Abstract
Purpose: To describe the efficacy and safety of managing ectopic pregnancies (EP) with ultrasound-guided local injections of absolute ethanol (AE).
Methods: 69 cases of EP following IVF performed in our clinic were treated with a local injection of 0.3 ml AE with a 23-gauge needle under transvaginal ultrasonic guidance. The efficacy was evaluated comparing serum beta-human chorionic gonadotropin (β-hCG) levels before and after the injection.
Results: In the 60 successful cases (87%), the serum β-hCG level decreased by 10–30% in two hours postinjection. Of these, 46 were effective with a single injection and the half-life of β-hCG was achieved within 4 days in 45 cases. In 56 cases (including repetitive administration) serum β-hCG levels decreased to 20 mIU/mL within 20 days. The treatment showed no side effects and could be given on an outpatient basis without anesthesia.
Conclusions: This method was shown to be a safe, effective new approach to treating EP.
KEY WORDS: Absolute ethanol local injection, assisted reproductive technology (ART), ectopic pregnancy, transvaginal ultrasonography
INTRODUCTION
The widespread use of Assisted Reproductive Technology (ART) has unavoidably led to an increase in the incidence of ectopic pregnancies (EP). Depending on the literature, the incidence of EP among clinical pregnancies resulting from ART is said to be between 2–5% [1, 2]. The rate was 1.25% in our clinic, despite the fact that we tried to reduce the incidence by introducing such measures as blastocyst transfer and single embryo transfer. In recent years, however, the detection of EP at an early gestational age (GA) has become possible due to the improved accuracy of transvaginal ultrasonotomography and through the detection of the serum β-hCG level. In our clinic, we diagnose pregnancy from 4 weeks 0 day (GA) or 13 days postfertilization by observing the serum β-hCG level. This early diagnosis is made possible by the fact that we use the flare-up effect by GnRH agonist for retrieving oocytes, as well as the fact that we do not use hCG for luteal support. Prognosis of pregnancy is made based on the level of serum β-hCG and by observing the changes in the level, we can swiftly respond to EP. EP is commonly treated with a local injection of MTX and other modalities [3]. However, we decided to study the efficacy and safety of treating EP with a local injection of absolute ethanol (AE).
MATERIALS
The subjects of our study were 69 patients (the mean age was 35 years old) diagnosed for EP following IVF performed in our clinic between January 2002 and December 2004. The condition was diagnosed according to the criteria that intrauterine gestational sacs (GS) were not found by transvaginal ultrasonotomography on and after 20 days postfertilization (5 weeks 0 day GA) and yet a serum β-hCG level of 1000 mIU/mL or above was shown (Table 1).
Table 1.
Criteria for Ectopic Pregnancy
| 1. Gestational age ≥5 weeks 0 day (≥20 days postfertilization) |
| 2. Serum β-hCG level ≥1000 mIU/mL |
| 3. No intrauterine GS |
METHODS
Informed consent was obtained from each patient. The study protocol was approved by the Ethics Board of our clinic. Monitoring of the serum β-hCG level was commenced from 4 weeks 0 day GA, and the progress of the pregnancy was observed by checking the changes in its level. Spontaneous abortions and EP were diagnosed based on the β-hCG level and confirmation of the absence of an intrauterine gestational sac on and after 5 weeks GA. For those diagnosed EP, 0.3 ml of AE was injected into the GS and its surrounding area using a 23-gauge needle under transvaginal ultrasonic guidance (Fig. 1). At the time of injection, GS fluid was aspirated in order to decrease the pressure inside the GS. The serum β-hCG level was monitored before and after the injection in order to evaluate the response. Cases where the serum β-hCG level decreased once after the injection but increased again were re-injected with the same amount of AE at the same location when the level rose again. Anesthesia was not employed in any of the cases. If the serum β-hCG level had not decreased or villi were not found pathologically, laparoscopy was carried out. The serum β-hCG level was assessed using the enzyme immunoassay (EIA) method (TOSOH, AIA-1800).
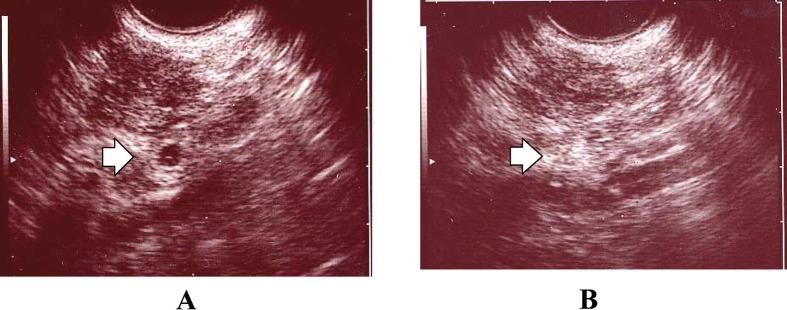
Fig. 1.
The case was of a 38-year-old, nulligravid woman who underwent IVF-ET. The GS was found inside the left fallopian tube on 5 weeks 3 days GA (A). The serum β-hCG level before the injection was 6694 mIU/ml. Absolute ethanol 0.3 ml was directly injected into the GS and its surrounding area using a 23-gauge needle under transvaginal ultrasonic guidance. After the injection, although GS fluid was absorbed and became invisible, the injected site could be clearly seen on the ultrasonic image as a high-intensity mass (B). The serum β-hCG level measured 2 hours post-injection was 4993 mIU/ml, showing a decrease of 28.6%. The level continued to decrease to 1374 mIU/ml, 668 mIU/ml, and 25 mIU/ml on 2 days, 6 days, and 2 weeks post-injection, respectively. During the follow-up, the injected site continued to be visible as a high-intensity area.
RESULTS
The breakdown of 69 cases studied (mean age of 35 years old) is shown in Table 2. The 20 cases were those where no intrauterine GS was observed and the changes in the level of serum β-hCG suggested spontaneous abortion. Therefore they were simply diagnosed as spontaneous abortions and D&C was performed. However, as those cases did not show changes in the level of serum β-hCG after D&C, ultrasound probing was carried out and the presence of an extrauterine GS was recognized. AE injection was then given to treat those 20 cases. The remaining 49 cases were those where an extrauterine GS was observed clearly and were treated with local injections of AE without D&C. We judged that a serum β-hCG of 2000 mIU/mL or more has a higher level of chorionic activity and thus classified the patients into two groups: a higher level group (31 cases) and a lower level group with less than 2000 mIU/mL of serum β-hCG (38 cases).
Table 2.
Cases of Ectopic Pregnancy and Their Locations
| Ectopic location | n=69 | Higher level groupa | Lower level groupb | |
|---|---|---|---|---|
| Right fallopian tube | 38 | Number of cases | 31 | 38 |
| Left fallopian tube | 28 | Mean gestational age | 5 weeks 3 days | 6 weeks 2 days |
| Right interstitial portion of the fallopian tube | 1 | Mean serum β-hCG level (mIU/mL) | 4022 | 1321 |
| Cervical canal | 2 | |||
| Total | 69 | |||
aSerum β-hCG ≥ 2000 mIU/mL.
bSerum β-hCG < 2000 mIU/mL.
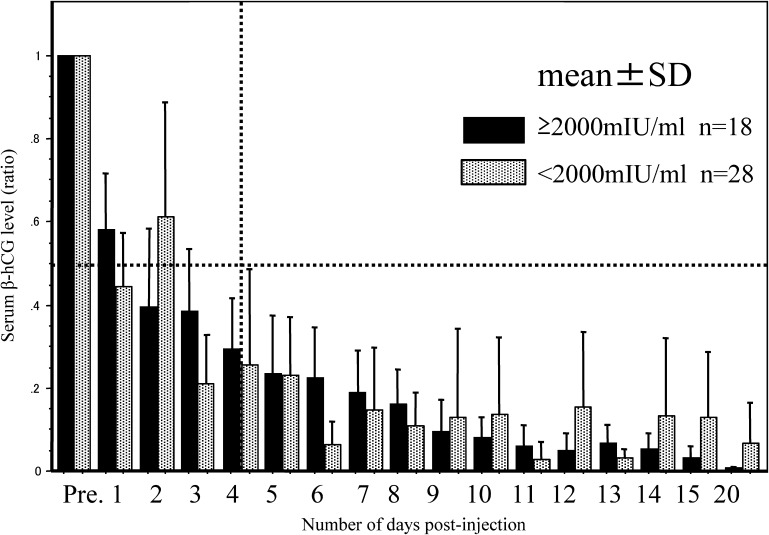
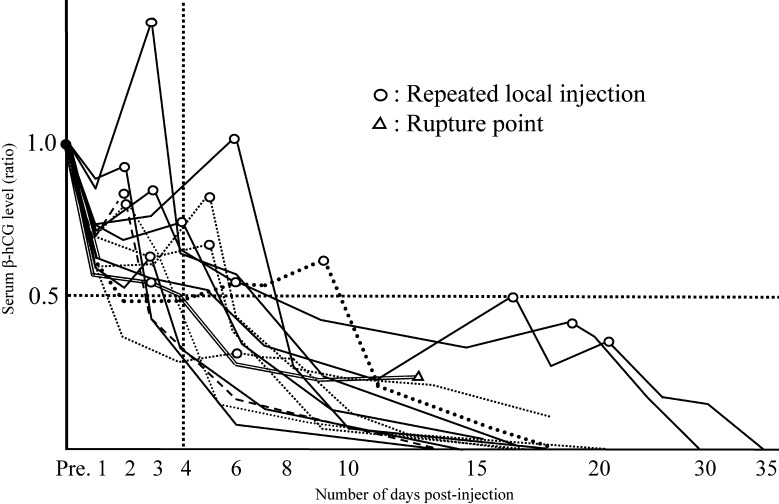
Of a total of 69 cases, the 60 cases in which the treatment was effective all showed a decrease in the level of serum β-hCG by 10–30% in the first 2 h following the injection (Figs. 2.1–2.2). Of 46 cases which required only an initial injection to cause a subsequent decrease in the level (Fig. 2.1), 45 achieved the half-life of β-hCG within 4 days, and 44 cases showed a decrease in the level down to less than 20 mIU/mL within 20 days following the injection. 14 cases were those in which the level of serum β-hCG decreased once after the initial injection then rose again, thus requiring additional injection(s). Those cases were determined as successful by observing their subsequent course of action. Of these, seven achieved the half-life of β-hCG within 4 days and 11 showed a decrease of serum β-hCG level down to 20 mIU/mL or less within 20 days after the injection.
Fig. 2.1.
Post-injection course of serum β-hCG level in the cases treated with single local injection of AE. This figure shows the post-injection course of the higher (≥2000 mIU/ml; n=18) and lower (<2000 mIU/ml; n=28) serum β-hCG level groups, both of which responded effectively to a single administration of local injection. In all cases, the half-life was achieved within 4 days.
As a total, of the 60 successful cases, 56 showed a decrease of serum β-hCG level down to 20 mIU/mL or less within 20 days after the injection.
On the other hand, nine cases did not gain any benefit from the treatment. Of those, eight cases presented physical problems in which, although the presence of extrauterine GS was observed, their location prevented the accurate injection of AE. The complications accompanying these cases were leiomyoma (three cases), endometrial cyst (one case), and frozen pelvis (four cases). The remaining case of failure was due to bilateral tubal pregnancy (Fig. 3). In all nine failed cases, EP was confirmed by laparoscopy and treated by laparoscopic surgery.
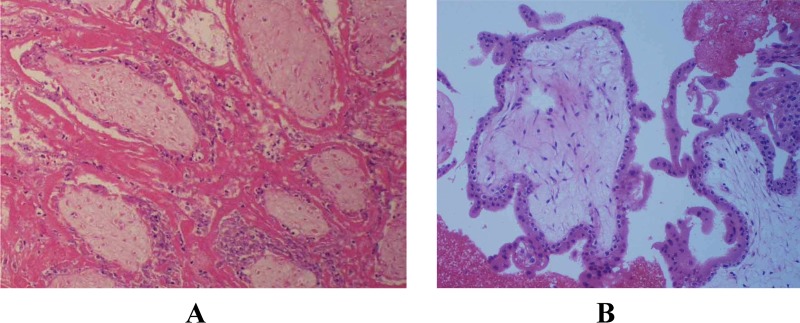
Fig. 3.
Histological findings after alcohol injection (HE stained). The case was that of a 33-year-old nulligravid woman who underwent IVF-ET. Two 5-cell embryos (G1 and G2) were transferred on day 2, resulting in pregnancy. As no intrauterine GS was observed but a tubal GS was observed in the left ampulla of the fallopian tube on 6 weeks 4 days, 0.3 ml of AE was directly injected to the GS under transvaginal ultrasonic guidance. On the following day, as the serum β-hCG level was not reduced, laparoscopy was carried out and bilateral tubal pregnancies in both the left and right ampulla were confirmed. The right fallopian tube was removed. Linear salpingostomy was carried out to the left fallopian tube, extracting the fertile ovum, and salpingoplasty was carried out. Photograph A shows the histological finding of chorionic tissue (HE stained) after the alcohol injection and Photograph B shows the villous tissue (HE stained) in the tubal pregnancy on the right fallopian tube.
One case, which had an accompanying tubal hematoma before the injection, was shown to be effectively treated with the injection of AE as far as the decline of the serum β-hCG level was concerned (Fig. 2.2; marked with △). However, bleeding developed during the follow-up and a laparotomy was given. Thus from the point of view of safety, we subsequently excluded cases showing tubal hematoma from this treatment. Apart from this particular case, no bleeding following the injection was observed. We have now ceased inpatient treatment and treat all cases on an outpatient basis. There was no accompanying pain in any of the cases, and no local nor general anesthesia was necessary. No side effects of the AE injection were observed. Furthermore, as AE's antiseptic property meant a low likelihood of causing a local infection during the procedure, no preventive administration of drugs, including antibiotics, was conducted. The success rate, including the cases of repetitive administration, was 87% (60/69 cases).
Fig. 2.2.
Post-injection course of serum β-hCG level in the cases that required repeated local injections. This figure shows the post-injection course of the 14 cases in which the level of β-hCG decreased once but rose again. They responded effectively after repeated local injections. The local injection was administered when the level rose (marked with o). One case, in which the presence of a tubal hematoma was observed before the injection, resulted in laparotomy because a hemorrhage developed after the injection (marked with △).
DISCUSSION
The primary benefits of AE local injection on treating EP are as follows: 1) its response evaluation can be conducted as quickly as two hours after the injection; 2) it has little impact on the body as only a minimal amount of AE is necessary; 3) it does not affect the intrauterine fetus in the case of heterotopic pregnancies; 4) its antiseptic property means that there is a low probability of causing a local infection during the procedure; 5) as AE does not contain water, the flow of ethanol during the injection is seen in real-time as a high-intensity image on ultrasound imaging. Furthermore, once AE is injected, the site stays as a high-intensity area, facilitating re-injection.
The biggest disadvantage of AE injection is that only a local effect could be expected. In comparison, MTX has an advantage of systemic administration when local administration has failed. However, MTX has the following disadvantages: 1) its response evaluation takes 2–3 days; 2) it is an anticarcinogenic drug and has various side effects; 3) it may not be used in the case of a heterotopic pregnancy as it may affect the intrauterine fetus.
The success rate of treating EP with MTX is 70–95% [3–7], and laparoscopic treatment is necessary for failed cases. By comparison, although the failure rate with AE injection is 13%, it leaves two options for treating failed cases, i.e. systemic administration of MTX and laparoscopic procedure.
Let us consider these points more closely. The primary benefit of using AE was that we can confirm the decrease in the serum β-hCG level by 10–30% as quickly as within two hours after the injection. The patients can be informed of the effect of the treatment 3 h after the procedure, including one hour for gaining the blood test result, and then can go home. The success rate, although it varies in the literature, proved to be equal to or more promising than that of MTX injection [3–7]. The aim of AE injection is to dehydrate and destroy chorionic villi. It is thought that the acute changes in the tissue cause the rapid decrease in the serum β-hCG level (Fig. 3). Therefore the key technique is to have AE infiltrate into the chorionic tissue surrounding the GS, rather than aspirating the fluid inside the GS. AE's antiseptic property means that the risk of local infection is reduced during the procedure, which is advantageous for transvaginal manipulation. No preventive administration, including antibiotics, needs to be performed. The use of a fine needle prevents bleeding and pain, making anesthesia and hospitalization unnecessary (i.e. it can be used as an outpatient treatment). The patients’ financial and time burdens are alleviated due to the fact that AE costs less than MTX and hospitalization is unnecessary. The cases in which the serum β-hCG level decreased once but rose again can be treated by administering additional injections. With all those points in mind, we have summarized the criteria for expectant management as shown in Table 3. In addition, this method is expected to be applicable to heterotopic pregnancies from the point of view of the fact that there are no side effects. Also, it may be applicable as a diagnostic procedure for cases where it is difficult to decide between intrauterine pregnancy and EP because the serum β-hCG level will not decrease when AE is locally injected in areas other than the implanted site.
Table 3.
Criteria for Expectant Management
| 1. The serum β-hCG level is reduced by 10–30% 2 h after the local injection. |
| 2. The half-life is achieved between 2–4 days after the local injection. |
| 3. No bleeding around the GS was seen before the injection. |
| 4. An additional local injection is administered for persistent ectopic pregnancies. |
We gained favorable results with the early detection of EP arising from ART and their treatment by means of a local injection of AE. However, it is still not known up to what gestational age this method is applicable and whether it is effective for cases where crown-rump length (CRL) is measurable and fetus heartbeat can be confirmed. For the treatment of those cases, there are reports of providing local injections of MTX in combination with potassium chloride (KCl) and of the systemic administration of MTX [7]. Incidentally, there is a report showing that, in the case of MTX, the success rate declines when the serum β-hCG level reaches 15000 mIU/mL or above [8]. However, in our cases, even the higher level group's mean value is as low as 4022 mIU/mL, as shown in Fig. 1 The reason for this is that we focus on the earlier detection of EP for those cases where the serum β-hCG level is 1000 mIU/mL or more and yet no GS is observed, by following the progress of pregnancy from 4 weeks 0 day GA, as mentioned earlier. In our present study, the highest level of serum β-hCG shown among the effective cases of the single administration group was 16742 mIU/mL of a cervical pregnancy (5 weeks 1 day GA; GS was 10 mm in diameter) and 6853 mIU/mL of a tubal pregnancy (5 weeks 2 days GA; GS was 8 mm in diameter). Although there should be no pain caused by the procedure per se, leakage of AE into the abdominal cavity can cause peritoneal irritation, which may in turn cause pain to the patient. Furthermore, as mentioned above, cases where hematoma is present before the procedure should be excluded because safety following the AE injection cannot be guaranteed. Also, for cases where the location of the fallopian tubes is abnormal due to such complications as leiomyoma, ovarian cysts, and frozen pelvis, this approach cannot be expected to be effective as it is difficult to inject AE directly in an accurate manner. However, those cases present the same conditions for MTX from the point of view of local injection. Conventional surgery under the guidance of laparoscopy is thought to be the best treatment for such cases.
CONCLUSIONS
The present study has shown that the local injection of AE in the treatment of EP is effective and safe. The technique of ultrasound diagnosis is relatively easy as long as the anatomic location is identified. This method, which can be carried out on an outpatient basis and enables the speedy evaluation of the effect of the treatment, can be thought to be a beneficial new approach to managing EP.
(Some of the contents of this report were presented at the 48th Annual Meeting of the Japanese Society of Fertility and Sterility.)
Footnotes
Transvaginal ultrasound-guided local injections of absolute ethanol are a safe and effective approach to treating ectopic pregnancies.
REFERENCES
- 1.Fernandez H, Gervaise A. Ectopic pregnancies after infertility treatment. Modern diagnosis and therapeutic strategy. Hum Reprod Update. 2004;10(6):503–513. doi: 10.1093/humupd/dmh043. [DOI] [PubMed] [Google Scholar]
- 2.Pyrgiotis E, Sultan KM, Neal GS, Liu HC, Grifo JA, Rosenwaks Z. Ectopic pregnancies after in vitro fertilization and embryo transfer. J Assist Reprod Genet. 1994;11(2):79–84. doi: 10.1007/BF02215992. [DOI] [PubMed] [Google Scholar]
- 3.Darai E, Benifla JL, Naouri M, Pennehouat G, Guglielmina JN, Deval B, Filippini F, Crequat J, Madelenat P. Transvaginal intratubal methotrexate treatment of ectopic pregnancy. Report of 100 cases. Hum Reprod. 1995;11(2):420–424. doi: 10.1093/humrep/11.2.420. [DOI] [PubMed] [Google Scholar]
- 4.Halperin R, Vaknin Z, Schneider D, Yaron M, Herman A. Conservative management of ectopic pregnancy with fetal cardiac activity by combined local (sonographically guided) and systemic injection of methotrexate. Gynecol Obstet Invest. 2003;56:148–151. doi: 10.1159/000073774. [DOI] [PubMed] [Google Scholar]
- 5.Merz E, Bahlmann F, Weber G, Macchiella D, Kruczynski D, Pollow K, Knapstein PG. Unruptured tubal pregnancy: Local low-dose therapy with methotrexate under transvaginal ultrasonographic guidance. Gynecol Obstet Invest. 1996;41:76–81. doi: 10.1159/000292045. [DOI] [PubMed] [Google Scholar]
- 6.Tulandi T, Atri M, Bret P, Falcone T, Khalife S. Transvaginal intratubal methotrexate treatment of ectopic pregnancy. Fertil Steril. 1992;58(1):98–100. doi: 10.1016/s0015-0282(16)55143-7. [DOI] [PubMed] [Google Scholar]
- 7.Monteagudo A, Minior VK, Stephenson C, Monda S, Timor-Tritsch IE. Non-surgical management of live ectopic pregnancy with ultrasound-guided local injection.A case series. Ultrasound Obstet Gynecol. 2005;25:282–288. doi: 10.1002/uog.1822. [DOI] [PubMed] [Google Scholar]
- 8.Lipscomb GH, McCord ML, Stovall TG, Huff G, Portera SG, Ling FW. Predictors of success of methotrexate treatment in women with tubal ectopic pregnancies. N Engl J Med. 1999;341:1974–1978. doi: 10.1056/NEJM199912233412604. [DOI] [PubMed] [Google Scholar]