Abstract
Introduction
During the last two decades, obesity has proved to be one of the most important problems of public health, and it is considerably more frequent in developed countries, not only in adults, but in children, too. The aim of the current study is to evaluate the prevalence of overweight and obesity in children.
Material and methods
Two thousand three hundred and seventy-four pupils in primary education were considered for the study (1206 boys and 1168 girls).
Results
In the population-based study, the proportion of overweight children was 23.9%, of obese children 7.3%, and of those with central obesity 35.5%. The boys were obese in a higher percentage than the girls (9.2% vs. 5.3%, p < 0.05). The obesity rates were gradually reduced as the children were growing older. The nutritional habits which were identified to have a positive association with obesity were the following: skipping breakfast, not consuming fruits and vegetables, and consuming bread and soft drinks. Children's healthy nutrition in school was related to lower rates of generalised and central obesity, while the hours spent watching TV were positively associated with all types of obesity.
Conclusions
Results from the study suggest that a high proportion of children are overweight or obese. Therefore, it is important to adhere to a healthy lifestyle which emphasizes healthy food choices and habits, regular physical activity, and limiting screen time.
Keywords: childhood obesity, central obesity, prevalence, nutrition, eating behaviour, physical activity
Introduction
Obesity is a multifactorial condition characterized by abnormal or excessive body fat accumulation. The aetiology of obesity includes genetic, metabolic and environmental factors [1]. Obesity appears mainly when the intake of calories is higher than the calories consumed (positive energy balance) [2]. During the last two decades, obesity has emerged as a leading public health problem; it is more prevalent in developed countries, affecting adults and children alike [3–6].
In particular, childhood obesity increases the likelihood of several consequences for a child (precocious puberty, gynecomastia, polycystic ovary syndrome, diabetes mellitus type 2, hypertension, etc) [6–11] and also later in adulthood (increased mortality due to cardiovascular disease, diabetes mellitus, colorectal cancer, etc.) [11, 12]. Obese children and adolescents have a higher probability of remaining obese later as adults [13]. Studies in Greek urban and rural areas showed higher scores for childhood obesity indicators (body mass index (BMI), waist-to-hip ratio, cutaneous wrinkles); compared to other countries, Greece is closer to those countries with higher percentages of childhood obesity (36% boys, 16% girls) [14–18].
Emphasis has been given lately to the type of obesity, as perivisceral fat accumulation is related not only to diabetes type 2, but to increased cardiovascular risk for adults and children as well [19–21]. Sex-related central obesity is diagnosed by the patient's waist circumference (according to the International Diabetes Federation (IDF) and Adult Treatment Panel III (ATP III)) and the waist-to-hip ratio [22]. Body mass index is a measure of obesity for adults and children [23]. However, BMI depends on age and it may give incorrect results, as is the case with children with increased muscle or osteal mass who have been mistakenly assessed as overweight or obese [24, 25].
The International Obesity Task Force (IOTF) linked the child BMI-sex-age percentiles with the adult-defined classes of overweight and obesity; thus, a BMI-sex-age percentile higher than the 85th percentile accords with the adult definition of overweight, while the 95th percentile or higher accords with the adult definition of obesity [26, 27]. By Cole's LMS method (L: the power in the Box-Cox transformation, M: the median, S: the coefficient of variation), curves drawn in a 2000 study were linked to the 95th and 85th percentile, corresponding to BMI 25.0 kg/m2 and 30.0 kg/m2 at age 18 years [28].
The main reasons for this soaring childhood obesity epidemic are excessive intake of fat- and sugar-rich foods, low fibre intake, larger portions of food, and low physical activity levels, especially in developed countries [14, 17].
The objectives of this study were (a) to investigate the prevalence of overweight and obesity among Greek students, and (b) to determine the correlation between eating habits and physical activity among Greek students aged 6-12 years.
Material and methods
From 2009 to 2010, a sample of 2374 students (1206 males, 1168 females) 6 to 12 years old participated in our study. This cross-sectional study was based on a convenience sample of primary school students. In order for the schools to allow the distribution of questionnaires, our research protocol had to be first approved by the Pedagogical Institute.
Questionnaires
The questionnaire was drawn up by the researchers. It included an introduction about the research and its objectives, a parental consent form for participation in the study, body measurements of the students, parents’ education level and 37 questions about eating habits and physical activity levels of the students. The questions regarding eating habits and physical activity were based on the Child Feeding Questionnaire (CFQ) [29].
Closed format questions in the form of multiple-choice questions were given and the students had to circle their preferred answer. In questions regarding how often the students eat specifically Mediterranean-type foods, they had to give specific answers on lunch and dinner consumed during a week. The questionnaire was distributed to each student individually; each student's body measurements were taken by the researchers. The well-known BMI formula was used with reference to age-adjusted BMI charts by employing Cole's LMS method [28]. Parental consent forms were sent to all parents. Out of 2650 mailed forms, 2374 were returned and signed. Unsigned forms were not accepted. The parents’ response rate was 89.5% (n = 2374). Two successive pilot studies of 50 students each followed, which allowed some minor adjustments to the questionnaire to be made. Students, parents and schools were assured anonymity. No personal data were collected or used.
Research ethics
All parents were mailed informed consent forms for the participation of children in the study. More specifically, 2650 consent forms were mailed and 2374 of them were returned signed by the parents. Children who did not return those forms signed by their parents were excluded from the study. The parents’ response rate was 89.5% (n = 2374).
Students, parents and schools were assured anonymity. No personal data were collected or used. The students could also opt out of the study at any point in time.
Statistical analysis
Statistical analyses were performed using SPSS version 15.0 (SPSS Chicago, IL USA). A p-value < 0.05 was accepted for statistical significance. The Bonferroni correction was used to correct type I errors, because of multiple comparisons, for which the level of significance was 0.05/k (k = number of comparisons). Parametric analysis and data dissemination (ANOVA) were employed for the comparison of students’ knowledge levels (as a quantitative variable) between three or more different groups; Student's t-test was used for the comparison of total scores between the two groups. Reliability and internal cohesion according to Cronbach's α was α = 0.76.
Results
In the results the total number of students was included (males n = 1206, females n = 1168). The families’ socioeconomic status showed that most of the parents were middle-class high-school graduates. As far as the students were concerned, BMI measurements showed that 68.8% of the children had an average BMI, 23.9% were classified as overweight, and 7.3% were classified as obese (p < 0.05).
Cross-correlation between overweight and obese children and sex showed that more males (9.2%) were obese than females (5.3%) (p < 0.05) (Table I). Moreover, cross-correlation between central obesity and sex showed that males slightly outnumbered females, but this was not a statistically significant difference (p = 0.48) (Table I). The distribution of BMI scores (Table III) showed that the majority of the subjects had an average BMI (68.8%), and overweight participants outnumbered obese participants (p < 0.05).
Table I.
Distribution of overweight, obesity and central obesity of children according to sex
| n | Overweight [%] | Obesity [%] | Central obesity [%] | |
|---|---|---|---|---|
| p = 0.05 | p = 0.05 | p = 0.48 | ||
| Total | 2374 | 23.9 (n = 567) | 7.3 (n = 173) | 35.5 (n = 840) |
| Boys | 1206 | 26.4 (n = 318) | 9.2 (n = 110) | 36.6 (n = 441) |
| Girls | 1168 | 21.3 (n = 249) | 5.3 (n = 63) | 34.3 (n = 399) |
Table III.
Cross-correlation of daily follow-up of television and obesity
| Not active | 1 h/day | > 3 h/day | Value of p | |
|---|---|---|---|---|
| Overweight | 27.3% | 28.9% | 26.1% | < 0.01 |
| Obesity | 4.1% | 7.8% | 8.6% | < 0.01 |
In our study, obesity appears to decrease with age. In fact, in the 6-9 year group the obesity percentage was 10.3%, while in the 10-12 year group the percentage was 3.3% (p < 0.001). This striking discrepancy between the two age groups shows a positive correlation with the increase of physical activity levels; more specifically, in the 6-9 year group cross-correlation reaches 60.3%, and in the 10-12 year group it is 68.6% (p < 0.05) (Table II).
Table II.
Distribution of age and obesity according to physical activity after school
| Age [years] | Obesity [%] | Value of p | Physical activity [%] | Physical activity total [%] | Value of p | |
|---|---|---|---|---|---|---|
| 6-9 | 10.3 | < 0.001 | > 2 h* | 39.7 | 60.3 | < 0.05 |
| 2-3 h** | 40.1 | |||||
| 3-5 h** | 17.5 | |||||
| < 5 h*** | 2.7 | |||||
| 10-12 | 3.3 | < 0.001 | > 2 h | 31.4 | 68.6 | < 0.05 |
| 2-3 h | 43.3 | |||||
| 3-5 h | 22.1 | |||||
| < 5 h | 3.2 | |||||
Physical activity in school
participation in sport
systematic participation in sport
Nevertheless, a parallel reduction of central obesity percentages does not seem to exist. More specifically, central obesity prevalence between the two age groups (6-9 years and 10-12 years) shows no statistically significant difference (33.5% vs. 33.7%, p = 0.18).
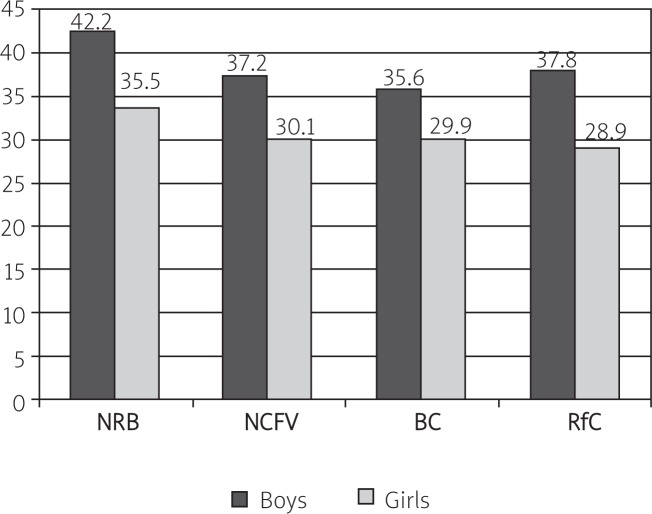
Some eating habits that positively cross-correlated with obesity, as shown in Figure 1 (p < 0.05), were avoiding breakfast, not consuming fruits and vegetables, and avid consumption of white bread and cola-type beverages. Cross-correlation between these eating habits and sex showed that males are more prone to erroneous eating habits than girls.
Figure 1.
Distribution of alimentary habits and sex
NRB – not receiving breakfast, NCFV – not consuming fruits and vegetables, BC – consumption of bread, RfC – consumption of refreshments
Fast food consumption is connected to central obesity, as shown in Table I. Only 25% of children who did not eat fast (junk) food had central obesity, 33% of children with abdominal obesity consumed fast food once a week, and 42% of children having central obesity were found to consume fast food more than twice a week (p < 0.05).
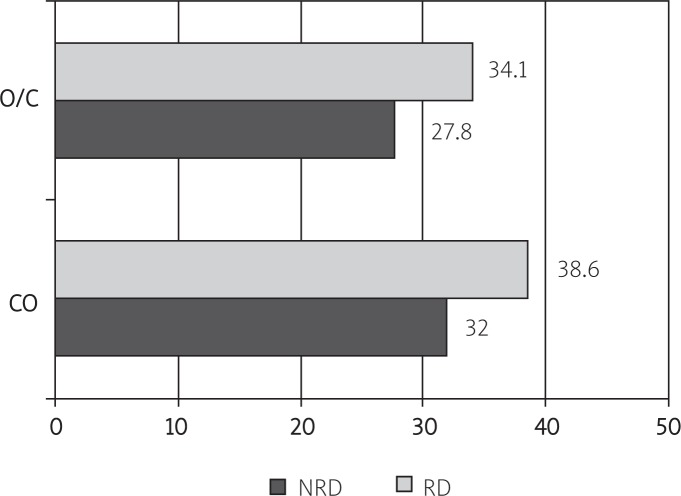
Regarding eating habits of children in school, it appears that children who were used to a healthy diet had lower percentages of general and central obesity, as shown in Figure 2 (p < 0.05). Regarding children who did not follow a healthy diet in school, 34.1% of them were overweight or obese and 38.6% had central obesity; 32% of the children who had a healthy diet in school were overweight or obese, and 27.8% of them had central obesity (p < 0.05).
Figure 2.
Cross-correlation of alimentary habits in the school environment and obesity
NRD – not right diet, RD – right diet, O/C – overweight/corpulent, CO – central obesity
Moreover, this study found a significant increase of obesity percentage (p < 0.01) and central obesity frequency (p < 0.05), depending on hours of daily TV watching and spending too much time in front of the computer. On the other hand, the percentage of overweight children, as shown in Table III, does not increase significantly regardless of the time spent in front of the computer and television (p < 0.01).
Discussion
The present study examined the prevalence of overweight and obesity among elementary school students (6-12 years old). The percentage of overweight or obese children is high, males outnumbering females in all age groups. A significant positive cross-correlation was found among the students’ BMI and frequent consumption of fast food, as well as time spent in front of the computer and television.
It appears that about 1/3 of the students (boys and girls) who participated in the study were found to be overweight and/or obese, a result which is in accordance with other international and Greek studies [30–36]. Central obesity does not present a statistically significant difference among males and females, and it does not seem to have a statistically significant difference when physical activity levels are increased. Several researchers have proposed that BMI and waist circumference are sufficient indicators for the evaluation of children's obesity, and can also be used to predict risk factors for the child's health [37, 38].
Comparative studies in 2002 and afterwards report higher rates of obesity and overweight in boys and significantly lower levels in girls, mainly in urban areas [39–42].
Several studies report a change of eating habits and a 7-11% increase of calorie intake in the last two decades. This change appears to be a result of higher consumption of carbohydrates, fat and added sweeteners [43, 44]. Increased consumption of fast food, which results in high calorie intake, has also been established by many researchers. It has been reported that between 1977 and 1996 there was an increase of 30% in fast food consumption in US children between 2 and 5 years old (2004), while family expenses for fast food between 1992 and 2002 were doubled, and pizza and fast food restaurants were found to be the most popular places for dining in Australia (2003, 2005) [45]. Increased adult obesity rates have been connected to long hours of wa tching TV, but no causative relationship has been established between those two factors [46, 47]. Long hours of television watching can decrease the time for physical activities and it seems that there is a positive cross-correlation between time spent in front of the TV and percentages of overweight or obese children [17, 48].
Many agencies and non-profit organizations in several countries have required some restrictions, or even a ban, on junk food advertisements on television – especially advertisements aimed at children younger than 12 years [49, 50]. The food industry, on the other hand, considers that there is some relation between childhood obesity and watching television, but food advertising has nothing to do with obesity. Other researchers focus on high calorie intake and not on hours watching television [44].
In conclusion, the percentage of children found to be overweight or obese is high, males outnumbering females in all age groups. Childhood obesity, and in particular central obesity, is significantly correlated with eating habits. Breakfast avoidance, lack of fruits and vegetables and increased consumption of white bread and cola-type beverages are arguably some habits leading to obesity. A significant positive cross-correlation was observed between the students’ BMI and frequent consumption of fast food, as well as spending excessive time watching television, but that was not the case as far as computer and videogames were concerned.
It is considered that the students’ adjustment towards better eating habits is of vital importance, as well as increased physical activity; such behavioural adjustments are achievable through expert support with well-organized and targeted educational school and governmental programmes, in order to educate all population groups. Extensive professional interventions targeting health promotion, in accordance with current health policies, are of supreme importance.
References
- 1.Woods SC, Seeley RJ. Understanding the physiology of obesity: review of recent developments in obesity research. Int J Obes Relat Metab Disord. 2002;26(Suppl 4):S8–10. doi: 10.1038/sj.ijo.0802211. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord. 1998;22:39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- 3.Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology, and demographics. Pediatrics. 1998;101:497–504. [PubMed] [Google Scholar]
- 4.Chinn S, Hughes JM, Rona RJ. Trends in growth and obesity in ethnic groups in Britain. Arch Dis Child. 1998;78:513–7. doi: 10.1136/adc.78.6.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hanley AJ, Harris SB, Gittelsohn J, Wolever TM, Saksvig B, Zinman B. Overweight among children and adolescents in a Native Canadian community: prevalence and associated factors. Am J Clin Nutr. 2000;71:693–700. doi: 10.1093/ajcn/71.3.693. [DOI] [PubMed] [Google Scholar]
- 6.Sinha R, Fisch G, Teague B, et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Eng J Med. 2002;346:802–10. doi: 10.1056/NEJMoa012578. [DOI] [PubMed] [Google Scholar]
- 7.Figueroa-Muñoz JI, Chinn S, Rona RJ. Association between obesity and asthma in 4-11 year old children in the UK. Thorax. 2001;56:133–7. doi: 10.1136/thorax.56.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strauss RS, Barlow SE, Dietz WH. Prevalence of abnormal serum aminotransferase values in overweight and obese adolescents. J Pediatr. 2000;136:727–33. [PubMed] [Google Scholar]
- 9.Adelman RD, Restaino IG, Alon US, Blowey DL. Proteinuria and focal segmental glomerulosclerosis in severely obese adolescents. J Pediatr. 2001;138:481–5. doi: 10.1067/mpd.2001.113006. [DOI] [PubMed] [Google Scholar]
- 10.Goulding A, Jones IE, Taylor RW, Williams SM, Manning PJ. Bone mineral density and body composition in boys with distal forearm fractures: a dual-energy X-ray absorptiometry study. J Pediatr. 2001;139:509–15. doi: 10.1067/mpd.2001.116297. [DOI] [PubMed] [Google Scholar]
- 11.Gunnell DJ, Frankel SJ, Nanchahal K, Peters TJ, Davey Smith G. Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort. Am J Clin Nutr. 1998;67:1111–8. doi: 10.1093/ajcn/67.6.1111. [DOI] [PubMed] [Google Scholar]
- 12.Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH. Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1922 to 1935. N Eng J Med. 1992;327:1350–5. doi: 10.1056/NEJM199211053271904. [DOI] [PubMed] [Google Scholar]
- 13.Dietz WH. Childhood weight affects adult morbidity and mortality. J Nutr. 1998;128(2 Suppl):411S–4. doi: 10.1093/jn/128.2.411S. [DOI] [PubMed] [Google Scholar]
- 14.Kapantais E, Tzotzas T, Ioannidis I, et al. First national epidemiological survey on the prevalence of obesity and abdominal fat distribution in Greek adults. Ann Nutr Metab. 2006;50:330–8. doi: 10.1159/000094296. [DOI] [PubMed] [Google Scholar]
- 15.Mamalakis G, Kafatos A, Manios Y, Anagnostopoulou T, Apostolaki I. Obesity indices in a cohort of primary school children in Crete: a six year prospective study. Int J Obes Relat Metab Disord. 2000;24:765–71. doi: 10.1038/sj.ijo.0801223. [DOI] [PubMed] [Google Scholar]
- 16.Panagiotakos DB, Pitsavos C, Chrysohoou C, et al. Epidemiology of overweight and obesity in a Greek adult population: the ATTICA Study. Obes Res. 2004;12:1914–20. doi: 10.1038/oby.2004.239. [DOI] [PubMed] [Google Scholar]
- 17.Sothern MS. Obesity prevention in children: physical activity and nutrition. Nutrition. 2004;20:704–8. doi: 10.1016/j.nut.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 18.Decoda Study Group. Nyamdorj R, Qiao Q, et al. BMI compared with central obesity indicators in relation to diabetes and hypertension in Asians. Obesity. 2008;16:1622–35. doi: 10.1038/oby.2008.73. [DOI] [PubMed] [Google Scholar]
- 19.Miles JM, Jensen MD. Counterpoint: visceral adiposity is not causally related to insulin resistance. Diabetes Care. 2005;28:2326–8. doi: 10.2337/diacare.28.9.2326. [DOI] [PubMed] [Google Scholar]
- 20.Pi-Sunyer FX. The relation of adipose tissue to cardiometabolic risk. Clin Cornerstone. 2006;8(Suppl 4):S14–23. doi: 10.1016/s1098-3597(06)80040-2. [DOI] [PubMed] [Google Scholar]
- 21.Janssen I, Katzmarzyk PT, Ross R. Body mass index, waist circumference, and health risk: evidence in support of current National Institutes of Health guidelines. Arch Intern Med. 2002;162:2074–9. doi: 10.1001/archinte.162.18.2074. [DOI] [PubMed] [Google Scholar]
- 22.Alberti KG, Zimmet P, Shaw J. The metabolic syndrome – a new worldwide definition. Lancet. 2005;366:1059–62. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 23.Dietz WH, Bellizzi MC. Introduction: the use of body mass index to assess obesity in children. Am J Clin Nutr. 1999;70:123S–5S. doi: 10.1093/ajcn/70.1.123s. [DOI] [PubMed] [Google Scholar]
- 24.Charney E. Childhood obesity: the measurable and the meaningful. J Pediatr. 1998;132:193–5. doi: 10.1016/s0022-3476(98)70427-5. [DOI] [PubMed] [Google Scholar]
- 25.Malina RM, Katzmarzyk PT. Validity of the body mass index as an indicator of the risk and presence of overweight in adolescents. Am J Clin Nutr. 1999;70:131S–6S. doi: 10.1093/ajcn/70.1.131s. [DOI] [PubMed] [Google Scholar]
- 26.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291:2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 27.de Onis M, Habicht JP. Anthropometric reference data for international use: recommendations from a World Health Organization Expert Committee. Am J Clin Nutr. 1996;64:650–8. doi: 10.1093/ajcn/64.4.650. [DOI] [PubMed] [Google Scholar]
- 28.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36:201–10. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- 30.Canning PM, Courage ML, Frizzell LM. Prevalence of overweight and obesity in a provincial population of Canadian preschool children. CMAJ. 2004;171:240–2. doi: 10.1503/cmaj.1040075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elgar FJ, Roberts C, Moore L, Tudor-Smith C. Sedentary behaviour, physical activity and weight problems in adolescents in Wales. Public Health. 2005;119:518–24. doi: 10.1016/j.puhe.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 32.Wang Y. Diet. Physical activity, childhood obesity and risk of cardiovascular disease. Inter Cong Ser. 2004;1262:176–9. [Google Scholar]
- 33.Whitlock EP, Williams SB, Gold R, Smith PR, Shipman SA. Screening and interventions for childhood overweight: a summary of evidence for the US Preventive Services Task Force. Pediatrics. 2005;116:e125–44. doi: 10.1542/peds.2005-0242. [DOI] [PubMed] [Google Scholar]
- 34.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity. 2008;16:2323–30. doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]
- 35.Snethen JA, Broome ME, Cashin SE. Effective weight loss for overweight children: a meta-analysis of intervention studies. J Pediatr Nurs. 2006;21:45–56. doi: 10.1016/j.pedn.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 36.Papandreou D, Stamou M, Malindretos P, Rousso I, Mavromichalis I. Prevalence of hypertension and association of dietary mineral intake with blood pressure in healthy schoolchildren from northern Greece aged 7-15 years. Ann Nutr Metab. 2007;51:471–6. doi: 10.1159/000111169. [DOI] [PubMed] [Google Scholar]
- 37.Mc Carthy HD. Body fat measurements in children as predictors for the metabolic syndrome: focus on waist circumference. Proc Nutr Soc. 2006;65:385–92. doi: 10.1017/s0029665106005143. [DOI] [PubMed] [Google Scholar]
- 38.Aeberli I, Ammann RS, Knabenhans M, Molinari L, Zimmermann MB. Decrease in the prevalence of paediatric adiposity in Switzerland from 2002 to 2007. Public Health Nutr. 2010;13:806–11. doi: 10.1017/S1368980009991558. [DOI] [PubMed] [Google Scholar]
- 39.Demerath E, Muratova V, Spangler E, Li J, Minor VE, Neal WA. School-based obesity screening in rural Appalachia. Prev Med. 2003;37:553–60. doi: 10.1016/j.ypmed.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 40.Liu J, Bennett KJ, Harun N, Probst JC. Urban-rural differences in overweight status and physical inactivity among US children aged 10-17 years. J Rural Health. 2008;24:407–15. doi: 10.1111/j.1748-0361.2008.00188.x. [DOI] [PubMed] [Google Scholar]
- 41.Smith DT, Vendela MJ, Bartee RT, Carr LJ. Body mass index in rural first grade schoolchildren: progressive increase in boys. J Rural Health. 2008;24:40–8. doi: 10.1111/j.1748-0361.2008.00135.x. [DOI] [PubMed] [Google Scholar]
- 42.Montgomery-Reagan K, Bianco JA, Heh V, Rettos J, Huston RS. Prevalence and correlates of high body mass index in rural Appalachian children aged 6-11 years. Rural Remote Health. 2009;9:1234. [PubMed] [Google Scholar]
- 43.Somerset SM. Refined sugar intake in Australian children. Public Health Nutr. 2003;6:809–13. doi: 10.1079/phn2003501. [DOI] [PubMed] [Google Scholar]
- 44.Jackson P, Romo MM, Castillo MA, Castillo-Durán C. Junk food consumption and child nutrition. Nutritional anthropological analysis. Rev Med Chil. 2004;132:1235–42. doi: 10.4067/s0034-98872004001000012. [DOI] [PubMed] [Google Scholar]
- 45.Krebs-Smith SM. Choose beverages and foods to moderate your intake of sugars: measurement requires quantification. J Nutr. 2001;131(2S-1):527S–35. doi: 10.1093/jn/131.2.527S. [DOI] [PubMed] [Google Scholar]
- 46.Jeffery RW, French SA. Epidemic obesity in the United States: are fast foods and television viewing contributing? Am J Public Health. 1998;88:277–80. doi: 10.2105/ajph.88.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Crawford DA, Jeffery RW, French SA. Television viewing, physical inactivity and obesity. Int J Obes Relat Metab Disord. 1999;23:437–40. doi: 10.1038/sj.ijo.0800845. [DOI] [PubMed] [Google Scholar]
- 48.Carter OB. The weighty issue of Australian television food advertising and childhood obesity. Health Promot J Austr. 2006;17:5–11. doi: 10.1071/he06005. [DOI] [PubMed] [Google Scholar]
- 49.Caroli M, Argentieri L, Cardone M, Masi A. Role of television in childhood obesity prevention. Int J Obes Relat Metab Disord. 2004;28(Suppl 3):S104–8. doi: 10.1038/sj.ijo.0802802. [DOI] [PubMed] [Google Scholar]
- 50.Dyer O. US government rejects WHO's attempts to improve diet. BMJ. 2004;328:185. doi: 10.1136/bmj.328.7433.185. [DOI] [PMC free article] [PubMed] [Google Scholar]