Abstract
Objectives
Overcapacity issues plague emergency departments (EDs). Studies suggest triage liaison providers (TLPs) may shorten patient length of stay (LOS) and reduce the proportion of patients who leave without being seen (LWBS), but these results are not universal. Previous studies used physicians as TLPs. We evaluated whether a physician assistant (PA), acting as a TLP, would shorten LOS and decrease LWBS rates.
Methods
The authors used an observational cohort controlled before-and-after study design with predefined outcome measures, comparing eight pilot days to eight control days. The TLP evaluated all Emergency Severity Index (ESI) level 3, 4, and 5 patients, excluding pediatric and behavioral health patients.
Results
Three hundred fifty-three patients were included on pilot days, and 371 on control days. LOS was shorter on pilot days than control days (median 229 minutes [IQR 168 to 303 minutes] vs. 270 minutes [IQR 187 to 372 minutes], p < 0.001). Waiting room times were similar between pilot and control days (median 69 minutes [IQR 20 to 119 minutes] vs. 70 minutes [IQR 19 to 137 minutes], p = 0.408), but treatment room times were shorter (median 151 minutes [IQR 92 to 223 minutes] vs. 187 minutes [IQR 110 to 254 minutes], p < 0.001). Finally, a lower proportion of patients LWBS on pilot days (1.4% vs. 9.7%, p < 0.001).
Conclusions
The addition of a PA as a TLP was associated with a 41 minute decrease in median total LOS, and a lower proportion of patients who LWBS. The decrease in total LOS is likely attributable to the addition of the TLP, with patients having shorter duration in treatment rooms on pilot days compared to control days.
INTRODUCTION
Emergency department (ED) crowding is a growing national problem, fueled by increases in total numbers of ED visits occurring during a period of retraction in total number of hospital EDs.1 Crowding has been correlated with long patient wait times, decreased patient safety, and delays in care and treatment.2–4
To address crowding, some EDs have explored the use of a triage liaison provider (TLP).1 A TLP is a triage-based physician or advanced-level provider who begins patient assessment before a formal ED treatment room is available. Some studies have suggested that TLPs may reduce patient length of stay (LOS),5–11 whereas others have failed to replicate this finding.12–15 The effect of TLPs on patients who leave without being seen (LWBS) has also varied.16 These heterogeneous findings may be attributed to TLP model type, patient volume, patient complexity, and provider type.
To address our own overcapacity issues, we investigated whether a TLP would be effective in our practice setting. Although most studies have examined the use of physicians as TLPs,16 we chose to evaluate the use of a physician assistant (PA) in this role. We hypothesized that a PA, acting as a TLP, would decrease LOS and the proportion of patients who LWBS.
METHODS
Study Design
We used an observational cohort controlled before-and-after study design with predefined outcome measures. The study was approved by the Mayo Clinic Institutional Review Board (IRB), and consent was waived by the IRB.
Study Setting and Population
Our ED is located in Saint Mary’s Hospital, an academic tertiary care hospital and Level I trauma center, part of the Mayo Clinic in Olmsted County, MN (population 141,360). The ED at Saint Mary’s Hospital has approximately 72,000 patient visits per year, and a hospital admission rate of 30%.
All adult Emergency Severity Index (ESI) level 3, 4, and 5 patients who registered during the pilot hours were considered for this study. We excluded pediatric patients since dedicated providers see our pediatric population in a separate portion of the ED during pilot hours. We also excluded ESI level 1 and 2 patients, as these patients typically bypass the triage assessment area and are taken immediately to a resuscitation area where dedicated providers evaluate the patients and initiate treatment and diagnostics within minutes. We also excluded any behavioral health patients, because they are evaluated in our behavioral health care area, and do not undergo formal triage assessment in the main triage area.
All remaining adult ESI level 3, 4, and 5 patients were included in the study, regardless of whether they arrived by ambulance or private vehicle. These patients initially register at the entrance and are called to a triage assessment room where a triage nurse collects and records vital signs and a brief history. If there are no treatment rooms available in the non-resuscitation area, the patient is directed back to the waiting room and called when a room becomes available.
Study Protocol
For this intervention, we tested the TLP pilot during predictably busy days and times. Because adding a TLP to existing staffing required incremental personnel resources (rather than a reallocation of personnel to a different location in the ED), we selected pilot days when an additional provider was available. We chose the hours of 12:00 PM to 8:00 PM on Mondays and Wednesdays for the pilot times, because ED treatment rooms are predictably full and patients often wait to be seen during these hours. We had sufficient funding to add incremental staffing for eight days. Two different PAs functioned as the TLP, each with at least four years of experience working in our ED. The pilot dates were May 2, 4, 9, 11, 16, 18, 25, and June 1, 2011. To decrease the risk of observational bias, we chose control dates immediately before the pilot dates by overlaying a calendar and selecting the same days of the week in the immediately preceding month. The control dates were April 4, 6, 11, 13, 18, 20, 28, and 30, 2011. The ED registration time of the first and last patient who had a test ordered by the TLP marked the start and end of the pilot for each given pilot day. For control days, we collected data on all patients with ED registration times corresponding to the matching pilot times.
For the pilot days, the TLP was instructed to be present for at least a portion of the triage assessment. The TLP would listen to the assessment, ask a limited number of questions as appropriate, and/or perform a very brief physical exam. Patients were clothed as they normally would be for their triage assessment. The TLP would order any blood tests or radiographic studies they felt appropriate for initial testing using the electronic ordering system used throughout the ED (ED PulseCheck, Picis Inc., Wakefield, MA). Of note, no electrocardiograms or urine tests were ordered in triage, as there was no means to undress the patient or collect urine in an appropriate manner. The TLP did not have any other clinical duties during this shift. He or she would try to evaluate every ESI level 3, 4, or 5 adult patient who presented to the ED, whether by ambulance or private vehicle. The triage nurses controlled the flow of patient assessments and, in collaboration with the TLP, facilitated rapid patient assessments. The TLP interacted with a clinical assistant working in triage to coordinate performance of tests (e.g., sending the patient for x-rays after blood was collected).
When the triage nurse completed the assessment, the patient was directed to an available treatment room or back to the waiting room. A phlebotomist assigned to the waiting room continuously monitored the electronic medical record (EMR) for waiting room patients with pending blood test orders and complete those orders. Additionally, the clinical assistant would monitor the EMR for outstanding radiology orders and would call the radiology department to facilitate patient transport for any pending studies. As a general rule, the TLP would not check on any collected tests, leaving this task for the downstream providers covering the ED treatment room where the patient would eventually be taken. If the laboratory or radiologist noted critical results, however, the TLP would be contacted, leading to a discussion with triage nurses about potentially upgrading the patient’s triage level. Also, the TLP generally did not try to dismiss any patients, leaving this to the providers working in regular ED treatment areas, since the time necessary to complete the necessary documentation and provide prescriptions, work excuses, and/or follow-up appointments would limit the time available for evaluation of other rapidly triaged patients, and potentially decrease the number of patients the TLP could evaluate in a shift.
Measurements
All data were extracted from the EMR and electronic ED tracking system. Adult ESI level 3, 4, or 5 patients who LWBS were included in the general study demographics, but were excluded from LOS analysis, since measures of their LOS could not be reliably estimated.
We collected patient demographic information, ESI triage level, registration time, room time, and the time the patient left the treatment room. This was done on all eligible patients regardless of final disposition (discharged to home or admitted to the hospital). Data were collected for all patients who met eligibility criteria during the pilot and control periods.
Data Analysis
We present all continuous data as either means with standard deviation (± SD) or medians with interquartile range (IQR) as appropriate for the distribution of the data. Categorical data are presented as frequency counts and percentages. Statistical comparisons between pilot and control phases were conducted using the following tests: the chi-square test was used to compare differences in the proportions of sex, day of week (Monday versus Wednesday), ESI triage levels, and LWBS; and the Mann-Whitney U-test was used to compare differences in age, number of patients presenting to the ED, and LOS. The effect of pilot versus control days on total LOS after adjusting for age, day of the week, the number of patients presenting to the ED, ESI triage level, and individual TLP was evaluated using multiple linear regression. For the multivariable model, LOS was transformed using the square root to meet the normality assumption. Residuals and influential statistics indicated that the linearity and equal variance assumptions were satisfied. Comparisons between pilot and control phases occurred for all ESI level 3, 4, and 5 patients. As Level 3 patients are often more complex and require extensive laboratory and radiologic imaging when compared to ESI Level 4 and 5 patients, we conducted an a-priori analysis of the effect of the TLP on these two subgroups: ESI 3 patients vs. ESI 4 and 5 patients. All tests were two-sided, and p-values less than 0.05 were considered statistically significant. With the sample size and the observed LOS and LWBS rates, the study had > 98% statistical power to detect differences in LOS and LWBS between the two groups using a significance level of 0.05. Analyses were performed using SAS (SAS Institute Inc., Cary, NC).
RESULTS
Baseline Demographics
A total of 724 adult ESI level 3, 4, and 5 patient encounters met eligibility criteria during the study periods and provided authorization for their medical records to be used for research purposes according to the Health Insurance Portability and Accountability Act (Table 1). Of these, 371 (51%) were on control days, and 353 (49%) on pilot days. For LOS calculations, the 41 patients who LWBS (36 on control days, 5 on pilot days) were excluded, leaving 335 patients on control days, and 348 patients on pilot days for analysis.
Table 1.
Demographics of Study Patients
| Demographic | Control Days (n=371) | Pilot Days (n=353) | p-value |
|---|---|---|---|
| Age, years (mean, ±SD) | 51.2 (±21.3) | 53.9 (±21.0) | 0.069 |
| Female (%) | 223 (60) | 205 (58) | 0.578 |
| Day of week (Monday, %) | 204 (55) | 131 (37) | <0.001 |
| Census per daily study times (mean, ±SD) | 51.0 (±8.6) | 48.6 (±6.0) | <0.001 |
| Patients by ESI level (%) | 0.007 | ||
| ESI Level 3 | 267 (72) | 289 (82) | |
| ESI Level 4 | 94 (25) | 58 (16) | |
| ESI Level 5 | 10 (3) | 6 (2) | |
| Left without being seen | 36 (9.7) | 5 (1.4) | <0.001 |
SD = standard deviation; ESI = Emergency Severity Index.
N = 724
Table 1 summarizes the demographics of the included study patients. There were no statistically significant differences in age or sex between pilot and control periods. In the control period, a greater percentage of patients presented on Monday than in the pilot period (p < 0.001). Fewer patients presented to the ED during pilot dates and times, as compared to control (mean 48.6 [SD ±6.0] patients vs. 51.0 [SD ±8.6], p < 0.001), and higher acuity ESI triage levels were observed on pilot days (p = 0.007). There was a lower proportion of patients who LWBS on pilot days compared to control days (1.4% vs. 9.7%, p < 0.001).
Primary Outcome – Total LOS for all ESI Level 3, 4, and 5 patients
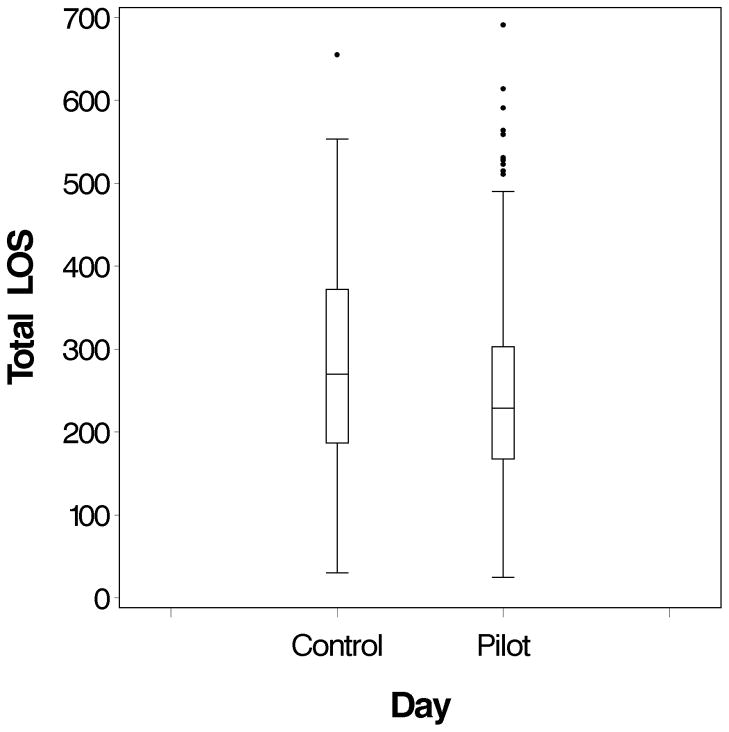
Total LOS was shorter on pilot days compared to control days (median 229 minutes [IQR 168 to 303 minutes] vs. 270 minutes [IQR 187 to 372 minutes], p < 0.001) (Table 2). Figure 1 depicts the distribution of total LOS on pilot and control days. The significant difference in total LOS between pilot vs. control days was still apparent after adjusting for age, day of the week, the number of patients presenting to the ED during testing times, and ESI triage level in a multivariable setting (p < 0.001). Specifically, the effect of the pilot on total LOS did not appear to differ between patients with ESI level 3 and those with ESI level 4 or 5 (p = 0.82 for the interaction term between pilot and triage level).
Table 2.
LOS Data for All Included ESI Level 3, 4, and 5 Patients
| Length of Stay | Control Days | Pilot Days | p-value |
|---|---|---|---|
| Median total | 270 (187–372) | 229 (168–303) | <0.001 |
| Median waiting room | 70 (19–137) | 69 (20–119) | 0.408 |
| Median treatment room | 187 (110–254) | 151 (92–223) | <0.001 |
LOS = length of stay; IQR = interquartile range.
All results reported as minutes (IQR)
Figure 1.
Distribution of the Total LOS on Pilot and Control Days for Included ESI Level 3, 4, and 5 Patients
Within the subset of patients seen during pilot days, there was not a significant difference in total LOS between the two PAs, after adjusting for age, day of the week, the number of patients presenting to the ED, and ESI triage level (p = 0.58). This is also true for the subset of ESI level 3 patients (p = 0.96), and the subset of ESI level 4/5 patients (p = 0.18) after adjusting for age, day of the week, and the number of patients presenting to the ED.
Secondary Outcomes
Waiting Room and Treatment Room LOS for all ESI Level 3, 4, and 5 Patients
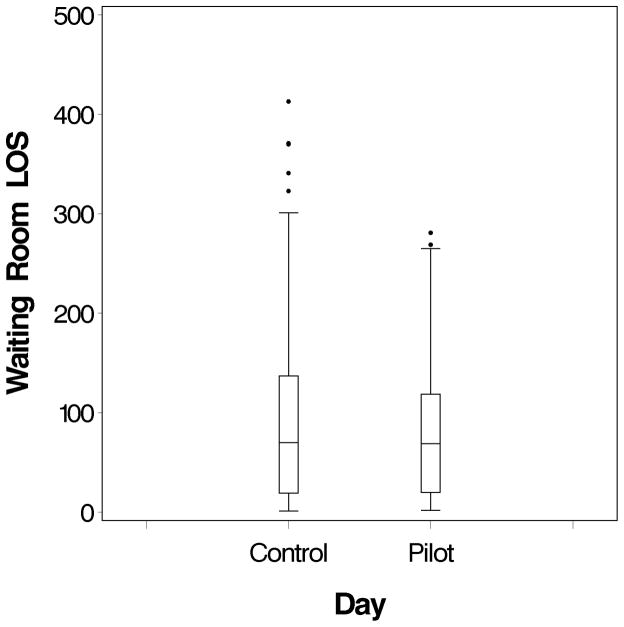
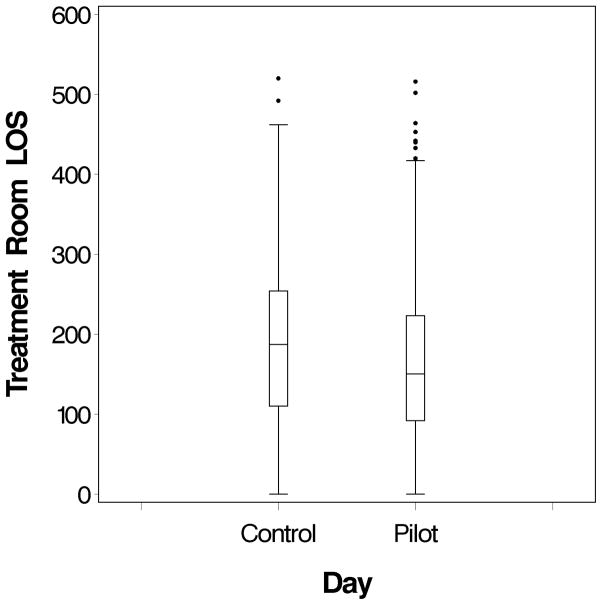
Secondary analyses examined the difference between the two components that comprise total LOS: waiting room LOS and treatment room LOS. There was no significant difference in the waiting room LOS on pilot days compared to control days (median 69 minutes [IQR 20 to 119 minutes] vs. 70 minutes [IQR 19 to 137 minutes], p = 0.408) (Table 2, Figure 2). There was, however, a difference in the treatment room LOS on pilot days compared to control days (median 151 minutes [IQR 92 to 223 minutes] vs. 187 minutes [IQR 110 to 254 minutes], p < 0.001) (Table 2, Figure 3).
Figure 2.
Distribution of the Waiting Room LOS on Pilot and Control Days for Included ESI Level 3, 4, and 5 Patients
Figure 3.
Distribution of the Treatment Room LOS on Pilot and Control Days for Included ESI Level 3, 4, and 5 Patients
Waiting Room and Treatment Room LOS for ESI level 3 patients, and ESI level 4, 5 patients
For ESI level 3 patients, total LOS was shorter on pilot days compared to control days (median 246 minutes [IQR 190 to 321 minutes] vs. 299 minutes [IQR 214 to 397 minutes], p < 0.001) (Table 3a). This difference remained after adjusting for age, day of the week, and the number of patients presenting to the ED during testing times (p < 0.001). The waiting room LOS on pilot days was similar to that of control days (median 70 minutes [IQR 16 to 123 minutes] vs. 76 minutes [IQR 14 to 148 minutes], p = 0.302). The treatment room LOS on pilot days was shorter compared to control days (median 170 minutes [IQR 115 to 241 minutes] vs. 212 minutes [IQR 152 to 273 minutes], p < 0.001).
Table 3a.
LOS Data for Included ESI Level 3 Patients Only
| Length of Stay | Control Days | Pilot Days | p-value |
|---|---|---|---|
| Median total | 299 (214–397) | 246 (190–321) | <0.001 |
| Median waiting room | 76 (14–148) | 70 (16–123) | 0.302 |
| Median treatment room | 212 (152–273) | 170 (115–241) | <0.001 |
LOS = length of stay; IQR = interquartile range.
All results reported as minutes (IQR)
For ESI level 4 and 5 patients, these trends remained. Total LOS was shorter on pilot days compared to control days (median 166 minutes [IQR 123 to 199 minutes] vs. 188 minutes [IQR 122 to 264 minutes], p = 0.041) (Table 3b). This difference remained after adjusting for age, day of the week, and the number of patients presenting to the ED during testing times (p = 0.030). The waiting room LOS on pilot days was similar to control days (median 63 minutes [IQR 31 to 106 minutes] vs. 65 minutes [IQR 32 to 111 minutes], p = 0.763). The treatment room LOS on pilot days was shorter compared to control days (median 81 minutes [IQR 53 to 110] vs. 101 minutes [IQR 72 to 155], p = 0.003).
Table 3b.
LOS Data for Included ESI Level 4 and 5 Patients Only
| Length of Stay | Control Days | Pilot Days | p-value |
|---|---|---|---|
| Median total | 188 (122–264) | 166 (123–199) | 0.041 |
| Median waiting room | 65 (32–111) | 63 (31–106) | 0.763 |
| Median treatment room | 101 (72–155) | 81 (53–110) | 0.003 |
LOS, length of stay; IQR, interquartile range.
All results reported as minutes (IQR)
DISCUSSION
We observed a 41-minute shorter total LOS, and a reduction in LWBS rates from 9.7% to 1.4%, in adult ESI level 3, 4, and 5 patients at times when a PA was added as a TLP. The decrease in total LOS was likely attributable to less time spent in regular treatment rooms for pilot patients compared to control patients. This shortened patient LOS persisted even after controlling for other known contributors to patient LOS, such as patient age, day of the week, patient volumes, and ESI triage level, and the individual working as the TLP. Similar findings were noted in a subanalysis of ESI level 3 patients, along with ESI level 4 and 5 patients, suggesting that all eligible patients benefited from the TLP model. By adding one provider to an already busy ED, we showed that this model could significantly affect two major areas of operational concern to EDs: patient LOS, and LWBS rates. This effect remained after controlling for other confounders.
As ED crowding is a widespread and growing concern, EDs must find solutions to address patient throughput problems. A recent paper by Wiler and colleagues1 highlights the need to improve patient management on the “front end” of ED care, where “front end” is defined as the time from patient presentation to the ED until placement in a formal treatment room. These authors note that the design, implementation, and assessment of innovative throughput solutions are essential components of departmental quality and operational performance improvement efforts.
The effects of TLPs have been mixed. Some studies have shown reduction in patient LOS,5–11 while others have not.12–15 Similar disparity exists with LWBS rates.16 Because the concept of TLP is relatively new, the methodologies of the published trials of TLPs differ. Of the studies that failed to show a significant reduction in patient LOS, key design or measurement differences exist. The study by Russ et al.13 used patients evaluated at the same time as the TLP model for controls, selecting patients who had orders placed by the TLP as the study patients, and patients who did not have orders placed by the TLP as control patients. The lack of effect demonstrated in their study could be confounded by the fact that all patients who are evaluated during times when a TLP is working may benefit from downstream efficiency improvements, leading to decreased LOS for patients who do not receive orders from the TLP. The other three studies12,14,15 each reallocated a physician to triage to serve as TLP, rather than adding the provider to the schedule like our model. One may conclude that reallocation of providers to serve as TLP may not reduce overall patient LOS, and adding the additional provider is necessary. However, it should be noted that Choi and colleagues8 demonstrated a significant decrease in LOS by reallocating a provider, though two other studies that reallocated providers12,14 did not. On the whole, three out of four studies that reallocated providers to serve as TLP did not observe a significant decrease in patient LOS.
Of published TLP studies that have demonstrated significant reductions in patient LOS, key differences exist as well. Several of the TLP models have been studied in other countries,7,8,10 and it is likely that differences exist in ED patient populations and operations on an international level. The study by Levsky and colleagues6 added a team of providers to the triage area, rather than a single TLP, and although this was beneficial to patient LOS, it may be particularly costly to departments considering this approach. The study by Chan and colleagues9 added several enhancements to a triage redesign, making it difficult to understand the isolated effect of simply adding a TLP. Of all published TLP studies that showed significant decreases in patient LOS, only the study by Partovi and colleagues11 showed a greater LOS reduction than the 41-minute reduction seen in our study. However, their baseline LOS was much longer, reducing LOS from 445 minutes to 363 minutes. This resulted in an 18.4% reduction in LOS, similar to our 15.2% reduction.
Finally, our study differs significantly in that this TLP model is, to the best of our knowledge, the first to solely evaluate PAs as TLPs. A recent review of TLPs noted that physicians are usually placed in this role.16 Our ED already employs PAs who work in conjunction with attending physicians when providing care for higher acuity patients. They also care for patients with a high level of autonomy in a dedicated “fast track” setting. The use of PAs in EDs has grown over time,17 and we hypothesized that they would be able to improve overall patient throughput in this emerging TLP role.
Because treatment rooms are often not immediately available for urgent but non-emergent patients, we explored ways to use patients’ waiting time more effectively. For decades psychologists have noted the frustrations of waiting for a service and have proposed theories for improving this frustration.18 Several of these psychological theories are applicable to the ED setting, including “occupied time feels shorter than unoccupied time,” and “people want to get started.” In our traditional model of care, patients who present to the ED during busy times are assessed by a nurse and then sent to the waiting room to pass the time until an ED treatment room becomes available. Care is subsequently initiated when they are placed in treatment rooms. In the TLP model we used waiting room time as “active time” where blood work and radiographic studies were performed. Although we did not design the study to measure patient satisfaction, we did demonstrate a substantial decrease in LWBS rates, and speculate that, in addition to the shortened LOS, this difference may be due to “occupying the patient’s time” and “getting started.”
Initiating diagnostics can also have a substantial effect on patient safety. The opportunity to more rapidly identify abnormalities such as a markedly elevated international normalized ratio, elevated potassium, depleted white blood cell count, or other urgent finding can theoretically decrease the probability that patients will decompensate during their ED stay. Laboratory and imaging abnormalities can also guide next steps of management when a patient is evaluated in a regular treatment room.
We understand that concerns exist regarding over- or under-testing in the TLP model. We recognize that the TLP was not able to evaluate every patient. However, we are unable to retrospectively measure how many, if any, patients were not evaluated by the TLP during the pilot times. Also, we are unable to evaluate testing rates for the patients who were evaluated. Over-testing can lead to unnecessary patient cost, while under-testing during the TLP evaluation can reduce any potential benefits on LOS due to the requirement for additional later testing. Of note, we did survey our ED providers and nurses after the completion of this pilot study. When asked whether “tests that were ordered in triage during the TLP pilot were appropriate,” 100% of respondents either “somewhat agreed” or “strongly agreed.” A prospective evaluation of TLP testing rates would be a valuable addition to the literature.
LIMITATIONS
This was a single-center study, and our findings may not readily generalize to other practice settings. As noted by Asplin and Yealy, further ED operations research needs to involve multiple sites with randomized controlled trials before nationwide recommendations can be made.19 Due to limited personnel resources, we were unable to randomize TLP shifts or the days on which a TLP was scheduled to work in triage. This increases the risk that factors other than the presence of the TLP influenced total LOS. It is possible that our results would not be generalizable to any PA working as TLP in the ED, as our study involved two PAs, and our diverse experience with using PAs across acuity levels may not represent those of others.
To the best of our knowledge, no other co-interventions were introduced during the study periods, and the risk that other confounding factors might explain the difference in LOS observed between pilot and control periods is low. Although differences between pilot and control days did exist, including ESI level and patient volume distributions, these were evaluated by subgroup analyses on triage levels and by multivariate analysis, and the significant benefit of TLP on LOS remained.
CONCLUSIONS
We observed a shorter total length of stay and a lower proportion of patients who left without being seen during busy periods when a physician assistant was added as a triage liaison provider. The decrease in total length of stay was likely attributable to shorter duration in treatment rooms for pilot patients compared to control patients, and these length of stay reductions were noted for more complex ESI level 3 patients, and for less complex ESI level 4 and 5 patients. Future multicenter trials are needed to determine whether this intervention can be generalized to other practice settings.
Acknowledgments
Funding Sources: This publication was made possible by the Mayo Clinic CTSA through grant number UL1 RR024150 from the National Center for Research Resources and the National Center for Advancing Translational Sciences, a component of the National Institutes of Health (NIH).
The authors wish to acknowledge and thank Christine Lohse for her assistance with this manuscript.
Footnotes
Prior Presentations: none
Disclosures: The authors have no disclosures or conflicts of interest to report
References
- 1.Wiler JL, Gentle C, Halfpenny JM, et al. Optimizing emergency department front-end operations. Ann Emerg Med. 2010;55:142–60. doi: 10.1016/j.annemergmed.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 2.Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16:1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 3.Pines JM, Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:1–5. doi: 10.1016/j.annemergmed.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 4.Derlet RW, Richards JR. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35:63–8. doi: 10.1016/s0196-0644(00)70105-3. [DOI] [PubMed] [Google Scholar]
- 5.Han JH, France DJ, Levin SR, Jones ID, Storrow AB, Aronsky D. The effect of physician triage on emergency department length of stay. J Emerg Med. 2010;39:227–33. doi: 10.1016/j.jemermed.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Levsky ME, Young SE, Masullo LN, Miller MA, Herold TJS. The effects of an accelerated triage and treatment protocol on left without being seen rates and wait times of urgent patients at a military emergency department. Military Med. 2008;173:999–1003. doi: 10.7205/milmed.173.10.999. [DOI] [PubMed] [Google Scholar]
- 7.Holroyd BR, Bullard MJ, Latoszek K, et al. Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial. Acad Emerg Med. 2007;14:702–8. doi: 10.1197/j.aem.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 8.Choi YF, Wong TW, Lau CC. Triage rapid initial assessment by doctor (TRIAD) improves waiting time and processing time of the emergency department. Emerg Med J. 2006;23:262–5. doi: 10.1136/emj.2005.025254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan TC, Killeen JP, Kelly D, Guss DA. Impact of rapid entry and accelerated care at triage on reducing emergency department patient wait times, lengths of stay, and rate of left without being seen. Ann Emerg Med. 2005;46:491–7. doi: 10.1016/j.annemergmed.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 10.Rogers T, Ross N, Spooner D. Evaluation of a see and treat; pilot study introduced to an emergency department. Accid Emerg Nurs. 2004;12:24–7. doi: 10.1016/j.aaen.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 11.Partovi SN, Nelson BK, Bryan ED, Walsh MJ. Faculty triage shortens emergency department length of stay. Acad Emerg Med. 2001;8:990–5. doi: 10.1111/j.1553-2712.2001.tb01099.x. [DOI] [PubMed] [Google Scholar]
- 12.Li J, Caviness AC, Patel B. Effect of a triage team on length of stay in a pediatric emergency department. Pediatr Emerg Care. 2011;27:687–92. doi: 10.1097/PEC.0b013e318226c7b2. [DOI] [PubMed] [Google Scholar]
- 13.Russ S, Jones I, Aronsky D, Dittus RS, Slovis CM. Placing physician orders at triage: the effect on length of stay. Ann Emerg Med. 2010;56:27–33. doi: 10.1016/j.annemergmed.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Subash F, Dunn F, McNicholl B, Marlow J. Team triage improves emergency department efficiency. Emerg Med J. 2004;21:542–4. doi: 10.1136/emj.2002.003665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grant S, Spain D, Green D. Rapid assessment team reduces waiting time. Emerg Med Australas. 1999;11:72–7. [Google Scholar]
- 16.Rowe BH, Guo X, Villa-Roel C, et al. The role of triage liaison physicians on mitigating overcrowding in emergency departments: a systematic review. Acad Emerg Med. 2011;18:111–20. doi: 10.1111/j.1553-2712.2010.00984.x. [DOI] [PubMed] [Google Scholar]
- 17.Hooker RS, Klocko DJ, Luke Larkin G. Physician assistants in emergency medicine: the impact of their role. Acad Emerg Med. 2010;18:72–7. doi: 10.1111/j.1553-2712.2010.00953.x. [DOI] [PubMed] [Google Scholar]
- 18.Maister DH. The psychology of waiting lines. Service Encounter. 1985;1:13–23. [Google Scholar]
- 19.Asplin BR, Yealy DM. Key requirements for a new era of emergency department operations research. Ann Emerg Med. 2011;57:101–3. doi: 10.1016/j.annemergmed.2010.07.026. [DOI] [PubMed] [Google Scholar]