Abstract
Purpose
To examine the socio-demographic and health characteristics of the underinsured – people who have some health insurance but are having trouble paying for health care or medications.
Methods
The Boston Area Community Health (BACH) Survey is a large (n=5503) community-based random sample of Boston residents aged 30–79 years (1767 Black, 1877 Hispanic, 1859 White; 2301 men and 3202 women).
Results
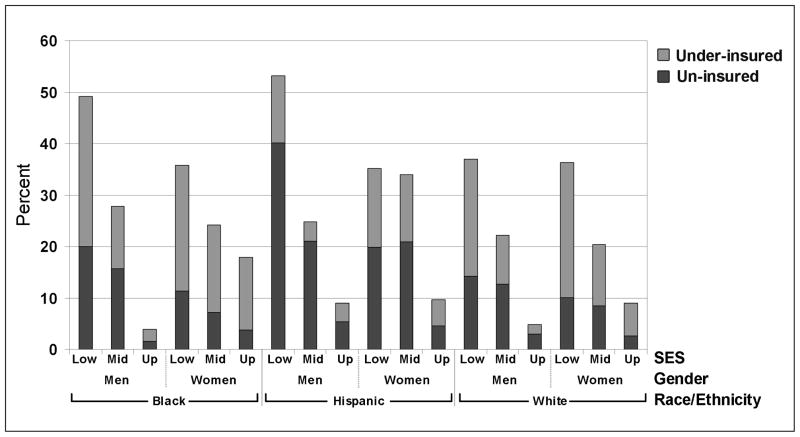
Minorities were less likely than Whites to have health insurance (30%/19% of Hispanic, 16%/9% of Black, and 9%/7% of White men/women lacked health insurance). Blacks were most the likely to be underinsured (18%/20% of Black vs. 9%/14% of Hispanic and 8%/12% of White men/women were underinsured). Those of lower and middle socioeconomic status were also more likely to be uninsured or underinsured. The health status of the uninsured was similar to those with adequate insurance, while those who were underinsured reported more co-morbidities and depression.
Conclusions
The underinsured are generally older, sicker, and make greater use of the health care system and may present a larger public health and health policy challenge than the uninsured.
“Much has been made of the 47 million Americans who don’t have health insurance. But the healthcare reform debate should also focus on the fact that an estimated 25 million working-aged Americans have health insurance but still can’t afford to see a doctor.”(1)
Introduction
That some 49.5 million American adults under the age of 65 (28%) have no health insurance is widely discussed in health policy circles. With few exceptions (2–4), much less attention is given to the additional 42.5 million (24%) who are underinsured (5, 6). In 2007, after some tightening of bankruptcy laws, it was estimated that over 60% of bankruptcies were due to medical bills, even though three quarters of these people had health insurance at the beginning of their illness (7). Another study found that people with health insurance were paying more out-of-pocket and avoiding needed health care (8, 9). The cost of American medical care has encouraged some residents to seek care (10) or medications (11) abroad.
Lack of health insurance has been linked to adverse health outcomes including emergency room or urgent care visits for worsening of asthma symptoms (12), use of thiazolidinediones among diabetics (13), worse outcomes after acute myocardial infraction (14), health care utilization after injury or acquiring a new chronic condition (15), cancer diagnosed at advanced stages (16) and utilization of care for cancer (17). The recent nationwide increase in so-called “retail clinics” has been linked to inadequate health insurance coverage (18).
Using a community-based random sample of Boston, Massachusetts residents aged 30–79 years, this study sought to identify: 1) the socio-demographic characteristics of those who were underinsured – people who had health insurance but reported having trouble paying for health care or medications; 2) the health characteristics (co-morbidities, health related quality-of-life, and risk factors) according to their health insurance status; and 3) how underinsurance affects health care utilization.
Methods
The Boston Area Community Health (BACH) survey is an ongoing epidemiologic survey of Boston residents aged 30–79 years. Detailed methods have been described elsewhere (19). In brief, a stratified two-stage cluster sample was used to recruit residents of Boston, with the goal of approximately equal number of participants by gender, race/ethnicity (Black, Hispanic, White), and age group (30–39, 40–49, 50–59, 60–79). In total, 5503 adults participated in BACH (1767 Black, 1877 Hispanic, 1859 White; 2301 men and 3202 women). The response rate was 63.3 percent of screened eligible participants, which is typical of an epidemiologic field survey requiring a lengthy in-home protocol and phlebotomy. Data were collected between 2002 and 2005, before mandatory health insurance became law in Massachusetts (20–25). After obtaining written informed consent, data were collected during a two hour interview (in English or Spanish), usually in the respondent’s home. All protocols and procedures were approved by the New England Research Institutes’ Institutional Review Board.
Socio-demographics and health insurance status
Race/ethnicity was determined by self-report using the Office of Management and Budget classifications (26). Socioeconomic status (SES) was determined as a combination of education and income, and categorized such that ¼ of the study population was lower, ½ middle, and ¼ upper (27). Respondents reported their current employment status (working for pay, unemployed and looking for work, temporarily laid off or on sick leave, disabled, retired, homemaker, full-time student, or other). A person was said to have no health insurance if they reported no private (from employer, spouse’s employer, military health, self-pay), public (Medicare or Medicaid), or workman’s compensation health insurance. A person was considered to be underinsured if they had health insurance but reported trouble paying for health care or medications or adequately-insured if they had health insurance and did not report trouble paying for medical care.
Health status
We report three aspects of health status: (a) co-morbidities, (b) health related quality-of-life, and (c) risk factors. Co-morbidities were assessed by self-report with the exception of depression which was ascertained using an abridged Center for Epidemiologic Studies Depression scale (28) in which 5 or more (out of 8) symptoms suggested significant depression. Participants’ perception of their current health related quality-of-life was assessed using the SF-12 whose 12 questions can be combined into a physical and mental health component score, each with a mean of 50 and standard deviation of 10 in the United States (US) adult population (29). The first question of the SF-12 is: “In general, would you say your health is: (excellent, very good, good, fair, poor)”. The number responding fair or poor are reported. Risk factors included uncontrolled high blood pressure, physical activity, obesity, smoking, and alcohol consumption. Interviewers measured blood pressure twice using a stethoscope, appropriate size blood pressure cuff, and Sphygmomanometer two minutes apart. Using the second reading, a participant was said to have uncontrolled high blood pressure if the systolic reading was 140 mmHg or higher, or if the diastolic reading was 90 mmHg or higher. Physical activity was measured using the Physical Activity Scale for the Elderly (PASE) (30) and was categorized into low, moderate, and high. The interviewer also measured the respondent’s height and weight which may be converted to body mass index (BMI) (kg/m2) (31). BMI has been categorized as normal (<25), overweight (25–30), or obese (30+). Smoking (cigarettes or cigars) history was classified as never, former, or current smoker. Alcohol consumption of beer, wine, or liquor was categorized using average number of drinks per day as none, less than 1 drink per day, 1 to less than 3 drinks per day, and 3+ drinks per day.
Health care utilization
We asked participants about the number of visits to a health care provider (including routine care, emergency, dental, physical therapy) within the last year. If any, we asked if they had sought care for an urgent (acute) problem, a routine visit for an ongoing problem, a flare-up of an ongoing problem, surgery or injury care, or non-illness care. We also asked if they went for regular care. All prescription and over the counter (OTC) medications used in the last four weeks were collected at the start of the interview with the label information recorded by the interviewer. In addition, participants were asked if they currently took medications for specific indications (such as high blood pressure or pain) and these reports were recorded. Medications were coded using the Slone Drug Dictionary created by the Slone Epidemiology Center at Boston University School of Public Health (32). The coding process identifies drug components and classifies them using a modified form of the American Hospital Formulary Service Drug Pharmacologic Therapeutic Classification System (33). We have counted the number of classes of medications used by prescribed, OTC, or herbal/vitamin preparations as indicative of number of different medications used.
Statistical analysis
Chi-square tests and logistic regression were used to test the assumption of equal distributions by race/ethnicity or health insurance status. Multiple imputation was used to impute plausible values for missing observations using SAS 9.1.3 (SAS Institute, Cary, NC). Twenty-five multiply imputed data sets were created by gender and race/ethnicity. For most variables less than 1 percent of the data were missing. The only exception was income, for which 4/11/3 percent was missing for Black/Hispanic/White participants respectively. Observations were weighted inversely to their probability of selection and weights were post-stratified to the Boston census population in 2000. Analyses were conducted in SUDAAN 9.0.1 (Research Triangle Institute, Research Triangle Park, NC).
Results
Basic socio-demographic information, by gender and race/ethnicity, are presented in Table 1. Minorities are less likely to have health insurance than Whites. Hispanics are twice as likely to be uninsured compared to Blacks. Blacks are most likely to be underinsured.
Table 1.
Descriptive statistics by gender and race/ethnicity
| Gender | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| RE a | B | H | W | p b | B | H | W | p b |
| Demographics | ||||||||
| Age c | <.0001 | <.0001 | ||||||
| 30–39 | 34.5 | 46.4 | 36.4 | 32.7 | 43.3 | 31.6 | ||
| 40–49 | 28.7 | 28.8 | 24.0 | 27.1 | 27.7 | 22.2 | ||
| 50–64 | 26.5 | 17.9 | 24.3 | 27.4 | 19.8 | 26.8 | ||
| 65–79 | 10.4 | 7.0 | 15.3 | 12.8 | 9.2 | 19.4 | ||
| SES ac | <.0001 | <.0001 | ||||||
| lower | 37.3 | 58.7 | 11.8 | 44.1 | 63.3 | 16.2 | ||
| middle | 52.8 | 30.2 | 51.6 | 46.8 | 30.9 | 47.8 | ||
| upper | 9.9 | 11.2 | 36.6 | 9.1 | 5.8 | 36.0 | ||
| Employment status c | <.0001 | <.0001 | ||||||
| employed | 58.7 | 68.3 | 64.8 | 53.6 | 47.6 | 62.1 | ||
| unemployed | 9.9 | 9.2 | 6.5 | 9.0 | 12.5 | 4.3 | ||
| laid off | 3.3 | 2.4 | 4.2 | 3.0 | 0.8 | 1.0 | ||
| disabled | 14.8 | 14.7 | 7.4 | 15.1 | 17.0 | 8.3 | ||
| retired | 11.4 | 3.7 | 14.0 | 12.2 | 3.2 | 15.3 | ||
| other d | 1.9 | 1.6 | 3.2 | 7.1 | 19.0 | 9.1 | ||
| Foreign born c | 24.5 | 84.2 | 8.8 | <.0001 | 18.7 | 86.6 | 10.9 | <.0001 |
| Spanish interview c | 0.1 | 61.8 | 0.4 | <.0001 | 0.4 | 67.9 | 0.1 | <.0001 |
| Trouble paying for health carec | 24.0 | 21.1 | 13.2 | .0001 | 24.0 | 21.6 | 14.8 | .0024 |
| Health related quality-of-life | ||||||||
| PCS 12 e | 48.8 | 50.0 | 50.9 | .0150 | 47.3 | 47.3 | 48.9 | .0567 |
| MCS 12 e | 50.0 | 50.7 | 50.5 | .5356 | 48.7 | 47.9 | 49.9 | .0661 |
| Health insurance status c | <.0001 | <.0001 | ||||||
| Uninsured | 15.9 | 30.5 | 9.3 | 8.7 | 19.3 | 6.6 | ||
| Under | 17.5 | 9.3 | 8.2 | 20.0 | 14.0 | 12.2 | ||
RE = Race/Ethnicity B = Black, H = Hispanic, W = White, SES = Socioeconomic status
Percent
p values from a chi-square test for the null hypothesis that the race/ethnic groups have the same distribution by gender
homemaker – full time student - other
PCS 12 – physical health component score from SF-12, MCS 12 – mental health component score from SF-12 (means)
Table 2 summarizes the socio-demographic characteristics of our sample by gender, race/ethnicity, and health insurance status. In keeping with the predominant source of health insurance in the US (the workplace), BACH participants are less likely to have health insurance if they are unemployed and looking for work or temporarily laid off. However, being employed does not necessarily mean having health insurance since a third of employed Hispanic men, 25 percent of employed Hispanic women and 16 percent of employed Black men report having no health insurance. Those of lower and middle SES are less likely to have health insurance and to be underinsured than those of upper SES. People who are employed are less likely to be underinsured. The proportion of men without health insurance tends to drop as they become older, but the same pattern does not hold for women where it increases in the 40s before dropping. We found that some people (recent immigrants and others) lack any health insurance after the age of 65. Hispanics who are foreign-born or who preferred to do their interview in Spanish are less likely to have health insurance than US born or English speaking Hispanics, although they were more likely to be underinsured. Figure 1 gives the percent of un- or underinsured by gender, race/ethnicity, and SES.
Table 2.
Percent of BACH participants without health insurance (No) or under insured (Under) by gender, race/ethnicity, and socio-demographic characteristics
| Gender | Men | ||||||
|---|---|---|---|---|---|---|---|
| RE a | B | H | W | ||||
| Insurance | No | Under | No | Under | No | Under | p b |
| Age c | |||||||
| 30–39 | 19.6 | 11.3 | 34.8 | 4.7 | 8.6 | 6.7 | <.0001 |
| 40–49 | 15.0 | 17.6 | 31.9 | 10.7 | 15.0 | 7.0 | .0006 |
| 50–64 | 13.5 | 21.3 | 21.3 | 15.1 | 9.1 | 9.2 | .0009 |
| 65–79 | 12.5 | 28.0 | 19.7 | 18.8 | 2.6 | 12.5 | .0094 |
| SES c | |||||||
| lower | 20.0 | 29.2 | 40.1 | 13.2 | 14.2 | 22.8 | .0001 |
| middle | 15.8 | 12.0 | 21.0 | 3.8 | 12.7 | 9.4 | .0081 |
| upper | 1.6 | 2.4 | 5.4 | 3.7 | 3.0 | 1.9 | .7238 |
| Employment status c | |||||||
| employed | 15.7 | 7.9 | 33.4 | 5.2 | 8.9 | 4.4 | <.0001 |
| unemployed | 30.6 | 17.4 | 53.2 | 12.1 | 28.4 | 5.6 | .0956 |
| laid off | 28.2 | 32.9 | 10.7 | 3.2 | 18.8 | 34.2 | .6406 |
| disabled | 8.4 | 43.0 | 10.0 | 25.7 | 4.9 | 17.1 | .0244 |
| retired | 9.8 | 28.6 | 18.9 | 17.5 | 2.7 | 13.0 | .0463 |
| other d | 20.4 | 24.0 | 17.0 | 6.9 | 8.0 | 17.2 | .7407 |
| Foreign born | |||||||
| yes | 15.7 | 15.5 | 32.3 | 9.6 | 3.4 | 6.5 | <.0001 |
| no | 16.0 | 18.1 | 22.9 | 7.8 | 9.9 | 8.4 | .0005 |
| Interview language c | |||||||
| English | 15.9 | 17.5 | 22.9 | 5.4 | 9.3 | 8.3 | <.0001 |
| Spanish | 56.3 | 0.0 | 35.2 | 11.6 | 9.8 | 0.0 | .1647 |
| Gender | Women | ||||||
|---|---|---|---|---|---|---|---|
| RE a | B | H | W | ||||
| Insurance | No | Under | No | Under | No | Under | p b |
| Age c | |||||||
| 30–39 | 6.5 | 20.2 | 16.2 | 13.3 | 7.1 | 12.0 | .0109 |
| 40–49 | 11.6 | 22.7 | 23.2 | 12.5 | 5.9 | 14.9 | .0004 |
| 50–64 | 11.8 | 16.3 | 21.4 | 15.7 | 9.1 | 11.7 | .0125 |
| 65–79 | 1.5 | 21.7 | 17.8 | 18.0 | 3.3 | 10.1 | .0330 |
| SES c | |||||||
| lower | 11.4 | 24.4 | 19.9 | 15.3 | 10.1 | 26.2 | .0194 |
| middle | 7.2 | 17.0 | 21.0 | 13.0 | 8.5 | 11.8 | .0048 |
| upper | 3.8 | 14.0 | 4.6 | 5.0 | 2.6 | 6.4 | .7189 |
| Employment status c | |||||||
| employed | 7.9 | 16.1 | 25.4 | 8.2 | 6.4 | 9.0 | <.0001 |
| unemployed | 21.8 | 34.9 | 15.9 | 14.8 | 17.4 | 28.8 | .5182 |
| laid off | 19.1 | 25.9 | 31.4 | 40.9 | 34.1 | 12.6 | .4918 |
| disabled | 4.1 | 25.1 | 1.6 | 31.5 | 3.1 | 33.0 | .5120 |
| retired | 5.9 | 21.6 | 3.7 | 24.5 | 1.6 | 9.8 | .0613 |
| other d | 8.5 | 14.7 | 24.5 | 9.2 | 12.3 | 11.3 | .3612 |
| Foreign born | |||||||
| yes | 9.2 | 21.0 | 21.1 | 11.6 | 10.7 | 8.0 | .0004 |
| no | 8.6 | 19.8 | 7.6 | 29.3 | 6.2 | 12.7 | .0280 |
| Interview language c | |||||||
| English | 8.6 | 20.0 | 11.0 | 19.8 | 6.6 | 12.2 | .0038 |
| Spanish | 26.2 | 22.4 | 23.2 | 11.2 | 82.3 | 17.7 | .5343 |
RE = Race/Ethnicity B = Black, H = Hispanic, W = White, SES = Socioeconomic status
p values from a chi-square or F test for the null hypothesis that the race/ethnic groups have the same distribution of insurance status by gender and socio-demographic variable
Percent
homemaker – full time student - other
Figure 1.
Percent of uninsured or underinsured by gender (Male/Female), race/ethnicity (Black/Hispanic/White), and socioeconomic status
Next we describe the health status of respondents by gender, race/ethnicity, and health insurance status (Table 3). While men who are underinsured are older, this is not the case for women. In general, people with no health insurance have similar levels of co-morbidities as those with adequate insurance, while those who are underinsured have higher prevalences of some co-morbidities such as depression. In terms of health related quality-of-life, people who are underinsured are more likely to report poor or fair health and they report lower physical and mental health component scores.
Table 3.
Health status (co-morbidities, health related quality-of-life as measured by the SF-12, and risk factors) and health care utilization by gender, race/ethnicity, and insurance status
| Group | Black Men | Hispanic Men | White Men | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| INS a | No | Under | Adq. | p b | No | Under | Adq. | p b | No | Under | Adq. | p b |
| Age c | 46.7 | 51.6 | 47.2 | .0184 | 41.9 | 49.9 | 44.6 | .0001 | 45.2 | 51.1 | 48.4 | .0925 |
| Co-morbidities d | ||||||||||||
| Diabetes | 5.2 | 25.4 | 11.8 | .0005 | 9.7 | 17.0 | 12.1 | .4160 | 14.7 | 11.0 | 6.0 | .4070 |
| CHD a | 7.6 | 27.5 | 10.6 | .0018 | 5.0 | 21.8 | 6.1 | .0815 | 3.1 | 23.4 | 8.9 | .0076 |
| Depres a | 12.6 | 38.5 | 11.7 | .0025 | 17.1 | 38.9 | 13.4 | .0037 | 9.5 | 39.5 | 9.9 | .1281 |
| Health related quality-of-life | ||||||||||||
| PCS 12 a | 50.3 | 41.8 | 50.2 | <.0001 | 51.0 | 45.3 | 50.3 | .0011 | 51.3 | 42.0 | 51.8 | .0001 |
| MCS 12 a | 48.9 | 42.2 | 52.2 | <.0001 | 51.5 | 46.4 | 51.0 | .0635 | 50.8 | 44.8 | 51.0 | .0067 |
| Poor/fair health d | 13.6 | 42.3 | 13.4 | .0001 | 29.3 | 47.1 | 27.8 | .0402 | 8.8 | 18.4 | 9.7 | .2657 |
| Risk factors d | ||||||||||||
| HBP a | 29.5 | 30.1 | 32.5 | .8287 | 18.9 | 25.3 | 18.1 | .5434 | 13.9 | 17.3 | 16.9 | .8337 |
| Physical activity | .0001 | .0005 | .0427 | |||||||||
| low | 19.9 | 45.6 | 21.2 | 16.3 | 46.9 | 27.5 | 22.7 | 48.8 | 26.0 | |||
| moderate | 59.7 | 39.5 | 44.5 | 60.9 | 32.9 | 41.4 | 61.6 | 42.4 | 47.1 | |||
| high | 20.4 | 14.8 | 34.3 | 22.8 | 20.3 | 31.1 | 15.6 | 8.8 | 26.8 | |||
| Health care utilization d | ||||||||||||
| HCP a visits in last year | <.0001 | .0008 | .0019 | |||||||||
| 0 | 22.7 | 2.3 | 5.8 | 41.1 | 18.5 | 12.5 | 21.8 | 1.6 | 7.1 | |||
| 1–4 | 55.1 | 42.2 | 58.8 | 41.0 | 37.6 | 58.8 | 45.3 | 27.5 | 48.3 | |||
| 5–9 | 7.3 | 20.0 | 17.9 | 9.6 | 15.4 | 12.8 | 20.1 | 17.1 | 20.5 | |||
| 10+ | 15.0 | 35.5 | 17.5 | 8.4 | 28.6 | 16.0 | 12.9 | 53.8 | 24.1 | |||
| Regular care | 50.9 | 91.8 | 86.0 | <.0001 | 43.0 | 78.7 | 77.3 | <.0001 | 48.4 | 90.6 | 79.0 | <.0001 |
| Prescription med a (classes) | .0011 | .0027 | <.0001 | |||||||||
| 0 | 67.2 | 28.7 | 56.6 | 73.6 | 36.1 | 55.9 | 64.0 | 23.4 | 43.1 | |||
| 1–2 | 15.6 | 27.3 | 18.2 | 14.3 | 25.1 | 20.9 | 29.8 | 28.7 | 29.0 | |||
| 3–4 | 8.1 | 16.3 | 13.9 | 6.8 | 20.2 | 12.4 | 2.6 | 24.1 | 17.7 | |||
| 5+ | 9.1 | 27.8 | 11.3 | 5.2 | 18.6 | 10.8 | 3.6 | 23.8 | 10.1 | |||
| Group | Black Women | Hispanic Women | White Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| INS a | No | Under | Adq. | p | No | Under | Adq. | p | No | Under | Adq. | p |
| Age c | 47.7 | 47.7 | 48.6 | .7656 | 46.8 | 47.1 | 44.8 | .3690 | 48.9 | 49.7 | 50.8 | .6252 |
| Co-morbidities c | ||||||||||||
| Diabetes | 10.3 | 13.3 | 12.6 | .8619 | 7.5 | 13.8 | 12.0 | .1947 | 3.8 | 11.9 | 7.3 | .1509 |
| CHD a | 3.4 | 20.7 | 9.2 | .0052 | 6.3 | 11.9 | 4.1 | .1090 | 8.3 | 6.7 | 6.7 | .9560 |
| Depres a | 20.6 | 42.6 | 20.4 | .0120 | 35.2 | 55.5 | 32.4 | .0331 | 12.6 | 35.2 | 10.8 | .0002 |
| Health related quality-of-life | ||||||||||||
| PCS 12 a | 49.2 | 46.1 | 47.4 | .2929 | 47.8 | 44.3 | 47.8 | .2114 | 50.0 | 43.5 | 49.6 | .0010 |
| MCS 12 a | 51.2 | 43.3 | 49.9 | .0015 | 50.0 | 38.0 | 49.4 | .0005 | 47.3 | 44.5 | 50.9 | <.0001 |
| Poor/fair health d | 17.6 | 26.2 | 21.5 | .4312 | 41.4 | 49.2 | 33.7 | .1234 | 9.1 | 26.2 | 8.9 | .0006 |
| Risk factors c | ||||||||||||
| HBP a | 10.1 | 20.8 | 16.5 | .1081 | 11.7 | 12.8 | 10.3 | .8124 | 17.4 | 14.7 | 8.0 | .0784 |
| Physical Activity | .4069 | .3513 | .0010 | |||||||||
| low | 36.5 | 28.9 | 24.9 | 32.2 | 45.6 | 31.4 | 25.5 | 42.8 | 24.8 | |||
| moderate | 48.3 | 50.4 | 54.0 | 59.6 | 45.3 | 57.2 | 66.0 | 46.1 | 53.6 | |||
| high | 15.2 | 20.7 | 21.1 | 8.2 | 9.1 | 11.4 | 8.5 | 11.0 | 21.5 | |||
| Health care utilization d | ||||||||||||
| HCP a visits in last year | .0075 | .0300 | .0050 | |||||||||
| 0 | 15.9 | 0.7 | 1.59 | 6.3 | 8.6 | 5.6 | 5.3 | 0.3 | 2.3 | |||
| 1–4 | 45.2 | 45.7 | 51.0 | 52.2 | 28.5 | 54.4 | 53.9 | 33.4 | 40.9 | |||
| 5–9 | 19.7 | 11.4 | 22.4 | 16.8 | 34.0 | 20.2 | 21.9 | 23.2 | 26.9 | |||
| 10+ | 19.2 | 42.2 | 25.0 | 24.7 | 28.9 | 19.8 | 18.8 | 43.1 | 30.0 | |||
| Regular care | 82.3 | 95.3 | 95.1 | .0350 | 84.4 | 92.5 | 95.2 | .0041 | 79.9 | 93.4 | 95.3 | .0397 |
| Prescription med a (classes) | .0035 | .0001 | .2162 | |||||||||
| 0 | 59.1 | 30.6 | 36.8 | 50.0 | 36.5 | 42.4 | 45.0 | 24.9 | 31.9 | |||
| 1–2 | 21.8 | 27.6 | 35.4 | 34.9 | 32.4 | 30.4 | 29.3 | 30.2 | 32.8 | |||
| 3–4 | 7.1 | 18.8 | 12.9 | 11.5 | 12.1 | 13.0 | 11.7 | 18.0 | 18.4 | |||
| 5+ | 12.0 | 23.0 | 14.9 | 3.6 | 19.0 | 14.2 | 14.0 | 26.9 | 16.8 | |||
INS = health insurance, No = no health insurance, Under = under insured (health insurance but trouble paying for health care), Adq. = insured and no trouble paying for health care), CHD = heart disease, Depres = 5 or more (of 8) depressive symptoms, PCS 12 – physical health component score from SF-12 (mean), MCS 12 – mental health component score from SF-12 (mean), HBP = uncontrolled hypertension, HCP = Health care provider
p value from a chi-square or F test that the proportion or mean is the same across health insurance status by gender and race/ethnicity
years (mean)
Percent
In a logistic regression model with uncontrolled hypertension as the dependent variable and including age and gender as explanatory variables, respondents who were uninsured (odds ratio 1.20 with 95% confidence interval 0.83, 1.75) or who were underinsured (odds ratio 1.36 with 95% confidence interval 1.04, 1.77) were more likely to have (interviewer measured) uncontrolled hypertension. People with adequate health insurance tend to have higher levels of physical activity and are less likely to be current smokers. Minority men who have adequate insurance are less likely to have 3 or more drinks per day. White men with adequate health insurance are less likely to be obese (BMI 30+ kg/m2).
We next consider health care utilization (Table 3). Those without health insurance had fewer health care provider visits in the last year, with 20–40 percent of the men without health insurance having no visits to any health care provider in the last year. People who are underinsured are the most likely to have 10 or more health care provider visits in the last year, perhaps reflecting their poorer health status. However, participants were equally likely to go to a health care provider for an urgent or acute problem or a flare-up of an ongoing problem if they had no or adequate health insurance, with higher levels for those who were underinsured (data not shown). Men without health insurance were less likely to go for a routine visit for an ongoing problem or non-illness care (data not shown). Both men and women without health insurance were less likely to go for regular care. Participants without health insurance were less likely to report the use of prescription medications. The use of OTC medications was similar for those without health insurance and for those who were adequately insured, with somewhat higher use in those who were underinsured (minority men and White women) (data not shown). The use of herbal/vitamin preparations was similar regardless of health insurance status (data not shown).
Discussion
In our population-based survey, we found that minorities and those of lower and middle socioeconomic status are less likely to have health insurance or to be underinsured compared to Whites and those of upper socioeconomic status. Hispanics, particularly young Hispanic men, were the least likely to have health insurance. This is consistent with other studies (34–36). Being 65 or older does not guarantee a person health insurance, as 12–20 percent of minority men aged 65 or older reported not having health insurance. Because Massachusetts residents are more likely to have health insurance than the national average (37), we do not use these data to project the number of Americans who are uninsured.
It is not surprising that those without health insurance have worse health outcomes down the road (38–40), since they are less likely to go for regular care, even routine care for an ongoing problem. In addition, co-morbidities among the uninsured may reflect loss of insurance or difficulty getting insurance following diagnosis of a major medical problem.
Underinsurance appears to be more of a problem than uninsurance for many groups. While we found that those who were underinsured were likely to make more health care provider visits, they were less healthy (more co-morbidities and more likely to have uncontrolled hypertension) and had lower health related quality-of-life. This may be a function of our operational definition of underinsurance — those reporting trouble paying for health care may be the ones who are using it most and hence, have the highest costs. Regardless, our analyses suggest that for those who have many health problems, it is a struggle to pay for health care and traditional insurance may be inadequate. Our findings are timely since the Kaiser Family Foundation recently reported 32% of Americans live in a household where at least one person had trouble paying medical bills; with 18% having medical bills exceeding $1000 (41). The same study also reported 47% of Americans live in a household in which someone put off or postponed getting health care they needed, skipped recommended medical tests or treatments, didn’t fill a prescription, cut pills or skipped doses of medications, or had problems getting mental health care because of cost. It has been found that important global determinants of health include universal coverage and low or no co-payments (42) which may explain why Americans have a lower life expectancy at birth compared to many other industrialized countries (43). Researchers have recently found that 45,000 deaths per year in the US are associated with uninsurance (44). Additional mortality is likely associated with underinsurance as wealth has been shown to be an independent predictor of health status and life expectancy (45).
Use of a community-based random sample (with adequate representation of different race/ethnic and socioeconomic groups) allows us to include people who are uninsured and not presenting for care. The proportion of people with health insurance is considered a ‘leading health indicator’, and improving the proportion with coverage is a goal of the national 2010 Healthy People initiative (46). Since BACH has transitioned to a prospective cohort design, we will be able to follow-up to determine if race/ethic and socioeconomic disparities change in the wake of Massachusetts health care reform (20–25).
Our study has major strengths: It uses a community-based random sample with adequate race/ethnic and socioeconomic diversity. We are able to consider a wide variety of covariates including socio-demographics, health status, co-morbidities, health related quality of life, lifestyle, and health care utilization. Some of our measures are interviewer measured (height, weight, blood pressure) while others rely on self-report which has been found to be well correlated with medical records (47–49). Our study also has some limitations: Unfortunately, we were unable to include other minority groups (e.g. Asian Americans) because the city of Boston does not have them in sufficient numbers to include them given our survey sampling design. While a combination of education and income may not fully capture what is signified by the concept of SES, it does appear to account for much of the variation of health insurance status. The generalizability of our findings may be questioned because the BACH study was conducted in a single inner-city area. However, we have compared the health status of BACH participants to national surveys such as the Behavior Risk Factor Surveillance System (BRFSS), National Health Interview Survey (NHIS), and the National Health Examination and Nutrition Survey (NHANES) and find comparable prevalence rates (with the exception of asthma which appears to be more prevalent in Boston) which indicates that these results with suitable modification for different demographics and health insurance status may be generalizable to the US population.
Conclusions
Using data from a representative, population-based sample, we have estimated the sizeable proportions of the population who are underinsured, and describe their socio-demographic characteristics, health status and utilization behavior. While much attention is justifiably focused on the national challenge of uninsurance, which is the situation for some 49 million Americans, we have highlighted what may be an even more insidious problem: the underinsurance of an additional 42 million people in the US. Our data permit us to describe in some detail who exactly the underinsured are and provide new information on their health status, utilization behavior and quality of life.
For most people in the U.S. health insurance is inextricably tied to employment. The last two decades has witnessed a decline in the large manufacturing sectors (with strong workers unions and excellent health and retirement benefits) and an increase in the competitive, small-business sector (with disproportionately non-unionized older minority workers who are uninsured or underinsured). To simply remain economically viable, many small businesses cannot offer (ever more costly) health insurance coverage to employees, or they can only offer the bare minimum (underinsurance), or introduce cost sharing measures. Present trends in the U.S. economy suggest that this trend will increase, with even the largest employers reducing or eliminating health insurance coverage due to the explosive increase in health care costs. Changes in the composition of the workplace (especially The increase in the small business sector appears to make employment-based health insurance an unsustainable foundation for our future U.S. health care system.
Acknowledgments
Funding: BACH is supported by NIH, NIDDK U01 DK56842. Additional support for this manuscript was provided by the National Center on Minority Health and Health Disparities (NCMHD). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases, the National Center on Minority Health and Disparities, or the National Institutes of Health.
Both authors participated in the conception, design, analysis, and interpretation of data and drafting of the manuscript. Neither author has any conflict of interest nor any commercial relationships relevant to this manuscript. Both authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Biographies
Carol Link, PhD, Sr. Statistician is a mathematical statistician and received her PhD from Stanford in 1979. She has extensive experience in applied data analysis at NERI and previously with the federal Government. She has been the senior statistician on several clinical decision making studies, two involved international comparisons of doctors in three different health care systems (the private insurance system (United States), the government supported system (United Kingdom), and the decentralized care administered by social security agencies in Germany). Other work at NERI includes epidemiologic surveys, clinical trials, and health services research. She has co-authored over 80 journal articles.
John B. McKinlay, PhD, FACE, is an internationally respected health services researcher/epidemiologist. At Boston University for 20+ years he held Professorships in Sociology, Epidemiology, Statistics and Medicine and directed several research centers. He was among the first to write on effectiveness-based resource allocation (“comparative effectiveness”), and the corporatization of doctoring in the U.S. He is a recipient of numerous professional awards and a 2-time NIH MERIT award recipient. He has contributed over 400 research papers and 17 books. He is Senior Vice President and Director at NERI and Co-Director of the Health Services Research and Policy and Health Disparities program.
Footnotes
Reprint requests: John B. McKinlay, Ph.D, FACE, New England Research Institutes, Inc., 9 Galen Street, Watertown, MA 02472, Tele. +1 (617) 972-3012, FAX +1 (617) 926-8246, jmckinlay@neriscience.com
References
- 1.Dean H. Howard Dean’s Prescription for Real Healthcare Reform. Chelsea Green Publishing Co; Vermont: 2009. [Google Scholar]
- 2.Fronstin P. Sources of health insurance and characteristics of the uninsured: Analysis of the March 2007 Current Population Survey. EBRI Issue Brief. 2007;310:1–33. [PubMed] [Google Scholar]
- 3.Ahluwalia IB, Bolen J, Garvin B. Health insurance coverage and use of selected preventive services by working-age women, BRFSS, 2006. J Womens Health (Larchmt) 2007;16(7):935–40. doi: 10.1089/jwh.2007.CDC8. [DOI] [PubMed] [Google Scholar]
- 4.Ahluwalia IB, Bolen J. Lack of health insurance coverage among working-age adults, evidence from the Behavioral Risk Factor Surveillance System, 1993–2006. J Community Health. 2008;33(5):293–296. doi: 10.1007/s10900-008-9106-8. [DOI] [PubMed] [Google Scholar]
- 5.Schoen C, et al. How many are underinsured? Trends among U.S. adults, 2003 and 2007. Health Aff (Millwood) 2008;27(4):w298–309. doi: 10.1377/hlthaff.27.4.w298. [DOI] [PubMed] [Google Scholar]
- 6.Cunningham PJ. Trade-offs getting tougher: Problems paying medical bills increase for US families, 2003–2007. Center for Studying Health System Change; Washington, D.C: Tracking Report No. 21:1–5, 2008 http://www.hschange.com/CONTENT/1017/ (August 24, 2009) [PubMed] [Google Scholar]
- 7.Himmelstein DU, et al. Medical bankruptcy in the United States, 2007: Results of a national study. Am J Med. 2009;122(8):741–6. doi: 10.1016/j.amjmed.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 8.Doty MM, et al. Failure to protect: Why the individual insurance market is not a viable option for most U.S. families: Findings from the Commonwealth Fund Biennial Health Insurance Survey 2007. Issue Brief (Commonwealth Fund) 2009;62:1–16. [PubMed] [Google Scholar]
- 9.Doty MM, Edwards JN, Holmgren AL. Results from a National Survey. Issue Brief (Commonwealth Fund) 837. 2005. Seeing red: Americans driven into debt by medical bills; pp. 1–12. [PubMed] [Google Scholar]
- 10.Pafford B. The third wave-medical tourism in the 21st century. South Med J. 2009;102(8):810–813. doi: 10.1097/SMJ.0b013e3181aa8ce4. [DOI] [PubMed] [Google Scholar]
- 11.Rivera JO, Ortiz M, Cardenas V. Cross-border purchase of medications and health care in a sample of residents of El Paso, Texas, and Ciudad Juarez, Mexico. J Natl Med Assoc. 2009;101(2):167–73. doi: 10.1016/s0027-9684(15)30831-2. [DOI] [PubMed] [Google Scholar]
- 12.Markovitz BP, Andresen EM. Lack of insurance coverage and urgent care use for asthma: a retrospective cohort study. BMC Public Health. 2006;6:14. doi: 10.1186/1471-2458-6-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aquilante CL, Zhang W, McCollum M. Race, ethnicity, and use of thiazolidinediones among US adults with diabetes. Curr Med Res Opin. 2007;23(3):489–94. doi: 10.1185/030079906X167354. [DOI] [PubMed] [Google Scholar]
- 14.Rahimi AR, et al. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA. 2007;297(10):1063–72. doi: 10.1001/jama.297.10.1063. [DOI] [PubMed] [Google Scholar]
- 15.Hadley J. Insurance coverage, medical care use, and short-term health changes following an unintentional injury or the onset of a chronic condition. JAMA. 2007;297(10):1073–84. doi: 10.1001/jama.297.10.1073. [DOI] [PubMed] [Google Scholar]
- 16.Halpern MT, et al. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: A retrospective analysis. Lancet Oncol. 2008;9(3):222–31. doi: 10.1016/S1470-2045(08)70032-9. [DOI] [PubMed] [Google Scholar]
- 17.Ward E, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58(1):9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 18.McKinlay JB, Marceau LD. Unpublished working paper. New England Research Institutes; Watertown, Ma: Jul, 2009. From cottage industry to a dominant mode of primary care: 6 stages in the emergence of convenient care clinics. [Google Scholar]
- 19.McKinlay JB, Link CL. Measuring the urologic iceberg: design and implementation of the Boston Area Community Health (BACH) Survey. Eur Urol. 2007;52(2):389–96. doi: 10.1016/j.eururo.2007.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Himmelstein DU, Woolhandler S. Massachusetts’ approach to universal coverage: high hopes and faulty economic logic. Int J Health Serv. 2007;37(2):251–7. doi: 10.2190/Q81U-215K-6570-5121. [DOI] [PubMed] [Google Scholar]
- 21.Kleinpeter MA. The Massachusetts health insurance law: providing health insurance to all. J Natl Med Assoc. 2006;98(11):1867–73. [PMC free article] [PubMed] [Google Scholar]
- 22.Blumberg LJ, et al. Setting a standard of affordability for health insurance coverage. Health Aff (Millwood) 2007;26(4):w463–73. doi: 10.1377/hlthaff.26.4.w463. [DOI] [PubMed] [Google Scholar]
- 23.Holahan J, Blumberg L. Massachusetts health care reform: a look at the issues. Health Aff (Millwood) 2006;25(6):w432–43. doi: 10.1377/hlthaff.25.w432. [DOI] [PubMed] [Google Scholar]
- 24.McGlynn EA, Wasserman J. Massachusetts health reform: beauty is in the eye of the beholder. Health Aff (Millwood) 2006;25(6):w447–9. doi: 10.1377/hlthaff.25.w447. [DOI] [PubMed] [Google Scholar]
- 25.McDonough JE, et al. Massachusetts health reform implementation: major progress and future challenges. Health Aff (Millwood) 2008;27(4):w285–97. doi: 10.1377/hlthaff.27.4.w285. [DOI] [PubMed] [Google Scholar]
- 26.Executive Office of the President of the United States: Office of Management and Budget: Federal Register Notice, 1997.
- 27.Green LW. Manual for scoring socioeconomic status for research on health behavior. Public Health Rep. 1970;85(9):815–27. [PMC free article] [PubMed] [Google Scholar]
- 28.Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int Psychogeriatr. 1999;11(2):139–48. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- 29.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Washburn RA, et al. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–62. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 31.McKinlay SM, et al. Health Survey Research Methods: Proceedings of the fourth conference on Health Survey Research Methods. DHHS Publication No. (PHS) 84–3346. U.S. Government Printing Office; Washington, D.C: 1984. A field approach for obtaining physiological measures in surveys of general populations: Response rates, reliability, and costs. [Google Scholar]
- 32.Kelley KE, et al. The Slone Drug Dictionary: A research driven pharmacoepidemiology tool. Pharmacoepidemiol Drug Saf. 2003;12(S1–189):168–9. [Google Scholar]
- 33.American Society of Health-System Pharmacists: AHFS Drug Information. Bethesda: American Society of Health-System Pharmacists, Inc; 2007. http://www.ahfsdruginformation.com/ (August 24, 2009) [Google Scholar]
- 34.Donelan K, DesRoches CM, Schoen C. Inadequate health insurance: costs and consequences. MedGenMed. 2000;2(3):E37. [PubMed] [Google Scholar]
- 35.Gary TL, et al. Racial/ethnic differences in the healthcare experience (coverage, utilization, and satisfaction) of US adults with diabetes. Ethn Dis. 2003;13(1):47–54. [PubMed] [Google Scholar]
- 36.U.S. Census Bureau. Income, Poverty, and Health Insurance Coverage in the United States 2004. 2005 Aug; http://www.census.gov/prod/2005pubs/p60-229.pdf (August 24, 2009)
- 37.Davern M. A Comparison of the health insurance coverage estimates from four national surveys and six state surveys. An Invited Presentation at the Joint Statistical Meetings of the American Statistical Association; Denver, CO. August 5, 2008. [Google Scholar]
- 38.Hadley J. Sicker and poorer--the consequences of being uninsured: A review of the research on the relationship between health insurance, medical care use, health, work, and income. Med Care Res Rev. 2003;60(2 Suppl):3S–75S. doi: 10.1177/1077558703254101. discussion 76S–112S. [DOI] [PubMed] [Google Scholar]
- 39.Kasper JD, Giovannini TA, Hoffman C. Gaining and losing health insurance: strengthening the evidence for effects on access to care and health outcomes. Med Care Res Rev. 57(3):298–318. doi: 10.1177/107755870005700302. discussion 319–25, 2000. [DOI] [PubMed] [Google Scholar]
- 40.Schoen C, DesRoches C. Uninsured and unstably insured: the importance of continuous insurance coverage. Health Serv Res. 2000;35(1 Pt 2):187–206. [PMC free article] [PubMed] [Google Scholar]
- 41.Kaiser Family Foundation. Kaiser Health Tracking Poll: Election 2008. 2008;(11) http://www.kff.org/kaiserpolls/upload/7832.pdf (August 2009)
- 42.Starfield B, Shi L. Policy relevant determinants of health: an international perspective. Health Policy. 2002;60(3):201–18. doi: 10.1016/s0168-8510(01)00208-1. [DOI] [PubMed] [Google Scholar]
- 43.The World Factbook 2009. Central Intelligence Agency; Washington, D.C: 2009. [Google Scholar]
- 44.Wilper AP, et al. Health insurance and mortality in US adults. Am J Public Health. 2009 Sep 17; doi: 10.2105/AJPH.2008.157685. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kennickell AB. What is the difference? Evidence on the distribution of wealth, health, life expectancy, and health insurance coverage. Stat Med. 2008;27(20):3927–40. doi: 10.1002/sim.3375. [DOI] [PubMed] [Google Scholar]
- 46.U.S. Department of Health and Human Services. Healthy People 2010: Leading Health Indicators. http://www.healthypeople.gov/LHI/LHIPrioritiesforAction.pdf (August 24, 2009)
- 47.Bergmann MM, et al. Validity of self-reported diagnoses leading to hospitalization: a comparison of self-reports with hospital records in a prospective study of American adults. Am J Epidemiol. 1998;147(10):969–77. doi: 10.1093/oxfordjournals.aje.a009387. [DOI] [PubMed] [Google Scholar]
- 48.Okura Y, et al. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57(10):1096–103. doi: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 49.St Sauver JL, et al. Agreement between patient reports of cardiovascular disease and patient medical records. Mayo Clin Proc. 2005;80(2):203–10. doi: 10.4065/80.2.203. [DOI] [PubMed] [Google Scholar]