Spasticity is a common complication after an upper motor neuron lesion and can involve a single or multiple muscle groups. When spasticity involves muscles around the foot, the typical pattern is ankle plantar flexed and inverted and toes flexed and adducted, giving rise to equinovarus deformity [1]. This pattern occurs due to the involvement of several muscles working in combination. Spasticity of the gastrocnemius, soleus and toe flexor muscles causes the ankle to plantarflex while the posterior tibialis muscle adds to the inward turn of the foot [2, 3].
Spasticity can also occur in a single muscle in the foot, for example spasticity of the extensor hallucis longus (EHL), also known as hitchhiker's toe. This condition, albeit focal, occasionally causes pain and discomfort and is worth treating. However, spasticity involving a single muscle group such as the ankle dorsiflexors is rare and the complications are unknown. We report on a patient diagnosed with transverse myelitis presenting an unusual pattern of lower limb spasticity involving unilateral ankle dorsiflexor muscles. The spasticity resulted in foot deformity and difficulty wearing shoes, impairing gait, causing discomfort and generating disabili ties in activities of daily living (ADL).
The patient is a 59-year-old woman diagnosed with transverse myelitis following symptoms of acute lower limb weakness and incontinent bladder and bowel. The patient's initial clinical findings revealed flaccid tone and areflexia with Medical Research Council (MRC) grade 0/5 motor power in both of the lower limbs. Both upper limbs were intact neurologically. Pin prick sensation was impaired bilaterally from spinal level T8 downwards. Magnetic resonance imaging of the spinal cord disclosed a hyperintense area from the level of T9 vertebra to the conus medullaris. She was treated with 1 g of intravenous (IV) methylprednisolone for 5 days and three courses of intravenous immunoglobulin.
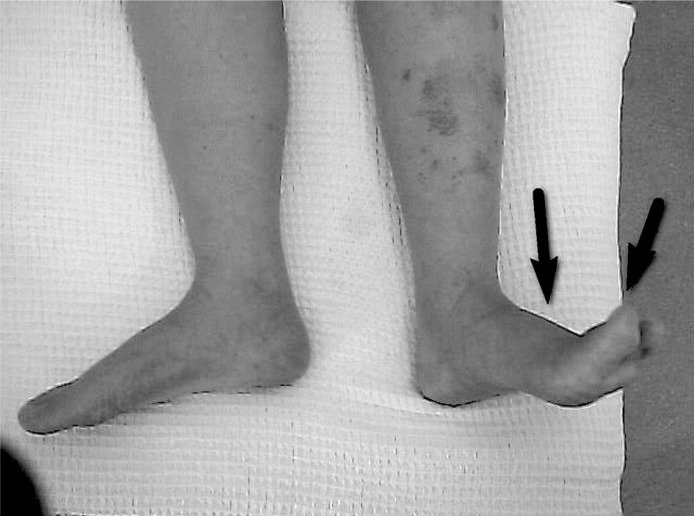
The patient's neurological impairments improved gradually after treatment. At 18 months, her right lower limb tone was normal with MRC grade 4/5 power. Her left lower limb tone was flaccid proximally. Distally, there was increased tone with ankle dorsiflexors showing Modified Ashworth Scale (MAS) grade 2 spasticity and toe extensors with MAS grade 3 spasticity (Figure 1). Her hip flexion had MRC grade 3/5, knee flexion and extension had MRC grade 2/5, whereas ankle dorsiflexion and plantarflexion had MRC grade 1/5. Pin prick sensation improved markedly with only impairment over bilateral lower legs remaining. Functionally, she was able to stand and walk therapeutically using a walking frame.
Figure 1.
Anterior view of lower limbs showing left foot ankle dorsiflexion and toes hyperextension
The patient complained that her left foot and toes spontaneously hyperextended when she tried to move her left leg. This became more prominent when she was standing. As a result, she had difficulties balancing herself standing and had to bear weight on her left heel during the stance phase of walking. With her foot and toes hyperextended, she was only able to take ten steps before complaining of tiredness and severe discomfort on her left heel. She had to sit on a wheelchair to perform ADL that require standing. She also had difficulty performing lower body dressing because the hyperextended foot got in the way when she tried to put on her pants. She was also unable to put on her shoes due to the foot deformity. These complications caused severe disabilities and impaired her independence.
The patient was treated with intramuscular injections of botulinum toxin type A (BTX-A) to the left tibialis anterior, EHL and extensor digitorum longus (EDL) under electromyography guidance followed by a programme of intensive stretching and strengthening exercises. The BTX-A dosages given were 50, 25 and 25 units to each muscle respectively without any complications. One month post-injection, the spasticity decreased a half grade for ankle dorsiflexors (MAS grade 1 + ) and one grade for toe extensors (MAS grade 2) when examined at rest. When assessed during standing and walking, her spasticity decreased significantly with the left foot achieving plantigrade position. Performing lower body dressing was not as cumbersome as before and she could wear shoes comfortably.
Spasticity is a common complication following spinal cord lesions from traumatic and non-traumatic aetiologies with reported prevalence between 27% and 36% [4, 5]. It normally affects both lower limbs although the clinical patterns of spasticity are more varied in cases of incomplete lesions or incomplete recovery. In our case, the patient developed an uncommon pattern of ankle spasticity: a focal spasticity of unilateral ankle dorsiflexor muscles (tibialis anterior, EHL and EDL) following incomplete recovery of acute transverse myelitis.
Problems have been encountered in patients with ankle spasticity affecting other muscles around the foot such as ankle plantar flexors, invertors or EHL alone [2, 3, 6]. In this case, the ankle dorsiflexor spasticity was causing problems for the patient. Not only did it affect the standing balance, it also reduced her walking tolerance and distance. The discomfort experienced was so severe that it caused her to compensate using a wheelchair to perform certain ADL. Treatment with BTX-A to the ankle dorsiflexors was useful to correct the abnormal foot posture, and thus achieved improved function.
Despite the occurrence of disabling ankle spasticity, the patient has shown a marked overall recovery in sensory and motor power following treatment with IV methylprednisolone. Controlled studies of acute myelitis treatment are lacking but current expert consensus favours acute treatment with high-dose corticosteroids for a better outcome as observed in this case [7]. In cases with incomplete myelitis and refractory to steroid therapy, treatable causes such as bacterial infection should be suspected to facilitate appropriate treatments [8].
Spasticity is a common complication after transverse myelitis. However, involvement of unilateral ankle dorsiflexors is uncommon, so its effect on daily function is unknown. The treatment decision to use BTX-A injection relies partly on the pattern of muscle involvement, the spasticity severity and whether it causes problems or offers benefits to patients [9]. BTX-A injection targeting the specific muscles has been reported to reduce spasticity and improve the patient's functional outcome [6, 10], which is also relevant in this case even though the spasticity presented is uncommon.
References
- 1.Davies PM. Typical patterns of spasticity or hypertonicity. In: Davies PM, editor. Steps to follow: the comprehensive treatment of patients with hemiplegia. 2nd ed. Berlin: Springer; 2000. pp. 63–4. [Google Scholar]
- 2.Lamontagne A, Richards CL, Dumas F, Tardif D, Comeau F. Larger contribution of passive stiffness to ankle plantarflexor moment during gait after stroke. Soc Neurosci. 1997;23:769. doi: 10.1016/s0003-9993(00)90083-2. [DOI] [PubMed] [Google Scholar]
- 3.Lamontagne A, Malouin F, Richards CL. Locomotor-specific measure of spasticity of plantarflexor muscles after stroke. Arch Phys Med Rehabil. 2001;82:1696–704. doi: 10.1053/apmr.2001.26810. [DOI] [PubMed] [Google Scholar]
- 4.Joseph LH, Ismail OH, Naicker AS, Ying PP, Mohammad AR. Three-year study of spinal cord injury outcomes and related secondary complications in a tertiary centre – a retrospective analysis. Arch Med Sci. 2009;5:190–4. [Google Scholar]
- 5.Gupta A, Taly AB, Srivastava A, Murali T. Non-traumatic spinal cord lesions: epidemiology, complications, neurological and functional outcome of rehabilitation. Spinal Cord. 2009;47:307–11. doi: 10.1038/sc.2008.123. [DOI] [PubMed] [Google Scholar]
- 6.Yelnik AP, Colle FM, Bonan IV, Lamotte DR. Disabling overactivity of the extensor hallucis longus after stroke: clinical expression and efficacy of botulinum toxin type A. Arch Phys Med Rehabil. 2003;84:147–9. doi: 10.1053/apmr.2003.50077. [DOI] [PubMed] [Google Scholar]
- 7.Schmalstieg WF, Weinshenker BG. Approach to acute or subacute myelopathy. Neurology. 2010;75(18 Suppl):S2–8. doi: 10.1212/WNL.0b013e3181fb3638. [DOI] [PubMed] [Google Scholar]
- 8.Feng Y, Guo N, Liu J, et al. Mycobacteria infection in incomplete transverse myelitis is refractory to steroids: a pilot study. Clin Dev Immuno. 2011;2011:501369. doi: 10.1155/2011/501369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gormley ME, Jr, O'Brien CF, Yablon SA. A clinical overview of treatment decisions in the management of spasticity. Muscle Nerve Suppl. 1997;6:S14–20. [PubMed] [Google Scholar]
- 10.Dengler R, Neyer U, Wohlfarth K, Bettig U, Janzik HH. Local botulinum toxin in the treatment of spastic drop foot. J Neurology. 1992;239:375–8. doi: 10.1007/BF00812153. [DOI] [PubMed] [Google Scholar]