Abstract
Focal nodular hyperplasia is a benign liver lesion incidentally discovered with increasing frequency because of the proliferation of imaging studies. Radiographic characterization can diagnose this pathologic lesion and nonoperative therapy is the standard of care. However, surgical resection may be required for diagnostic reasons or symptomatic patients. Depending on the anatomic location of the lesion, biopsy and/or resection can be performed laparoscopically. We herein report the case of a 26-year-old Japanese woman with a hepatic tumor who required a medical examination. Her medical history was negative for alcohol abuse, oral contraceptive administration and trauma. Clinical examination showed no significant symptoms. Ultrasonography, computed tomography and magnetic resonance imaging showed a mass located in the left lateral segment of the liver with a diameter of about 40 mm. It was difficult to diagnose the tumor definitively from these imaging studies, so we performed laparoscopic partial hepatectomy with successive firing of endoscopic staplers. The histopathological diagnosis was focal nodular hyperplasia. Surgical procedures and postoperative course were uneventful and the patient was discharged from the hospital on postoperative day 5.
Key words: Focal nodular hyperplasia, Laparoscopic partial hepatectomy, Benign liver tumor
Introduction
Focal nodular hyperplasia (FNH) is the second most common benign tumor of the liver, following hemangioma [1]. The definition was developed by Edmonson, who described it first in 1958 [2]. The pathogenesis of the disease is unknown [3]. However, it is thought to involve altered blood flow due to vascular malformation [4]. The prevalence of FNH is approximately 1% in the general population, and it is more frequent in women of reproductive age than in men (8:1) [5, 6]. Clinically, FNH is asymptomatic and discovered incidentally in 80% of cases [2]. The remaining 20% of patients with FNH have concurrent symptoms [3]. Occasionally, patients complain of chronic abdominal pain. Rarely, patients present with jaundice or nausea and vomiting. A palpable abdominal mass is present only 4% of the time [6]. FNH is discovered most often as an incidental finding on imaging studies or during abdominal surgery [3].
Differentiation of FNH and other hypervascular liver lesions, such as hepatocellular carcinoma (HCC), metastases and hepatocellular adenoma (HCA), is important because of the drastically different therapeutic approaches [7, 8]. HCC and metastases are always treated surgically as long as the general and local conditions do not contraindicate an operation, but HCA usually requires surgical removal because of the associated risk of hemorrhage or malignant transformation [2]. In contrast, FNH does not require treatment if it does not show associated symptoms, rapid increase in size or intralesional hemorrhage, which are considered indications for resection together with unclear radiologic aspect [9], which actually is the most frequent indication for surgery.
However, FNH can be well distinguished from other hypervascular lesions only if it shows a typical aspect. In contrast, in case of atypical FNH, imaging findings are not specific enough to provide a secure diagnosis and histologic verification of the lesion is required [2]. Here we report the case of a patient with a FNH resected laparoscopically.
Case Report
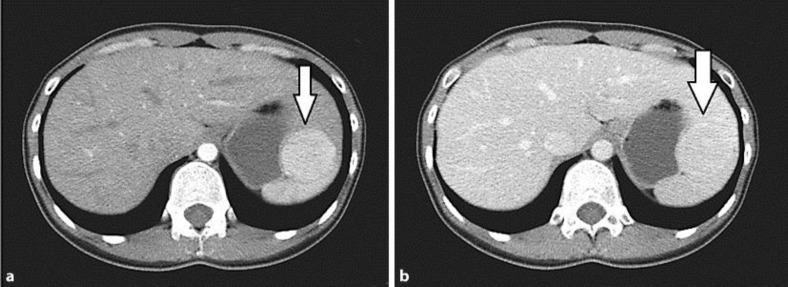
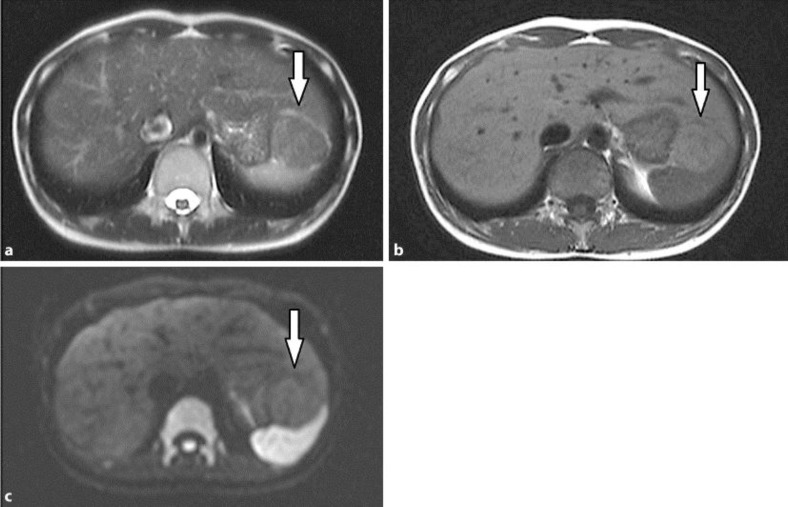
A 26-year-old Japanese woman required a medical examination and presented to our hospital. Her medical history was negative for alcohol abuse, oral contraceptive (OC) administration and trauma. Clinical examination showed no significant symptoms. Her complete blood counts including normal hemoglobin and platelet levels and the following: white blood cell count 4,100/μl, red blood cell count 376 × 104/μl, hemoglobin 11.2 g/dl, and platelets 20.4 × 104/μl. Laboratory studies showed normal albumin and liver enzymes, and negative hepatitis B surface antigen and antibodies to hepatitis C; prothrombin time was also unremarkable. Tumor markers including carcinoembryonic antigen (CEA), carbohydrate antigen 19-9 (CA19-9), α-fetoprotein (AFP), and PIVKA-II were within normal limits and as follows: CEA 1.0 ng/ml, CA19-9 <2.0 U/ml, AFP 2.3 ng/ml, and PIVKA-II 16 mAU. Ultrasonography documented a low-echoic mass with a diameter of 39 × 21 mm between the left lobe of the liver and the stomach. Computed tomography (fig. 1) showed a mass without a capsule located in the left lateral segment with a diameter of 39 × 37 mm. The mass was consistent with a solid, exophytic tumor. The tumor was highly hyperdense during the arterial phase, with no contrast enhancement in the late phase. No central scar was seen inside the lesion. Magnetic resonance imaging (fig. 2) detected a focal area about 40 × 34 mm in diameter, hypointense on T2-weighted images, isointense on T1-weighted images and hypointense on diffusion-weighted images. Since we could not diagnose it definitively as FNH from the results of imaging studies and taking into consideration its small size and superficial localization, and the patient being young and in a good general condition, laparoscopic resection of the lateral segment of the liver was planned.
Fig. 1.
Abdominal dynamic computed tomography showed a mass in the left lateral segment of the liver (arrow), which was highly hyperdense during the arterial phase (a), with no contrast enhancement in the late phase (b). The mass was 39 × 37 mm in diameter and consistent with a solid, exophytic tumor without central scar inside the lesion.
Fig. 2.
Magnetic resonance imaging showed a focal area of about 40 × 34 mm in diameter in the left lateral segment of the liver (arrow), hypointense on T2-weighted images (a), isointense on T1-weighted images (b) and hypointense on diffusion-weighted images (c).
After the induction of general anesthesia, in the lithotomy position, a 10 mm trocar was introduced through a small incision of the umbilical scar (open method) and laparoscopy was performed under carbon dioxide pneumoperitoneum, with abdominal pressure maintained below 10 mm Hg. A trocar of 12 mm was introduced in the right lateral quadrant and three other trocars of 5 mm were introduced in the right upper quadrant, the left lateral quadrant, and the epigastric region. The tumor was located in the peripheral left lateral segment of the liver without invasion to the stomach and spleen. We resected the tumor with firing of endoscopic staplers two times. After the resection was complete, the specimen was placed into a plastic bag and its extraction was performed through the slightly enlarged umbilical trocar incision. Operating time was 118 min with limited blood loss.
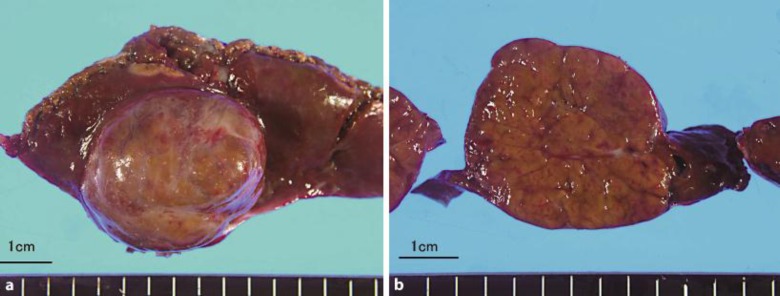
The 48 g specimen (fig. 3) measured 4 × 4 × 5 cm and was composed of mature hepatocytes, ductular reaction and abnormal vessels, so it was FNH histologically, without a central scar. This tumor was hard to diagnose as HCA, there being ductular reaction and no inflammation. These hepatocytes were mature and the background liver was normal, so this tumor was also hard to diagnose as dysplastic nodule and HCC. Surgical procedure and postoperative course were uneventful and the patient was discharged from the hospital on postoperative day 5.
Fig. 3.
The macroscopic specimen showed a nonencapsulated solitary mass in the left lateral segment of the liver, which was 48 g and 4 × 3.5 cm in diameter (a, b). Microscopic examination showed this tumor to be composed of mature hepatocytes, ductular reaction and abnormal vessels, and revealed FNH without a central scar.
Discussion
FNH is the second most common benign tumor of the liver, following hemangioma [1]. The pathogenesis of the disease is unknown [3]. FNH is more frequent in women of reproductive age than in men (8:1) [5, 6]. Although widely investigated, the relationship of OCs to FNH is not well characterized [3]. Recent studies have indicated that there is no association between FNH and the use of OCs [3]. However, OCs may promote FNH progression because patients taking OCs tend to have larger lesions and are more likely to be symptomatic [10]. FNH is often discovered incidentally on imaging studies or during abdominal surgery [3]. In our case, the patient was a young woman, but she had not taken OCs before. She was also asymptomatic and just underwent a general medical examination.
When we find FNH incidentally, we have to distinguish the tumor from other solid liver tumors. The examination of a resected specimen remains the gold standard when radiographic studies cannot clarify the diagnosis [11]. Once confirmed, FNH is usually treated conservatively [2]. Indications for surgery include progressive disease, increasing pain and a lesion for which malignancy cannot be ruled out [9].
Laparoscopic surgery has benefits for many traditional open procedures including appendectomy, cholecystectomy, nephrectomy and splenectomy [12, 13, 14, 15]. Recently, minimally invasive resection of solid liver tumors has been documented in the literature [3]. However, laparoscopic surgery for liver resection is a highly specialized procedure because the liver, given its unique anatomical features, presents technical difficulties for surgery such as the control of bleeding and bile leakage from the intrahepatic vessels. However, important technological developments and improved endoscopic procedures are being established. Equipment modifications, such as intraoperative ultrasonography, ultrasonic dissection, microwave coagulators and argon laser beam coagulators, have all been recognized for their efficacy in liver surgery, as has the introduction of endoscopic linear staplers and laparoscopic coagulation shears. Thus, laparoscopic partial hepatectomy has recently been performed more often [16]. There have been reports of laparoscopic right and left lobectomy [17, 18], and laparoscopic surgery has also been applied to left lateral segmentectomy for living donor liver for transplantation [19]. The anatomical location of the lesion is the most important determinant of laparoscopic resectability [3]. Anterolateral lesions, Couinaud segments II-VI, are most amenable to the laparoscopic approach [20]. In our case, we thought the tumor might be FNH from the imaging studies, but we could not diagnose it as FNH definitively. In addition, the tumor was located in the peripheral left lateral segment of the liver, so we performed not a laparotomy but laparoscopic surgery safely, which is considered less invasive and more cosmetic.
In conclusion, whenever clinicians, radiologists and surgeons are faced with difficulty, we have to make a complete diagnosis. The importance of differentiating these diseases should not be underestimated simply because of their benignity. Moreover, surgical resection should not be considered as a failure of the preoperative diagnostic attempt, but as the mainstay for definitive diagnosis [2]. We suggest that laparoscopic surgery is a good alternative to open surgery for minor liver resection in selected patients. Further studies with a large number of cases, a longer follow-up period and prospective randomization are needed for better definition of the role of laparoscopic hepatectomy.
Disclosure Statement
The authors declare that they have no conflicts of interest.
References
- 1.Karhunen PJ. Benign hepatic tumours and tumour like conditions in men. J Clin Pathol. 1986;39:183–188. doi: 10.1136/jcp.39.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Carlo I, Pulvirenti E, Toro A, Priolo GD. Adenoma or atypical hepatic focal nodular hyperplasia: role of preoperative imaging and laparoscopic treatment. Surg Laparosc Endosc Percutan Tech. 2010;20:e105–e109. doi: 10.1097/SLE.0b013e3181e0b2e6. [DOI] [PubMed] [Google Scholar]
- 3.Felsher J, Brody F. Laparoscopic resection of focal nodular hyperplasia. Surg Laparosc Endosc Percutan Tech. 2003;13:276–279. doi: 10.1097/00129689-200308000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Wanless IR, Mawdsley C, Adams R. On the pathogenesis of focal nodular hyperplasia of the liver. Hepatology. 1985;5:1194–1200. doi: 10.1002/hep.1840050622. [DOI] [PubMed] [Google Scholar]
- 5.Wanless IR, Albrecht S, Bilbao J, Frei JV, Heathcote EJ, Roberts EA, Chiasson D. Multiple focal nodular hyperplasia of the liver associated with vascular malformations of various organs and neoplasia of the brain: a new syndrome. Mod Pathol. 1989;2:456–462. [PubMed] [Google Scholar]
- 6.Nguyen BN, Fléjou JF, Terris B, Belghiti J, Degott C. Focal nodular hyperplasia of the liver: a comprehensive pathologic study of 305 lesions and recognition of new histologic forms. Am J Surg Pathol. 1999;23:1441–1454. doi: 10.1097/00000478-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Kim TK, Jang HJ, Burns PN, Murphy-Lavallee J, Wilson SR. Focal nodular hyperplasia and hepatic adenoma: differentiation with low-mechanical-index contrast-enhanced sonography. AJR Am J Roentgenol. 2008;190:58–66. doi: 10.2214/AJR.07.2493. [DOI] [PubMed] [Google Scholar]
- 8.Herman P, Pugliese V, Machado MA, Montagnini AL, Salem MZ, Bacchella T, D'Albuquerque LA, Saad WA, Machado MC, Pinotti HW. Hepatic adenoma and focal nodular hyperplasia: differential diagnosis and treatment. World J Surg. 2000;24:372–376. doi: 10.1007/s002689910059. [DOI] [PubMed] [Google Scholar]
- 9.Bonney GK, Gomez D, Al-Mukhtar A, Toogood GJ, Lodge JP, Prasad R. Indication for treatment and long-term outcome of focal nodular hyperplasia. HPB (Oxford) 2007;9:368–372. doi: 10.1080/13651820701504173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pain JA, Gimson AE, Williams R, Howard ER. Focal nodular hyperplasia of the liver: results of treatment and options in management. Gut. 1991;32:524–527. doi: 10.1136/gut.32.5.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bioulac-Sage P, Balabaud C, Bedossa P, Scoazec JY, Chiche L, Dhillon AP, Ferrell L, Paradis V, Roskams T, Vilgrain V, Wanless IR, Zucman-Rossi J, Laennec and Elves groups Pathological diagnosis of liver cell adenoma and focal nodular hyperplasia: Bordeaux update. J Hepatol. 2007;46:521–527. doi: 10.1016/j.jhep.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 12.Frazee RC, Roberts JW, Symmonds RE, Snyder SK, Hendricks JC, Smith RW, Custer MD, 3rd, Harrison JB. A prospective randomized trial comparing open versus laparoscopic appendectomy. Ann Surg. 1994;219:725–728. doi: 10.1097/00000658-199406000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW. Laparoscopic cholecystectomy. The new ‘gold standard’? Arch Surg. 1992;127:917–921. doi: 10.1001/archsurg.1992.01420080051008. discussion 921-923. [DOI] [PubMed] [Google Scholar]
- 14.Clayman RV, Kavoussi LR, Soper NJ, Dierks SM, Merety KS, Darcy MD, Long SR, Roemer FD, Pingleton ED, Thomson PG. Laparoscopic nephrectomy. N Engl J Med. 1991;324:1370–1371. doi: 10.1056/NEJM199105093241917. [DOI] [PubMed] [Google Scholar]
- 15.Lefor AT, Melvin WS, Bailey RW, Flowers JL. Laparoscopic splenectomy in the management of immune thrombocytopenia purpura. Surgery. 1993;114:613–618. [PubMed] [Google Scholar]
- 16.Mamada Y, Yoshida H, Taniai N, Mizuguchi Y, Kakinuma D, Ishikawa Y, Yokomura S, Arima Y, Akimaru K, Tajiri T. Usefulness of laparoscopic hepatectomy. J Nippon Med Sch. 2007;74:158–162. doi: 10.1272/jnms.74.158. [DOI] [PubMed] [Google Scholar]
- 17.Cherqui D, Husson E, Hammoud R, Malassagne B, Stéphan F, Bensaid S, Rotman N, Fagniez PL. Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg. 2000;232:753–762. doi: 10.1097/00000658-200012000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gigot JF, Glineur D, Santiago Azagra J, Goergen M, Ceuterick M, Morino M, Etienne J, Marescaux J, Mutter D, van Krunckelsven L, Descottes B, Valleix D, Lachachi F, Bertrand C, Mansvelt B, Hubens G, Saey JP, Schockmel R. Laparoscopic liver resection for malignant liver tumors: preliminary results of a multicenter European study. Ann Surg. 2002;236:90–97. doi: 10.1097/00000658-200207000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cherqui D, Soubrane O, Husson E, Barshasz E, Vignaux O, Ghimouz M, Branchereau S, Chardot C, Gauthier F, Fagniez PL, Houssin D. Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet. 2002;359:392–396. doi: 10.1016/S0140-6736(02)07598-0. [DOI] [PubMed] [Google Scholar]
- 20.Katkhouda N, Hurwitz M, Gugenheim J, Mavor E, Mason RJ, Waldrep DJ, Rivera RT, Chandra M, Campos GM, Offerman S, Trussler A, Fabiani P, Mouiel J. Laparoscopic management of benign solid and cystic lesions of the liver. Ann Surg. 1999;229:460–466. doi: 10.1097/00000658-199904000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]