Abstract
Laryngeal amyloidosis is uncommon and poorly understood, with limited long-term studies. Although primary localized laryngeal amyloidosis is extremely rare, it frequently involves the ventricles and the false and true vocal cords. We present a 58-year-old woman with localized laryngeal amyloidosis who presented no symptoms. On indirect laryngoscopic examination, the mass involved both arytenoids only, and had a likeness to a "boxer glove." She was treated surgically by microlaryngoscopy under general anesthesia and the mass was excised using a carbon dioxide laser. We present this case and a review of literature.
Keywords: Amyloidosis, Larynx
INTRODUCTION
Amyloidosis is an uncommon benign disorder, characterized by the extracellular deposition of amyloid. Clinically, amyloidosis is classified into two main forms, systemic and localized. If the deposition is systemic, the prognosis is worse than in localized forms. Laryngeal amyloidosis is a rare lesion representing 1% of all benign laryngeal tumors. The ventricles and the false and true vocal cords are the most common sites for localized amyloidosis in the respiratory tree [1]. A high degree of suspicions is necessary since clinical presentation of the disease may mimic that of a laryngeal neoplasm. We describe here a patient with primary localized laryngeal amyloidosis whose laryngoscopic finding had a likeness to a "boxer glove" on both arytenoids only.
CASE REPORT
A 58-year-old woman presented to our clinic for evaluation of her larynx. She was in relatively good health with no history of previous illness. She had gone to a local clinic one week prior, and the physician had detected a laryngeal mass by chance during a gastrofiberscopic examination. She had no laryngeal symptoms (hoarseness, stridor, voice change, dyspnea, cough, etc). There were no specific past and family histories. Also, she did not take any surgery before.
Fiberoptic laryngoscopy disclosed large, symmetric, smooth, round, yellow masses on the apices of both arytenoid cartilages (Fig. 1A). The masses looked like a pair of boxer gloves. The true and false vocal cords were mobile and appeared normal. On physical examination, there were no specific findings in head and neck area and no bony tenderness, lymphadenopathy, or splenomegaly.
Fig. 1.
(A) Fiberoptic laryngoscopy revealed two yellowish masses located on the apices of both arytenoid cartilages. (B) Two month follow-up fiberoptic laryngoscopy revealed a nearly clean state.
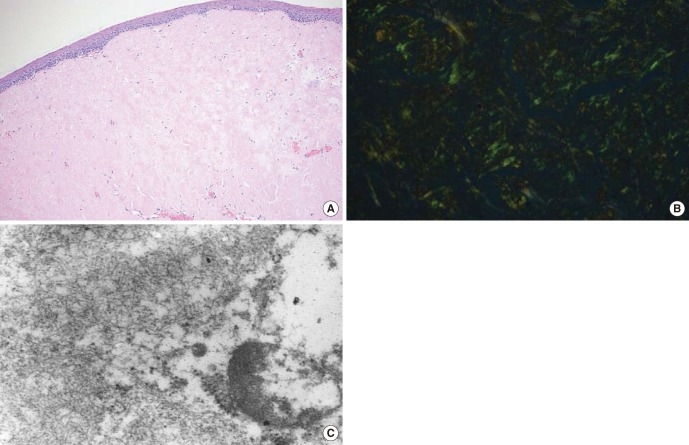
We proceeded to perform microlarygoscopy under general anesthesia and removal of the masses using a carbon dioxide laser. A biopsy specimen was obtained, and histopathologic analysis with Congo-red stain and electron microscopy confirmed the diagnosis of amyloidosis. On microscopy, acellular, eosinophilic, and amorphous materials were noted below the surface epithelium (Fig. 2A). Congo-red stain, under polarized microscopy, showed apple-green birefringence throughout the mass due to the presence of amyloid (Fig. 2B). Electron microscopy revealed the characteristic linear, non-branching, fibrillar amyloid materials (Fig. 2C).
Fig. 2.
(A) Subepithelial deposition of acellular, eosinophilic, and amorphous materials (H&E, ×200). (B) Amyloid was identified as Congo red-positive material with apple-green birefringence in polarized light. (C) Electron microscopy showed linear, non-branching, fibrillar amyloid materials.
Further examinations were done to rule out systemic amyloidosis or multiple myeloma. The patient's complete blood count, erythrocyte sedimentation rate, basic metabolic and biochemical panel and liver function test were within normal limits. Serum calcium and serum and urine β-2 microglobulin were also normal. Serum and urine electrophoresis were normal. Based on these results systemic amyloidosis and multiple myeloma were excluded from the differential diagnosis. A two month follow-up endoscopy revealed no scarring or recurrence (Fig. 1B).
DISCUSSION
Amyloidosis is a benign, slowly progressive disease that is characterized by the deposition of extracellular fibrillar, insoluble, proteinaceous material with a well-defined β-pleated sheet ultrastructure, which is mainly derived from the mesoderm [2]. Amyloidosis occurs twice as frequently in the larynx as in any other part of the head and neck, and is either tumor like or takes the form of diffuse infiltrates [3]. However, localized laryngeal amyloidosis is a rare, accounting for 0.2-1.2% of benign tumors of the larynx [4]. Lesions in the larynx are localized to the ventricle, false vocal cords, true vocal cords, aryepiglottic folds, and subglottis, in decreasing order of frequency [5]. In this case, amyloidosis invaded both arytenoid cartilages symmetrically, and the shape of the mass looked like a pair of boxer gloves. This form is as unique as ever reported. The other parts of the larynx were not invaded.
Amyloidosis is now classified as primary amyloidosis, myeloma-associated amyloidosis, localized amyloidosis (laryngeal), secondary amyloidosis, familial amyloidosis, senile amyloidosis, and dialysis-associated amyloidosis. In a large review, 70% of the cases were primary, 19% were localized, 4% were familial, and 3% were secondary [6]. The prognosis of systemic amyloidosis is worse than for the localized form [4]. In a prolonged follow-up of 43 patients with amyloidosis of the larynx and trachea, none of the patients developed systemic amyloidosis, B cell lymphoma or multiple myeloma. Nevertheless, a systemic workup is considered obligatory in every patient [7]. Regarding the requested laboratory control, in cases of localized laryngeal amyloidosis, Lewis et al. [8] studied 22 patients in the Mayo Clinic suffering from amyloidosis located exclusively in the larynx during the period 1950 to 1988 and recommended urine and serum electrophoresis as a basic initial approach. They did not recommend bowel and bone marrow biopsies as absolutely necessary. Our patient had no signs of systemic amyloidosis, such as lymphadenopathy, tender bones or splenomegaly. Serum and urine electrophoresis and abdominal ultrasonography showed normal patterns. Serum and urine β-2microglobulin were within normal limits.
The most common presenting symptoms of primary laryngeal amyloidosis are hoarseness, dysphonia and stridor. Dyspnea can also occur. Hemoptysis is an uncommon but potentially fatal complication caused by mucosal ulceration. Rarely, airway obstruction occurs and an alternative airway may be necessary. In this case, our patient had no laryngeal symptoms, because the masses were not too huge to obstruct air way and not extended to vocal cord anteriorly.
The "gold standard" for the diagnosis of amyloidosis is a tissue biopsy. Histology of the biopsied specimen using routine haematoxylin and eosin staining shows amyloid as eosinophilic extracellular infiltrate, sparing the overlying epithelium. Further staining with Congo red shows characteristic apple green birefringence and dichroism under a polarizing microscope. Staining with methyl violet discloses metachromatic pink-violet staining [4]. The differential diagnosis of a laryngeal mass includes benign and malignant tumors and non-neoplastic masses. These include laryngeal sarcoidosis, pseudotumor, lymphoma, chondrosarcoma, epidermoid cancer, laryngeal polyp, etc.
The computed tomographic appearance of laryngeal amyloidosis is nonspecific. The lesion looks like a submucosal, homogenous, nonenhanced mass. The magnetic resonance signal characteristic of laryngeal amyloidosis reveals intensity equal to that of the surrounding muscles on T1-weighted images and remains isointense or slightly hyperintense on T2-weighted images.
There is no effective medical treatment for laryngeal amyloidosis. Surgical treatment is the treatment of choice for laryngeal amyloidosis. We used a carbon dioxide laser for treatment. This laser approach is known to be more effective than conventional surgery because it minimizes scarring and trauma.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Vazquez de la Iglesia F, Sanchez Ferrandis N, Rey Martinez J, Ruba San Miguel D, Rama Lopez J, Fernandez Gonzalez S. Amyloidosis in the ORL field. Acta Otorrinolaringol Esp. 2006 Mar;57(3):145–148. doi: 10.1016/s0001-6519(06)78680-0. [DOI] [PubMed] [Google Scholar]
- 2.Kennedy TL, Patel NM. Surgical management of localized amyloidosis. Laryngoscope. 2000 Jun;110(6):918–923. doi: 10.1097/00005537-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Raymond AK, Sneige N, Batsakis JG. Amyloidosis in the upper aerodigestive tracts. Ann Otol Rhinol Laryngol. 1992 Sep;101(9):794–796. doi: 10.1177/000348949210100915. [DOI] [PubMed] [Google Scholar]
- 4.Thompson LD, Derringer GA, Wenig BM. Amyloidosis of the larynx: a clinicopathologic study of 11 cases. Mod Pathol. 2000 May;13(5):528–535. doi: 10.1038/modpathol.3880092. [DOI] [PubMed] [Google Scholar]
- 5.Daudia A, Motamed M, Lo S. Primary amyloidosis of the larynx. Postgrad Med J. 2000 Jun;76(896):364–365. doi: 10.1136/pmj.76.896.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chin SC, Fatterpeckar G, Kao CH, Chen CY, Som PM. Amyloidosis concurrently involving the sinonasal cavities and larynx. AJNR Am J Neuroradiol. 2004 Apr;25(4):636–638. [PMC free article] [PubMed] [Google Scholar]
- 7.Ergas D, Abramowitz Y, Lahav Y, Halperin D, Sthoeger ZM. Exertion dyspnea and stridor: an unusual presentation of localized laryngeal amyloidosis. Isr Med Assoc J. 2006 Jan;8(1):73–74. [PubMed] [Google Scholar]
- 8.Lewis JE, Olsen KD, Kurtin PJ, Kyle RA. Laryngeal amyloidosis: a clinicopathologic and immunohistochemical review. Otolaryngol Head Neck Surg. 1992 Apr;106(4):372–377. doi: 10.1177/019459989210600410. [DOI] [PubMed] [Google Scholar]