Abstract
Background and Aims:
Ventilator-associated pneumonia (VAP) is one of the most common Intensive Care Unit (ICU)-acquired infection. The aim of this study was to compare the clinical outcome of continuous and intermittent administration of piperacillin–tazobactam by serial measurements of the Clinical Pulmonary Infection Score (CPIS).
Subjects and Methods:
Groups were designed as parallel and the study was designed as quasi-experimental and conducted at a semi-closed ICU between September 2008 and May 2010. Patients received 3.375 g (piperacillin 3 g/tazobactam 0.375 g) either through intermittent infusion every 6 h for 30 min [Intermittent Infusion (II) group; n = 30] or through continuous infusion every 8 h for 4 h [Continuous Infusion (CI) group; n = 31]. CPIS was used to assess the clinical diagnosis and outcome of VAP patients.
Results:
Sex, age, Acute Physiology and Chronic Health Evaluation II II score on ICU admission, diagnosis and underlying disease of VAP patients were not significantly different in the CI (n = 31) and II (n = 30) groups. Duration of mechanical ventilation, length of stay, total number of antibiotics used per patient and duration of piperacillin/tazobactam treatment were similar in both groups. Mortality rates of VAP patients were similar between both groups during hospitalization.
Conclusion:
There was no significant difference in clinical outcomes of patients receiving piperacillin–tazobactam via CI or II when measured by serial CPIS score.
Keywords: Piperacillin, tazobactam, ventilator-associated pneumonia
Introduction
Ventilator-associated pneumonia (VAP) is one of the most common Intensive Care Unit (ICU)-associated infections in patients who receive ventilation support, which would prolong ICU and/or hospital lengths of stay, and induce high mortality rate and heavy financial burden on health care services.[1] The patient outcome could considerably develop by early and precise diagnosis, more selective anti-microbial use and better routes of administration.[2,3] Piperacillin–tazobactam is a broad-spectrum β-lactam-β-lactamase inhibitor antibiotic used for the treatment of critically ill patients with VAP.[4] It is recognized that β-lactams are time-dependent antibiotics and that their effectiveness is in association with duration of free drug concentrations over the minimum inhibitory concentration (t > MIC) of organisms.[5] Although the routine mode of piperacillin administration is intermittent infusion (II), continuous infusion (CI) may also be advocated for improving the time above the MIC.[6] Animal studies have confirmed the greater efficacy of β-lactam CI over II.[5,7] However, the clinical benefit of CI or II of β-lactam antibiotics is in doubt in humans. Clinical outcomes such as mortality,[8–16] time to normalization of leukocytosis or pyrexia,[10,14,17,18] adverse events,[19] microbiological outcome,[18,20] duration of mechanical ventilation[11,15,17,20] and length of stay are comparable between bolus and continuous dosing of β-lactam antibiotics in seriously ill patients.[11,15,17,19] CI of β-lactam antibiotics may not also lead to a significant progression in the clinical cure compared with an intermittent bolus.[9–11,13,15,17,21,22] On the other hand, clinical cure[20,21] and 14-day mortality[23] of VAP patients could be significantly improved in the CI group compared with the intermittent bolus. Thus, further studies are required to evaluate the outcomes between continuous and intermittent administration of β-lactam antibiotics in critically ill patients. Here, in this study, we attempted to compare the clinical outcomes of continuous and intermittent administration of piperacillin–tazobactam by serial measurements of the Clinical Pulmonary Infection Score (CPIS).
Materials and Methods
Groups were designed as parallel and the study was conducted as quasi-experimental at the semi-closed Intensive Care Unit (ICU) in a university hospital between September 2008 and May 2010. All of the following criteria were necessary for diagnosis of VAP: white blood cell count >10,000 cells/mm3 or <4000 cells/ mm3; body temperature >38°C or <35.5°; new onset of purulent sputum or a change in sputum character; chest radiography indicating new or progressive infiltrate and a significant quantitative pathogen culture from respiratory secretions (tracheal aspirate >106 colony-forming units/mL or growth of ≥104 colony-forming units/mL of microorganism on bronchoscopic broncho alveolar lavage (BAL) culture )or isolation of the same microorganism in blood and respiratory secretions on Day 3 and Day 8. All of them should be older than 18 years, and the estimated length of ventilation is greater than 48 h. The presence of Gram-negative bacteria was verified by a significant quantitative culture from respiratory secretions Exclusion criteria were hypersensitivity or allergy to β-lactam antibiotics, pregnancy or lactation, neutropenia (<1000 cells/mm3), acquired immunedeficiency syndrome (AIDS), glomerular filtration rate (GFR) <60 mL/min by the Cockcroft–Gault equation, solid or hematological tumor and finding of any other known source of infection such as early-onset hospital-acquired pneumonia (HAP) or health-care-associated pneumonia (HCAP) without any risk factors for multidrug-resistant (MDR) pathogens according to the VAP guidelines.[4] Seventy patients were eligible to enter the study. Nine patients expired on Day 8 and did not complete the study protocol to the final analysis. Patients received 3.375 g (piperacillin 3 g/tazobactam 0.375 g) either by II every 6 h for 30 min (I) group; n = 30) or CI every 8 h for 4 h (CI group; n = 31). CPIS was used to assess the clinical diagnosis and outcome of VAP.[24] Also, Acute Physiology and Chronic Health Evaluation II (APACHE II) score was primarily used to predict the mortality of the patients.[25] Clinical and laboratory data conforming to the APACHE II score were recorded on admission and CPIS was measured at the onset of VAP symptoms (Day 1) and at Day 3 and Day 8. The definition for the day of onset of VAP was the day that the attending physicians made the clinical diagnosis (according to both prior inclusion criteria and based on CPIS >6) and prescribed antimicrobials for VAP. Demographic data, diagnosis at the time of admission, comorbidities, antibiotic regimen, duration of mechanical ventilation, length of stays and pathogen responsible for VAP were also recorded. The value of APACHE II was used in the prediction of mortality of VAP patients. For outcome criteria, mortality during hospital stay was applied. CPIS was monitored closely on Days 1, 3 and 8, and changes of each CPIS component were analyzed throughout the course of VAP therapy.
Statistical analysis
Statistical analysis was performed using SPSS version 16.0 software (SPSS Inc., Chicago, IL, USA). Quantitative variables were reported as mean and standard deviation. Categorical variables were analyzed using the chi-square test or Fisher's exact test where appropriate, and continuous variable were compared using the Student T-test or Mann-Whitney U test. P-values <0.05 were considered significant.
Results
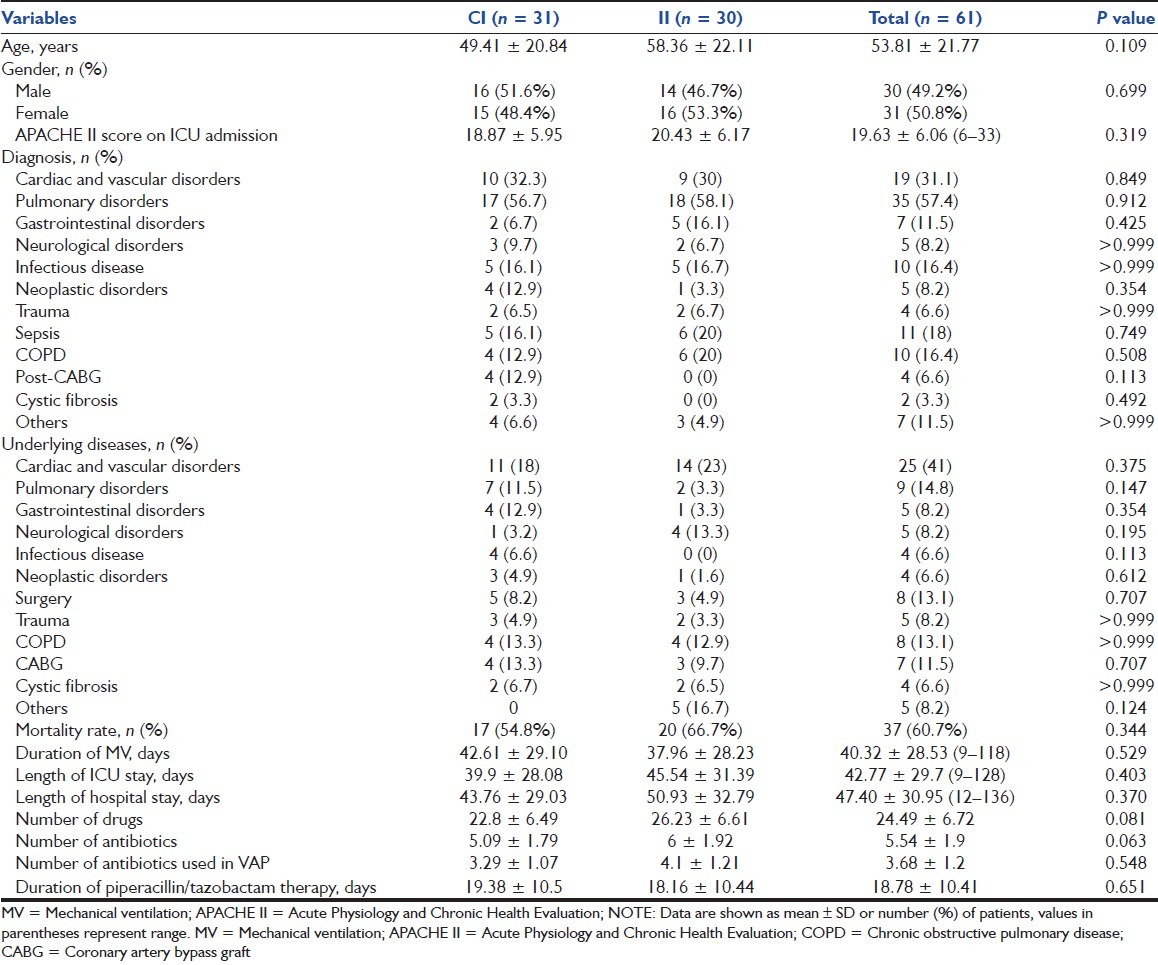
No significant differences were found between the CI (n = 31) and II (n = 30) groups for sex, age, APACHE II score on ICU admission, diagnosis and underlying disease of VAP patients. Mortality rates of VAP patients during hospitalization were similar in both groups. More deaths occurred in patients with a higher mean age (58.7 ± 19.9 years, P = 0.047). There were no significant differences in the duration of mechanical ventilation and length of stay between the two groups. The total number of antibiotics used per patient was similar in both groups. Duration of piperacillin/tazobactam treatment for VAP patients was not significantly different between the two groups [Table 1].
Table 1.
Baseline characteristics of patients with ventilator-associated pneumonia
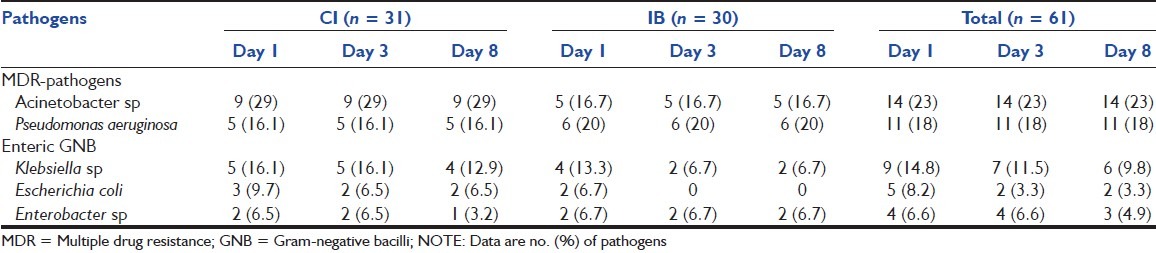
The distribution of bacterial pathogens isolated from BAL specimen on Days 1, 3 and 8 between the groups is displayed in Table 2. The most common microorganisms were Acinetobacter sp, Pseudomonas aeruginosa, Klebsiella sp, Escherichia coli and Enterobacter sp.
Table 2.
Pathogens responsible for VAP within the 8-day treatment
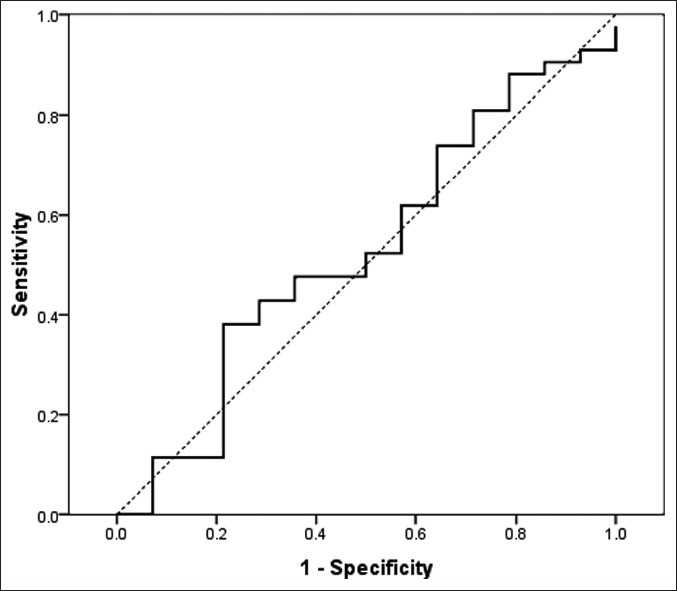
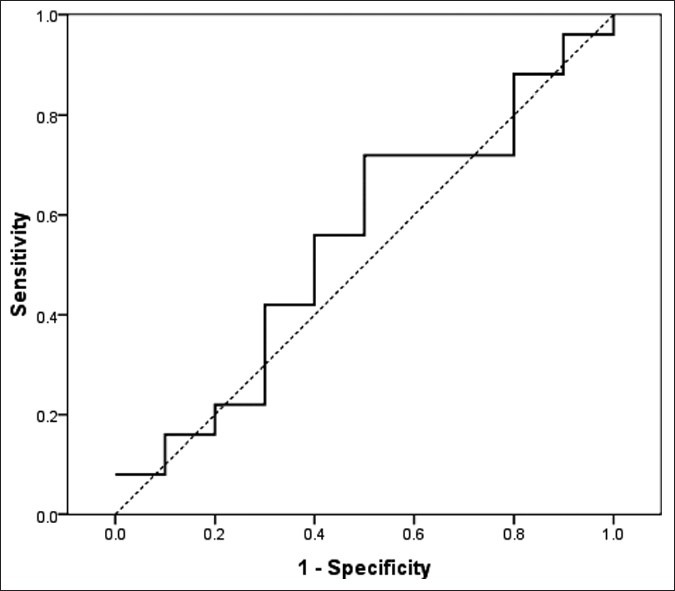
A time-dependent analysis of CPIS was conducted on the overall population and independently on patients who received CI or II of piperacillin/tazobactam. Our results demonstrated that CI of piperacillin–tazobactam was not associated with a significant improvement in clinical outcomes when compared with II. The CPIS score declined from Day 1 to Day 3 (8.70 ± 2.13 vs. 7.04 ± 1.55); thereafter, CPIS illustrated tendency to incline again from Day 3 up to Day 8 (8.55 ± 2.13 vs. 8.70 ± 2.13) in the population as a whole [Figure 1]. The mean CPIS scores were similar in both groups on Day 1 (7.12 ± 1.33 vs. 6.96 ± 1.77; P = 0.687), Day 3 (8.74 ± 1.76 vs. 8.66 ± 2.48; P = 0.892) and Day 8 (8.51 ± 2.07 vs. 8.60 ± 2.22; P = 0.880). The CPIS components’ scores were not significantly different between the two groups. Temperature did not show a significant improvement during the 8-day treatment of VAP in both groups [Figure 2]. Leukocyte count declined until Day 3, and then inclined until Day 8 in both groups (12536.8 cells/mm3 on Day 1, 13183.9 cells/mm3 on Day 3 and 12041.9 cells/mm3 on Day 8), but these changes were not significantly different in the two groups [Figure 3]. The PaO2/FiO2 ratio was not significantly increased in both groups. It increased from a value of 159.07 ± 79.9 on Day 1 to a value of 175.6 ± 67.3 on Day 3, and then decreased to a value of 162.7 ± 62.06 on Day 8. The PaO2/FiO2 increased from a value of 144.5 ± 64.9 on Day 1 to a value of 151.2 ± 57.6 on Day 3, and then decreased to a value of 142.5 ± 61.9 on Day 8 in the CI group [Figure 4]. Secretions did not show significant improvement within the 8-day treatment of VAP in both groups. The lung infiltrate did not show significant improvement within the 8-day treatment in both groups. The area under the curve (AUC) for receiver operating characteristics (ROC) curve was 0.543 (95% CI: 0.338–0.747) for CPIS on Day 1 in the CI group and 0.484 (95% CI: 0.273–0.695) for CPIS on Day 1 in the II group, 0.519 (95% CI: 0.316–0.721) for CPIS on Day 3 in the CI group and 0.534 (95% CI: 0.325–0.743) for CPIS on Day 3 in the II group, and 0.624 (95% CI: 0.435–0.813) for CPIS on Day 8 in the CI group and 0.602 (95% CI: 0.417–0.787) for CPIS on Day 8 in the II group; 0.578 (95% CI: 0.384–0.773) for APACHE II in the CI group and 0.614 (95% CI: 0.400–0.828) for APACHE II in the II group [Figures 5 and 6].
Figure 1.
Clinical pulmonary infection score changes within the 8-day treatment in the studied groups
Figure 2.
Temperature changes within the 8-day treatment in the studied groups
Figure 3.
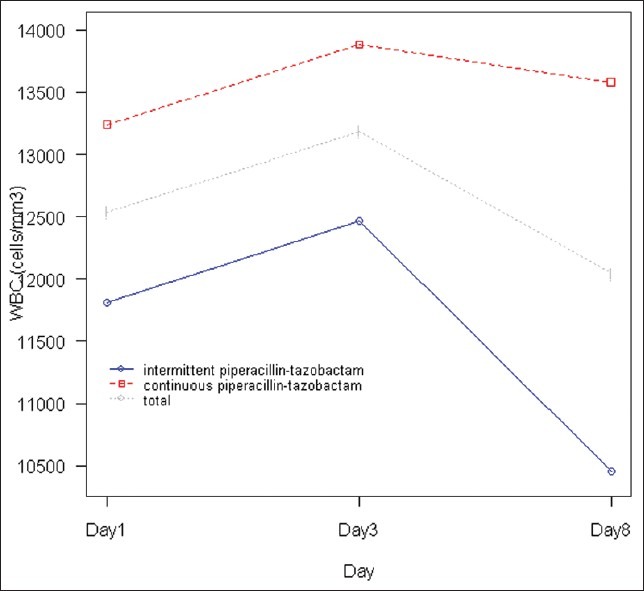
Leukocyte count changes within the 8-day treatment in the studied groups
Figure 4.
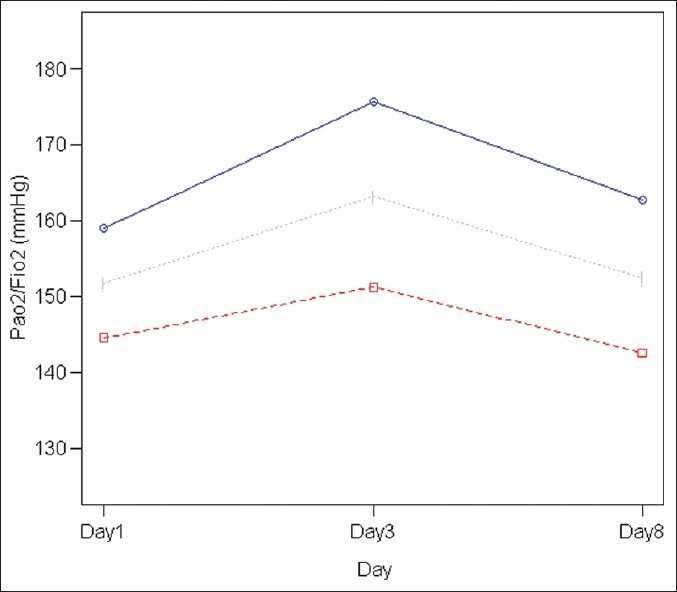
The PaO2/FiO2 ratio changes within the 8-day treatment in the studied groups
Figure 5.
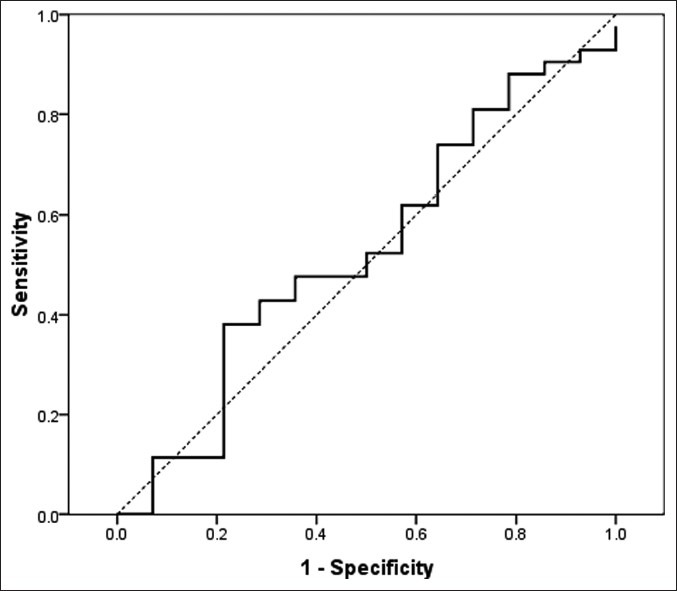
Receiver operating characteristic curve for acute physiology and chronic health evaluation II in the continuous infusion group
Figure 6.
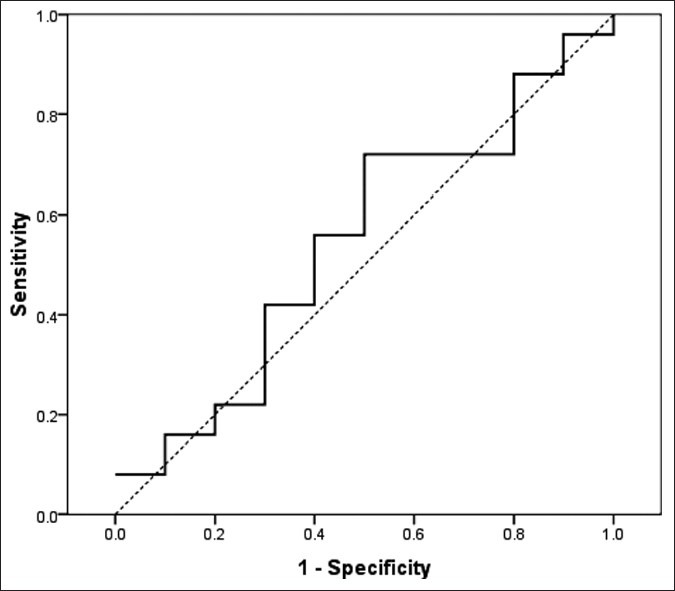
Receiver operating characteristic curve for acute physiology and chronic health evaluation II in the intermittent infusion group
Discussion
Dosing for infections has been revised since developments of pharmacodynamic characteristics of antimicrobials and different patterns of their bactericidal activity.[26] Although the standard mode of administration of piperacillin is II, CI is of particular importance for optimizing the time above the MIC (t > MIC) in clinical cure improvement.[6] In addition, several studies have evaluated clinical outcomes including severity of illness, duration of mechanical ventilation, mortality, clinical cure from actual infection, time to normalization of leukocytosis or pyrexia and lengths of ICU stay.[8–22] Similar to other studies,[11,20,23,27] no significant differences were found between the CI (n = 31) and the II (n = 30) groups in terms of sex, age, APACHE II score at ICU admission, diagnosis and microorganism responsible for VAP in this study. Consequently, mortality is not mainly dissimilar in the continuous and intermittent dosed groups.[8–11,13,14,20,27] Rapid improvement in PaO2/FiO2 has been granted as the most precise marker for adequate treatment. Duration of treatment was directly associated with the CPIS score at the time of pulmonary infection diagnosis in the Micek et al. study.[28] Also, duration of piperacillin–tazobactam therapy was correlated with the CPIS score at the onset of VAP symptoms (r = 0.364, P = 0.004), similar to our study. In this regard, CPIS scores from Day 1 to Day 8 and, more importantly, from Day 1 to Day 3 were not significantly different between the groups in our study. Although we observed that the temperature, leukocyte count (on Day 8), secretions and PaO2/FiO2 ratio (on Day 3) improved, these changes were mostly slight. We did not find any improvement in infiltrates. Similar studies have indicated limited value of chest radiography for clinical outcome assessment in patients with pneumonia,[29–31] while quickly deteriorating pathologies are indicative of either progression or recurrence of VAP. The PaO2/FiO2 ratio was the only parameter that increased slightly within 3 days of the onset, especially in group II, but did not achieve a normal value. Similar to our findings, Dennesen and coworkers demonstrated that temperature, PaO2/FiO2 ratio and leukocyte counts improved in time after initiation of antibiotic treatment, and the resolution of these parameters was generally slow.[32] Another study used CPIS to define whether a patient was responding to therapy, with most classic parameters of infection, such as amount and quality of secretions, radiographic infiltrate, leukocytosis and fever being poor indicators of t to therapy, while a more specific physiologic marker, the PaO2/FiO2 ratio, was more precise.[33] Temperature rise and leukocyte count are considered as reliable criteria for supporting VAP diagnosis; however, this may lead to incorrect decision because they are nonspecific markers in severely ill patients who suffer from sepsis, shock, physical stress or acute respiratory distress syndrome, or receive medications such as corticosteroids or b-agonists.[34,35] It emphasizes the effects of confounding factors such as underlying disease, prior antibiotic therapy, other medications in combination with piperacillin–tazobactam and previous treatment in each groups on outcome. In addition, lack of established criteria in our ICU compared with other studies produced a lower CPIS score on Day 3. Moreover, ample referral patients with preoccurred VAP episodes could have skewed our estimation for timing of VAP onset. Consequently, false and late diagnosis of VAP may have misleaded our CPIS scores on Days 1, 3 and 8. In previous VAP clinical trials, a wide range of mortality rates have been reported. By reviewing VAP studies since 1987, the rough mortality rates ranged from 24% to 76%. This wide range probably reflects differences in patient characteristics, underlying disease, diagnostic criteria and the pathogens involved.[36] According to another study, the mortality of Pseudomonas or Acinetobacter species-associated pneumonia was 87%, compared with a 55% mortality rate of pneumonia due to other organisms.[37] Similarly, Kollef et al. reported that patients with high-risk pathogens causing VAP (Pseudomonas aeruginosa, Acinetobacter spp and Stenotrophomonas maltophilia) had a considerably higher hospital mortality rate (65%) than VAP patients with other organisms (31%).[38] The mortality of 60.7% in the whole population, 66.7% in the II group and 54.8% in the CI group, of our study was close to those reports. Pseudomonas aeruginosa and Acinetobacter sp were detected as the most common MDR pathogens in our study. In this study, the etiology of VAP isolated from the BAL specimen during the course of piperacillin–tazobactam therapy on Days 1, 3 and 8 did not significantly vary between the two groups. The predominant Gram-negative bacteria were Acinetobacter sp and Pseudomonas aeruginosa, followed by Klebsiella sp, Escherichia coli and Enterobacter sp. Several studies have reported that more than 60% of VAP is caused by aerobic Gram-negative bacteria.[39,40] The limitations of our study include the fact that the two modes of administration were not compared using a randomized design, piperacillin–tazobactam serum concentrations were not determined and the microbiological and laboratory data were not available as soon as other clinical information or at the favorite days. Also, it was performed within a single ICU and in a small sample.
Conclusion
In conclusion, there were no significant differences in the clinical outcomes of patients receiving piperacilin/tazobactam via CI or II by serial measurements of CPIS score. Therefore, we should emphasize that before choosing the standard mode of administering β-lactams, more randomized clinical trials are necessary to establish the potential advantage of administering β-lactams by CI or II in accordance with the MIC of the microorganism responsible, the ratio of tissue and serum concentration, the volume of distribution of the antimicrobial agent and the stability of the antimicrobial agent once dissolved between the two groups.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Joseph NM, Sistla S, Dutta TK, Badhe AS, Parija SC. Ventilator-associated pneumonia. Eur J Intern Med. 2010;21:360–8. doi: 10.1016/j.ejim.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 2.Kollef MH, Schuster DP. Ventilator-associated pneumonia: Clinical considerations. AJR Am J Roentgenol. 1994;163:1031–5. doi: 10.2214/ajr.163.5.7976871. [DOI] [PubMed] [Google Scholar]
- 3.Memish ZA, Cunningham G, Oni GA, Djazmati W. The incidence and risk factors of ventilator-associated pneumonia in a Riyadh hospital. Infect Control Hosp Epidemiol. 2000;21:271–3. doi: 10.1086/501758. [DOI] [PubMed] [Google Scholar]
- 4.American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 5.Craig WA. Pharmacokinetic/pharmacodynamic parameters: Rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998;26:1–10. doi: 10.1086/516284. quiz 11-2. [DOI] [PubMed] [Google Scholar]
- 6.Turnidge JD. The pharmacodynamics of beta-lactams. Clin Infect Dis. 1998;27:10–22. doi: 10.1086/514622. [DOI] [PubMed] [Google Scholar]
- 7.Vondracek TG. Beta-lactam antibiotics: Is continuous infusion the preferred method of administration? Ann Pharmacother. 1995;29:415–24. doi: 10.1177/106002809502900413. [DOI] [PubMed] [Google Scholar]
- 8.Angus BJ, Smith MD, Suputtamongkol Y, Mattie H, Walsh AL, Wuthiekanun V, et al. Pharmacokinetic-pharmacodynamic evaluation of ceftazidime continuous infusion vs intermittent bolus injection in septicaemic melioidosis. Br J Clin Pharmacol. 2000;50:184–91. doi: 10.1111/j.1365-2125.2000.00179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pédeboscq S, Dubau B, Frappier S, Hernandez V, Veyssières D, Winnock S, et al. [Comparison of 2 administration protocols (continuous or discontinuous) of a time-dependent antibiotic, Tazocin] Pathol Biol (Paris) 2001;49:540–7. doi: 10.1016/s0369-8114(01)00210-3. [DOI] [PubMed] [Google Scholar]
- 10.Nicolau DP, McNabb J, Lacy MK, Quintiliani R, Nightingale CH. Continuous versus intermittent administration of ceftazidime in intensive care unit patients with nosocomial pneumonia. Int J Antimicrob Agents. 2001;17:497–504. doi: 10.1016/s0924-8579(01)00329-6. [DOI] [PubMed] [Google Scholar]
- 11.Georges B, Conil JM, Cougot P, Decun JF, Archambaud M, Seguin T, et al. Cefepime in critically ill patients: Continuous infusion vs.an intermittent dosing regimen. Int J Clin Pharmacol Ther. 2005;43:360–9. doi: 10.5414/cpp43360. [DOI] [PubMed] [Google Scholar]
- 12.Kojika M, Sato N, Hakozaki M, Suzuki Y, Takahasi G, Endo S, et al. [A preliminary study of the administration of carbapenem antibiotics in sepsis patients on the basis of the administration time] Jpn J Antibiot. 2005;58:452–7. [PubMed] [Google Scholar]
- 13.Lau WK, Mercer D, Itani KM, Nicolau DP, Kuti JL, Mansfield D, et al. Randomized, open-label, comparative study of piperacillin-tazobactam administered by continuous infusion versus intermittent infusion for treatment of hospitalized patients with complicated intra-abdominal infection. Antimicrob Agents Chemother. 2006;50:3556–61. doi: 10.1128/AAC.00329-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rafati MR, Rouini MR, Mojtahedzadeh M, Najafi A, Tavakoli H, Gholami K, et al. Clinical efficacy of continuous infusion of piperacillin compared with intermittent dosing in septic critically ill patients. Int J Antimicrob Agents. 2006;28:122–7. doi: 10.1016/j.ijantimicag.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 15.Roberts JA, Boots R, Rickard CM, Thomas P, Quinn J, Roberts DM, et al. Is continuous infusion ceftriaxone better than once-a-day dosing in intensive care? J Antimicrob Chemother. 2007;59:285–91. doi: 10.1093/jac/dkl478. [DOI] [PubMed] [Google Scholar]
- 16.Sakka SG, Glauner AK, Bulitta JB, Kinzig-Schippers M, Pfister W, Drusano GL, et al. Population pharmacokinetics and pharmacodynamics of continuous versus short-term infusion of imipenem-cilastatin in critically ill patients in a randomized, controlled trial. Antimicrob Agents Chemother. 2007;51:3304–10. doi: 10.1128/AAC.01318-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hanes SD, Wood GC, Herring V, Croce MA, Fabian TC, Pritchard E, et al. Intermittent and continuous ceftazidime infusion for critically ill trauma patients. Am J Surg. 2000;179:436–40. doi: 10.1016/s0002-9610(00)00388-3. [DOI] [PubMed] [Google Scholar]
- 18.Grant EM, Kuti JL, Nicolau DP, Nightingale C, Quintiliani R. Clinical efficacy and pharmacoeconomics of a continuous-infusion piperacillin-tazobactam program in a large community teaching hospital. Pharmacotherapy. 2002;22:471–83. doi: 10.1592/phco.22.7.471.33665. [DOI] [PubMed] [Google Scholar]
- 19.McNabb JJ, Nightingale CH, Quintiliani R, Nicolau DP. Cost-effectiveness of ceftazidime by continuous infusion versus intermittent infusion for nosocomial pneumonia. Pharmacotherapy. 2001;21:549–55. doi: 10.1592/phco.21.6.549.34539. [DOI] [PubMed] [Google Scholar]
- 20.Lorente L, Jiménez A, Martín MM, Iribarren JL, Jiménez JJ, Mora ML. Clinical cure of ventilator-associated pneumonia treated with piperacillin/tazobactam administered by continuous or intermittent infusion. Int J Antimicrob Agents. 2009;33:464–8. doi: 10.1016/j.ijantimicag.2008.10.025. [DOI] [PubMed] [Google Scholar]
- 21.Buck C, Bertram N, Ackermann T, Sauerbruch T, Derendorf H, Paar WD. Pharmacokinetics of piperacillin-tazobactam: Intermittent dosing versus continuous infusion. Int J Antimicrob Agents. 2005;25:62–7. doi: 10.1016/j.ijantimicag.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 22.van Zanten AR, Oudijk M, Nohlmans-Paulssen MK, van der Meer YG, Girbes AR, Polderman KH. Continuous vs.intermittent cefotaxime administration in patients with chronic obstructive pulmonary disease and respiratory tract infections: Pharmacokinetics/pharmacodynamics, bacterial susceptibility and clinical efficacy. Br J Clin Pharmacol. 2007;63:100–9. doi: 10.1111/j.1365-2125.2006.02730.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lodise TP, Jr, Lomaestro B, Drusano GL. Piperacillin-tazobactam for Pseudomonas aeruginosa infection: Clinical implications of an extended-infusion dosing strategy. Clin Infect Dis. 2007;44:357–63. doi: 10.1086/510590. [DOI] [PubMed] [Google Scholar]
- 24.Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM. Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic “blind” bronchoalveolar lavage fluid. Am Rev Respir Dis. 1991;143:1121–9. doi: 10.1164/ajrccm/143.5_Pt_1.1121. [DOI] [PubMed] [Google Scholar]
- 25.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 26.Nicolau D, Quintiliani R, Nightingale CH. Once-daily aminoglycosides. Conn Med. 1992;56:561–3. Erratum in: Conn Med 1992;56:694. [PubMed] [Google Scholar]
- 27.Patel GW, Patel N, Lat A, Trombley K, Enbawe S, Manor K, et al. Outcomes of extended infusion piperacillin/tazobactam for documented Gram-negative infections. Diagn Microbiol Infect Dis. 2009;64:236–40. doi: 10.1016/j.diagmicrobio.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 28.Micek ST, Ward S, Fraser VJ, Kollef MH. A randomized controlled trial of an antibiotic discontinuation policy for clinically suspected ventilator-associated pneumonia. Chest. 2004;125:1791–9. doi: 10.1378/chest.125.5.1791. [DOI] [PubMed] [Google Scholar]
- 29.Fagon JY, Chastre J, Hance AJ, Guiguet M, Trouillet JL, Domart Y, et al. Detection of nosocomial lung infection in ventilated patients.Use of a protected specimen brush and quantitative culture techniques in 147 patients. Am Rev Respir Dis. 1988;138:110–6. doi: 10.1164/ajrccm/138.1.110. [DOI] [PubMed] [Google Scholar]
- 30.Wunderink RG, Woldenberg LS, Zeiss J, Day CM, Ciemins J, Lacher DA. The radiologic diagnosis of autopsy-proven ventilator-associated pneumonia. Chest. 1992;101:458–63. doi: 10.1378/chest.101.2.458. [DOI] [PubMed] [Google Scholar]
- 31.Salata RA, Lederman MM, Shlaes DM, Jacobs MR, Eckstein E, Tweardy D, et al. Diagnosis of nosocomial pneumonia in intubated, intensive care unit patients. Am Rev Respir Dis. 1987;135:426–32. doi: 10.1164/arrd.1987.135.2.426. [DOI] [PubMed] [Google Scholar]
- 32.Dennesen PJ, van der Ven AJ, Kessels AG, Ramsay G, Bonten MJ. Resolution of infectious parameters after antimicrobial therapy in patients with ventilator-associated pneumonia. Am J Respir Crit Care Med. 2001;163:1371–5. doi: 10.1164/ajrccm.163.6.2007020. [DOI] [PubMed] [Google Scholar]
- 33.Luna CM, Blanzaco D, Niederman MS, Matarucco W, Baredes NC, Desmery P, et al. Resolution of ventilator-associated pneumonia: Prospective evaluation of the clinical pulmonary infection score as an early clinical predictor of outcome. Crit Care Med. 2003;31:676–82. doi: 10.1097/01.CCM.0000055380.86458.1E. [DOI] [PubMed] [Google Scholar]
- 34.Garrard CS, A’Court CD. The diagnosis of pneumonia in the critically ill. Chest. 1995;108(2 Suppl):17S–25S. doi: 10.1378/chest.108.2_supplement.17s. [DOI] [PubMed] [Google Scholar]
- 35.Abramson N, Melton B. Leukocytosis: Basics of clinical assessment. Am Fam Physician. 2000;62:2053–60. [PubMed] [Google Scholar]
- 36.Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165:867–903. doi: 10.1164/ajrccm.165.7.2105078. [DOI] [PubMed] [Google Scholar]
- 37.Fagon JY, Chastre J, Domart Y, Trouillet JL, Pierre J, Darne C, et al. Nosocomial pneumonia in patients receiving continuous mechanical ventilation.Prospective analysis of 52 episodes with use of a protected specimen brush and quantitative culture techniques. Am Rev Respir Dis. 1989;139:877–84. doi: 10.1164/ajrccm/139.4.877. [DOI] [PubMed] [Google Scholar]
- 38.Kollef MH, Silver P, Murphy DM, Trovillion E. The effect of late-onset ventilator-associated pneumonia in determining patient mortality. Chest. 1995;108:1655–62. doi: 10.1378/chest.108.6.1655. [DOI] [PubMed] [Google Scholar]
- 39.Torres A, Aznar R, Gatell JM, Jimenez P, Gonzalez J, Ferrer A, et al. Incidence, risk, and prognostic factors of nosocomial pneumonia in mechanically ventilated patients. Am Rev Respir Dis. 1990;142:523–8. doi: 10.1164/ajrccm/142.3.523. [DOI] [PubMed] [Google Scholar]
- 40.Spencer R. Predominant pathogens found in the European prevalence of infection in intensive care study. Eur J Clin Microbiol Infect Dis. 1996;15:281–5. doi: 10.1007/BF01695658. [DOI] [PubMed] [Google Scholar]


