A 69-year-old man was admitted to the hospital with complaints of exertional substernal chest pain and dyspnea for 3 weeks. His medical history consisted of dyslipidemia, type 2 diabetes mellitus, and valvular heart disease. He had a mitral commissurotomy through a left thoracotomy for mitral stenosis at age 16 years followed by mitral valve replacement with a 25 mm Carpentier Edwards bovine pericardial prosthesis in February, 2007. He also had a aortic valve replacement with a 19 mm Carpentier Edwards bovine pericardial prosthesis at that time.
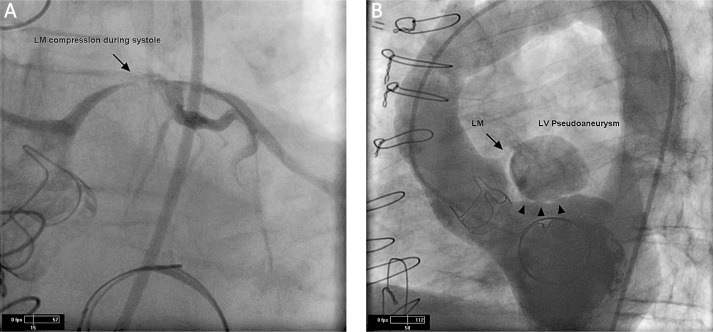
On this admission, he had a maximum troponin I level of 0.12 (normal < 0.05 ng/ml), a creatine kinase-MB fraction of 3.4 (normal < 5.0 ng/ml), and a creatine phosphokinase of 288 (normal 35-232 U/l). Coronary angiography revealed near complete systolic obliteration of the left main coronary artery with normal caliber in diastole and discrete stenosis of the mid left anterior descending coronary artery resulting in 40% obstruction of the vessel (Figure 1A). Left ventriculography revealed systolic aneurysmal dilatation of a segment of the left ventricle (LV) compressing the left main coronary artery in systole and a LV ejection fraction of 50% (Figure 1B).
Figure 1.
Findings on the initial cardiac catheterization. A – Baseline coronary angiogram in left anterior oblique caudal view demonstrating systolic compression of the left main coronary artery (LM). B – Left anterior oblique cranial view of initial left ventriculogram showing left ventricular pseudoaneurysm compressing the LM during systole. Arrowheads indicate LV pseudoaneurysm stalks
A thoracic computed tomography (CT) scan and a transesophageal echocardiogram (TEE) were obtained to provide anatomical delineation of the LV pseudoaneurysm The thoracic CT scan revealed an abnormal 3 cm × 2.4 cm contrast-filled structure to the left of the aorta, superior to the LV outflow tract, and inferior to the left main coronary artery likely representing a LV pseudoaneurysm. The TEE showed a normal LV ejection fraction, a small inferoposterior wall hypokinesis, and a LV pseudoaneurysm with a 1.3 cm opening originating below the mitral annulus anteriorly adjacent to the left atrial appendage extending superiorly to the left main coronary artery.
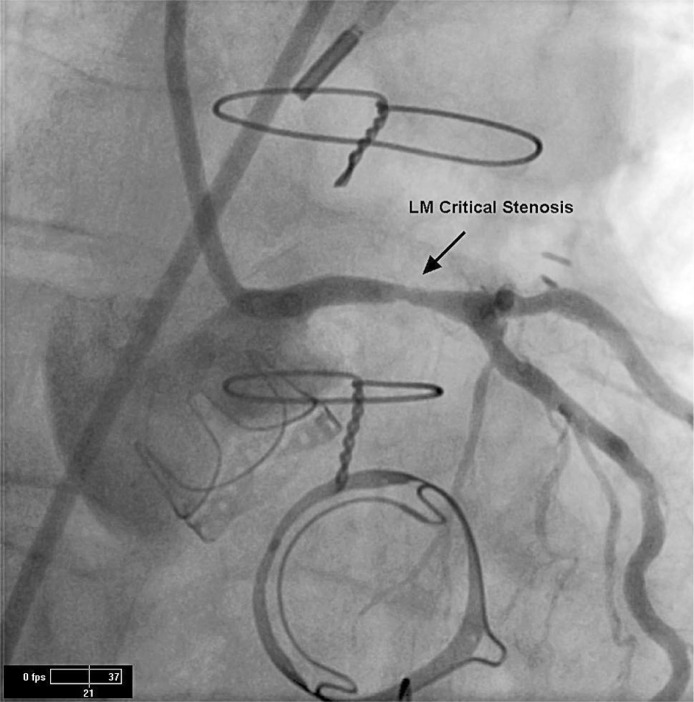
The patient subsequently had a bovine patch repair of the LV pseudoaneurysm with resection of the left atrial appendage. A coronary angiogram obtained after surgery demonstrated a discrete fixed stenosis of the mid left main coronary artery resulting in 70% obstruction of the vessel (Figure 2). Intravascular ultrasound of the left main coronary artery stenosis revealed a cross sectional area of 2.9 mm2.
Figure 2.
Coronary angiogram in right anterior oblique caudal view of LM after resection of LV pseudoaneurysm showing evidence of critical LM stenosis
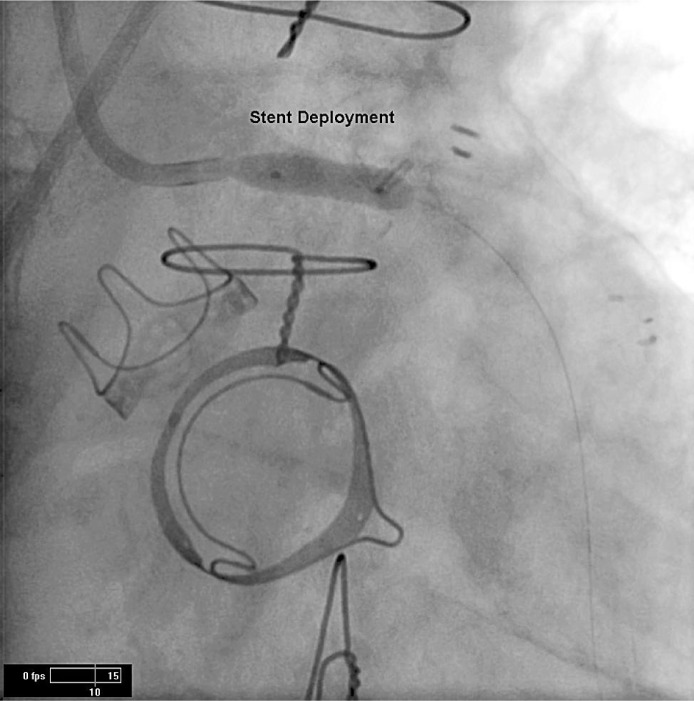
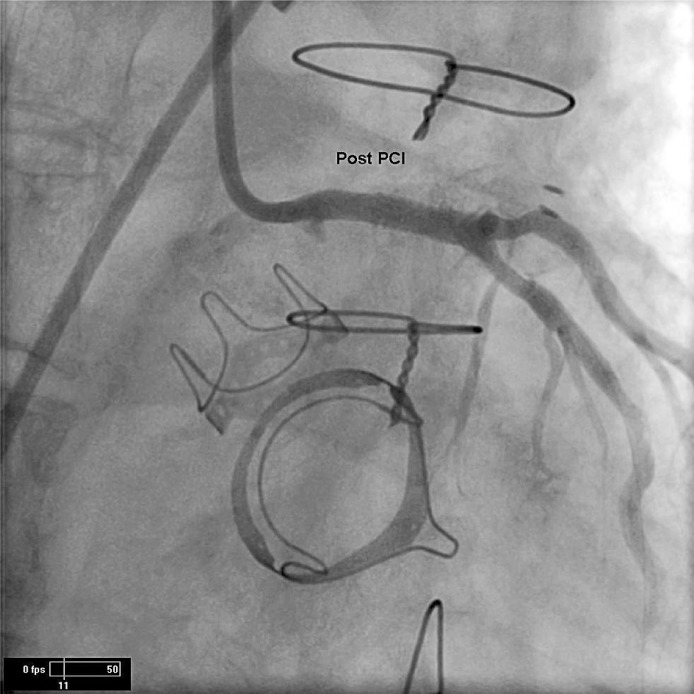
The left main coronary artery was predilated with a 3.5 mm × 9 mm balloon inflated to 8 atm for 6 s. The stenosis was treated with a 4.0 mm × 12 mm everlimus drug-eluting stent that was deployed at 8 atm for 12 s with excellent results (Figures 3 and 4). Intravascular ultrasound imaging after percutaneous coronary intervention revealed a well apposed stent.
Figure 3.
Coronary angiogram displaying deployment of 4.0 mm × 12 mm PROMOS stent to the LM on right anterior oblique caudal view
Figure 4.
Right anterior oblique cranial view of LM after deployment of 4.0 mm × 12 mm PROMOS stent. after percutaneous coronary intervention (post PCI)
A LV pseudoaneurysm is an incomplete rupture of the LV myocardium that is contained by organized LV thrombus, adherent scar tissue, and portions of the epicardum and parietal pericardium. In comparison to a true LV aneurysm, the LV pseudoaneurysm has a maximal neck to internal orifice width ratio of ≤ 0.5, a saccular or globular chamber, and a turbulent Doppler flow pattern through the neck [1]. The LV pseudoaneurysm can drain off significant portions of each LV stroke volume.
A LV pseudoaneurysm can develop due to transmural myocardial infarction, previous ventriculotomy, replacement of the mitral valve, trauma, or infective endocarditis. It occurs in 0.02% to 2.0% of mitral valve replacement surgeries.
Factors predisposing to LV psudoaneurysm include resection of the posterior leaflet of the mitral valve, excessive decalcification of the mitral annulus, placement of an oversized mitral valve prosthesis, and reoperation for mitral valve replacement [2]. The LV pseudoaneurysm following mitral valve replacement tends to be subannular in location [3].
Congestive heart failure, chest pain, and dyspnea are the most frequently reported symptoms associated with LV pseudoaneurysm. Approximately 70% of patients have systolic heart murmurs. A pansystolic murmur due to leaking of blood into the LV pseudoaneurysm may be heard on auscultation [4]. The majority of patients have electrocardiographic abnormalities which are usually nonspecific ST-segment changes. Lethal complications of LV pseudoaneurysm are LV failure, LV thrombus formation, embolization, rupture of the aneurysm and death [5].
To the best of our knowledge, there is only one published case of a patient with a history of open mitral commissurotomy and annuloplasty, aortic valve and mitral valve replacement presenting with chest pain and dyspnea with subsequent development of a LV pseudoaneurysm causing systolic compression of the left main coronary artery [6]. Unique to our case was critical left main coronary artery stenosis seen on coronary angiography after surgery which was successfully treated with percutaneous coronary intervention.
References
- 1.Reeves S, May B. Contained rupture of a left ventricular pseudoaneurysm. Echo Rounds. 2007;105:38–9. doi: 10.1213/01.ane.0000265542.98187.b3. [DOI] [PubMed] [Google Scholar]
- 2.Pretre R, Linka A, Jenni R, Turina M. Surgical treatment of acquired left ventricular pseudoaneurysm. Ann Thorac Surg. 2000;60:553–7. doi: 10.1016/s0003-4975(00)01412-0. [DOI] [PubMed] [Google Scholar]
- 3.Naboodiri N, Dora S, Thomas B, Misra M. Subannular left ventricular pseudoaneurysm following mitral valve replacement. J Cardiothorac Surg. 2008;3:28. doi: 10.1186/1749-8090-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ono M, Wolf R. Left ventricular pseudoaneurysm late after mitral valve replacement. Ann Thorac Surg. 2002;73:1303–5. doi: 10.1016/s0003-4975(01)03268-4. [DOI] [PubMed] [Google Scholar]
- 5.Lanjewar C, Thakkar B, Kerkar P, Khandeparkar J. Submitral left ventricular pseudoaneurysm after mitral valve replacement: early diagnosis and successful repair. Interact CardioVasc Thorac Surg. 2007;6:505–7. doi: 10.1510/icvts.2006.149625. [DOI] [PubMed] [Google Scholar]
- 6.Suda H, Ikeda K, Doi K, Shiraishi R, Furukawa K, Ito T. Successful repair of left ventricular pseudoaneurysm after mitral reoperation under hypothermic circulatory arrest. Jpn J Thorac Cardiovasc Surg. 2003;51:18–20. doi: 10.1007/s11748-003-0060-1. [DOI] [PubMed] [Google Scholar]