Abstract
Postnatal depression and anxiety have been shown to increase the risk of disturbances in mother–child interaction and child development. Research into mechanisms has focused on genetics and maternal behavior; maternal cognitions have received little attention. Our aim was to experimentally determine if worry and rumination in mothers with generalized anxiety disorder (GAD) and major depressive disorder (MDD), diagnosed in the postnatal 6 months, interfered with maternal responsiveness to their 10-month old infants. Mothers (N = 253: GAD n = 90; MDD n = 57; control n = 106) and their infants were randomized to either a worry/rumination prime (WRP) or a neutral prime (NP); mother–infant interactions were assessed before and after priming. Type of priming was a significant predictor of maternal cognitions, with WRP resulting in more negative thoughts, higher thought recurrence and more self-focus relative to NP across the entire sample. Interaction effects between group and priming were significant for two parenting variables: Compared with controls, WRP had a more negative impact on maternal responsiveness to infant vocalization for GAD, and to a lesser extent for MDD; WRP led to decreased maternal vocalization for GAD. Also, mothers with GAD used stronger control after the NP than WRP, as well as compared with other groups, and overall post-priming, their children exhibited lower emotional tone and more withdrawal. Across the entire sample, WRP was associated with increased child vocalization relative to NP. This study demonstrated that disturbances in maternal cognitions, in the context of postnatal anxiety and to a lesser degree depression, play a significant role in mother–child interaction.
Keywords: mother–child interaction, worry, rumination, attention, infancy
Postnatal psychiatric disorder has been shown to increase the risk of disturbances in mother–child interaction, which, in turn, have an adverse impact on child emotional development (Merikangas, Dierker, & Szatmari, 1998; Stein, Ramchandani, & Murray, 2008). Much of this research has derived from studies of postnatal depression (Goodman, 2007; Murray, Halligan, & Cooper, 2010) and, to a lesser extent, from studies of anxiety (Murray et al., 2008) and eating disorders (Patel, Wheatcroft, Park, & Stein, 2002; Stein, Woolley, Cooper, & Fairburn, 1994; Stice, Agras, & Hammer, 1999). In postnatal depression at least, the impact on the children can persist well after remission of the parental disorder (Murray et al., 2010).
There is a need to understand the mechanisms by which postnatal anxiety and depression influence child development. Significant progress has been made toward identifying mechanisms at the behavioral (Stein, Lehtonen, Harvey, Nicol-Harper, & Craske, 2009) and genetic (Plomin, DeFries, Craig, & McGuffin, 2003) levels. However, maternal cognitions, which are likely to underlie maternal behaviors in these affective disorders, have received little investigation. For example, recurrent intrusive negative thoughts (i.e., worry and rumination), and the resultant attentional disturbance, are core features of generalized anxiety disorder and depression, but their specific effects upon parenting and child development have not yet been systematically investigated (Stein et al., 2009). Worry, typically studied in the context of generalized anxiety disorder, is defined as a related chain of repetitive and uncontrollable negative thoughts about perceived threats (Craske & Hazlett-Stevens, 2002; Craske, Rapee, Jackel, & Barlow, 1989; Roemer & Borkovec, 1993). Rumination, typically studied in the context of depression, involves focusing on depressive feelings and symptoms, personal inadequacies, and perceived failures (Nolen Hoeksema, 1991). Hence, rumination and worry are presumed to share common core processes, characterized by thoughts that are difficult to control, repetitive and negative in valence (Nicol-Harper, 2005; Stein et al., 2009).
There is a large body of research documenting that these cognitive processes have profound adverse effects on an individual's capacity to attend and respond to the outside world. First, an individual's direction of attention is altered, in that the focus of attention is narrowed principally to disorder-congruent stimuli, ranging from external events to internal experiences. Thus, in the presence of multiple competing stimuli, attentional resources are preferentially allocated to stimuli that have personal relevance. More specifically, in anxiety, attentional resources are directed either externally by scanning the environment for threat (Williams, Watts, MacLeod, & Mathews, 1997) or internally by scanning the self for how one appears to others (Clark & Wells, 1997). In depression, the focus of attention is predominately directed toward the self (Ingram, 1990; Mor & Winquist, 2002) including dysphoric symptoms and their consequences (Nolen Hoeksema, 1991). Second, because attentional resources have limited capacity, differential allocation of attentional resources impairs the processing of other stimuli in the environment and adversely affects speed of performance, performance on a secondary task, and problem solving (Eysenck & Calvo, 1992; Sarason, Sarason, Keefe, Hayes, & Shearin, 1986; Williams et al., 1997).
Although occasional worry and rumination are experienced by most individuals, they are much more readily activated by personally relevant, moment-to-moment daily life experiences in individuals with generalized anxiety disorder and major depression, resulting in relatively pervasive states of worry and rumination. In addition to their effects upon attention, worry and rumination are associated with increased negative affect (Nolen Hoeksema, 1991; Segerstrom, Tsao, Alden, & Craske, 2000; Startup & Davey, 2001). Such increases in negative affect appear to be even greater in individuals with generalized anxiety disorder and major depression than in nondisordered individuals, possibly due to elevated baseline levels of negative mood. Thus, when individuals with anxious or depressive disorders worry or ruminate, the effects are presumed to be even more negative in comparison to healthy controls.
In what ways might these cognitive processes have an impact on the quality of parental responsiveness and thereby on the infant's development? There is an increasing body of evidence that, from the first months of life, infants are very sensitive to the quality of parental responsiveness (Brazelton, Koslowski, & Main, 1974; Cohn & Tronick, 1983; Nadel, Carchon, Kervella, Marcelli, & Reserbat-Plantey, 1999; Trevarthen, 1979). Parental responsiveness plays a crucial role in parent–infant interaction, which in turn impacts the child's development (Murray et al., 2010; NICHD Early Child Care Research Network, 1999). It is thus proposed that worry and rumination interfere with the carer's communications by altering attentional focus and reducing the carer's responsiveness to the environment. As a consequence, the carer's ability to respond sensitively to infant cues and needs is reduced. The present study was designed to investigate the possibility that mothers with generalized anxiety disorder and major depression will have impaired responsivity to their infants, since they spend more of their time worrying or ruminating than nonclinical mothers. Further, evidence in the context of parental psychiatric disorders indicates that parenting difficulties are most likely to emerge under conditions of stress or challenge (Ginsburg, Grover, Cord, & Ialongo, 2006). Thus, we examined whether common, everyday, negative challenges led to a reduction in the quality of parenting—responsiveness and interaction in particular—relative to baseline conditions.
The overall aim of the study was to investigate whether a direct experimental manipulation of maternal worry and rumination affected mother–infant interaction in mothers with generalized anxiety disorder, depression and nondisordered controls. This experiment was embedded in a larger, 24-month prospective study investigating the influence of maternal cognitions on the child and mother–child interaction in the context of postnatal depression and anxiety. The sample was recruited in the first six months of the child's life and the experiment reported herein was conducted at 10 months. The rationale for the 10-month window was twofold. First, a significant developmental shift occurs around 10 months, with infants becoming more aware of their mothers' behavior and her focus of attention to the wider environment (known as social referencing and joint attention) (Campos & Stenberg, 1981; Striano & Stahl, 2005). Thus, 10 months provides a critical period in which to evaluate the influence of maternal attention upon mother–infant interactions. Second, since a significant proportion of maternal postnatal depressive disorders remit within a few months (Cooper & Murray, 1995) it was possible to assess the extent to which remission of early maternal psychopathology conferred residual effects upon the quality of mother–child interaction at later months.
The first aim was to evaluate whether an experimental manipulation that activates states of worry and rumination in mothers with generalized anxiety disorder and depression leads to diminished quality of mother–child interactions, compared with nonactivated control conditions, and compared with control mothers. The two key aspects of maternal behavior during mother–infant interactions assessed were the quality of maternal responsiveness and the extent of maternal interaction. With regard to the quality of maternal responsiveness, several aspects were targeted. An important feature of parental responsiveness is “mild control”, which refers to facilitation, or parental actions that help or enable the infant with an activity. Diminished levels of such behavior have been associated both with parental depression (Murray et al., 2010) and anxiety (McLeod, Wood, & Weisz, 2007; Murray et al., 2008). In addition, two specific aspects of parental responsiveness were assessed: (a) The extent to which parents provided behavioral evidence that they noticed and responded specifically to the infant's vocalizations, and (b) given that 10 months is the beginning of joint attention, the extent to which mothers followed and responded to changes in the child's attention. Strong control and intrusiveness, two aspects of parenting responsiveness that are considered to be inappropriate were measured at both verbal and behavioral levels. “Strong control” refers to parental language such as commands or prohibitions, and “intrusiveness” refers to parents' behavior which is either coercive or fails to pick up on infant signals but instead, inappropriately cuts across or disrupts infant activities. Over-control and intrusiveness have been associated with postnatal depression (Field, 1995; Murray et al., 2010), and are considered important components of parenting involved in transmission of anxiety (Wood, McLeod, Sigman, Hwang, & Chu, 2003). Finally, a general measure of the extent to which the mother interacted with the child was operationalized as the amount she spoke and the extent of her withdrawal/engagement. Mothers with depression have been found to be withdrawn and to speak less to their children (Field, 1995; Murray et al., 2010), and there is also evidence for less maternal active engagement in the context of maternal anxiety (Moore, Whaley, & Sigman, 2004; Murray, Cooper, Creswell, Schofield, & Sack, 2007). Thus, an experimental manipulation which activates states of worry or rumination was hypothesized to lead to less responsive parenting in mothers with generalized anxiety disorder and major depression, relative to control conditions and control mothers. This change in parenting would manifest as more maternal strong control and intrusiveness, less facilitation, less responsiveness to infant vocalizations and following of infant attention, and less maternal interaction. Finally, specific activation of worry and rumination was hypothesized to lead mothers to self-report more self-focus, more negative thinking, more repetitive thinking and more difficulty controlling thoughts, which are characteristics of worry and rumination (Nicol-Harper, 2005; Stein et al., 2009).
As part of the aim to examine the effects of the experimental manipulation on mother–infant interaction, a number of aspects of infant behavior were assessed. Two constructs were of interest. The first, complementary to the maternal interaction variables, concerned the extent of interaction, as measured by the amount of infant vocalization and withdrawal/engagement. Children of mothers with depression (Field, 1995) and anxiety (Wood et al., 2003) have been shown to have withdrawn behavior. The second was the infant's mood/emotional tone, given the evidence that if parents become unresponsive, infants in turn often become distressed (Murray & Trevarthen, 1985). The hypothesis tested was that activation of worry and rumination in mothers with generalized anxiety disorder and major depression would lead to more negative infant emotional tone and less vocalization and engagement with the mother or tasks, compared to control conditions and control mothers.
The second aim was to evaluate whether any observed effects of the experimental manipulation were evident among the subgroup where the mother's disorder had remitted by the time the infant was 10 months old. Because of the evidence that latent cognitive disturbances are vulnerable to reemergence in individuals whose depression or anxiety has remitted (Lyubomirsky & Nolen-Hoeksema, 1995; Joormann & Gotlib, 2007; Singer & Dobson, 2007; Mathews, May, Mogg, & Eysenck, 1990), we hypothesized that the effects would be apparent even in mothers whose disorders had remitted by 10 months, relative to controls. If indeed these latent cognitions are easily primed in remitted mothers and they, in turn, lead to negative effects on mother–infant interaction, this process may represent a mechanism through which parental behaviors negatively impact child development after remission of parental psychiatric disorders (Murray et al., 2010; Rutter, 1990).
Method
Overall Design
When the infants were three and six months old, mothers were categorized into one of three diagnostic groups: Generalized anxiety disorder, major depression, or nondisordered controls. When the infant was 10 months old, mothers in each group were randomized to one of two priming conditions (stratified randomization): The first was designed to activate worry and rumination, and the other was designed to be neutral. Mother–infant interactions were assessed before and after priming, and the mother's diagnostic status was also reassessed.
Participants
The majority of participants for our longitudinal observational cohort study, the Oxford Parent Project (OPP), were recruited from postnatal wards at the John Radcliffe Hospital, Oxford. Recruitment was supplemented through a number of health centers in Oxfordshire. Eligibility criteria for the mothers were: 17 years of age or older, having sufficient level of English, living within 35 miles of Oxford, having no life-threatening medical conditions, and planning to be the infant's principal caretaker. Eligibility criteria for the infants were: having had over 35 weeks' gestation, weighing over 2000 g at birth, and having no life-threatening medical complications. Ethical approval was provided by the Oxford Psychiatric Research Ethics Committee.
Two screening questionnaires were completed by 2202 women when the infant was approximately 9 weeks old. The Edinburgh Postnatal Depression Scale (EPDS) is a well-validated and extensively used screening measure for postnatal depression (Cox, Holden, & Sagovsky, 1987) with a sensitivity and specificity of over 80% (Murray & Carothers, 1990). The Generalized Anxiety Disorder Questionnaire (GAD-Q) is a validated self-report diagnostic questionnaire with specificity and sensitivity over 80% (Newman et al., 2002).
Mothers who scored high on either screening questionnaire (>12 on the EPDS, >5.70 on the GAD-Q), and a randomly selected group of women who scored below the cut-off on both questionnaires, were visited at home when their infants were 3 months old. At that time, 472 scored above the GAD-Q cut-off, 293 above the EPDS cut-off, including 226 who scored above both cut-offs. The Structured Clinical Interview for Diagnostic and statistical manual of mental disorders (4th ed., Text Rev.; DSM–IV–TR) Axis I Disorders was administered (SCID, research version; First, Spitzer, Gibbon, & Williams, 2002) to establish diagnostic group status (i.e., GAD, MDD, and controls [CON]). A second home visit was conducted when the infant was 6 months old to reassess the mother's diagnosis using the SCID. Interviewers also rated the clinical severity (i.e., distress and interference) of each disorder using the Clinician Severity Rating (CSR; Brown, Di Nardo, Lehman, & Campbell, 2001; DiNardo, Moras, Barlow, Rapee, & et al., 1993), a 0–8-point scale on which a score of 4 or more indicates clinical severity. All interviews were audio-recorded. Interviewers (bachelors/master's level) were trained extensively. Interviewer drift was minimized by the following steps: throughout the study, supervision and review of diagnostic assessments were led by the primary author of this study in weekly case meetings; the second author reviewed tapes of randomly selected interviews during the first six months of the study; and after each interviewer completed five to six interviews, an independent interviewer corated the next interview to assure interrater reliability. The second author then reviewed tapes periodically throughout the study.
Group Assignment
Diagnostic group assignment was based on DSM–IV–TR diagnostic criteria for GAD or MDD with a CSR of 4 or higher at the 3-month assessment. In cases of comorbidity, participants were assigned according to the disorder with the highest CSR. Mothers with subthreshold disorders (usually because the length of symptomatology did not fulfill DSM criteria) or who had a history of depression or anxiety at 3 months were reassessed at 6 months. If they met DSM criteria at 6 months, they were included in the respective study groups. This occurred for five participants (one GAD and four MDD). Furthermore, prior to the 10-month assessment, participants were sent the two screening questionnaires, the EPDS and the GAD-Q. Three mothers who had a history of depression or anxiety but had not met diagnostic criteria at 3 or 6 months scored above the cut-off values at 10 months and were reassessed with the SCID. All three were confirmed to have developed a disorder: Two GAD and one MDD, and were included in the respective study groups.
Participants were assigned to the Control group (CON) if the SCID interviews confirmed that they did not meet criteria for any disorder at any assessment point, if they reported no history of a psychiatric disorder, and if their partners reported no current or history of a psychiatric disorder. In addition, one participant, who scored above the cut-off on the EPDS just before the 10-month assessment, was confirmed through the SCID interview to meet diagnostic criteria and was removed from the control group and placed in the MDD group.
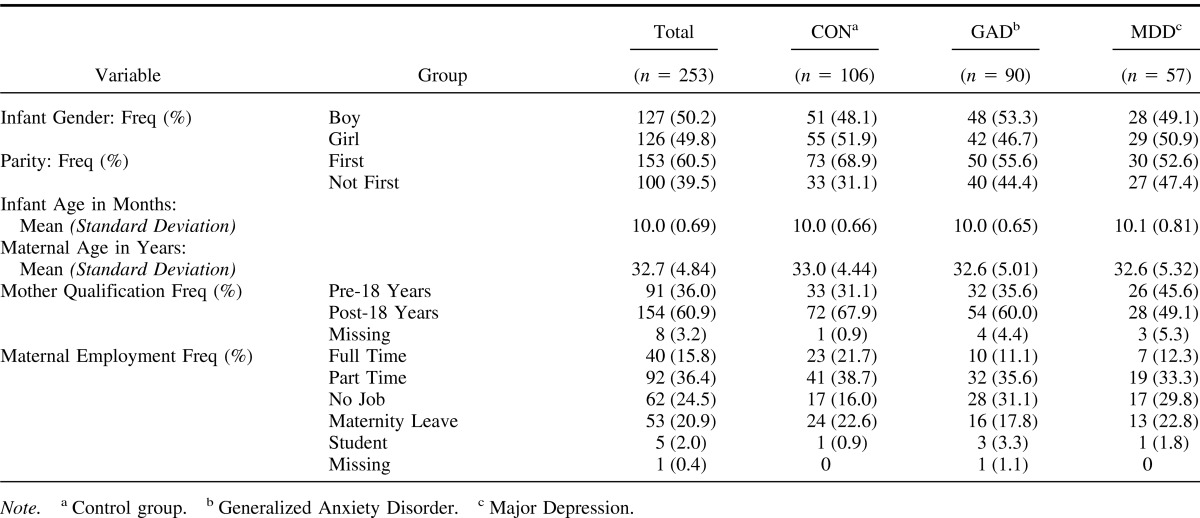
A total of 296 (GAD n = 105; MDD n = 67; CON n = 124) participants were recruited into the OPP study across the three assessment time points. A total of 253 participants (GAD n = 90; MDD n = 57; CON n = 106) completed the 10-month assessment, comprising 85% of the total sample recruited. At the 10-month assessment, 12 (13.3%) mothers with a principal diagnosis of GAD were comorbid for MDD and 10 (17.5%) mothers with a principal diagnosis of MDD were comorbid for GAD. Table 1 presents the demographic information for the study sample; there were no significant differences on any of the demographic variables across the three groups, or between the randomized priming conditions. The 15% who dropped out before the 10-month assessment did not differ significantly from those who completed the study, except that they were somewhat younger and had lower levels of education.
Table 1. Demographics by Case Group.
Of the 90 mothers with GAD, 87 were entered into the study at 3 months, one at 6 months, and two at 10 months; 15 (16.7%) were comorbid for MDD at 3 months and six (6.7%) at 6 months. Of the 57 mothers with MDD, 51 were entered at 3 months, four at 6 months, and two at 10 months; 19 (33.3%) were comorbid for GAD at 3 months, and 17 (29.8%) at 6 months. In addition, of the 88 mothers diagnosed with GAD at 3 or 6 months, 41 (46.6%) had remitted by the 10-month assessment. Of the 55 mothers diagnosed with MDD at 3 or 6 months, 27 (49.1%) had remitted by the 10-month assessment. These rates of remission are consistent with the evidence that many cases of postnatal depression remit within a few months (Cooper & Murray, 1995), although similar longitudinal research has not been conducted in the context of GAD.
Laboratory Assessment at 10 Months
Design
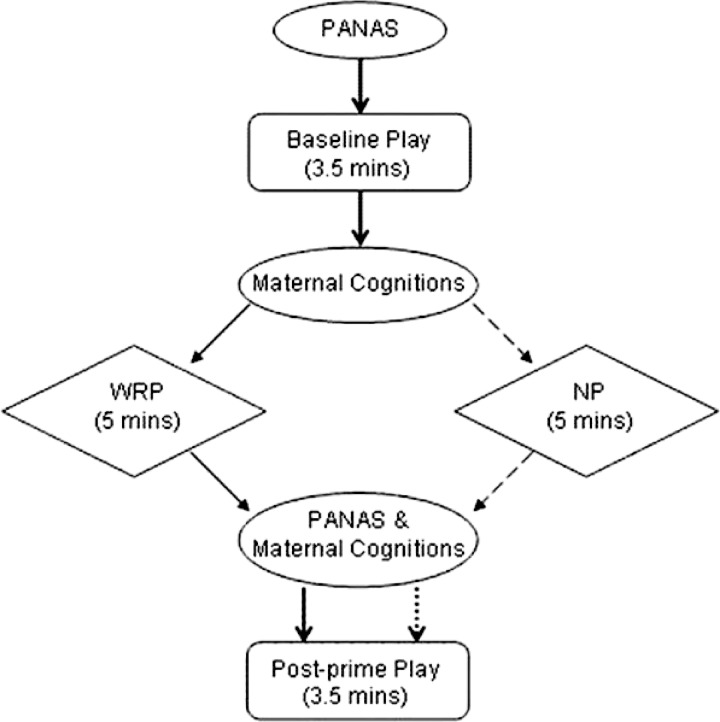
Participants from each group (CON, GAD, MDD) were randomized to one of two priming conditions: Worry/rumination prime (WRP) or neutral prime (NP). Mother–infant interactions were recorded on two occasions: Baseline (before priming), and postprime (after priming). Measures of maternal mood and cognitions (thoughts and direction of attention) were completed throughout (see Figure 1).
Figure 1. Flowchart of 10-month visit.
Priming conditions
The purpose of the priming conditions was to evaluate how activation of recurrent negative thinking affected mother–infant interaction relative to a control condition, matched on cognitive demand but without emotional valence. The WRP was designed to match states of worry/rumination as they would occur in daily life. The priming involved a set of instructions that directed thinking to particular topics for five minutes. In the WRP condition, GAD participants were instructed to “pick a topic that most worries you, close your eyes, and worry about that topic as you normally would, as intensely as you can”, a method shown in prior research to reliably induce worry (e.g., Oathes et al., 2008). Correspondingly, MDD participants were instructed to “think about something that has been most negative in your life, close your eyes, and concentrate on your negative thought, as intensely as you can”; and CON participants were instructed to “close your eyes and think about something in your life that has been negative or has been worrying you, as intensely as you can”. In the NP condition, all participants were instructed to “close your eyes and think about your journey here, in as much detail as you can”. These primes were piloted prior to use in the experimental condition.
Mother–infant interaction
The two structured mother–infant interactions each lasted 3.5 minutes. The mother and infant sat on a circular rug in the middle of the room and the mother was asked to play with him/her as she normally would, and to encourage her child to stay on the rug as much as possible (to facilitate video recording). In the baseline interaction, the mother was provided with two colorful soft toys that had squeaky and rattling parts. In the postprime interaction, she had one toy with multiple parts available, a container with rattling blocks. All three toys offered a range of tactile, visual and auditory stimuli. It was necessary to use a new, somewhat different toy in the postprime interaction, as otherwise the infants might lose interest. Though both baseline and postprime toys were developmentally equivalent in terms of challenge and complexity, two toys were offered at baseline to help the mother settle. Care was taken to ensure that all three toys were age-appropriate (they were tested with 10-month old pilot participants) and that pre- and postprime toys were developmentally equivalent and provided plenty of scope for exploration and play. Furthermore, the toys chosen were those which most 10-month-olds would need help with. Thus, effective play would require motor-cognitive support from the mother, thereby providing a suitable competing demand against which to compare the effects of recurrent negative thinking.
Coding of mother–infant interactions
Videotaped recordings of each interaction were coded by a rater who was blind to diagnostic group and priming condition and was not aware of the study hypotheses. The baseline and postprime observations were coded in random order. The rater was trained to reliability with a gold-standard rater prior to rating study videotapes. Periodic checks were made during the study to ensure that there was no drift. Each interaction was coded separately. A set of behaviors reflecting the key constructs being examined were rated on a predefined ordinal scale (3-point or 5-point) as used in prior research (Murray, Fiori-Cowley, Hooper, & Cooper, 1996; Stein et al., 1994). Of the total 253 mother–infant assessments, four were not coded (due to damage to the tapes or more than 90 seconds missing). Twenty-five cases (10% of the sample) were coded additionally by a second rater for reliability purposes, with square-weighted Kappa (κ) indicating good interrater reliability across the coded mother–infant interaction variables (values of κ are provided for each variable below; κ > 0.6 is considered substantial (Landis & Koch, 1977).
Maternal coded ratings assessed the quality of maternal responsiveness to the infant and the extent of maternal interaction, on 3-point and 5-point scales, with higher scores reflecting better functioning (more responsiveness and engagement) with one exception noted below. The ratings included: (a) intrusiveness (reverse scored, ordinal 1–5), which was operationalized as the extent to which the mother inappropriately cut across, took over, or disrupted infant's activities (weighted κ = 0.87); (b) strong control (ordinal 1–3 with lower scores representing better functioning): The extent to which the mother used language of strong control (command, prohibit, stern warning, or forbid), with or without strong nonverbal behavior (weighted κ = 0.62); (c) facilitation (ordinal 1–5): Actions by the mother that helped or enabled the infant with an activity that he or she was already engaged in, or had signaled he or she wished to do (weighted κ = 0.88); (d) maternal withdrawal (reverse scored, ordinal 1–5): The mother's lack of engagement/interaction with her infant (weighted κ = 0.69); (e) maternal vocalization (ordinal 1–5): The amount the mother spoke to the infant during the play session (weighted κ = 0.76); (f) following child's attention (ordinal 1–5), including the extent to which the mother had noticed that the child's attention had shifted to a different aspect of the task or away from the task; and if the child became distracted, the extent to which she acknowledged this before trying to draw him/ her back to the task (weighted κ = 0.79); and (g) maternal responsiveness to infant vocalizations (ordinal 1–5): The extent to which the mother demonstrated verbally or behaviorally (smiling or nodding or other behavioral gesture) that she had responded to the infant's vocalizations (weighted κ = 0.63).
Infant coded ratings comprised: (h) infant vocalization (ordinal 1–5): How vocal the child was throughout the session, taking account of whether vocalizations were speech-like (weighted κ = 0.93); (i) infant's emotional tone/mood (ordinal 1–5): A measure of the child's emotional tone (happiness/unhappiness) as expressed through vocalizations, facial expressions, and animated behavioral responses, ranging from 1 (very negative), to 3 (neutral), to 5 (very positive; weighted κ = 0.86); and (j) infant withdrawal (reverse scored, ordinal 1–5): The infant's lack of engagement and responsiveness to the mother and/or toys (weighted κ = 0.75).
Maternal mood and cognition ratings
Mothers completed two questionnaires. The first was the 10-item Short Positive and Negative Affect Scale (PANAS-SF, or Short PANAS; Kercher, 1992) to assess positive and negative affect. The Short PANAS demonstrates similar factor structure, reliability, discriminant validity, and internal consistency to the full 20-item PANAS (Watson, Clark, & Tellegen, 1988). The Short PANAS was completed before the baseline interaction, and after the prime.
The second questionnaire required the participants to rate different aspects of their cognitions. The items were based on a measure of preoccupation that was developed to encompass the definition of negative recurrent thinking (Nicol-Harper, Harvey, & Stein, 2007; Nicol-Harper, 2005; Stein et al., 2009). Specifically, participants rated (a) three items concerning the degree of focus upon the environment, infant, and self (0–10-point Likert scales); (b) affect of thoughts from negative to positive (−8 to + 8); (c) difficulty in controlling and directing thoughts (reverse scored, 0–10); and (d) level of thought recurrence (0–10). These items were used as they reflected the core features of worry (Nicol-Harper, 2005). The cognition ratings were completed after the baseline interaction, and after the prime.
Procedure
Study participants were invited to the laboratory when the infant was 10 months old; the visit lasted approximately 90 minutes. At the beginning of the visit, the experimenter spent considerable time explaining what would happen during the session and giving each mother a chance to ask questions. This provided the mother–infant dyad an opportunity to adjust to their surroundings and become familiar with the experimenter. After signing an informed consent form and updating demographic information, the participants completed the baseline mother–infant interaction task, priming, and the postprime interaction task, with questionnaires throughout (approx. 45 minutes;see Figure 1). Each task started with the experimenter again explaining what the mother was expected to do next. In general, the transitions from one experimental activity to another were done in a manner sensitive to the infant's needs and his or her readiness for interaction and play. When appropriate, he or she was included in the interaction between the mother and the experimenter. Also, the mother–infant interactions were ended after 3.5 minutes by the experimenter gently entering the interaction in a nonintrusive way. During each mother–infant interaction, the experimenter sat quietly at a table in the room, looking away from the dyad and not interacting with them in any way. This was considered less disruptive than the experimenter repeatedly leaving and entering the room. Three wall-mounted cameras ensured that the mother and infant could both be recorded. A second researcher moved the cameras remotely from another room to track the movement of the participants. During priming, the second researcher entered the room to look after the child while the first experimenter facilitated the priming task with the mother. The mother wore hearing protectors to reduce external noise and was asked to close her eyes to aid concentration. She was asked to carry on with the prime even if her baby came over to her, and she was reassured that the second researcher would look after the baby and keep him or her entertained. Nineteen mothers were approached by their infants during the priming, almost all very briefly: five MDD (four WRP and one NP); seven GAD (all WRP) and seven controls (three WRP and four NP).
At the end of the experimental session, there was an additional five minutes of free play which were recorded on DVD for the mother to take home, and another brief task that will be reported elsewhere. After this, mothers were debriefed by redirecting attention to positive aspects of their infant and providing support and reassurance. This was to address any lingering negative effects of the priming conditions. Finally, the mothers were offered refreshments and the SCID was administered to obtain a measure of the mother's current diagnostic status. At this time, the infant played with the mother or rested and was fed/changed as appropriate. It was made clear to mothers that they were free to respond to the infant's needs as they wished.
Analyses
The experiment employed a 3 (group) × 2 (prime) between-groups design. The principal comparison was between the WRP condition and the NP condition within each of the three diagnostic groups. Analyses were also performed across CON, GAD, and MDD within each priming condition. Ordinal logistic regression was used to assess the postprime mother–infant codes, adjusting for baseline ratings, due to the ordinal nature of the response data and associated distribution (Bender & Grouven, 1997; Long, 1997). Odds ratios (OR) are presented for main effects; these represent the increase (OR >1) or decrease (OR <1) in the odds of having a higher response on the ordinal scale associated with participation in a given experimental cohort. This technique, an extension of binary logistic regression, assumes proportional odds (i.e., that the effects do not differ across levels of the response variable) but requires neither distributional assumptions on the response variable nor data transformations. The logit (i.e., the logarithm of the odds of success) of the cumulative probability is modeled as a linear function of the predictors; Wald tests (for single terms) and likelihood ratio tests (for multiple terms within nested models) were used to investigate statistical significance, while residuals and formal tests of parallel lines were used to assess the proportional-odds assumption and general goodness of fit. Ordinal logistic regression and analysis of covariance (ANCOVA) were used where appropriate (log-transformed data when specified in order to satisfy ANCOVA's assumptions) to assess the effect of the priming conditions across diagnostic groups on maternal mood and cognitions, respectively.
Variable entry in model selection was in line with the hypotheses: First, the effect of the priming conditions was inspected, then diagnostic group was entered, and finally an interaction term was included to assess whether the effect of priming conditions was consistent across diagnostic groups. If this interaction term was significant, neither of the priming or group effects were described, as implicitly these would vary across levels of the other variable. Interaction plots, showing the difference between the pre- and postprime scores, are provided to aid the interpretation of significant priming by group interaction terms; note that these do not fully represent the complex ordinal nature of the data or the associated regression modeling process that was implemented. However, together with the testing of carefully defined contrasts of interest (e.g., between WRP and NP conditions within each group), interaction plots helped to deconstruct the differences that exist within the observed data. Finally, to evaluate whether remission status moderated significant priming, group, or priming-by- group interactions, a further interaction term with clinical status at 10 months (CSR ≥4; remission CSR <4) and all lower-order terms were included in these models. For example, in the instance of evidence of a priming effect, to test whether the effect was moderated by 10-month clinical status, a further prime × remission-interaction term and single remission term were included. Similarly, to investigate whether a prime-by-group interaction was moderated, a further 3-way interaction term (prime × group × remission) and all lower-order terms involving remission were then also included.
All regression models had postprime scores as the response, with preprime scores included as a covariate to adjust for observed baseline data; in addition, the inclusion of associated (p < .1) demographic characteristics as covariates were considered to ensure that significant differences were not due to known confounders for each given response. Likelihood ratio tests were used to establish the overall significance of introducing interaction terms. Data processing and analyses were conducted in the statistical computing environment R, version 2.7.1 (R Developmental Core Team, 2010) and SPSS, version 15.0.1 (SPSS for Windows, Rel. 15.0.1.; 2001).
Results
Maternal Mood and Cognition Ratings
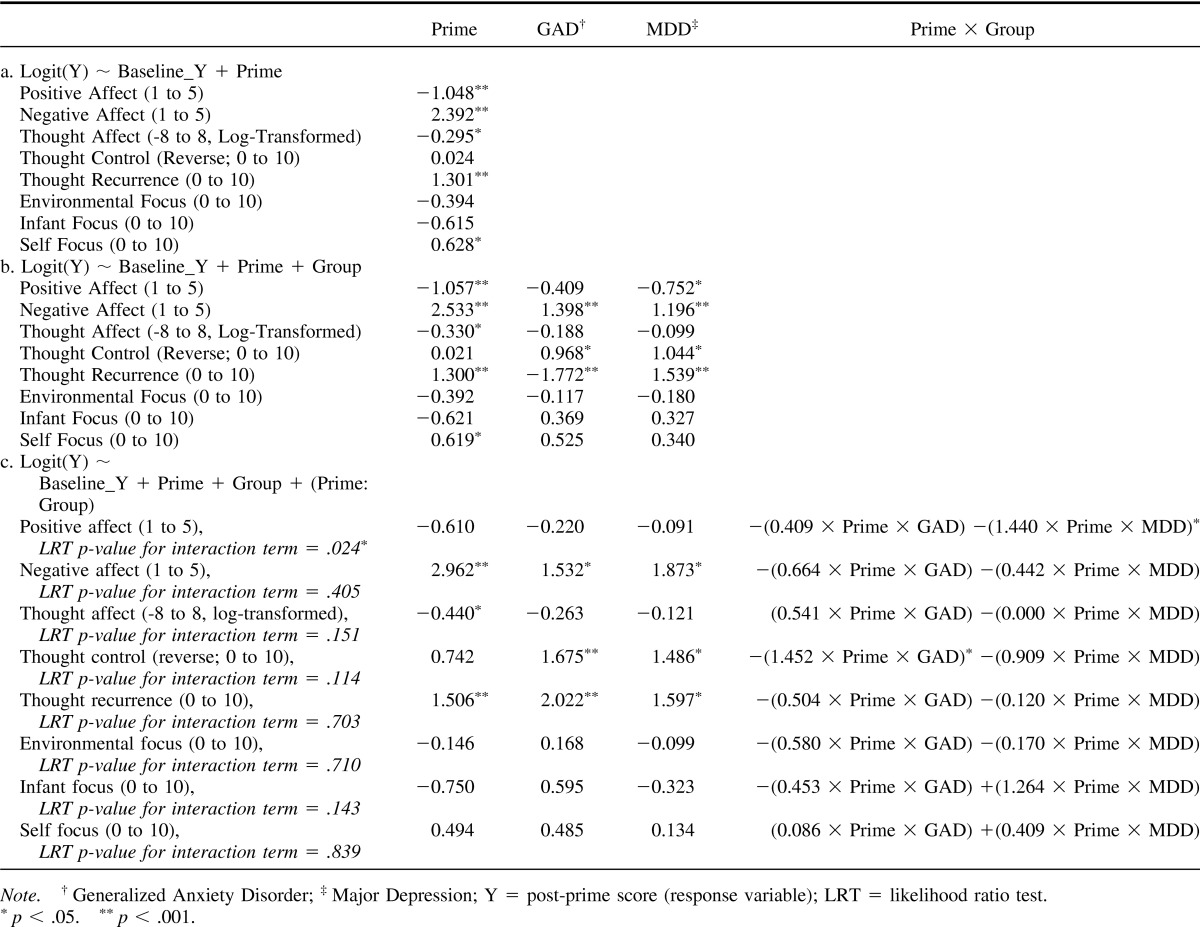
Table 2 presents the results of the ordinal logistic regression and ANCOVA modeling of postprime maternal mood and cognition ratings, adjusting for baseline interaction, with the NP condition and CON participants serving as the reference groups. First, priming condition was entered into the model to investigate the effect of prime across diagnostic groups. Second, differences between the diagnostic groups were examined. Finally the priming–by-group-interaction term was tested. Regression coefficients are presented for priming condition, diagnostic groups, and interaction terms.
Table 2. Modeling Post-Prime Maternal Mood and Cognition Ratings—Regression Coefficients of Main Effects and Interaction Terms.
PANAS
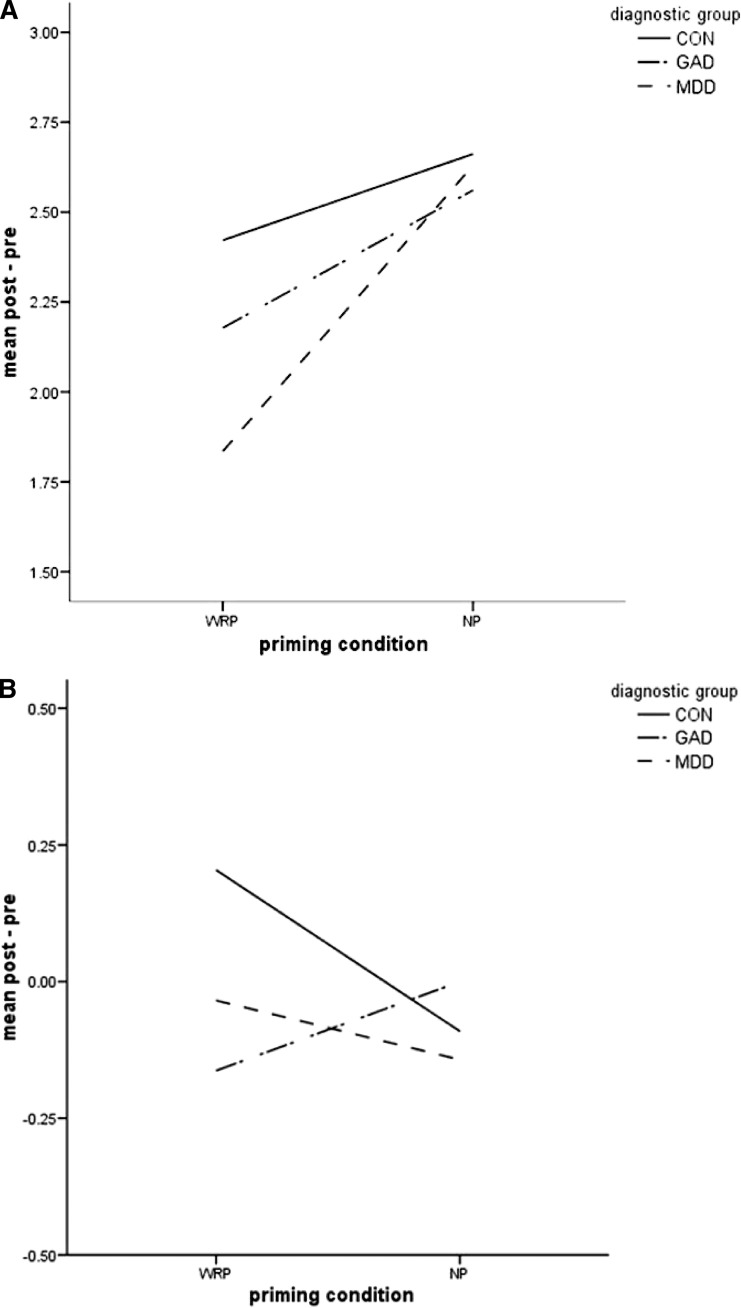
Significant interaction effects occurred between priming condition and diagnostic group for positive affect (p = .024); see Figure 2A. Contrast analyses were carried out to investigate the interaction. All between-groups, within-condition comparisons were nonsignificant (WRP: GAD vs. CON, p = .201; MDD vs. CON, p = .305; NP: GAD vs. CON, p = .570; MDD vs. CON, p = .837). However, positive affect was lower in the WRP condition than NP within GAD (p = .031) and MDD (p = .020), but not within CON (p = 0 .102).
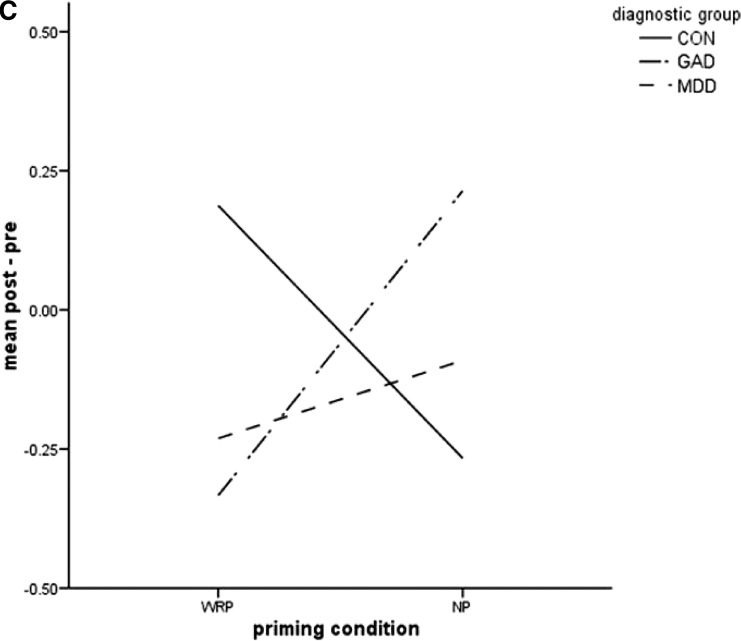
Figure 2. A. Interaction plot for maternal PANAS positive affect. B. Interaction plot for maternal vocalization. C. Interaction plot for maternal responsiveness to infant vocalization.
Interaction effects were not significant for negative affect. However, there was a significant main effect for priming condition, with the WRP condition having higher odds of high negative-affect ratings than NP (OR = 12.59 (95% CI = 6.67 to 23.76), p < .001). Also, there was a significant main effect of group, with both GAD and MDD having increased odds of higher postprime negative-affect ratings than CON (GAD: OR = 4.05 (2.05, 7.99), p < .001; MDD: OR = 3.31 (1.56, 7.01), p = .002).
Cognitions
There were no significant interactions between priming condition and diagnostic group. However, there was a significant main effect of priming condition, such that the WRP condition resulted in lower ratings of thought affect (p = .028), higher ratings of thought recurrence (p < .001) and higher ratings of self-focus (p = .019) than NP. Also, there was a significant main effect of group, with both GAD and MDD having higher ratings of thought recurrence (p's < 0.001) and more difficulty controlling thoughts (GAD: p = .008; MDD: p = .012) than CON.
Mother–Infant Interaction
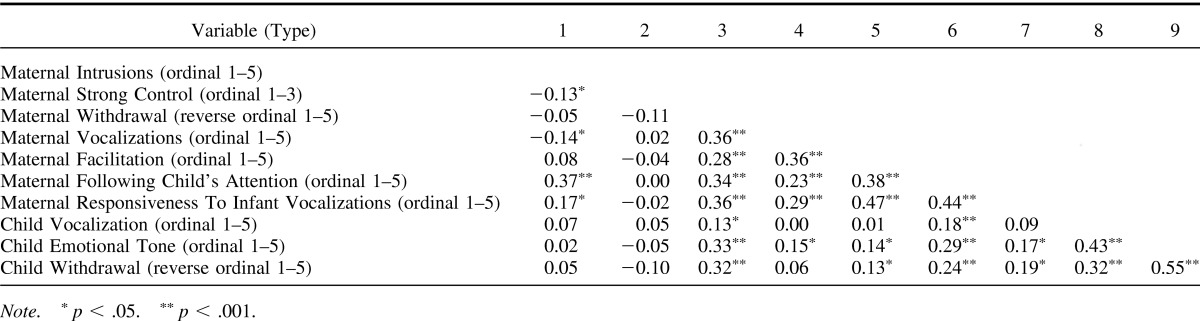
At baseline, the variables were weakly to moderately correlated (Spearman's ρ ranging from 0.00 to 0.55) and thus were nonredundant, see Table 3. The only significant effects of maternal group was that mothers with MDD followed their child's attention less than CON (Wilcoxon's-Mann–Whitney test, p = .037); mothers with GAD showed a similar pattern (p = .052).
Table 3. Pair-Wise Correlations Between Baseline Mother-Infant Interaction (Spearman's ρ).
Postprime interaction
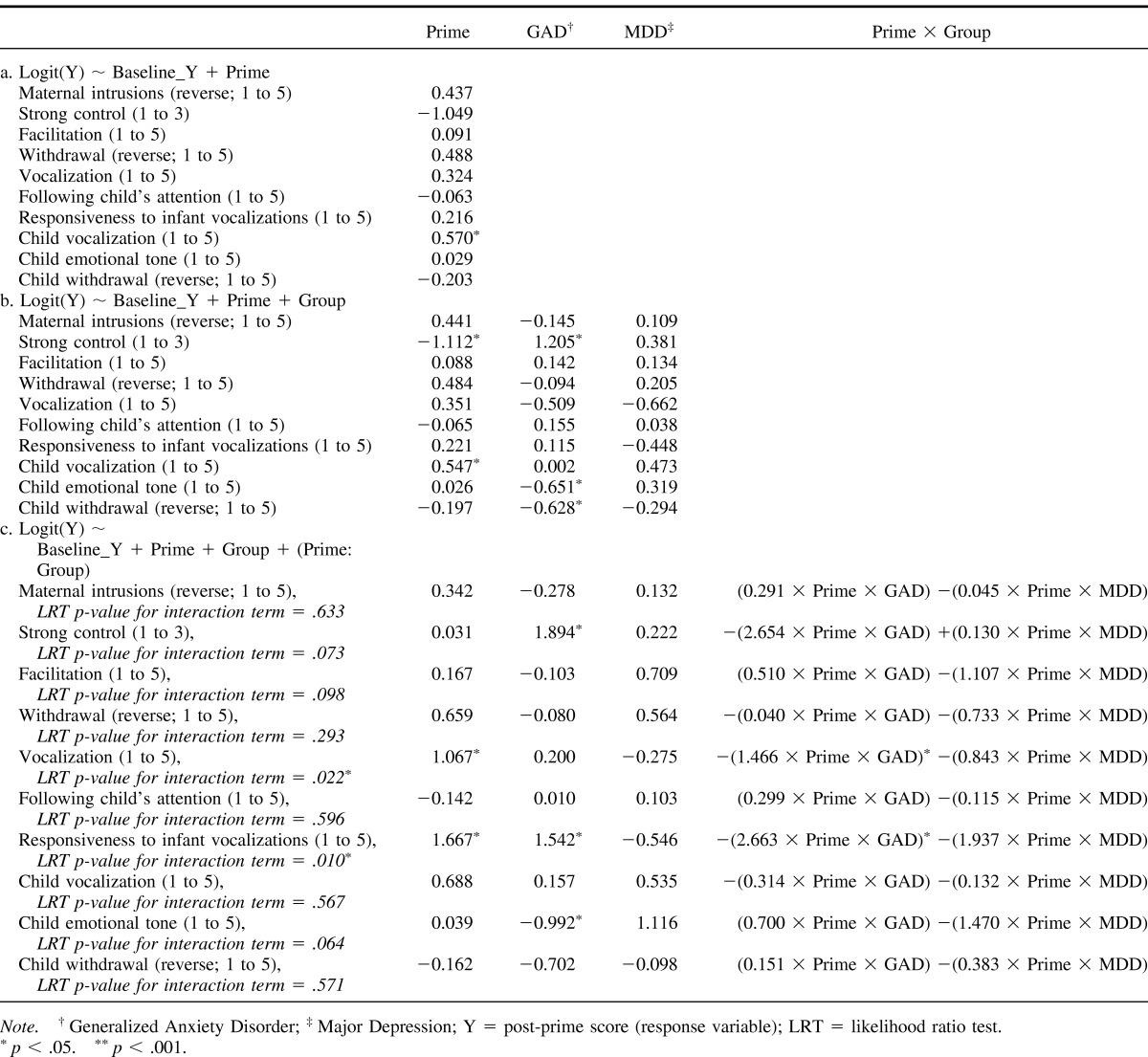
Table 4 presents the results of the ordinal logistic regression modeling of postprime mother–infant interaction, adjusting for baseline interaction, with the NP condition and CON serving as the reference groups. First, priming condition was entered into the model to investigate the effect of prime across diagnostic groups, then diagnostic group was entered, and finally the priming-by-group interaction term was tested. There was no evidence for significant associations between these outcome variables and sample demographics.
Table 4. Modeling Post-Prime Mother-Infant Interaction—Regression Coefficients of Main Effects and Interaction Terms.
Significant interaction effects occurred between priming condition and diagnostic group for two variables. The interaction effect was significant for maternal vocalization (p = .022), see Figure 2B; contrasts were tested to further elucidate the effects. The comparison between GAD and CON within WRP approached significance (p = .087), with maternal vocalization lower in mothers with GAD than control mothers, but the remaining between-groups comparisons were not significant (WRP: MDD vs. CON, p = .306; NP: GAD vs. CON, p = .647; MDD vs. CON, p = .579). Also, maternal vocalization was higher in the WRP condition than NP within CON (p = .013), whereas it tended to be lower in the WRP condition than NP within GAD (p = .087); the effects for MDD were nonsignificant (p = .306). The interaction effect was also significant for maternal responsiveness to infant vocalizations (p = .010), see Figure 2C. Testing the contrasts, we found that maternal responsiveness to infant vocalizations was significantly lower in GAD than CON within the WRP condition (p = .011), and significantly higher than CON in the NP condition (p = .036). Maternal responsiveness to infant vocalization tended to be lower in MDD than CON within the WRP condition (p = .082) but not within the NP condition (p = .479). Also, maternal responsiveness to infant vocalization was lower in the WRP condition than NP within GAD (p = .011), with a similar trend within MDD (p = .082), and higher in the WRP condition than NP within CON (p = .019).
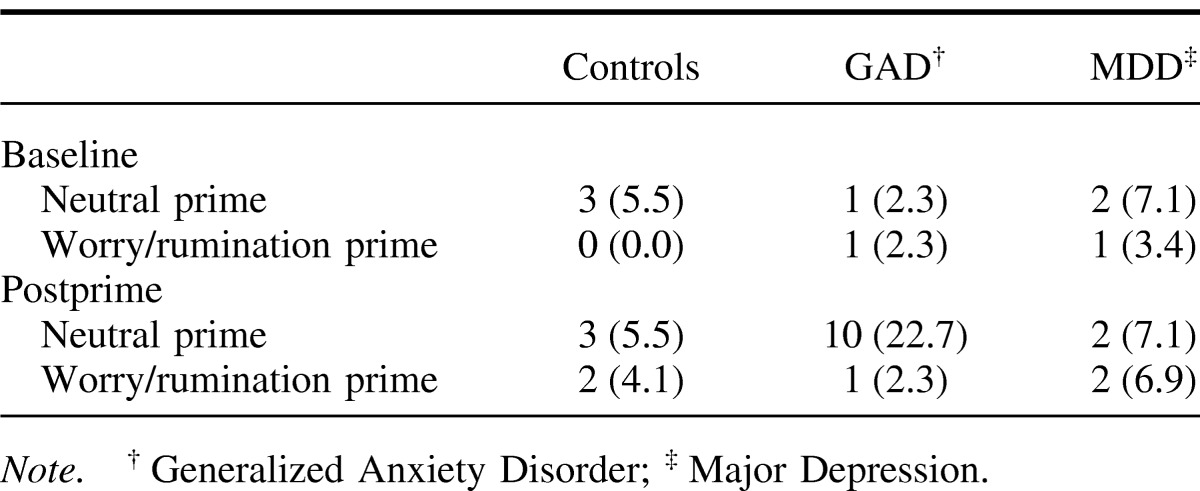
Four other variables showed significant effects of priming condition or of group. In terms of strong control, WRP yielded significantly lower odds of strong control than NP (OR = 0.33 (0.11, 0.96), p = .042), and GAD had significantly increased odds of strong control than CON (OR = 3.34 (1.06, 10.50), p = .039). Few mothers used strong control (the variable was dichotomized into “never” vs. “ever”) and the interaction term could not be tested due to a lack of variability. However, the raw data (see Table 5) clearly shows that the pre- to postprime score differences exist within one group only; that is, the observed group and priming effects appear attributable to higher odds of strong control in the GAD group after NP. The priming condition was also a significant predictor of child vocalization, with WRP showing increased odds of higher child vocalization than NP (OR = 1.77 (1.1.0, 2.84), p = .018). Additionally, GAD children showed increased odds of less positive emotional tone (mood) (OR = 0.52 (0.28, 0.98), p = .044) and more withdrawal than CON children (reverse scored; OR = 0.53 (0.30, 0.96), p = .035).
Table 5. Number (%) of Mothers Who Used Any Strong Control During Mother-Child Interaction.
Remission Status Effects on Maternal Cognitions and Mother–Infant Interaction
Cognitions
Adjusting for 10-month case status, the interaction and main effects presented remained significant. There were no significant differences between remitted and unremitted participants in ratings of maternal mood or cognitions.
Mother–Child Interaction
In order to investigate whether any of the differences observed between priming conditions, diagnostic groups, and priming-by-group interactions were moderated by the mothers' clinical statuses at 10 months, 2- and 3-way interaction terms with remission status were tested (while including all lower-order remission terms in each ordinal regression model). All were found to be nonsignificant. Thus, the previously observed interaction effects (for maternal vocalizations and maternal responsiveness to infant vocalizations), as well as main effects of priming and group, were not moderated by remission status. However, there was limited power for these complex moderation analyses and thus these results should be considered with caution.
Discussion
The overall aim of this study was to activate recurrent negative thinking (also known as worry and rumination) in mothers with generalized anxiety disorder and major depression, and to examine the effect on mother–infant interaction and infant behavior. Even with simple primes, states of worry/rumination were successfully activated in all groups, as indicated by measures of cognition. Furthermore, consistent with study hypotheses, the primes for worry and rumination resulted in significant changes in mother–infant interactions in comparison to a control condition that was matched on cognitive demand but not on negativity; the effects were significant in mothers with generalized anxiety compared to control mothers and there was evidence of a similar trend for those with major depression. In addition, whether mothers were remitted or not by the 10-month assessment did not significantly impact these findings, although the study may not have been sufficiently powered to detect such effects. Overall, these findings provide support for a causal role of maternal cognitions in mother–infant interactions within the context of postnatal anxiety and depression.
Maternal Mood and Cognition Ratings
The 5-min worry/rumination primes successfully activated recurrent negative thinking in mothers. Measures of mood and cognitions differed significantly from baseline to post-worry/rumination prime, and more so than in the neutral prime condition. In terms of specific effects, negative affect increased more in the worry/rumination prime than in the neutral prime, and to the same degree across all three groups. Furthermore, positive affect decreased following the worry/rumination prime compared with the neutral prime in the GAD and MDD mothers, but not within the control mothers. These findings are consistent with prior literature indicating that states of worry have a greater emotional impact in individuals with ongoing emotional disorders (e.g., Alloy, Kelly, Mineka, & Clements, 1990; Oathes et al., 2008). In addition, mothers with GAD and MDD rated more negative affect overall than did control mothers, as would be expected.
In terms of cognition, thoughts were rated by mothers as more self-focused, recurrent and more negative in the worry/rumination prime than the neutral prime, and similarly across all three groups. Overall, the anxious and depressed mothers rated their thoughts as being more recurrent and more difficult to control than mothers in the control group, in ways that did not differ across the neutral prime or the worry/rumination prime. This finding may suggest that the element of uncontrollability of thinking that traditionally has been linked only to states of worry and rumination may generalize to more neutral topics in anxious and depressed mothers. Alternatively, the neutral topic (i.e., details of the journey to the session) may have generated other negative topics for these mothers, as their comments sometimes portrayed (e.g., worries about being late, concerns about performance during the session). Thus, the neutral topic may have inadvertently induced negative cognition in the same way as has been observed when individuals with GAD worry during tasks that are intended to be relaxing (e.g., Borkovec & Inz, 1990). As indicated below, even stronger effects upon mother–infant interaction of the experimental manipulation may have been obtained with a truly neutral prime, if such a prime exists for individuals prone to negative cognition. It should be noted that these ratings reflect subjective judgments of thoughts and mood and do not necessarily represent the actual processes, since other unmeasured processes may be involved and since judgments can be subject to various responder biases. Thus, it is not possible to draw firm conclusions from these ratings about the effects of the priming; rather, these need to be inferred from changes in the (objective) mother–child interaction measures.
Mother–Infant Interaction
During the mother–infant interaction, mothers with postnatal disorders who received the worry/rumination prime condition were less responsive and less engaged than mothers who received the neutral prime. Specifically, a significant interaction indicated that mothers with generalized anxiety disorder, and to some extent those with depression, were less likely to respond to infant vocalizations than were control mothers, after the worry/rumination prime. Specific contrasts indicated that mothers with GAD who were primed to worry/ruminate were less likely to respond to infant vocalization than when they were neutrally primed, whereas this effect was reversed in control mothers. Mothers with MDD showed a trend similar to mothers with GAD. Also, specific contrasts indicated that the worry/rumination prime led to increased maternal vocalization compared with the neutral prime within control mothers, whereas mothers with GAD showed a trend toward less vocalization following the worry/rumination prime, although this was not evident for mothers with MDD. These results suggest that anxiety, and to a lesser degree depression, in mothers counteract the norm of increased responsiveness following worry or rumination. Perhaps the response of control mothers represents a type of emotion regulation of responding to negative cognitions with greater engagement in their surrounding environment (i.e., with her infant); something that mothers who are anxious or depressed may find difficult to do.
Together, these results indicate specific negative effects of worry/rumination upon maternal response to infants, beyond the effects of neutral cognitive demands. As such, they highlight a potentially important cognitive pathway through which maternal postnatal disorder negatively impacts mother–infant interactions. In other words, recurrent negative thinking patterns involved in worry and rumination appear to negatively influence subsequent mother–infant interactions; since mothers with generalized anxiety disorder and major depression frequently worry or ruminate and these conditions are easily activated, the observed effects upon mother–infant interaction presumably occur pervasively in their daily lives, and consequently impact on infant development. The results are particularly noteworthy given the relatively limited methods used in the current study to activate recurrent negative thinking, and that the effects of five minutes of worry/rumination extended to a subsequent play session with their infants without any further experimental induction. Also, as noted above, the observed effects may have been mitigated by mothers with anxiety and depression engaging in negative cognitions in the neutral prime condition; stronger effects may have been found in comparison with states of purely neutral mentation, if they exist.
Regardless of mother's diagnostic status, priming to worry/ruminate resulted in infants displaying more vocalizations than did the neutral prime. The finding of an associated increase in infant vocalizations is consistent with the still-face paradigm in which infants respond to the decreased interaction from their mothers with increased vocalization as if to acquire their mothers' attention (Cohn & Tronick, 1983). However, the current study did not demonstrate decreased maternal interaction and responsiveness across all groups and thus more research is required to fully understand this observation. In addition, mothers with GAD were more likely to use more strong control than the other groups in the neutral prime relative to the worry prime condition. Reasons why a neutral prime would lead to greater odds of strong control in mothers with GAD are unclear at this time.
The current findings highlight certain similarities and also some differences between maternal depression and anxiety. At baseline, mothers with MDD and mothers with GAD (although to a lesser degree), were less likely to follow their child's attention than control mothers. This finding is consistent with prior reports of the negative influence of maternal depression on mother–infant interactions (Murray et al., 2010). The current findings are relevant because most research to date concerning the effects of postnatal disorders on mother–child interaction and child development has focused on depression, and these data indicate pathways by which maternal GAD may also have adverse effects (Lederman et al., 2008). On the other hand, following child's attention was the only variable to differ across groups at baseline. That is, for the most part the groups did not differ at baseline, which is consistent with prior evidence for most negative effects of maternal psychopathology upon parenting to emerge under conditions of challenge or stress (Ginsburg et al., 2006). Also, as indicated above, mothers with GAD only were more likely to engage in strong control, albeit limited to the neutral prime condition. Furthermore, across both priming conditions, the infants of mothers with generalized anxiety disorder were more likely to show less positive emotional tone and to be more withdrawn than infants of control mothers. The infants' lowered emotional tone (mood) may be the result of the infants' perception of changes in the mothers' mood and behavior. These effects were not observed in the infants of depressed mothers. It was not realistic to formally test for mediation effects because the relatively short observation periods made it very difficult for sequential behavioral changes (i.e., first in mother then in infant) to be observed. Furthermore, the study was not powered for mediation analyses. Clearly, the findings call for more research attention to the impact of maternal generalized anxiety, and possibly other maternal anxiety disorders, on mother–infant interactions.
Remission Status
By evaluating diagnosis at the 10-month assessment, we were able to explore whether remission of maternal disorder influenced the findings. The results indicated that whether mothers had remitted or not did not significantly change the pattern of findings. These data suggest that in the context of the relatively limited procedures used to activate worry/rumination in this study, there exists a continuing potential negative impact in mothers whose diagnostic status has significantly improved over time. The findings are consistent with the research showing that latent cognitive vulnerabilities can be reactivated in individuals whose depression and anxiety has remitted (Joormann & Gotlib, 2007; Lyubomirsky & Nolen-Hoeksema, 1995; Mathews et al., 1990) and with the research showing that infant/child disturbances can persist despite remission of the parent's disorder. Consequently, the current findings suggest a possible cognitive pathway through which remitted status negatively impacts upon mother–infant interactions and child development. However, as there was limited power for these complex moderation analyses, these findings should be interpreted cautiously.
Limitations
The study had a number of limitations. First, for the worry/rumination prime the control participants were requested to concentrate 'on a negative thought' whereas GAD and MDD participants were asked to concentrate on 'their most negative thought.' This slight difference in wording was chosen for the control participants because it was assumed that GAD and MDD mothers would have multiple domains of worry/rumination. On the other hand, control mothers would not have to choose among multiple domains for worry/rumination. Nonetheless, the priming conditions were found to be equally effective across all groups in terms of cognitive ratings, suggesting the slight difference in wording did not have major effects. Second, the priming was quite short and it is possible that a longer prime may have had different effects. Third, the observational periods were relatively brief although similar in length to that used in other comparable experiments (Field, Healy, Goldstein, & Guthertz, 1990). Fourth, during the priming, the infant was looked after by an experimenter, which may have been stressful for some of the infants. However, infants had met the experimenter during the initial warm-up period and thus the experimenter was not a complete stranger. Furthermore, the experimenter was sensitive to the infant's readiness for playing and the way she interacted with the infant depended on the infant's behavior; thus, the interaction was designed to be as stress-free as possible for the infant. Fifth, while the toys for the infants were carefully chosen to be developmentally equivalent pre- and post prime, they were not counter balanced. Sixth, there were relatively high rates of remission in both major depression and generalized anxiety disorder groups from original recruitment at 3 months postnatally to 10 months, leaving a smaller subsample with full disorder at 10 months. Nevertheless, this permitted a test of one of the key questions, that is, whether remitted participants had latent disturbances in their cognitions and whether this impacted on the mother–infant interaction. Seventh, a small proportion of infants approached their mothers during the prime. These brief disturbances did not appear to disrupt the priming but, if they did, they would have had diminished the effect of the prime and if anything minimized differences between WRP and NP as the interruption occurred more commonly in the WRP. Finally, a proportion of the sample was comorbid, and comorbidity may play a role in the observed effects. However, the sample size was insufficient to evaluate the independent contributions of comorbidity to the observed effects.
In conclusion, this study demonstrated that disturbances in maternal cognitions, in the context of postnatal anxiety and depression, play a potentially causal role in the negative effects on mother–child interaction. The results are of note because the worry/rumination prime effects occurred over and above the considerable effects of a neutral condition. These findings suggest that the negative effects on the mother–child interaction may be due to increasing the cognitive load and narrowing maternal focus. Similar effects were evident in remitted participants, although there was limited power for these analyses. Clinically, these findings suggest that treatment efforts may be enhanced by focusing on worry and rumination in mothers with both current and remitted generalized anxiety disorder and major depression. For example, treatment may target ways of disengaging from these cognitions, as has been shown to be effective in samples that are not selected postnatally (Ladouceur et al., 2000; Watkins et al., 2007). Consideration may even be given to such treatments for remitted mothers. Thus, future research may address how well the findings generalize to more naturalistic settings in the home and the development of preventive and therapeutic interventions.
Acknowledgments
We are very grateful to all the mothers and their babies who generously participated in the study. We are grateful to Valerie West who coordinated this work, and to Nicole Jones, Heather Naylor, Lindsay Hague, Flora Carnwath, and the OPP team for their help with data collection. We gratefully acknowledge the help of Peter Cooper, Adriane Arteche, Elizabeth Rapa, Katie Young, Christine Parsons, Clem Turner-Powell and Isabelle Hubbard, and the statistical advice of David Rosenfield. The research was funded by the Wellcome Trust (grant No. 071571).
References
- Alloy L. B., Kelly K. A., Mineka S., & Clements C. M. (1990). Comorbidity of anxiety and depressive disorders: A helplessness-hopelessness perspective. Comorbidity in Anxiety and Mood Disorders, 499–543. [Google Scholar]
- Bender R., & Grouven U. (1997). Ordinal logistic regression in medical research. Journal of the Royal College of Physicians of London, 31, 546–551. [PMC free article] [PubMed] [Google Scholar]
- Borkovec T. D., & Inz J. (1990). The nature of worry in generalized anxiety disorder: A predominance of thought activity. Behaviour Research and Therapy, 28, 153–158. doi:10.1016/0005-7967(90)90027-G [DOI] [PubMed] [Google Scholar]
- Brazelton T. B., Koslowski B., & Main M. (1974). The origins of reciprocity: The early mother–infant interaction. In Lewis M. & Rosenblum L., A. (Eds.), The effect of the infant on its caregiver. New York, NY: Wiley. [Google Scholar]
- Brown T. A., Di Nardo P. A., Lehman C. L., & Campbell L. A. (2001). Reliability of DSM–IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology, 110(1), 49–58. doi:10.1037/0021-843X.110.1.49 [DOI] [PubMed] [Google Scholar]
- Campos J., & Stenberg C. (1981). Perception, appraisal, and emotion: The onset of social referencing. In Lamb M. E. & Sherrod L. R. (Eds.), Infant social cognition. Mahwah, NJ: Erlbaum. [Google Scholar]
- Clark D. M., & Wells A. (1997). Cognitive therapy for anxiety disorders. In Dickstein L., Riba M., & Oldham J. (Eds.), American Psychiatric Press Review of Psychiatry (Vol. 16, pp. 19–43). Washington, DC: American Psychiatric Association. [Google Scholar]
- Cohn J. F., & Tronick E. Z. (1983). Three-month-old infants' reaction to simulated maternal depression. Child Development, 54, 185–193. doi:10.2307/1129876 [PubMed] [Google Scholar]
- Cooper P. J., & Murray L. (1995). Course and recurrence of postnatal depression. Evidence for the specificity of the diagnostic concept. British Journal of Psychiatry, 166, 191–195. doi:10.1192/bjp.166.2.191 [DOI] [PubMed] [Google Scholar]
- Cox J. L., Holden J. M., & Sagovsky R. (1987). Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry, 150, 782–786. doi:10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- Craske M. G., & Hazlett-Stevens H. (2002). Facilitating symptom reduction and behavior change in GAD: The issue of control. Clinical Psychology: Science and Practice, 9, 69–75. doi:10.1093/clipsy.9.1.69 [Google Scholar]
- Craske M. G., Rapee R. M., Jackel L., & Barlow D. H. (1989). Qualitative dimensions of worry in DSM–III–R generalized anxiety disorder subjects and non-anxious controls. Behaviour Research and Therapy, 27, 397–402. doi:10.1016/0005-7967(89)90010-7 [DOI] [PubMed] [Google Scholar]
- Di Nardo P. A., Moras K., Barlow D. H., Rapee R. M., & Brown T. A. (1993). Reliability of DSM–III–R anxiety disorder categories: Using the Anxiety Disorders Interview Schedule–Revised (ADIS–R). Archives of General Psychiatry, 50, 251–256. doi:10.1001/archpsyc.1993.01820160009001 [DOI] [PubMed] [Google Scholar]
- Eysenck M. W., & Calvo M. G. (1992). Anxiety and performance: The processing efficiency theory. Cognition and Emotion, 6, 409–434. doi:10.1080/02699939208409696 [Google Scholar]
- Field T., Healy B., Goldstein S., & Guthertz M. (1990). Behavior-State Matching and Synchrony in Mother Infant Interactions of Nondepressed Versus Depressed Dyads. Developmental Psychology, 26, 7–14. doi:10.1037/0012-1649.26.1.7 [Google Scholar]
- Field T. (1995). Infants of depressed mothers. Infant Behavior & Development, 18, 1–13. doi:10.1016/0163-6383(95)90003-9 [Google Scholar]
- First M. B., Spitzer R. L., Gibbon M., & Williams J. B. W. (2002). Structured Clinical Interview for DSM–IV Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP). New York: Biometrics Research, New York State Psychiatric Institute, 2007. [Google Scholar]
- Ginsburg G. S., Grover R. L., Cord J. J., & Ialongo N. (2006). Observational measures of parenting in anxious and nonanxious mothers: Does type of task matter? Journal of Clinical Child and Adolescent Psychology, 35, 323–328. doi:10.1207/s15374424jccp3502_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman S. H. (2007). Depression in mothers. Annual Review of Clinical Psychology, 3, 107–135. doi:10.1146/annurev.clinpsy.3.022806.091401 [DOI] [PubMed] [Google Scholar]
- Ingram R. E. (1990). Self-focused attention in clinical disorders: Review and a conceptual model. Psychological Bulletin, 107, 156–176. doi:10.1037/0033-2909.107.2.156 [DOI] [PubMed] [Google Scholar]
- Joormann J., & Gotlib I. H. (2007). Selective attention to emotional faces following recovery from depression. Journal of Abnormal Psychology, 116, 80–85. doi:10.1037/0021-843X.116.1.80 [DOI] [PubMed] [Google Scholar]
- Kercher K. (1992). Assessing subjective well-being in the old-old. Research on Aging, 14, 131–168. doi:10.1177/0164027592142001 [Google Scholar]
- Ladouceur R., Dugas M. J., Freeston M. H., Léger E., Gagnon F., & Thibodeau N. (2000). Efficacy of a cognitive-behavioral treatment for generalized anxiety disorder: Evaluation in a controlled clinical trial. Journal of Consulting and Clinical Psychology, 68, 957–964. doi:10.1037/0022-006X.68.6.957 [PubMed] [Google Scholar]
- Landis J. R., & Koch G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33, 159–174. doi:10.2307/2529310 [PubMed] [Google Scholar]
- Lederman S. A., Jones R. L., Caldwell K. L., Rauh V., Sheets S. E., Tang D., . . . Perera F. P. (2008). Relation between cord blood mercury levels and early child development in a World Trade Center cohort. Environmental Health Perspectives, 116, 1085–1091. doi:10.1289/ehp.10831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long J. S. (1997). Regression models for categorical and limited dependent variables. Thousand Oaks, CA; London, United Kingdom: Sage. [Google Scholar]
- Lyubomirsky S., & Nolen-Hoeksema S. (1995). Effects of self-focused rumination on negative thinking and interpersonal problem solving. Journal of Personality and Social Psychology, 69, 176–190. doi:10.1037/0022-3514.69.1.176 [DOI] [PubMed] [Google Scholar]
- Mathews A., May J., Mogg K., & Eysenck M. (1990). Attentional bias in anxiety: Selective search or defective filtering? Journal of Abnormal Psychology, 99, 166–173. doi:10.1037/0021-843X.99.2.166 [DOI] [PubMed] [Google Scholar]
- McLeod B. D., Wood J. J., & Weisz J. R. (2007). Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review, 27, 155–172. doi:10.1016/j.cpr.2006.09.002 [DOI] [PubMed] [Google Scholar]
- Merikangas K. R., Dierker L. C., & Szatmari P. (1998). Psychopathology among offspring of parents with substance abuse and/or anxiety disorders: A high-risk study. Journal of Child Psychology and Psychiatry, 39, 711–720. doi:10.1017/S0021963098002522 [PubMed] [Google Scholar]
- Moore P. S., Whaley S. E., & Sigman M. (2004). Interactions between mothers and children: Impacts of maternal and child anxiety. Journal of Abnormal Psychology, 113, 471–476. doi:10.1037/0021-843X.113.3.471 [DOI] [PubMed] [Google Scholar]
- Mor N., & Winquist J. (2002). Self-focused attention and negative affect: A meta-analysis. Psychological Bulletin, 128, 638–662. doi:10.1037/0033-2909.128.4.638 [DOI] [PubMed] [Google Scholar]
- Murray L., & Carothers A. D. (1990). The validation of the Edinburgh Post-natal Depression Scale on a community sample. British Journal of Psychiatry, 157, 288–290. doi:10.1192/bjp.157.2.288 [DOI] [PubMed] [Google Scholar]
- Murray L., Cooper P., Creswell C., Schofield E., & Sack C. (2007). The effects of maternal social phobia on mother–infant interactions and infant social responsiveness. Journal of Child Psychology and Psychiatry, 48, 45–52. doi:10.1111/j.1469-7610.2006.01657.x [DOI] [PubMed] [Google Scholar]
- Murray L., de Rosnay M., Pearson J., Bergeron C., Schofield E., Royal-Lawson M., & Perera F. P. (2008). Intergenerational transmission of social anxiety: The role of social referencing processes in infancy. Child Development, 79, 1049–1064. doi:10.1111/j.1467-8624.2008.01175.x [DOI] [PubMed] [Google Scholar]
- Murray L., Fiori-Cowley A., Hooper R., & Cooper P. (1996). The impact of postnatal depression and associated adversity on early mother–infant interactions and later infant outcomes. Child Development, 67, 2512–2526. doi:10.2307/1131637 [PubMed] [Google Scholar]
- Murray L., Halligan S. L., & Cooper P. J. (2010). Effects of postnatal depression on mother–infant interactions, and child development In Bremner G. & Wachs T. (Eds.), Handbook of infant development (2nd ed.; Vol. 2, pp. 192–220). Chichester, United Kingdom: Wiley-Blackwell. doi:10.1002/9781444327588.ch8 [Google Scholar]
- Murray L., & Trevarthen C. (1985). Emotional regulation of interactions between two-month-olds and their mothers. In Field T. M. & Fox N. A. (Eds.), Social perception in infants (pp. 177–197). Norwood, NJ: Ablex. [Google Scholar]
- Nadel J., Carchon I., Kervella C., Marcelli D., & Reserbat-Plantey D. (1999). Expectancies for social contingency in 2-month-olds. Developmental Science, 2, 164–173. doi:10.1111/1467-7687.00065 [Google Scholar]
- National Institute of Child Health & Human Development (NICHD), Early Child Care Research Network. (1999). Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. Developmental Psychology, 35, 1297-1310. [DOI] [PubMed] [Google Scholar]
- Newman M. G., Zuellig A. R., Kachin K. E., Constantino M. J., Przeworski A., Erickson T., & Cashman-McGrath L. (2002). Preliminary Reliability and Validity of the Generalized Anxiety Disorder Questionnaire-IV: A Revised Self-Report Diagnostic measure of Generalized Anxiety Disorder. Behavior Therapy, 33, 215–233. doi:10.1016/S0005-7894(02)80026-0 [Google Scholar]
- Nicol-Harper R. J. (2005). An exploration of the impact of maternal preoccupation on mother–infant interaction. Oxford, United Kingdom: Oxford University Press. [Google Scholar]
- Nicol-Harper R., Harvey A. G., & Stein A. (2007). Interactions between mothers and infants: Impact of maternal anxiety. Infant Behavior & Development, 30, 161–167. doi:10.1016/j.infbeh.2006.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. (1991). Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology, 100, 569–582. doi:10.1037/0021-843X.100.4.569 [DOI] [PubMed] [Google Scholar]
- Oathes D. J., Ray W. J., Yamasaki A. S., Borkovec T. D., Castonguay L. G., Newman M. G., & Nitschke J. B. (2008). Worry, generalized anxiety disorder, and emotion: Evidence from the EEG gamma band. Biological Psychology, 79, 165–170. doi:10.1016/j.biopsycho.2008.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxford Parent Project (OPP). (2008). Department of Psychiatry. Oxford University. Oxford. [Google Scholar]
- Patel P., Wheatcroft R., Park R. J., & Stein A. (2002). The children of mothers with eating disorders. Clinical Child and Family Psychology Review, 5, 1–19. doi:10.1023/A:1014524207660 [DOI] [PubMed] [Google Scholar]
- Plomin R., DeFries J. C., Craig I. W., & McGuffin P. (Eds.). (2003). Behavioral genetics in the postgenomic era. Washington, DC: American Psychological Association. doi:10.1037/10480-000 [Google Scholar]
- Roemer L., & Borkovec T. D. (1993). Worry: Unwanted cognitive activity that controls unwanted somatic experience. In Wegner D. M. & Pennebaker J. W. (Eds.), Handbook of mental control. (pp. 220–238). Englewood Cliffs, NJ: Prentice Hall. [Google Scholar]
- Rutter M. (1990). Commentary: Some Focus and Process Considerations Regarding Effects of Parental Depression on Children. Developmental Psychology, 26, 60–67. doi:10.1037/h0092669 [Google Scholar]
- Sarason I. G., Sarason B. R., Keefe D. E., Hayes B. E., & Shearin E. N. (1986). Cognitive interference: Situational determinants and trait-like characteristics. Journal of Personality and Social Psychology, 51, 215–226. doi:10.1037/0022-3514.51.1.215 [Google Scholar]
- Segerstrom S. C., Tsao J. C. I., Alden L. E., & Craske M. G. (2000). Worry and rumination: Repetitive thought as a concomitant and predictor of negative mood. Cognitive Therapy and Research, 24, 671–688. doi:10.1023/A:1005587311498 [Google Scholar]
- Singer A. R., & Dobson K. S. (2007). An experimental investigation of the cognitive vulnerability to depression. Behaviour Research and Therapy, 45, 563–575. doi:10.1016/j.brat.2006.05.007 [DOI] [PubMed] [Google Scholar]
- Startup H. M., & Davey G. C. L. (2001). Mood as input and catastrophic worrying. Journal of Abnormal Psychology, 110, 83–96. doi:10.1037/0021-843X.110.1.83 [DOI] [PubMed] [Google Scholar]
- Stein A., Lehtonen A., Harvey A. G., Nicol-Harper R., & Craske M. (2009). The influence of postnatal psychiatric disorder on child development. Is maternal preoccupation one of the key underlying processes? Psychopathology, 42, 11–21. doi:10.1159/000173699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein A., Ramchandani P., & Murray L. (2008). Impact of parental psychiatric disorder or physical illness. In Rutter M., Bishop D. V., Pine D., Scott S., Stevenson J., Taylor E. & Thapar A. (Eds.), Rutter's Child and Adolescent Psychiatry (pp. 407–420). Oxford, United Kingdom: Blackwell. doi:10.1002/9781444300895.ch27 [Google Scholar]
- Stein A., Woolley H., Cooper S. D., & Fairburn C. G. (1994). An observational study of mothers with eating disorders and their infants. Journal of Child Psychology and Psychiatry, 35, 733–748. doi:10.1111/j.1469-7610.1994.tb01218.x [DOI] [PubMed] [Google Scholar]
- Stice E., Agras W. S., & Hammer L. D. (1999). Risk factors for the emergence of childhood eating disturbances: A five-year prospective study. International Journal of Eating Disorders, 25, 375–387. doi:10.1002/(SICI)1098-108X(199905)25:4<375::AID-EAT2>3.0.CO;2-K [DOI] [PubMed] [Google Scholar]
- Striano T., & Stahl D. (2005). Sensitivity to triadic attention in early infancy. Developmental Science, 8, 333–343. doi:10.1111/j.1467-7687.2005.00421.x [DOI] [PubMed] [Google Scholar]
- Trevarthen C. (1979). Communication and cooperation in early infancy: A description of primary intersubjectivity. In Bullowa M. (Ed.), Before speech: The beginning of interpersonal communication (pp. 321–348). Cambridge, United Kingdom: Cambridge University Press. [Google Scholar]
- Watkins E., Scott J., Wingrove J., Rimes K., Bathurst N., Steiner H., . . . Malliaris Y. (2007). Rumination-focused cognitive behaviour therapy for residual depression: A case series. Behaviour Research and Therapy, 45, 2144–2154. doi:10.1016/j.brat.2006.09.018 [DOI] [PubMed] [Google Scholar]
- Watson D., Clark L. A., & Tellegen A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. doi:10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Williams J. M. G., Watts F. N., MacLeod C., & Mathews A. (1997). Cognitive psychology and emotional disorders. Chichester, United Kingdom: Wiley. [Google Scholar]
- Wood J. J., McLeod B. D., Sigman M., Hwang W. C., & Chu B. C. (2003). Parenting and childhood anxiety: Theory, empirical findings, and future directions. Journal of Child Psychology and Psychiatry, 44, 134–151. doi:10.1111/1469-7610.00106 [DOI] [PubMed] [Google Scholar]