Abstract
Introduction:
Hepatitis B virus (HBV) infection is a serious global public health problem affecting billions of people globally. The lack of information of its seroprevalence among the general population is an obstacle for formulating effective policies to reduce the burden viral hepatitis. Therefore, this population based serological survey was conducted in Kurdistan province, where no epidemiological data was available to determine the prevalence and risk factors of HBV infection.
Methods:
1613 healthy subjects were selected from all districts of Kurdistan province (in the western of Iran) using random cluster sampling. The subjects’ age ranged from 6 to 65 years old. Serum samples were tested for HBcAb, HBsAg and anti-HDV antibody. Screening tests were carried out by the third generation of ELISA. Various risk factors were recorded and multivariate analysis was performed.
Results:
The prevalence of HBsAg and HBcAb in Kurdistan was before 0.80% (95% CI 0.44; 1.34) and 5.02% (95% CI 4.03; 6.17), respectively. None of HBsAg carriers had positive anti-HDV antibody. Predictors of HBsAg or HBcAb in multivariate analysis were: older age and marriage. We did not find any significant differences between males and females.
Conclusion:
Our population based study suggests that intrafamilial HBV transmission plays a major role in HBV transmission in Kurdistan province. Furthermore, approximately 5% of general population in this province has prior exposure to HBV and less than 1% is HBsAg carriers. However, we could not find any case of HDV infection among them.
Keywords: Hepatitis B virus, prevalence, epidemiology, Iran
INTRODUCTION
Hepatitis B is one of the major health problems in the world and around two billion people are infected globally and most of them are Asian.[1] Just like other developing countries, hepatitis B virus (HBV) infection is the main cause of chronic liver disease in Iran.[2,3] It has been reported that 51-56% of Iranian cirrhotic patients are hepatitis B surface antigen (HBsAg) positive.[4,5] In 1979 seroprevalence of HBsAg was reported between 2.5% and 7.2%.[6] In that time it was estimated that approximately one million HBsAg positive carriers were living among 35 million Iranians. In 1990s rate of HBV infection was reported between 1.07 and 5% among blood donors or general population[3,7–10] and in 2000s between 1 and 2% in different provinces.[10–14] In fact, during the last two decades, obligatory infantile HBV vaccination with more than 95% of coverage has led to significant decline in rate of HBV infection in Iran.[2,15,16] In 2008, in a systematic review of literature we gathered and pooled available data on seroepidemiology of HBV infection in general population of Iran. The HBV infection prevalence in Iran was estimated 2.14% (95% CI: 1.92; 2.35). Despite unreliable meta-analysis, its comprehensive literature review showed that, the data were available for only 7 out of 30 provinces of Iran.[17] Kurdistan is one of the provinces with missing data regarding seroprevalence of HBV infection.
From public health view, in addition to seroepidemiology, the risk factors of HBV infection is of great important, since with proper intervention, HBV seroepidemiology can be contained. The major known risk factors for transmission of HBV are from HBsAg positive pregnancy, transfusion, hospitalization, tattoo, intravenous drug abuse and high risk sexual behaviors.[18,19] Since the lack of information on HBV prevalence and distribution of its risk factors among the general population is an obstacle for formulating effective policies to reduce the burden viral hepatitis, this population based study was designed to determinate accurate estimate of HBV infection epidemiology and associated risk factors in Kurdistan province. Kurdistan is a province with 54,592 km2 area and 2,880,312 populations that is located at western part of Iran. This province is of great importance since it has common border with Iraq that have impaired health care system and lacks major health statistics including rate HBV infection.
METHODS
Study population
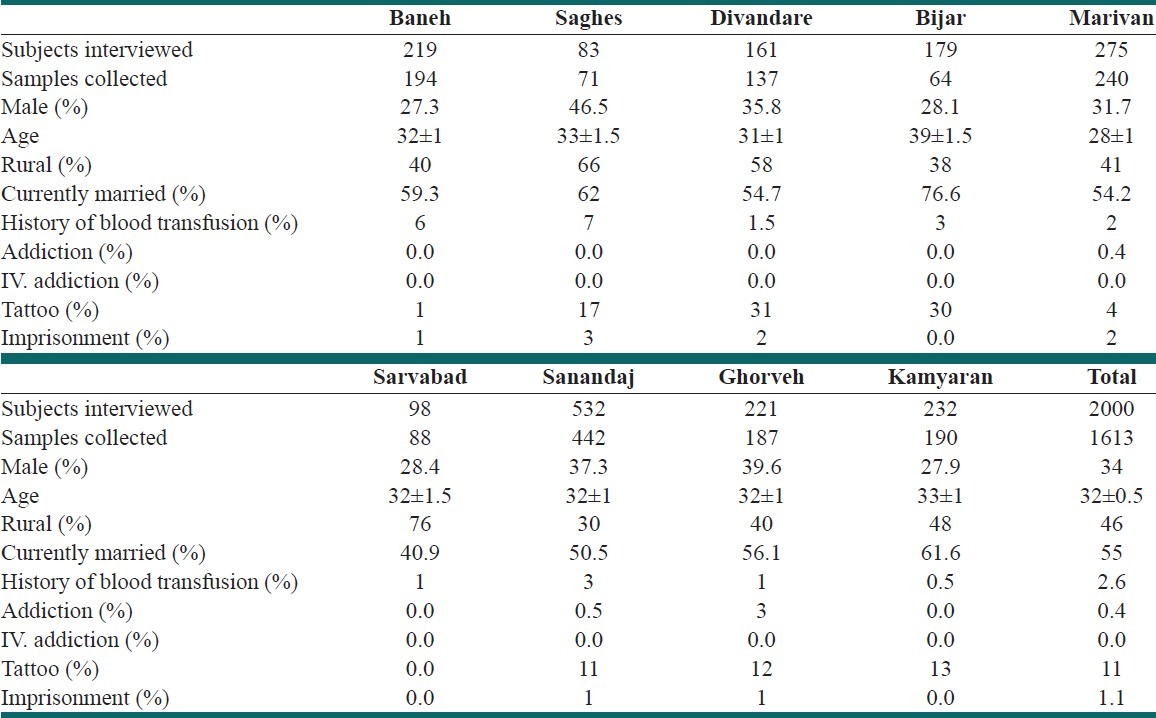
The general population of Kurdistan (in the western of Iran) was studied [Table 1]. Subjects between 6 and 65 years of age were included. Temporal inhabitants of the household, non-Iranian nationalities or those who did not consent to the study were excluded. The demographic characteristics of Kurdistan province are given in Table 2.
Table 1.
Census information–Kurdistan and 9 studied districts
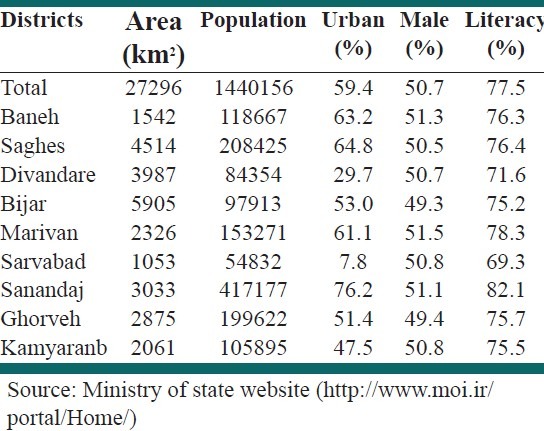
Table 2.
Demographic data of the study population
Sample size calculation
The sample size was determined using [DEFF*Np(1-p)]/[(d2/Z21-α/2*(N-1)+p*(1-p)] equation, when N is population size (1,440,518), P is Hypothesized % frequency of outcome factor in the population (here 5% ± 2), d is Confidence limits as % of 100 (absolute ±%, here 2%) and DEFF is design effect for cluster surveys that was set to 1. The sample size was calculated 1796 subjects with 99.99% confidence level. This number was rounded up to 2000 subjects.
Sampling and randomization
Clustered random sampling was used. One hundred clusters were selected from nine districts within Kurdistan province with a cluster size of 20. Postal code or family registry code was used to randomly select the first household for each cluster. Blood samples were obtained from each subject and a questionnaire was completed by a trained interviewer. The questionnaire included demographic and anthropometric data and risk factors for hepatitis B.
Laboratory tests
The blood samples were transferred to the regional laboratory. After separation of serum from blood samples in local laboratory, serums were frozen in –20°C and transferred to the central laboratory of Iranian Blood transfusion organization. HBsAg, HBcAb, and anti-HDV antibody were evaluated using Enzygnost HBsAg, 5.0 kit (Dade Behring, Germany), Hepanostica anti-HBc Uni-Form kit (Biomerieux, France), and (ETI-ABDELTAK-2; Diasorin, Dietzenbach, Germany), respectively.
Ethics
The study was approved by the Institutional Review Board of the Baqiyatallah University of Medical Sciences, Baqiyatallah Research Center for Gastroenterology and Liver Disease and Iranian Blood Transfusion Organization. Written informed consent was obtained from all subjects before data collection.
Statistical analysis
Statistics of all variables are summarized in Tables. Continuous variables are presented as mean values±standard deviation (SD), while qualitative and discrete variables are presented as absolute and relative frequencies in the form of percentage. Chi-squared test was applied to assess associations between categorical variables. The 95% CI for rate of HBcAb or HBsAg positivity was calculated by Mid P-Exact method if NPQ ≤5 when N is sample size, P is the rate of positive cases and Q is 1 – (rate of positive cases). If NPQ had been ≥5, then normal approximation method (Wald) would have been used to make 95% CI. The comparisons between continuous and qualitative variables were performed by student's t-test. Multivariable logistic-regression analysis involving recorded risk factors and patients’ characteristics that had significant P value in univariate analysis of HBV serostatus was performed to identify independent predictors of positive HBV seromarkers. A stepwise procedure was deployed with P = 0.05 as the threshold level for variables to be entered into and retained in the final model, and P = 0.1 as the threshold level for variables to be removed. All computations were carried out using SPSS version 18.
RESULTS
A total of 2000 subjects were interviewed from 9 districts of Kurdistan province. 387 subjects that refused to give blood sample or had inadequate sample were excluded. A total of 1613 samples were analyzed. The demographic characteristics of study population are given in Table 2.
Totally 81, 5.02% (95% CI 4.03; 6.17), and 13, 0.80% (95% CI 0.44; 1.34) subjects from 1613 participants were HBcAb and HBsAg positive, respectively. The rate of positive HBV seromarkers in various districts of Kermanshah province is given in Figure 1.
Figure 1.
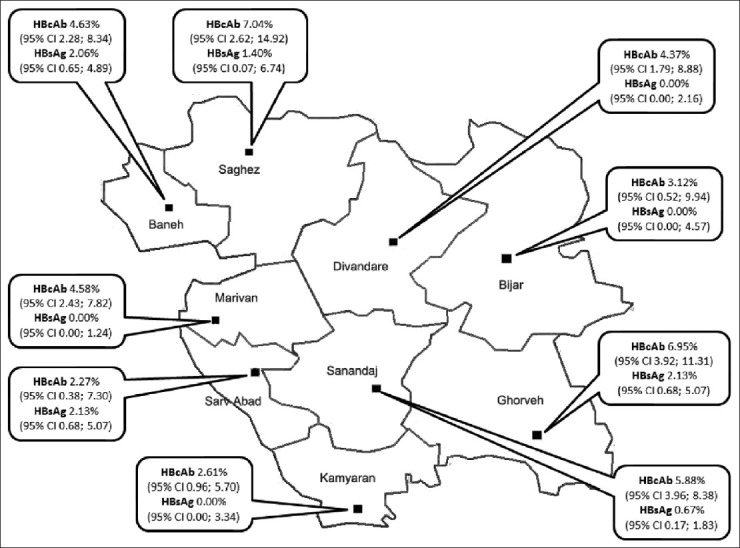
Geographical distribution of HBcAb and HBsAg seropositivity in various districts of Kurdistan province
HBcAb seroprevalence ranged between 2 and 7%. No case of HBsAg positive was found in Divandare, Bijar, Kamyaran and Marivan. In Sarv Abad, Ghorveh and Baneh, around 2% of general population was HBsAg positive. In univariate analysis, there was no significant difference in the rate of HBsAg (P=0.1) or HBcAb (P=0.8) among various districts. Table 3 shows the age-specific seroprevalence of HBcAb for each sex. It can be seen that HBcAb seroprevalence and the difference between males and females increase with age group.
Table 3.
Seroprevalence of HBcAb in male and female subjects in different age groups
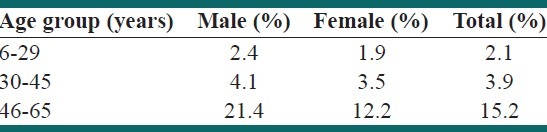
Figure 2 shows univariate analyses of studied risk factors. Marital status, age and literacy were significant risk factors of HBcAb or HBsAg seropositivity.
Figure 2.
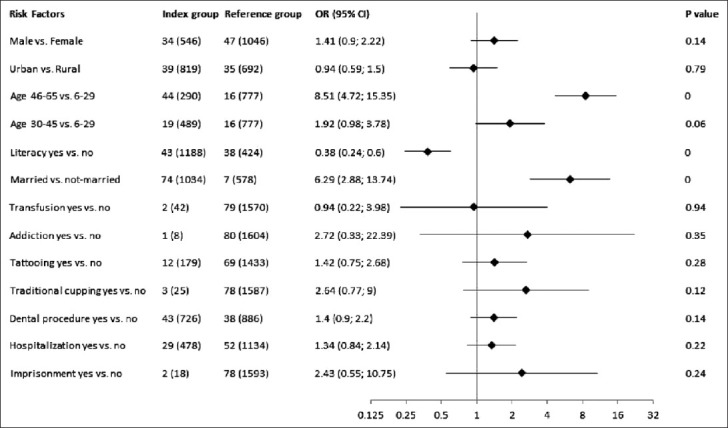
Risk factors associated with HBcAb or HBsAg in univariate analysis
Figure 3 shows multivariate analysis of risk factors with significant P values in univariate analyses. Age group 46-65 and marital status were independent predictors of HBcAb or HBsAg seropositivity.
Figure 3.
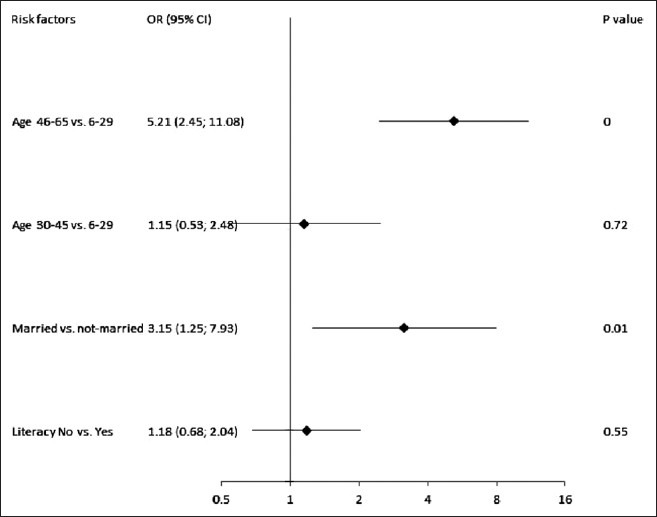
Risk factors associated with HBcAb or HBsAg in multivariate analysis
DISCUSSION
Hepatitis B virus (HBV) infection is a major cause of liver disease in the world. WHO has estimated that in more than 350 million people acute infection have turned to chronic infection. It is also estimated that more than 500,000 deaths occur annually mainly of cirrhosis and hepatocellular carcinoma caused by chronic HBV infection.[2,6] Monitoring of several scattered population based studies that have been carried out in different part of Iran shows that HBV prevalence has decreased dramatically in Iranian population during the last decade. It is now considerably less than many developing countries and only slightly higher than that seen in industrialized countries such as the United States.[20,21] Improvement of the people's knowledge about HBV risk factors, national vaccination program from 1993 for all neonates, vaccination of high risk groups such as healthcare workers and the introduction of disposable syringes for use in vaccinations, hospitals and clinics might justify this decrease. Unfortunately there were no available data from Kurdistan province so we could identify the trend of HBV epidemiology in the general population after introduction of universal HBV vaccination program.
Our current survey shows that approximately less than 1% and around 5% of the general population in Kurdistan province are chronic HBsAg carrier and had previous exposure to HBV infection. We can estimate that 23,042 chronic HBsAg carriers are living in this province and 144,016 have resolved HBV infection and some have occult HBV infection and are at greater risk of cirrhosis and hepatocellular carcinoma.
In multivariate analysis only age and marital status were independent risk factors for HBV seropositivity. Age is a common risk factor that almost is reported in all of seroepidemiologic studies of HBV infection. The reason is that the risk and cumulative frequency of high risk behaviors increase with age and consequently increase the rate of HBV exposure. Another independent risk factor of HBV seropositivity was being married. 10 and 1% of married subjects had positive HBcAb and HBsAg, respectively. Therefore checking couples before marriage and vaccination are advisable since they can considerably decrease the prevalence of HBV infection in this province.
CONCLUSION
Our population based study suggests that intrafamilial HBV transmission plays a major role in HBV transmission in Kurdistan province. Furthermore, approximately 5% of general population in this province has prior exposure to HBV and less than 1% is HBsAg carriers. However, we could not find any case of HDV infection among them.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Te HS, Jensen DM. Epidemiology of hepatitis B and C viruses: A global overview. Clin Liver Dis. 2010;14:1–21. doi: 10.1016/j.cld.2009.11.009. vii. [DOI] [PubMed] [Google Scholar]
- 2.Alavian SM, Fallahian F, Lankarani KB. The changing epidemiology of viral hepatitis B in Iran. J Gastrointestin Liver Dis. 2007;16:403–6. [PubMed] [Google Scholar]
- 3.Merat S, Malekzadeh R, Rezvan H, Khatibian M. Hepatitis B in Iran. Arch Iran Med. 2000;2:192–201. [Google Scholar]
- 4.Lankarani KB, Froozi MS, Nabipoor I, Fattahi F, Sarafrazyazdi M, Malekzadeh R, et al. Reassessment of the role of hepatitis B and C viruses in postnecrotic cirrhosis and chronic hepatitis in southern Iran. Irn J Med Sci. 1999;24:117–21. [Google Scholar]
- 5.Shamszad M, Farzadegan H. related cirrhosis and hepatocellular carcinoma in Iran. Journal of Iranian Medical Council. 1982;8:228. [Google Scholar]
- 6.Farzadegan H, Shamszad M, Noori-Arya K. Epidemiology of viral hepatitis among Iranian population: A viral marker study. Ann Acad Med Singapore. 1980;9:144–8. [PubMed] [Google Scholar]
- 7.Malekzadeh R, Khatibian M, Rezvan H. Viral hepatitis in the world and Iran. Journal of Iranian Medical Council. 1997;15:183–200. [Google Scholar]
- 8.Toukan AU. Control of hepatitis B in the Middle East. In: Rizetto M, Purcell RH, Gerin JL, Verme G, editors. Viral Hepatitis and Liver Diseases. 1st ed. Turin: Minerva Media; 1997. pp. 678–80. [Google Scholar]
- 9.Amini S, Mahmoodi MF, Andalibi S, Solati AA. Seroepidemiology of hepatitis B, delta and human immunodeficiency virus infections in Hamadan province, Iran: A population based study. J Trop Med Hyg. 1993;96:277–87. [PubMed] [Google Scholar]
- 10.Ghavanini AA, Sabri MR. Hepatitis B surface antigen and anti-hepatitis C antibodies among blood donors in the Islamic Republic of Iran. East Mediterr Health J. 2000;6:1114–6. [PubMed] [Google Scholar]
- 11.Alizadeh AH, Ranjbar M, Ansari S, MirArab A, Alavian SM, Mohammad K, et al. Seroprevalence of hepatitis B in Nahavand, Islamic Republic of Iran. East Mediterr Health J. 2006;12:528–37. [PubMed] [Google Scholar]
- 12.Khedmat H, Alavian SM, Miri SM, Amini M, Abolghasemi H, Hajibeigi B, et al. Trends in seroprevalence of hepatitis B, hepatitis C, HIV, and syphilis infections in Iranian blood donors from 2003 to 2005. Hepat Mon. 2009;9:24–8. [Google Scholar]
- 13.Nokhodian Z, Kassaian N, Ataei B, Javadi AA, Shoaei P, Farajzadegan Z, et al. Hepatitis B markers in Isfahan, Central Iran: A Population-Based Study. Hepat Mon. 2009;9:12–6. [Google Scholar]
- 14.Vahid T, Alavian SM, Kabir A, Kafaee J, Yektaparast B. Hepatitis B prevalence and risk factors in blood donors in Ghazvin, IR, Iran. Hepat Mon. 2005;5:117–22. [Google Scholar]
- 15.Adibi P, Ghassemian R, Alavian SM, Ranjbar M, Mohammadalizadeh AH, Nematizadeh F, et al. Effectiveness of hepatitis B vaccination in children of chronic hepatitis B mothers. Saudi Med J. 2004;25:1414–8. [PubMed] [Google Scholar]
- 16.Kabir A, Alavian SM, Ahanchi N, Malekzadeh R. Combined passive and active immunoprophylaxis for preventing perinatal transmission of the hepatitis B virus in infants born to HBsAg positive mothers in comparison with vaccine alone. Hepatol Res. 2006;36:265–71. doi: 10.1016/j.hepres.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Alavian SM, Hajariazdeh B, Ahmadzad Asl M, Kabir A, Bagheri Lankarani K. Hepatitis B virus infection in Iran: A systematic review. Hepat Mon. 2008;8:281–94. [Google Scholar]
- 18.Mir-Nasseri MM, Mohammadkhani A, Tavakkoli H, Ansari E, Poustchi H. Incarceration is a major risk factor for blood-borne infection among intravenous drug users: Incarceration and blood borne infection among intravenous drug users. Hepat Mon. 2011;11:19–22. [PMC free article] [PubMed] [Google Scholar]
- 19.Sali SH, Bashtar R, Alavian SM. Risk factors in chronic hepatitis B infection: A case-control study. Hepat Mon. 2005;5:109–15. [Google Scholar]
- 20.Alter MJ, Mast EE. The epidemiology of viral hepatitis in the United States. Gastroenterol Clin North Am. 1994;23:437–55. [PubMed] [Google Scholar]
- 21.Ioannou GN. Hepatitis B virus in the United States: Infection, exposure, and immunity rates in a nationally representative survey. Ann Intern Med. 2011;154:319–28. doi: 10.7326/0003-4819-154-5-201103010-00006. [DOI] [PubMed] [Google Scholar]


