Abstract
A 56-year-old female with metastatic gallbladder cancer involving the liver and stenosis of the hilar bile duct was treated with gemcitabine (1,000 mg/m2) plus S-1 (60 mg/m2). After 9 cycles of therapy, CT showed evidence of stable disease; however, the serum CEA level was increased. Therefore, the chemotherapy regimen was changed to weekly low-dose paclitaxel (60 mg/m2). After 12 cycles of therapy, paclitaxel was reduced to 30 mg/m2 as the patient developed neutropenia. The patient completed 32 cycles of therapy, and the tumor was reduced in size and marked improvement in bile duct stenosis was noted without any impairment in quality of life. The patient succumbed to the disease 25 months after treatment was initiated. Thus, in this case paclitaxel was more effective than gemcitabine plus S-1. Palliative chemotherapy with paclitaxel after failure of gemcitabine and 5-FU was well-tolerated; therefore, it may be an effective treatment for biliary tract cancer (BTC). A phase I study of palliative chemotherapy with weekly low-dose paclitaxel following gemcitabine (plus cisplatin) and 5-FU is currently in progress in patients with unresectable or recurrent BTC.
Keywords: gallbladder cancer, biliary tract cancer, paclitaxel, palliative chemotherapy
Introduction
Biliary tract cancers (BTCs) include carcinomas of the gallbladder and intra- and extra-hepatic bile ducts (cholangiocarcinoma). Gallbladder cancer is the most common type of BTC, and it affects females more frequently than males. Gallbladder cancer is also considered to be the most aggressive type of BTC, with the shortest survival (1). Most BTCs are detected at an advanced, incurable stage, and are typically treated with chemotherapy drugs such as 5-FU, gemcitabine and cisplatin, often in combination. Response rates range from 20 to 40%, with a median overall survival of 8 to 14 months (1). The most notable advance in the treatment of BTC is the result of a phase III randomized trial of gemcitabine alone versus gemcitabine plus cisplatin; the chemotherapy doublet improved overall survival by 3.6 months (2). However, the median overall survival with gemcitabine plus cisplatin remains less than 1 year (11.7 months). In fact, there is no appropriate drug for third-line chemotherapy following gemcitabine (plus cisplatin) and 5-FU for BTC.
Paclitaxel is an anticancer agent (3) that acts by stabilizing polymerized microtubules and enhancing microtubule assembly, which arrests the cell cycle in the G0/S1 and G2/M phases and leads to cell death (4,5). Recent studies have shown that low-dose paclitaxel ameliorates tissue fibrosis by inhibiting TGF-β/Smad activity (6,7). Therefore, paclitaxel may be useful for treating BTC, a cancer that is associated with tissue fibrosis.
The present study documents the individual response of a patient with gallbladder cancer with multiple liver metastasis and stenosis of the bile duct who was treated with low-dose paclitaxel as palliative chemotherapy following gemcitabine and S-1 (oral prodrug of 5-FU).
Case report
A 56-year-old woman in good health was admitted to our hospital with right upper quadrant pain. Physical examination was notable for right upper quadrant tenderness and hepatomegaly. CT of the abdomen revealed multiple hepatic nodules, a thick gallbladder wall and dilation of the intrahepatic bile duct (Fig. 1A). CEA was 14.3 IU/ml (upper limit of normal, 5.0 IU/ml) and CA19-9 was 58 IU/ml (upper limit of normal, 37 IU/ml). The patient was diagnosed with unresectable gallbladder cancer with multiple liver metastasis and local infiltration to the liver and hilar bile duct (Fig. 2A).
Figure 1.
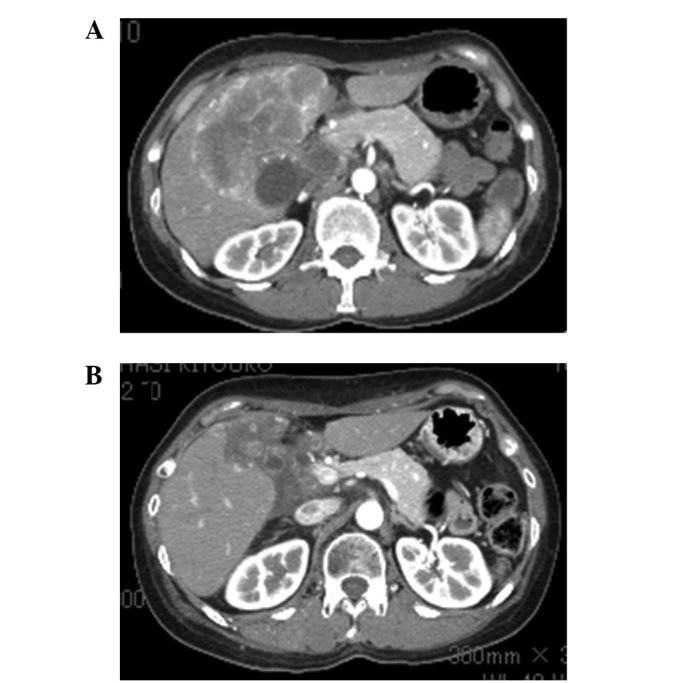
Abdominal CT (A) before and (B) after treatment. (A) Abdominal CT showing a large gallbladder tumor infiltrating the liver and liver metastasis. (B) The tumor size was reduced following chemotherapy with low-dose paclitaxel.
Figure 2.
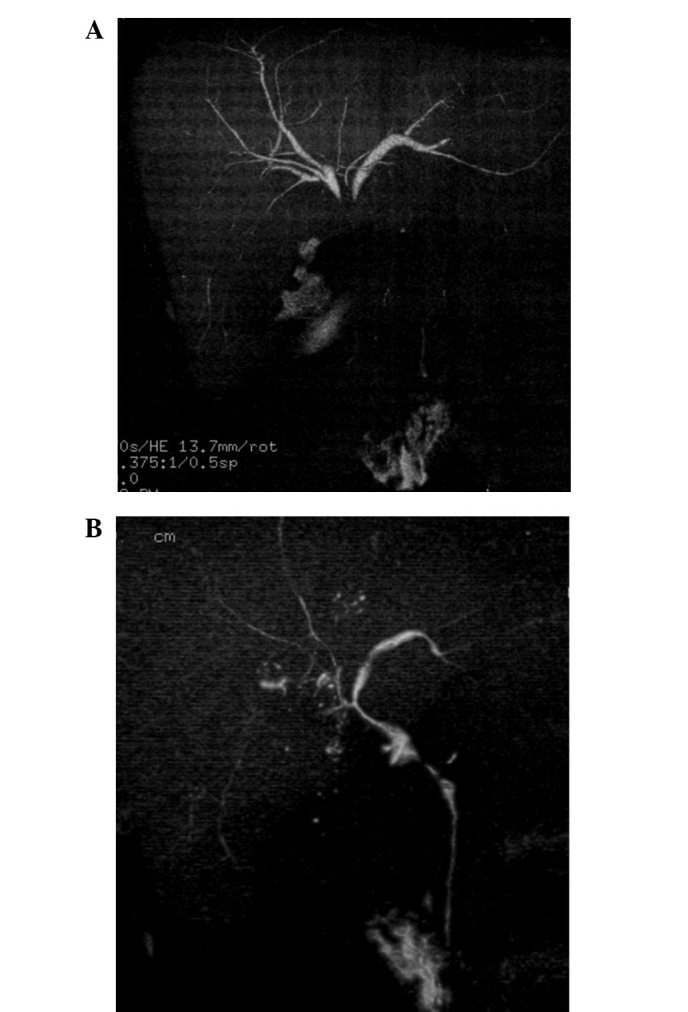
Drip-infusion cholangiography (DIC)-CT (A) before and (B) after treatment. (A) DIC-CT showing stenosis of the hilar bile duct. (B) Stenosis of the hilar bile duct improved following the administration of low-dose paclitaxel and radiation.
The patient was treated with oral S-1 (60 mg/m2) twice daily for 14 days plus gemcitabine (800 mg/m2) administered on days 8 and 14 [every 21 days as previously described for pancreatic carcinoma (8)]. After 4 cycles of therapy, the doses were reduced as the patient developed neutropenia. After 9 cycles of therapy, CT showed evidence of stable disease; however, the serum CEA level was increased (Fig. 3). Therefore, the chemotherapy regimen was changed to weekly paclitaxel (60 mg/m2). After 12 cycles of therapy, paclitaxel was reduced to 30 mg/m2 due to neutropenia. The patient completed 32 cycles of paclitaxel therapy and CT showed evidence of a partial response (Fig. 1B) and stenosis of the hilar bile duct was improved (Fig. 2B). At the beginning of paclitaxel therapy, irradiation of the stenotic hilar bile duct was performed. The toxicities evaluated were leucopenia (grade 2), general malaise (grade 1) and shedding of hair; however, no serious adverse events were observed. Therefore, the patient was treated at the outpatient clinic, without any impairment in the quality of life (QOL).
Figure 3.
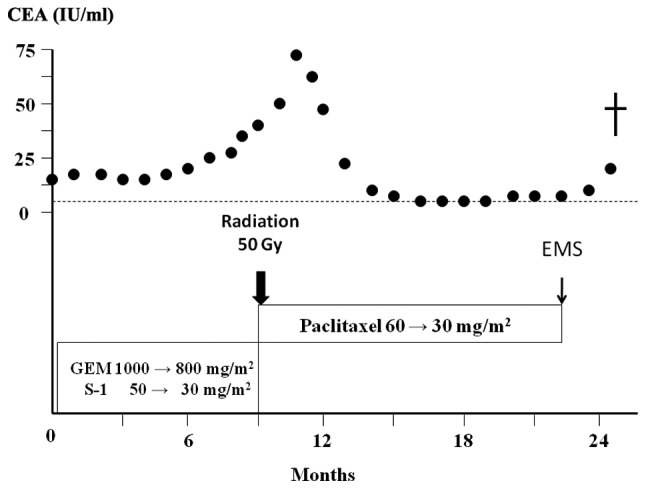
Clinical course of the patient. The patient’s treatment started with gemcitabine plus S-1. After 9 months of treatment, the serum CEA level increased; therefore, weekly low-dose paclitaxel administration was started. The patient was treated with paclitaxel for approximately 14 months. EMS: expandable metallic stent.
Written informed consent was obtained from the patient, and the treatment was undertaken with the approval of the Local Ethics Committee of Kanazawa University Hospital.
Endoscopic biliary drainage and expandable metallic stent placement was performed for obstructive jaundice due to lymph node metastasis 23 months after beginning treatment. The patient was then diagnosed with pancreaticobiliary maljunction (Fig. 4). The patient succumbed to the disease due to the progress of cachexia 25 months after the first visit. An autopsy was performed, and the patient was diagnosed with locally advanced, poorly differentiated adenocarcinoma of the gallbladder with multiple liver, lung, lymph node, left ovary and skin metastases.
Figure 4.
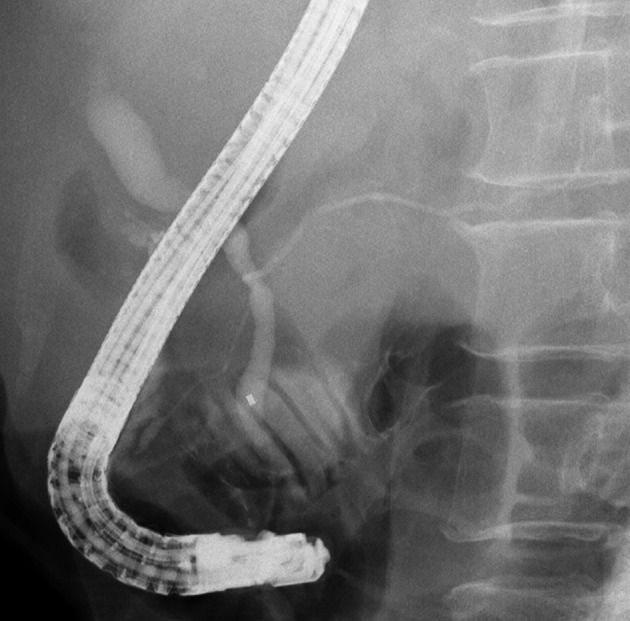
Endoscopic retrograde cholangiography showing that the main pancreatic duct had joined the common bile duct.
Discussion
The prognosis of patients with unresectable BTC is extremely poor. No standard chemotherapy was established for patients with unresectable BTC until the study of cisplatin plus gemcitabine by Valle et al (2). However, the median overall survival of patients treated with cisplatin plus gemcitabine was only 11.7 months. 5-FU is a major drug used in the treatment of hepatobiliary-pancreatic cancers; however, phase II studies using combinations primarily based on 5-FU regimens have revealed little or no benefit on survival and QOL (9,10). S-1 is an oral prodrug of 5-FU widely used in Japan (8). In a phase III trial (the GEST trial) announced by the American Society of Clinical Oncology in 2011, S-1 produced a favorable response and was not inferior to gemcitabine in terms of the overall survival of patients with unresectable pancreatic cancer (11). However, there is no appropriate drug for third-line chemotherapy following gemcitabine (plus cisplatin) and 5-FU for BTC.
Paclitaxel is a natural substance isolated from the western yew, Taxus brevifolia. Similar to the vinca alkaloids, it binds to microtubules. However, while the vinca alkaloids promote microtubule dissociation and disruption of the mitotic spindle, paclitaxel promotes microtubule formation and stabilization. There have been some retrospective studies and phase I and II studies of paclitaxel and docetaxel (taxanes) for pancreatic cancer and BTC (12–17). The disease control rates in these studies were 33 to 57% when used as first-line chemotherapy.
Recently, paclitaxel has been receiving attention for its effects other than antitumor activity; for example, its use in drug-eluting stents in coronary arteries (18). Moreover, it has been reported that paclitaxel ameliorates fibrosis in hepatic stellate cells and renal fibrosis through the inhibition of TGF-β/Smad activity (6,7). Paclitaxel also interrupts TGF-β1 signaling between gallbladder epithelial cells and myofibroblasts (19). Taghian et al reported that paclitaxel decreases interstitial fluid pressure and improves oxygenation in breast cancer tissues in patients treated with neoadjuvant chemotherapy and that patients with hypoxic tumors and/or tumors with high interstitial fluid pressure may start with paclitaxel chemotherapy to improve their physiological status (20). Pancreatic cancer and BTC are well-known hypoxic tumors associated with fibrosis. Therefore, taxanes may be effective in the treatment of pancreatic cancer and BTC.
Certain studies have also documented taxane chemotherapy in patients with gemcitabine-refractory pancreatic cancer (21,22). Cancer cells experience various forms of stress from anticancer drugs, irradiation, hypo-oxygenation, hypo-nutrition and heat treatment, and these stresses induce epithelial-to-mesenchymal transition (EMT), which is associated with the invasive potential of cancer cells (23). The inhibitory effect of paclitaxel on TGF-β/Smad activity is involved in the suppression of EMT in epithelial cells.
In the present case, paclitaxel was more effective than gemcitabine and S-1 for unresectable gallbladder cancer. Furthermore, paclitaxel has fewer side-effects; therefore, it should be suitable as a palliative chemotherapy for BTC as has been reported for breast cancer (24). In conclusion, palliative chemotherapy with paclitaxel after failure of gemcitabine and 5-FU is well-tolerated and may be effective for BTC. However, the appropriate dose of these anticancer drugs should be determined in a future study. A phase I study of palliative chemotherapy with weekly low-dose paclitaxel following gemcitabine (plus cisplatin) and 5-FU is currently in progress in patients with unresectable or recurrent BTC.
References
- 1.Xiu AX, Hong TS, Hezel AF, Kooby DA. Current management of gallbladder carcinoma. Oncologist. 2010;15:168–181. doi: 10.1634/theoncologist.2009-0302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valle JW, Wasan H, Palmer DH et al. ABC-02 Trial Investigators: Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362:1273–1281. doi: 10.1056/NEJMoa0908721. [DOI] [PubMed] [Google Scholar]
- 3.Gelmon K. The toxoids: paclitaxel and docetaxel. Lancet. 1994;344:1267–1272. doi: 10.1016/s0140-6736(94)90754-4. [DOI] [PubMed] [Google Scholar]
- 4.Donaldson KL, Goolsby GL, Kiener PA, Wahl AF. Activation of p34cdc2 coincident with taxol-induced apoptosis. Cell Growth Differ. 1994;5:1041–1050. [PubMed] [Google Scholar]
- 5.Schiff PB, Fant J, Horwitz SB. Promotion of microtubule assembly in vitro by taxol. Nature. 1979;277:665–667. doi: 10.1038/277665a0. [DOI] [PubMed] [Google Scholar]
- 6.Zhang D, Sun L, Xian W, Liu F, et al. Low-dose paclitaxel ameliorates renal fibrosis in rat UUO model by inhibition of TGF-beta/Smad activity. Lab Invest. 2010;90:436–447. doi: 10.1038/labinvest.2009.149. [DOI] [PubMed] [Google Scholar]
- 7.Zhou J, Zhong DW, Wang QW, Miao XY, Xu XD. Paclitaxel ameliorates fibrosis in hepatic stellate cells via inhibition of TGF-beta/Smad activity. World J Gastroenterol. 2010;16:3330–3334. doi: 10.3748/wjg.v16.i26.3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tajima H, Ohta T, Kitagawa H, et al. Pilot study of neoadjuvant chemotherapy with gemcitabine and oral S-1 for resectable pancreatic cancer. Exp Therap Med. 2012;3:787–792. doi: 10.3892/etm.2012.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ellis PA, Norman A, Hill A, O’Brien ME, Nicolson M, Hickish T, Cunningham D. Epirubicin, cisplatin and infusional 5-fluorouracil (5-FU) (ECF) in hepatobiliary tumors. Eur J Cancer. 1995;31A:1594–1598. doi: 10.1016/0959-8049(95)00323-b. [DOI] [PubMed] [Google Scholar]
- 10.Patt YZ, Jones DV, Jr, Hoque A, Lozano R, Markowitz A, Raijman I, Lynch P, Charnsangavej C. Phase II trial of intravenous fluorouracil and subcutaneous interferon alfa-2b for biliary tract cancer. J Clin Oncol. 1996;14:2311–2315. doi: 10.1200/JCO.1996.14.8.2311. [DOI] [PubMed] [Google Scholar]
- 11.Ioka T, Ikeda M, Ohkawa S, et al. Randomized phase III study of gemcitabine plus S-1 (GS) versus S-1 versus gemcitabine (GEM) in unresectable advanced pancreatic cancer (PC) in Japan and Taiwan: GEST study. J Clin Oncol. 2011;29(Suppl) doi: 10.1200/JCO.2012.43.3680. abstr 4007. [DOI] [PubMed] [Google Scholar]
- 12.Papakostas P, Kouroussis C, Androulakis N, et al. First-line chemotherapy with docetaxel for unresectable or metastatic carcinoma of the biliary tract. A multicentre phase II study. Euro J Cancer. 2001;37:1833–1838. doi: 10.1016/s0959-8049(01)00214-3. [DOI] [PubMed] [Google Scholar]
- 13.Okada S, Sakata Y, Matsuno S, et al. Phase II study of docetaxel in patients with metastatic pancreatic cancer: a Japanese cooperative study. Cooperative Group of Docetaxel for Pancreatic Cancer in Japan. Br J Cancer. 1999;80:438–443. doi: 10.1038/sj.bjc.6690375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ryan DP, Kulke MH, Fuchs CS, et al. A Phase II study of gemcitabine and docetaxel in patients with metastatic pancreatic carcinoma. Cancer. 2002;94:97–103. doi: 10.1002/cncr.10202. [DOI] [PubMed] [Google Scholar]
- 15.Jones DV, Jr, Lozano R, Hoque A, Markowitz A, Patt YZ. Phase II study of paclitaxel therapy for unresectable biliary tree carcinomas. J Clin Oncol. 1996;14:2306–2310. doi: 10.1200/JCO.1996.14.8.2306. [DOI] [PubMed] [Google Scholar]
- 16.Maeda S, Motoi F, Onogawa T, et al. Paclitaxel as second-line chemotherapy in patients with gemcitabine-refractory pancreatic cancer: a retrospective study. Int J Clin Oncol. 2011;16:539–545. doi: 10.1007/s10147-011-0220-8. [DOI] [PubMed] [Google Scholar]
- 17.Von Hoff DD, Ramanthan RK, Borad MJ, et al. Gemcitabine plus nab-paclitaxel is an active regimen in patients with advanced pancreatic cancer: a phase I/II trial. J Clin Oncol. 2011;29:4548–4554. doi: 10.1200/JCO.2011.36.5742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baek I, Bai CZ, Hwang J, Nam HY, Park JS, Kim DJ. Paclitaxel coating of the luminal surface of hemodialysis grafts with effective suppression of neointimal hyperplasia. J Vasc Surg. 2012;55:806–814. doi: 10.1016/j.jvs.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 19.Choi HS, Savard CE, Choi JW, Kuver R, Lee SP. Paclitaxel interrupts TGF-beta1 signaling between gallbladder epithelial cells and myofibroblasts. J Surg Res. 2007;141:183–191. doi: 10.1016/j.jss.2006.12.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taghian AG, Abi-Raad R, Assaad SI, et al. Paclitaxel decreases the interstitial fluid pressure and improves oxygenation in breast cancer in patients treated with neoadjuvant chemotherapy: clinical implications. J Clin Oncol. 2005;23:1951–1961. doi: 10.1200/JCO.2005.08.119. [DOI] [PubMed] [Google Scholar]
- 21.Shukuya T, Yasui H, Boku N, et al. paclitaxel after failure of gemcitabine in pancreatic cancer patients with malignant ascites: a retrospective study. Jpn J Clin Oncol. 2010;40:1135–1138. doi: 10.1093/jjco/hyq117. [DOI] [PubMed] [Google Scholar]
- 22.Cereda S, Reni M. Weekly docetaxel as salvage therapy in patients with gemcitabine-refractory metastatic pancreatic cancer. J Chemother. 2008;20:509–512. doi: 10.1179/joc.2008.20.4.509. [DOI] [PubMed] [Google Scholar]
- 23.Tajima H, Ohta T, Shoji Y, et al. Expression of epithelial-mesenchymal transition markers in locally recurrent hepatocellular carcinoma after radio frequency ablation. Exp Therap Med. 2010;1:347–350. [Google Scholar]
- 24.Schrama JG, de Boer MM, Baars JW, Schornagel JH, Rodenhuis S. Palliative chemotherapy after failure of high-dose chemotherapy in breast cancer - toxicity and efficacy. Anticancer Res. 2003;23:2795–2800. [PubMed] [Google Scholar]


