Abstract
Glomus tumors are uncommon lesions of glomus cell origin with ultrastructural and immunohistochemical features of smooth muscle. In the majority of the cases reported in the literature glomus tumors are benign, but there are some rare cases in which they demonstrate aggressive and malignant clinical and histological features. Glomangiosarcomas of the lung are extremely rare malignant tumors, because of the fact that glomus bodies are rare or absent. Due to their rarity they are misdiagnosed. Surgical resection is considered to be the most effective treatment for this condition. We report a case of a 35 year old female with a pulmonary glomangiosarcoma.
KEY WORDS : Glomangiosarcoma, misdiagnosis, surgical resection
Introduction
Glomus tumors are uncommon lesions of glomus cell origin with ultrastructural and immunohistochemical features of smooth muscle (1,2). These tumors occur either as solitary or as multiple lesions of the dermis or the subcutis with subungual location. It is less common for glomus tumors to appear in the mediastinum and the respiratory tract including the lungs. Among the organs of the respiratory tract the most common location, where they appear is the trachea (3,4). In the majority of the cases reported in the literature glomus tumors are benign, but there are some rare cases in which they demonstrate aggressive and malignant clinical and histological features (4). Conventionally, glomous tumors are divided into the following three general categories: locally infiltrative glomus tumors, glomangiosarcomas arising within a glomus tumor and de novo glomangiosarcoma (5). We report a case of a 35 years old female with a pulmonary glomangiosarcoma.
Case presentation
A female patient born in 1977 appeared to the emergency room of our hospital referring hemoptisis. The patient had a medical history of a mass in the left hilum of the lung (Figure 1). This mass was first discovered in 1996, when the patient was admitted to the hospital referring thoracic pain. The patient was advised to be submitted in surgical resection of the mass, which was considered to be either a teratoma or a dermoid cyst, due to its location in the anterior mediastinum. The patient refused the surgery and since then the mass was under surveillance with computer tomography of the thorax, every year (Figure 2). In order to search the cause of hemoptisis a new CT of the thorax was performed, which revealed new lesions, located not only in the left hilum of the lung but also in the left lung as well (Figure 3). After the CT a TBNA was performed and the histological analysis showed a glomangiosarcoma of the left lung (Figures 4,5). The patient was submitted to a pneumonectomy of the left lung and resection of eight lymph nodes. Pericardiectomy and reconstruction of the pericardium was also performed. The histological analysis of the surgical specimens revealed metastatic lesions in the resected lymph nodes and the left lung. The surgical limits were disease free.
Figure 1.
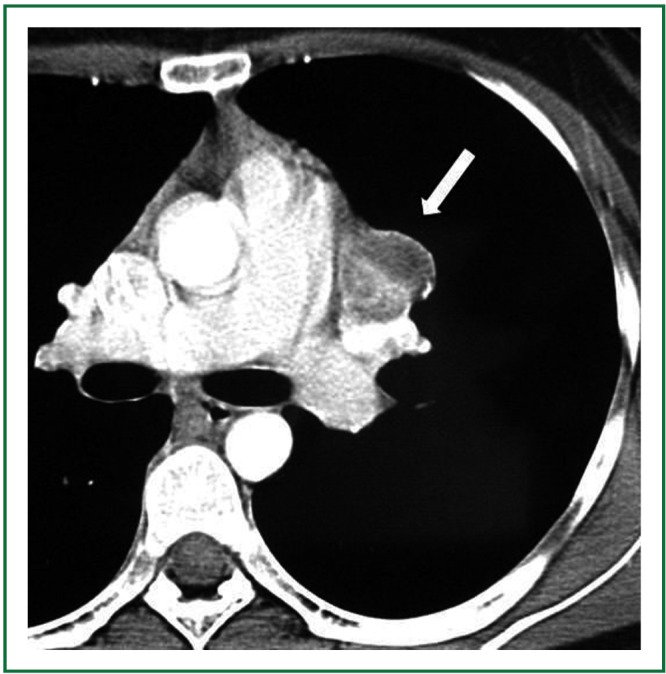
Axial CT image of the mediastinum demonstrates an inhomogeneously enhancing lesion close to the pulmonary trunk and the left pulmonary artery (arrow). The lesion corresponds to a mediastinal angiosarcoma.
Figure 2.
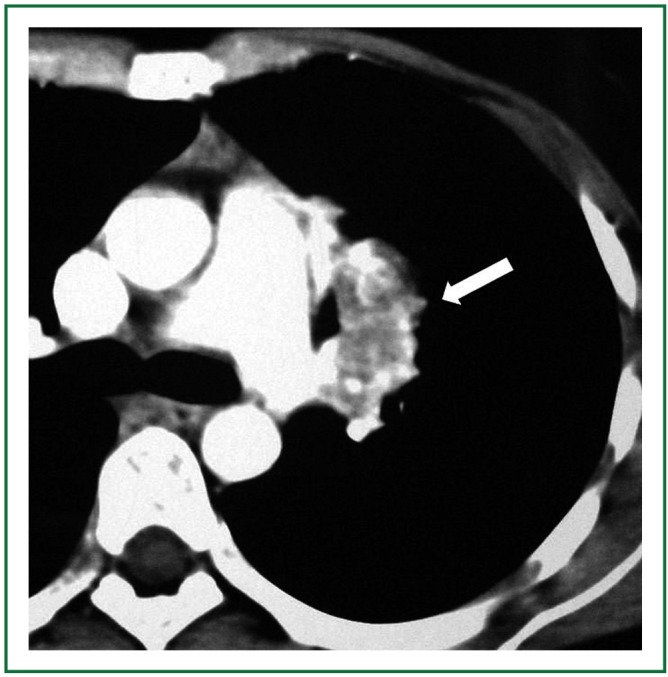
Six years later, an axial CT image of the mediastinum reveals enlargement of the angiosarcoma which enhances more intensively.
Figure 3.
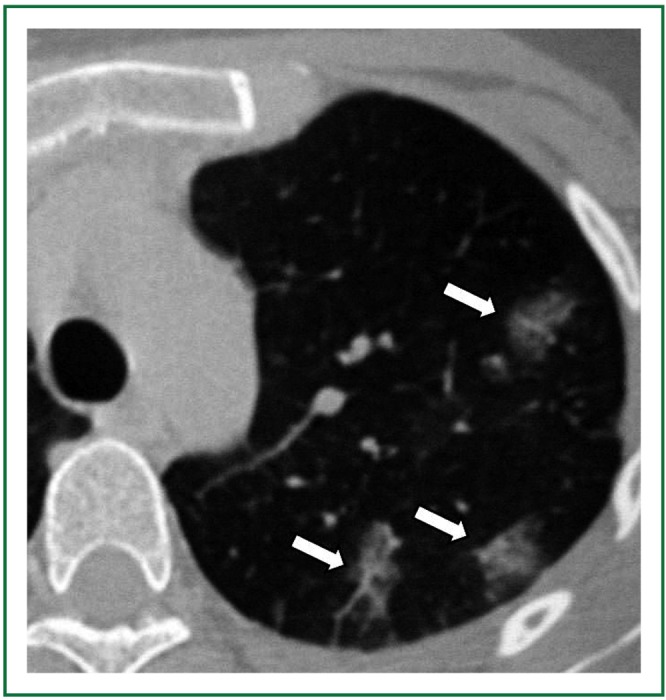
Axial CT image of the left lung shows three “ground glass” opacity areas in the parenchyma corresponding to mediastinal angiosarcoma metastases (arrows).
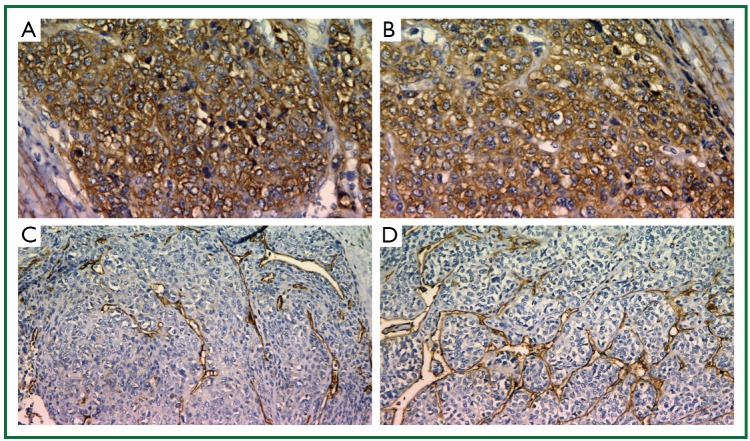
Figure 4.
A-B. Actin shows the myoepithelial nature of a glomus tumor; C-D. It is an exclusion diagnosis (CD31, CD34 - exclusion of primary angiosarcoma and fibromatous carcinoma of the pleura or the mediastinum)
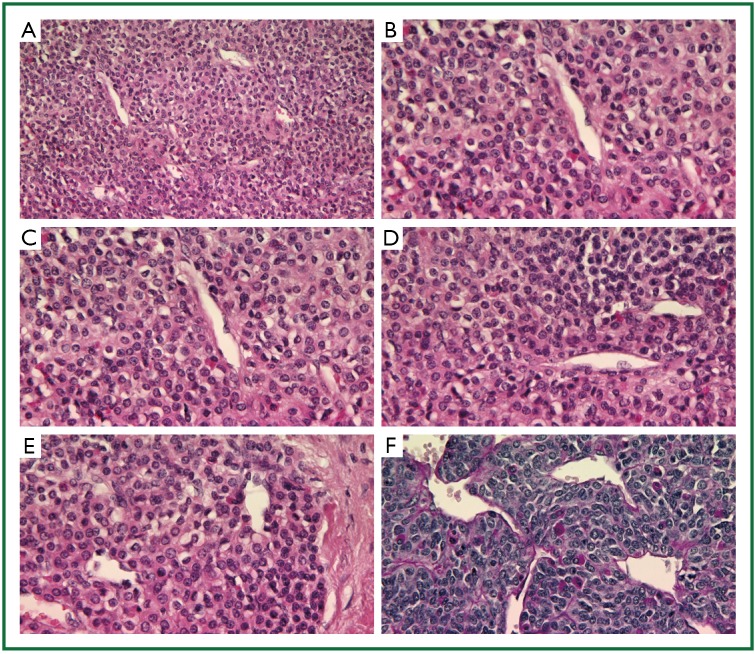
Figure 5.
A-E. HE shows the oncolytic sharp demasked nucleoli (typical appearance); F. PAS shows the scatter/network of basalmembran around the cells (typical)
Discussion
Glomangiosarcomas of the lung are extremely rare malignant tumors, because of the fact that glomus bodies are rare or absent (6). The exact incidence of these tumors is unknown. Glomus tumors can appear either as single or as multiple lesions. The single glomus tumors are more frequent in adults in comparison with other age groups. On the contrary, multiple glomus tumors appear ten to fifteen years earlier than solitary ones and more specifically one third of these cases occur before the twentieth year of life. Congenital glomus tumors are rare and they are considered to be a subtype of multiple glomus tumors (7). Glomangiosarcomas are by convention subdivided into two categories: glomangiosarcomas arising in a glomus tumor and de novo glomangiosarcoma. The difference is determined by the presence or the absence of a benign glomus tumor. Malignant glomus tumors associated with benign lesions are obviously easier to recognize and generally manifest by focal “spindling” of cells with cytologic malignancy. These malignant areas have molecular abnormalities that are not present in the surrounding glomocytes, including increased BCL-2 and p53 expression (4,8). On the contrary de novo glomangiosarcoma is more difficult to be diagnosed; as its diagnosis minimally requires recognition of histologic or ultrastructural features reminiscent of glomus tumors (4). Additionally they demonstrate malignant histologic features, including cytologic atypia, necrosis, elevated mitotic rate, and characteristically cystic degeneration (9). Glomangiosarcomas generally have an increased risk of local recurrence (5). As a result of their rarity glomangiosarcomas are misdiagnosed as hemangiomas or venous malformations (10,11). The proper treatment for these malignancies is surgical resection of the tumor with really good results (4,12).
Glomus tumors and particularly glomangiosarcomas are extremely rare tumors of the lung. These tumors are often misdiagnosed, as a result of their rarity and the variety of the clinical symptoms that patients with those lesions appear. The location of these tumors as well as their early diagnosis is of great importance for the prognosis of the disease. Surgical resection is considered to be the most effective treatment for this condition.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Murad TM, von Haam E, Murthy MS. Ultrastructure of a hemangiopericytoma and a glomus tumor. Cancer 1968;22:1239-49 [DOI] [PubMed] [Google Scholar]
- 2.Venkatachalam MA, Greally JG. Fine structure of glomus tumor: similarity of glomus cells to smooth muscle. Cancer 1969;23:1176-84 [DOI] [PubMed] [Google Scholar]
- 3.Heard BE, Dewar A, Firmin RK, et al. One very rare and one new tracheal tumour found by electron microscopy: glomus tumour and acinic cell tumour resembling carcinoid tumours by light microscopy. Thorax 1982;37:97-103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaertner EM, Steinberg DM, Huber M, et al. Pulmonary and mediastinal glomus tumors--report of five cases including a pulmonary glomangiosarcoma: a clinicopathologic study with literature review. Am J Surg Pathol 2000;24:1105-14 [DOI] [PubMed] [Google Scholar]
- 5.Gould EW, Manivel JC, Albores-Saavedra J, et al. Locally infiltrative glomus tumors and glomangiosarcomas. A clinical, ultrastructural, and immunohistochemical study. Cancer 1990;65:310-8 [DOI] [PubMed] [Google Scholar]
- 6.De Cocker J, Messaoudi N, Waelput W, et al. Intrapulmonary glomus tumor in a young woman. Interact Cardiovasc Thorac Surg 2008;7:1191-3 [DOI] [PubMed] [Google Scholar]
- 7.Kleontas A, Barbetakis N, Asteriou C, et al. Primary glomangiosarcoma of the lung: A case report. J Cardiothorac Surg 2010;5:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hegyi L, Cormack GC, Grant JW. Histochemical investigation into the molecular mechanisms of malignant transformation in a benign glomus tumour. J Clin Pathol 1998;51:872-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi YJ, Yang KH, Gang SJ, et al. Malignant glomus tumor originating in the superior mediastinum--an immunohistochemical and ultrastructural study. J Korean Med Sci 1991;6:157-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ruben RJ. The history of the glomus tumors - nonchromaffim chemodectoma: a glimpse of biomedical Camelot. Acta Otolaryngol 2007;127:411-6 [DOI] [PubMed] [Google Scholar]
- 11.Yen A, Raimer SS. Multiple painful blue nodules. Multiple glomus tumors (glomangiomas). Arch Dermatol 1996;132:704-5, 707-8 [DOI] [PubMed] [Google Scholar]
- 12.Takahashi N, Oizumi H, Yanagawa N, et al. A bronchial glomus tumor surgically treated with segmental resection. Interact Cardiovasc Thorac Surg 2006;5:258-60 [DOI] [PubMed] [Google Scholar]