Abstract
Nipple discharge (ND) can be the earliest presenting symptom of breast cancer. We hereby present two cases of breast cancer with no palpable mass manifesting as isolated ND, which was whitish in color. In both cases, cytology of the discharge revealed highly pleomorphic cells indicating a high grade malignancy. Mammography showed diffuse, extensive microcalcifications. Simple mastectomy with axillary clearance was done. Histology in both cases revealed diffusely spreading intraductal carcinoma, with focus of microinvasion in one case. ND if scanty or not blood stained is often ignored by the patients and at times, the clinicians. This article highlights that ND can be an early warning sign of intraductal carcinomas that are non-invasive in early stage. Irrespective of the color or nature of the discharge, unilateral ND needs to be evaluated. Proper clinical assessment, cytological evaluation of the ND, and mammography ought to be performed in all such cases. Considering the low level of awareness in women regarding the warning signs of breast cancer, the current focus is to create “breast awareness.” Women should be sensitized to recognize any unusual changes in their breasts and report to their health care providers at the earliest.
Keywords: Breast awareness, breast cancer, cytology, nipple discharge (ND), mammography
INTRODUCTION
Nipple discharge (ND) is common, accounting for 5% of all breast related symptoms.[1] ND may be physiological or pathological (abnormal). Physiological discharge is usually bilateral, emanating from many ducts. The common causes include pregnancy, lactation, hypothyroidism, pituitary adenoma, oral contraceptives, antihypertensives, and tranquilizers. Abnormal ND is often nonlactational (i.e., the patient is not pregnant or is more than 2 years from the last breast feeding), persistent, and unilateral, usually involving a single duct. Abnormal ND is most commonly caused by benign conditions like intraductal papillomas, duct ectasia, papillomatosis, mastitis, fibrocystic changes.[2] The reported incidence of breast carcinoma in pathological ND is between 7 to 15%.[3,4] A majority of patients with breast cancer who manifest with isolated ND have an early stage disease associated with in situ ductal carcinoma (DCIS).[5] Clinical examination, cytological evaluation of the ND, and mammography are first-line diagnostic approaches in patients presenting with abnormal ND.[2]
CASE REPORTS
Case A
A 39-year-old woman presented with history of scanty, whitish discharge from right nipple of 6 months duration. The discharge was barely visible and she had noticed it as her under garment would often stick to the right nipple. She came to seek medical attention only after she developed itching in the right nipple and areolar region.
Case B
A 42-year-old woman presented with spontaneous whitish discharge from the right nipple of almost 1 year duration. For the past 1 week, she had developed pain and noticed some excoriations over the nipple areolar region, which motivated her to come to our hospital.
In both these women, there was no history of mass or pain in the breast. We tried to explore the reason for their delay in seeking medical attention. They replied that as there was no pain or swelling in the breast, it was unlikely to be cancer. Both of them knew about breast cancer, but had no knowledge about other warning signs of breast cancer apart from swelling and pain.
Clinical evaluation in both cases did not reveal any mass in the underlying breast, axillary, or supraclavicular regions. In both cases, the discharge was thick and whitish in color. In case A, it was so scanty that gentle massage had to be done to extract material for making smears. Cytological evaluation of ND smears in both cases showed highly pleomorphic cells with hyperchromatic nuclei, prominent nucleoli, coarse chromatin pattern, and increased nuclear cytoplasmic ratio [Figure 1]. These features were suggestive of a high grade malignancy. Mammography in both cases was positive showing extensive microcalcifications [Figure 2].
Figure 1.
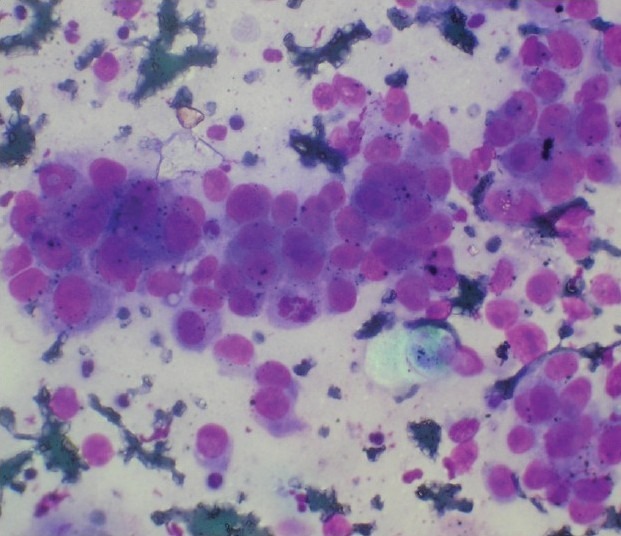
Cytological smear of ND showing discohesive, pleomorphic cells, and a mitotic figure. MGG stain. 45×
Figure 2.

Mammogram showing extensive microcalcifications
In view of the high nuclear grade and extensive microcalcifications, simple mastectomy [Figure 3] with axillary clearance was done. Histological evaluation in Case A revealed DCIS – grade 4 [Figure 4] with foci of microinvasion. Case B showed diffusedly spreading intraductal carcinoma with no evidence of microinvasion. Axillary tail contained 10 lymph nodes in Case A and 6 in Case B, largest measuring 1×0.5 cm all of which were reactive and did not show any metastasis. The surgical margins were free of tumor. Post-operative follow-up was uneventful [Figure 5]. Patients were advised chemotherapy and followed up for 1 year and both are doing well.
Figure 3.
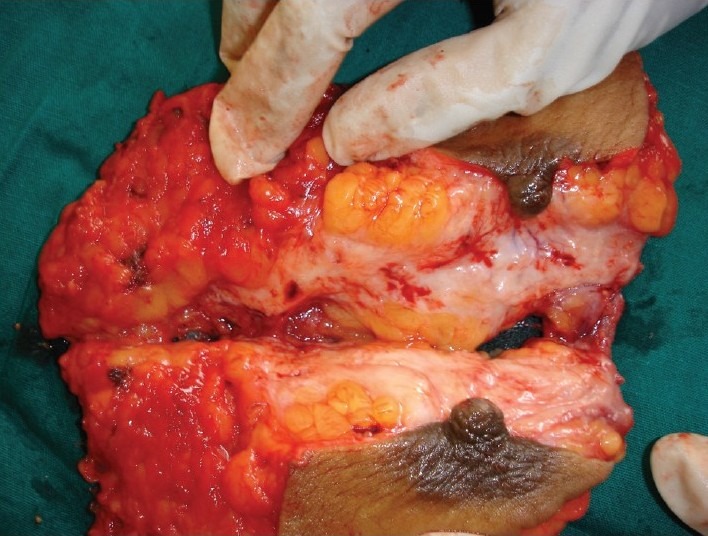
Simple mastectomy specimen
Figure 4.
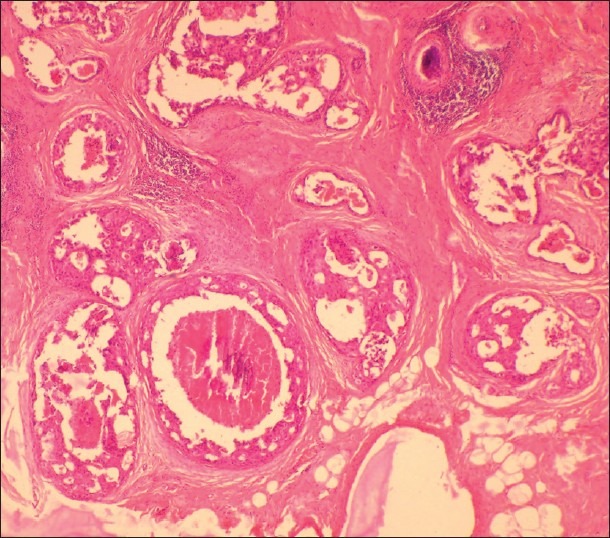
Histological section showing dilated ducts with ductal carcinoma in-situ. HandE stain 4×
Figure 5.

Post-mastectomy status in case-A
DISCUSSION
The incidence of malignancy in patients presenting with abnormal ND is 7% to 15%[3,4]. The possibility of cancer increases when the discharge is accompanied by a lump, and when the patient is over 50 years of age.[6] The proportion of breast carcinoma cases associated with ND ranges from 1.6% to 13%.[5] Most cancer-associated discharges are the result of DCIS or papillary carcinoma and are frequently associated with a clinically palpable lesion or positive findings on mammography.[7,8] ND owing to DCIS has been shown to be a marker for extensive disease, which often requires mastectomy to achieve adequate surgical margins.[9,10]
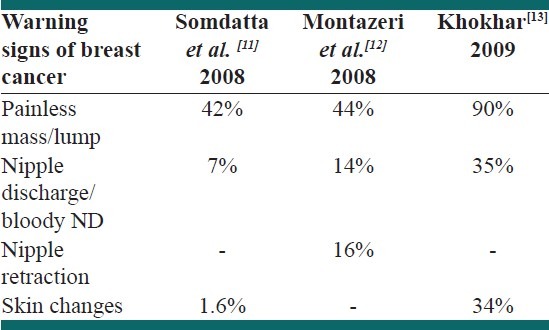
The awareness among women concerning the various warning signs of breast cancer as reported in various studies is shown in Table 1. Montazeri et al[12] and Somdutta et al[11] have reported a low level of awareness regarding the various warning signs. Khokhar[13] in a study conducted among Indian school teachers has reported higher level of awareness. However, it may be noted that in all these studies, awareness regarding ND was much lower (7–35%) compared to that of painless mass/lump (42–90%). This shows that majority of women do not consider isolated ND as an early warning sign of breast cancer, or a condition requiring medical intervention. In our study, both cases approached us for relief of symptoms like itching, pain, and excoriations. They did not regard isolated ND as a symptom requiring medical attention.
Table 1.
Awareness among Women about Warning Signs of Breast Cancer, as reported in Different Population Studies
Many authors have regarded white, yellow, green, brown/black ND as physiological and benign.[1,14] Some studies have considered blood stained, serosanguinous (pink), serous or clear ND as signifying an increased risk of malignancy.[15] However, in our study, both patients with DCIS presented with whitish discharge, which was not blood stained. Therefore, regardless of the gross appearance, unilateral ND needs to be evaluated for the possibility of cancer. Investigation of the ND includes Triple Assessment: Clinical examination, Cytological evaluation, and Mammography.[14]
Mammography is recommended to any patient presenting with abnormal ND. However, some studies have reported that mammography has a poor positive predictive value (16.7%).[2] It is also reported to have a low sensitivity (59%) in the diagnosis of malignant duct pathology.[16] However, most experts recommend that a mammogram should be performed in women over 30 years presenting with nonlactational, spontaneous ND.[17]
Ultrasonography, particularly with high-frequency probes (11–13 mHz) is complementary to mammography and could be useful in many patients.[2] Ductography involves retrograde injection of water soluble radio opaque contrast material into a discharging duct with subsequent mammographic imaging.[5] Li Gui-hua et al.[18] have reported that selective mammary ductography is of great value in patients with DCIS presenting with ND and could detect 90.3% of cases, while mammogram showed positive signs in 25.8%. Mammary ductoscopy is a new technique that allows direct visualization of the mammary ductal epithelium using sub-millimeter fiberoptic microendoscopes.[19] Ductoscopy also allows for ductal lavage, microbiopsies, and excision of intraductal lesions.[19,20] However, these evolving techniques are expensive and lack accessibility.[14]
Surgery has traditionally been considered the gold standard for confirming the diagnosis and treating abnormal ND.[1] Excision of the pathological duct(s) needs to be performed if ND is persistent. The two most common surgical procedures performed in patients with pathological ND are microdochectomy and Hadfield's procedure.[14] Microdochectomy involves identification and removal of the affected duct leaving intact the surrounding tissues and the unaffected ducts.[2] Hadfield's procedure involves radical subareolar duct excision.
BSE and breast awareness
Breast self-examination (BSE) is a systematic method of regular self-inspection and palpation of the breast and axilla.[21] Two large population-based randomized controlled trials in Russia (388,535 women) and Shanghai (260,000 women) followed up over a 5-year period could not demonstrate any beneficial effect of screening by BSE in terms of the size of primary tumor, incidence of lymph node involvement at detection, or cancer-related mortality.[22,23] Several studies have shown that awareness regarding BSE is low and very few women practice it regularly.[11–13]
At present, the emphasis is to raise breast cancer awareness among women and furthermore raise their knowledge about the warning signs of breast cancer.[12] Breast cancer awareness programs have been very successful on several grounds including creation of greater compliance with breast cancer prevention and screening strategies.[24] Being “breast aware” is currently defined as a woman becoming familiar with her own breasts and the way they change throughout her life.[25] This enhances her sensitivity and alerts her to any abnormal change in the breast, at the earliest. The important warning signs to be looked for are as follows.
Lump, thickening, continuous pain in one part of the breast.
Change in size or lowering of one breast.
Discharge from nipples, rashes over nipple, changes in shape or position of nipple, nipple inversion, any skin changes like puckering or dimpling.
Swelling or pain under the armpit or around the collar bone (lymph nodes)
Although the effectiveness of regular BSE remains controversial, it can be used as a strategy to create breast health awareness among women. Teaching BSE can help women to get acquainted with their breasts and alerts them to any abnormal changes at the earliest. Trained female health workers were successful in creating this awareness among rural women.[26] It is important to create awareness and educate the community through community-based educational programs Indeed the focus of primary health care providers should be to raise awareness about breast care and to encourage them to report “any unusual changes in their breasts” to their health care providers.[12]
CONCLUSION
ND can be an early sign of breast cancer. Diffusely spreading intraductal carcinomas which often have no clinically palpable breast mass can manifest as pathological ND. Isolated ND, particularly if not blood stained, is often ignored by the patient. Awareness among women regarding the warning signs of breast cancer and BSE is low. Currently, the emphasis is to raise breast cancer awareness and to enhance their knowledge concerning the warning signs of breast cancer. Women should be alerted to seek medical attention if they notice any unusual changes in their breasts.
Footnotes
Source of Support: ESI PGIMSR, Rajajinagar, Bangalore (Institute to which we are affiliated, as indicated in article)
Conflict of Interest: Nil
REFERENCES
- 1.Lang JE, Kuerer HM. Breast ductal secretions: clinical features, potential uses, and possible applications. Cancer control. 2007;14:350–9. doi: 10.1177/107327480701400405. [DOI] [PubMed] [Google Scholar]
- 2.Zervoudis S, Iatrakis G, Economides P, Polyzos D, Navrozoglou I. Nipple discharge screening. Womens Health. 2010;6:135–51. doi: 10.2217/whe.09.81. [DOI] [PubMed] [Google Scholar]
- 3.Louie LD, Crowe JP, Dawson AE, Lee KB, Baynes DL, Dowdy T, et al. Identification of breast cancer in patients with pathologic nipple discharge: Does ductoscopy predict malignancy? Am J Surg. 2006;192:530–3. doi: 10.1016/j.amjsurg.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Van Zee KJ, Ortega Perez G, Minnard E, Cohen MA. Preoperative galactography increases the diagnostic yield of major duct excision for nipple discharge. Cancer. 1998;82:1874–80. doi: 10.1002/(sici)1097-0142(19980515)82:10<1874::aid-cncr9>3.3.co;2-o. [DOI] [PubMed] [Google Scholar]
- 5.Cabioglu N, Krishnamurthy S, Kuerer HM, Hunt KK, Singletary SE, Meric-Bernstam F, et al. Feasibility of breast-conserving surgery for patients with breast carcinoma associated with nipple discharge. Cancer. 2004;101:508–17. doi: 10.1002/cncr.20394. [DOI] [PubMed] [Google Scholar]
- 6.Leis HP., Jr Management of nipple discharge. World J Surg. 1989;13:736–42. [PubMed] [Google Scholar]
- 7.Carter D, Orr SL, Merino MJ. Intracystic papillary carcinoma of the breast: After mastectomy, radiotherapy or excisional biopsy alone. Cancer. 1983;52:14–9. doi: 10.1002/1097-0142(19830701)52:1<14::aid-cncr2820520104>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 8.Haagensen CD. Diseases of the Breast. 3 ed. Philadelphia: WB Saunders; 1986. pp. 729–57. [Google Scholar]
- 9.Bauer RL, Eckhert KH, Nemoto T. DCIS associated nipple discharge: A clinical marker for locally extensive disease. Ann Surg Oncol. 1998;5:452–5. doi: 10.1007/BF02303865. [DOI] [PubMed] [Google Scholar]
- 10.Obedian E, Haffty BG. Breast-conserving therapy in breast cancer patients presenting with nipple discharge. Int J Radiat Oncol Biol Phys. 2000;47:137–42. doi: 10.1016/s0360-3016(99)00527-1. [DOI] [PubMed] [Google Scholar]
- 11.Somdatta P, Baridalyne N. Awareness of breast cancer in women of an urban settlement colony. Indian J Cancer. 2008;45:149–53. doi: 10.4103/0019-509x.44662. [DOI] [PubMed] [Google Scholar]
- 12.Montazeri A, Vahdaninia M, Harirchi I, Harirchi AM, Sajadian A, Khaleghi F, et al. Breast cancer in Iran: Need for greater women awareness of warning signs and effective screening methods. Asia Pac Fam Med. 2008;7:6. doi: 10.1186/1447-056X-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khokhar A. Level of Awareness Regarding Breast Cancer and its Screening amongst Indian Teachers. Asian Pac J Cancer Prev. 2009;10:247–9. [PubMed] [Google Scholar]
- 14.Richards T, Hunt A, Courtney S, Umeh H. Nipple discharge: a sign of breast cancer? Ann R Coll Surg Engl. 2007;89:124–6. doi: 10.1308/003588407X155491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salmon RJ, Merle S, Boue P. Demonstration of blood in nipple discharge using the Hemoccult. J Gynecol Obstet Biol Reprod (Paris) 1987;16:595–8. [PubMed] [Google Scholar]
- 16.Ito Y, Tamaki Y, Nakano Y, Kobayashi T, Takeda T, Wakasugi E, et al. Non-palpable breast cancer with nipple discharge: how should it be treated? Anticancer Res. 1997;17:791–4. [PubMed] [Google Scholar]
- 17.Gray RJ, Pockaj BA, Karstaedt PJ. Navigating murky waters: a modern treatment algorithm for nipple discharge. Am J Surg. 2007;194:850–5. doi: 10.1016/j.amjsurg.2007.08.027. [DOI] [PubMed] [Google Scholar]
- 18.Li G, Wang X, Cao G, Yang R, Yang J. Value of selective mammary ductography in the diagnosis of ductal carcinoma in situ. Beijing Da Xue Xue Bao. 2008;40:143–5. [PubMed] [Google Scholar]
- 19.Al Sarakbi W, Salhab M, Mokbel K. Does mammary ductoscopy have a role in clinical practice? Int Semin Surg Oncol. 2006;3:16. doi: 10.1186/1477-7800-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kapenhas-Valdes E, Feldman SM, Cohen JM, Boolbol SK. Mammary ductoscopy for evaluation of nipple discharge. Ann Surg Oncol. 2008;15:2720–7. doi: 10.1245/s10434-008-0012-1. [DOI] [PubMed] [Google Scholar]
- 21.Baxter N. Canadian Task Force on Preventive Health Care. Preventive health care, 2001 update: Should women be routinely taught breast self-examination to screen for breast cancer? CMAJ. 2001;164:1837–45. [PMC free article] [PubMed] [Google Scholar]
- 22.Thomas DB, Gao DL, Self SG, Allison CJ, Tao Y, Mahloch J, et al. Randomized trial of breast self-examination in Shanghai: Methodology and preliminary results. J Natl Cancer Inst. 1997;89:355–65. doi: 10.1093/jnci/89.5.355. [DOI] [PubMed] [Google Scholar]
- 23.Semiglazov VF, Moiseenko VM. Breast self-examination for the early detection of breast cancer: a USSR/WHO controlled trial in Leningrad. Bull World Health Organ. 1987;65:391–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Anonymous: Breast cancer awareness: too much of a good thing? Lancet Oncol. 2007;8:1041. doi: 10.1016/S1470-2045(07)70347-9. [DOI] [PubMed] [Google Scholar]
- 25.Linsell L, Burgess CC, Ramirez AJ. Breast cancer awareness among older women. Br J Cancer. 2008;99:1221–5. doi: 10.1038/sj.bjc.6604668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rao RS, Nair S, Nair NS, Kamath VG. Acceptability and effectiveness of a breast health awareness programme for rural women in India. Indian J Med Sci. 2005;59:398–402. [PubMed] [Google Scholar]


