisoning definitely were at an increased risk of mortality.
Some of the strategies to reduce the use and availability of pesticides used in poisoning are: voluntary guidelines, safe use initiatives and international policy instruments, changes in farming practice such as integrated pest management (IPM) and direct restrictions of pesticide use.[17]
Among the salient features of these strategies is the International Code of Conduct on the Distribution and Use of Pesticides.[18] This necessitates government authorities of countries to establish regulations and voluntary standards of conduct on the safe distribution, handling and availability of pesticides. It requires that highly toxic pesticides be prohibited for importation, sale and purchase if Good manufacturing practice is insufficient. However, implementation of the Code needs good infrastructure and resources, backed by a strong political will to prevent hazards due to the pesticides.
Industry initiatives in reducing the pesticides hazards will contribute greatly in preventing the poisoning emergencies. The literature shows that initiatives such as the Global Crop Protection Federation (GCPF) pilot projects in Guatemala did help in reducing the number of poison-related deaths.[19]
The IPM approach enables farmers to reduce the use of pesticides and has been found to be highly economical as investment on pesticides is less, safe as exposure to these chemicals is reduced and in addition profitable due to the high returns of produce.[20]
Studies from round the world have shown that restricting the availability of pesticides by banning potentially toxic poisons goes a long way in reducing the deaths due to poisoning.[17,21,22] Establishment of a minimum pesticide list on similar lines as the essential drug list will further help in curbing the poisoning-related events.[23]
Studies from across India have also shown DO to be one of the causes of suicidal deaths.[24–26] In our study, DO was significantly higher in women as compared with men. From the literature, we found that women tend to consume drugs frequently as compared with other poisonous compounds.[27] However, the western data show that DO is common in men.[28]
Barbiturates and benzodiazepines that constitute the majority of sedative drugs and antiepileptics were the most common among DO cases in our study(21%). This pattern is similar to other studies across India.[24,25,29] The probable reason could be that these drugs are easily available as over-the-counter medications in India.
Most of the DOs were managed symptomatically with supportive therapy. Phenobarbitone overdose was treated in our hospital with FAD.
Paracetamol was another drug found to be involved in overdose in our study. It has been reported to be a common cause of death due to DO in the UK and is treated with NAC, a specific antidote. Various measures have been undertaken in the west to reduce the incidence of DO, such as reducing the number of tablets available in the blister packs to 32 in government pharmacies and 16 in nongovernment pharmacies. This legislation introduced in 1998 is reported to reduce the estimated quantity of paracetamol ingestion but not the incidence.[30] The average number of tablets taken in paracetamol overdoses decreased by 7% (0–12%) and the proportion involving >32 tablets decreased by 17%.
Recently, in June 2009, the US Food and Drug Administration (FDA) has announced requirements to provide new information regarding acetaminophen-induced hepatotoxicity.[31] Apart from examining the possibility of removal of acetaminophen from popular analgesic combination products, the FDA is also currently evaluating whether changes need to be made for acetaminophen regarding the following: safe daily dose for healthy individuals, safe daily dose in chronic liver disease, safe daily dose when used with alcohol, appropriate dose for efficacy, package size restrictions.
Conclusion
OP compounds followed by pyrethroids and OC were the most common poisons, while sedatives, antiepileptics followed by antidepressants and paracetamol were the common drugs encountered in DO. Deliberate self-harm was the most common motive behind the cases. The CFR in our study was 2.4%
The mortality rate is low, which reflects on good management of these emergencies at a tertiary care set-up. However, the data on outcome of patients discharged against advice is largely unknown. The study thus indicates that poisoning and DO are still common public health problems. Educational and awareness programs, establishment of poison information and surveillance centers and regulations on pesticides/drug availability will form one of the important strategies for the prevention of these emergencies.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Chowdary AN, Banerjee S, Brahma A, Biswas MK. Pesticide poisoning in nonfatal, deliberate self-harm: A public health issue. Indian J Psychiatry. 2007;49:117–20. doi: 10.4103/0019-5545.33259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eddleston M, Buckley NA, Eyer P, Dawson AH. Management of acute organophosphorus pesticide poisoning. Lancet. 2008;371:597–607. doi: 10.1016/S0140-6736(07)61202-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eddleston M, Gunnell D, Karunaratne A, de Silva D, Sheriff MH, Buckley NA. Epidemiology of intentional self poisoning in rural Sri Lanka. Br J Psychiatry. 2005;187:583–4. doi: 10.1192/bjp.187.6.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chowdary AN, Sanyal D, Dutta SK, Weiss MG. Deliberate self-harm by ingestion of poisons on Sagar island in Sunderban delta, India. Int Med J. 2003;10:85–91. [Google Scholar]
- 5.Sunder RJ, Kumar SS, Jayarajan A, Kuppuswamy G. Continuous infusion of high doses of atropine in the management of OP compound poisoning. J Assoc Physicians India. 1991;39:190–3. [PubMed] [Google Scholar]
- 6.Srinivas Rao CH, Venkateshwarlu V, Surender T, Eddleston M, Buckley NA. Pesticide poisoning in South India- opportunities for prevention and improved medical management. Trop Med Int Health. 2005;10:581–9. doi: 10.1111/j.1365-3156.2005.01412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unnikrishnan SB. A profile of acute poisoning in Mangalore. J Clin Forensic Med. 2006;13:112–6. doi: 10.1016/j.jcfm.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Abdollahi M, Jalali N, Sabzevari O, Nikfar SH, Fallahpour M. Pesticide poisoning during an 18-month period (1995-1997) in Tehran, Iran. Irn J Med Sci. 1999;24:77–81. [Google Scholar]
- 9.Shadnia S, Esmaily H, Sasanian G, Pajoumand A, Hassanian-Moghaddam H, Abdollahi M. Pattern of acute poisoning in Tehran-Iran in 2003. Hum Exp Toxicol. 2007;26:753–6. doi: 10.1177/0960327107083017. [DOI] [PubMed] [Google Scholar]
- 10.Yurumez Y, Durukan P, Yavuz Y, Ikizceli I, Avsarogullari L, Ozkan S, et al. Acute organophosphorus poisoning in university hospital emergency room patients. Int Med J. 2007;46:965–9. doi: 10.2169/internalmedicine.46.6304. [DOI] [PubMed] [Google Scholar]
- 11.Manfredini R, Gallerani M, Caracciolo S, Tomelli A, Calò G, Fersini C. Circadian variation in attempted suicide by deliberate self poisoning. BMJ. 1994;309:774–5. doi: 10.1136/bmj.309.6957.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhattarai N, Rauniyar A, Chaudhary D, Jaiswal S, Banthia, Rana BB. Patterns of OP poisoning in a teaching hospital. J Nepal Med Assoc. 2006;45:228–32. [PubMed] [Google Scholar]
- 13.Chugh SN, Dushyant, Ram S, Arora B, Malhotra KC. Incidence & outcome of aluminium phosphide poisoning in a hospital study. Indian J Med Res. 1991;94:232–235. [PubMed] [Google Scholar]
- 14.Jain AK, Nigam M, Garg SD, Dubey BP, Arora A. Aluminium phosphide poisoning autopsy findings. J Ind Academy Forensic Med. 2005;27:35–39. [Google Scholar]
- 15.Gargi J, Rai H, Chanana A, Rai G, Sharma G, Bagga IJ. Current trend of poisoning--a hospital profile. J Indian Med Assoc. 2006;104:72–3. [PubMed] [Google Scholar]
- 16.Shadnia S, Sasanian G, Allami P, Hosseini A, Ranjbar A, Amini-Shirazi N, et al. A retrospective 7-years study of aluminum phosphide poisoning in Tehran: Opportunities for prevention. Hum Exp Toxicol. 2009;28:209–13. doi: 10.1177/0960327108097194. [DOI] [PubMed] [Google Scholar]
- 17.Konradsen F, van der Hoek W, Cole DC, Hutchinson G, Daisley H, Singh S, et al. Reducing acute poisoning in developing countries—options for restricting the availability of pesticides. Toxicology. 2003;192:249–61. doi: 10.1016/s0300-483x(03)00339-1. [DOI] [PubMed] [Google Scholar]
- 18.FAO. International Code of Conduct on the Distribution and Use of Pesticides. FAO, Rome. 2002 [Google Scholar]
- 19.GCPF Sponsored Pilot Projects Fostering the Safe and Responsible Use of Crop Protection. Brussels, Belgium: Global Crop Protection Federation; 1998. [Last accessed date 24 July 2010]. Global Crop Protection Federation. Safe Use Pilot Projects:Guatemala, Kenya, and Thailand. Available from: http://www.gcpf.org . [Google Scholar]
- 20.Hruska AJ, Corriols M. The impact of training in integrated pest management among Nicaraguan maize farmers: Increased net returns and reduced health risk. Int J Occup Environ Health. 2002;8:191–200. doi: 10.1179/107735202800338777. [DOI] [PubMed] [Google Scholar]
- 21.Roberts DM, Buckley NA, Manuweera G, Eddleston M. Influence of Pesticide Regulation on Acute Poisoning Death in Sri Lanka. Bulletin of the WHO. 2003 [PMC free article] [PubMed] [Google Scholar]
- 22.Loevinsohn ME. Insecticide use and increased mortality in rural central Luzon. Philippines Lancet. 1987;13:1359–62. doi: 10.1016/s0140-6736(87)90659-3. [DOI] [PubMed] [Google Scholar]
- 23.Eddleston M, Karalliedde L, Buckley NA, Fernando R, Hutchinson G, Isbister G, et al. Pesticide poisoning in the developing world — a minimum pesticide list. Lancet. 2002;12:1163–7. doi: 10.1016/s0140-6736(02)11204-9. [DOI] [PubMed] [Google Scholar]
- 24.Gururaj G, Issac MK. Epidemiology of suicides in Bangalore. NIMHANS. 2001 May; Report no 43. [Google Scholar]
- 25.Baby S, Manju PH, Yesudas KF. Psychiatric diagnosis in attempted suicide. Calicut Med J. 2006;4 [Google Scholar]
- 26.Nagendra Gouda M, Rao SM. Factors Related to Attempted Suicide in Davanagere. Indian J Community Med. 2008;33:15–8. doi: 10.4103/0970-0218.39237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Akhlaghi M, Arbabi Z, Khadivi R. Pattern of Acute Poisoning in Shahrekord. Asian J Epidemiol. 2009;2:9–12. [Google Scholar]
- 28.Shah R, Uren Z, Baker A, Majeed A. Trends in deaths from drug overdose and poisoning in England and Wales 1993-1998. J Public health. 2001;23:242–6. doi: 10.1093/pubmed/23.3.242. [DOI] [PubMed] [Google Scholar]
- 29.Dash SK, Aluri SR, Mohanty MK, Patnaik KK, Mohanty S. Sociodemographic profile of poisoning cases. JIAFM. 2005;27:133–8. [Google Scholar]
- 30.Hawkins LC, Edwards JN, Dargan PI. Impact of restricting paracetamol pack sizes on paracetamol poisoning in the United Kingdom: A review of the literature. Drug Saf. 2007;30:465–79. doi: 10.2165/00002018-200730060-00002. [DOI] [PubMed] [Google Scholar]
- 31.US Food and Drug Administration. Public health problem of liver injury related to the use of acetaminophen in both over-the-counter (OTC) and prescription (RX) products. [Last accessed date 24 July 2010]. Available from: http://www.fda.gov .


