Abstract
Although progress has been made to reduce global incidence of drug-susceptible tuberculosis, the emergence of multidrug-resistant (MDR) and extensively drug-resistant (XDR) tuberculosis (TB) during the past decade threatens to undermine these advances. XDR-TB has been found to be associated with scarce therapeutic options and high mortality rates. We describe the first case of XDR-TB cured by percutaneous lung puncture and with post-hospital 4 years follow-up involving radiologic imaging and septum smear and TB culture. We also review the epidemiology, diagnosis and treatment of tuberculosis all the world.
KEY WORDS : Multidrug-resistant (MDR), extensively drug-resistant (XDR), extensively drug-resistant tuberculosis (XDR-TB), percutaneous lung puncture, chemotherapy
Case summary
The patient, female, 24 y.o., nurse. She was admitted to our department in January 4th, 2007 due to two-year interrupted cough and half-month night sweating. The patient was diagnosed as primary mutli-drug resistant pulmonary tuberculosis two years ago, and received branchofiberoscope intervention therapy for 15 times during twice hospitalization, and administered with isoniazid (0.2 g) and amikacin (0.4 g) each time. In the process of 18 months of immune treatment with mycobacterium vaccae vaccine (22.5 μg each time, once a week in former three months, and then once two weeks, until once a month in the last six months) in combination with traditional Chinese therapy, the patient turned better and was discharged. The hospitalization period was 222 days in total. Soon after discharge, the septum bacteria test results changed to be positive, and the lung cavity size became larger. The septum tuberculosis bacteria culture and drug sensitive experiment indicated extensively drug-resistant tuberculosis (XDR-TB), which was highly resistant to isoniazid, rifampicin, streptomycin, paraminosalicylic acid, and medium to levofloxacin, lectra lung disease, capreomycin and ethambutol. The girl was depressed and pessimistic. Without any other effective methods, we performed percutaneous lung puncture, through which the isoniazid (0.1 g each time), amikacin (0.4 g each time) was perfused. One course later (10 times), the patient’s symptoms released and septum bacteria test results turned to negative, the cavity gradually decreased (Figures 1,2). Continuing treatment for 3 months in hospital (3PaEVATh/9PaETh therapy), the patient discharged (Figure 3). After 9 months, Chest-CT showed cavity closure (Figure 4), and patient medication stopped three months later since then. At present, the patient was followed up for 4 years, and multiple septum smear and TB culture results were all negative. She has gained weight (about 5 kg) during the last four years, and has been married now.
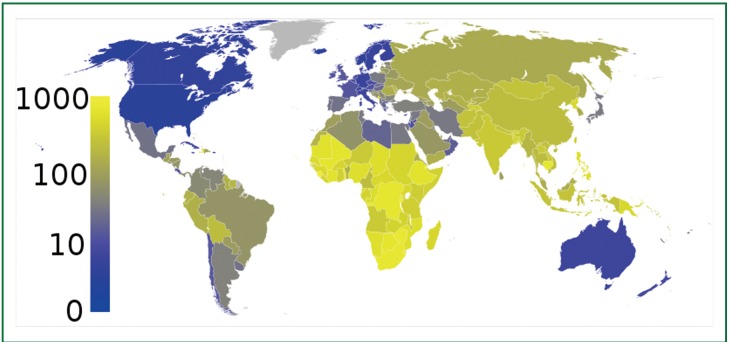
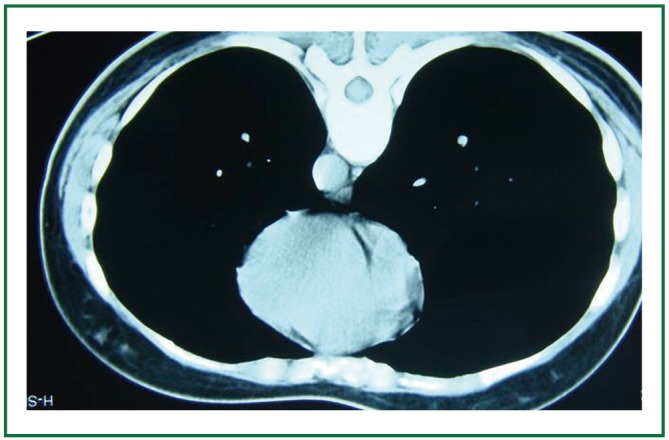
Figure 1.
The first injection of puncture, cavity shown in CT mediastinal window, plural lesion in the back of right upper lobe (January 9th, 2007).
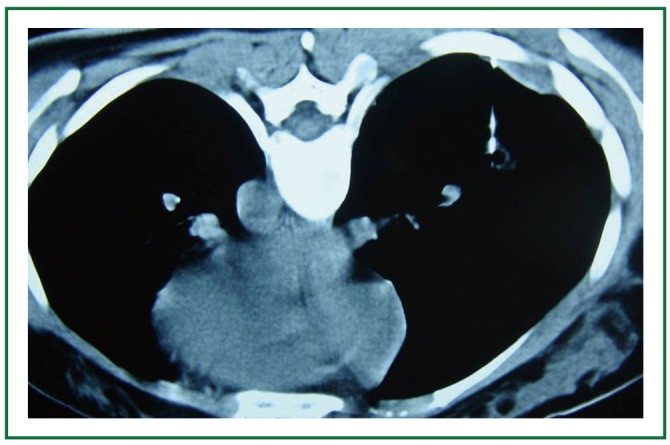
Figure 2.
The fifth injection of puncture, cavity decreased in CT mediastinal window, plural lesion disappeared (February 6th, 2007).
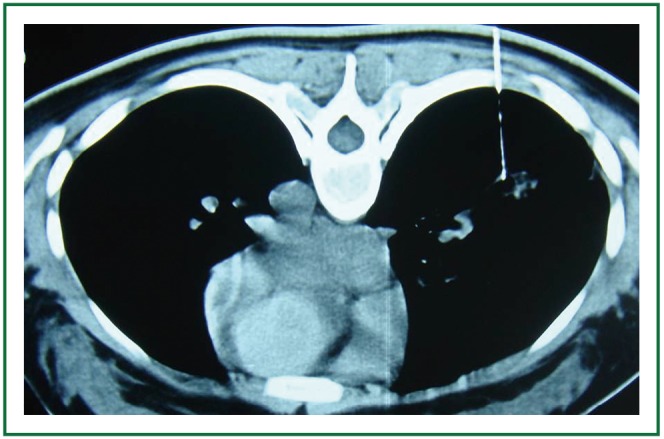
Figure 3.
The tenth injection of puncture, The puncture needle was pointed in the lesion in CT lung window (however in CT mediastinal window cavity disappeared, figure was not showed) (March 20th, 2007).
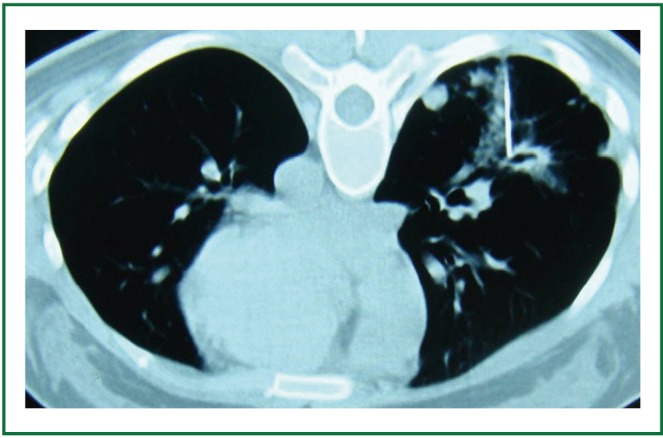
Figure 4.
Six months after discharge, cavity disappeared and lesion calcified in Chest reexamination (October 10th, 2007).
Discussion
Multiple-drug resistant cavitary pulmonary tuberculosis is the common difficulty and most threaten TB source of infection, which constitutes of the serious threat to TB control plan. Unfortunately, extensive drug-resistant TB was detected not only anti-isoniazid and rifampicin, but also secondary anti-TB drugs (capreomycin, kanamycin, amikacin) and fluoroquinolones, making it to be the “incurable” disease. Since 1997, we have investigated the percutaneous lung puncture protocol and achieved better outcomes in treating each kind of hard-to-treat tuberculosis including chronic cavitary pulmonary TB (1), MDR-TB (2) and pulmonary tuberculoma (3).
The protocol of percutaneous lung puncture was following: the position, puncture point and depth was determined under the guidance of CT. 2% Lidocaine (5 mL) was used for local anesthesia. 22 G lung puncture needle was selected, and pointed in the cavity after CT determination to inject isoniazid (0.1 g), amikacin (0.2 g). CT scan was performed after needle expelling to exclude pneumothorax. The patient was asked to lie down for two hours after operation. The protocol was repeated once a week, tenth as a course.
The XDR-TB in this case derived from originated multiple drug resistant tuberculosis (MDR-TB), and had no satisfactory results due to drug resistance in spite of regular anti-TB treatment. The characteristic of that disease is fibrosis cavity, where TB amount is about 1×107-1×109, and at their active growth stage (1). Routine administration could not infiltrate to cavity because of barrier effect of fibrosis cavity and surrounding vessels’ closure. In this way, the minimum inhibitory concentration (MIC) could not be achieved, and septum bacteria test is hard to be negative. However, percutaneous lung puncture could inject the drug directly to the cavity and lesion, letting drug kill the TB and making the local concentration reach tens and hundreds times than aforementioned MIC. The drugs eroded the cavity wall and accelerated the excretion of cheese lesions. Multiple injects might reduce the barrier effect of cavity and the drug could infiltrate to surrounding lesions through needle canal, which would facilitate the granulation tissue rehabilitation and cavity purification.
Isoniazid is the first-line general fungicides, with low molecular weight, high infiltration ability, less side effects, thus is the first-of-choice for TB. Amikacin is a highly-efficient antibacterial drug, and it has similar effect to aminoglycoside antibiotics resistant bacteria with lesser side effects compared to streptomycin and kanamycin. Therefore, the combination of isonizid and amikacin is more ideal.
The cure standard for MDR-TB was defined as continuous septum culture negative results at least for five times during the last 12 months of treatment process, with each interval for 30 days. The patient not only met above criteria, and septum smear and TB culture results all were negative during 4 years of follow up, which meant totally cure. Presently, it’s still lack of valid chemotherapy to XDR-TB and novel anti-TB drugs, thus making the choice limited for physicians and the chemotherapy schedule could only base on principles of MDR-TB, resulting in therapy course over 24 months. By the mean of lung puncture, only one year is enough. Our case also demonstrates that staffs in hospital are belongs to XDR-TB susceptible population, which needs to be cautioned.
Tang et al. reported (4) the prevalence, clinical characteristics and treatment outcomes of XDR-TB and found that 126/1,156 (10.9%) were XDR-TB in a specialist TB hospital in Shanghai and the clinical treatment outcome of XDR-TB is usually very poor. We are devoted to explored XDR-TB therapy for several years and firstly applied percutaneous lung puncture to injected anti-TB drugs directly to the lesion of XDR-TB and more importantly the septum smear and TB culture results all were negative during 4 years of follow up.
Epidemiology
Tuberculosis (TB) is caused by a bacterium called Mycobacterium tuberculosis. The bacteria usually attack the lungs, but can attack any part of the body such as the kidney, spine, and brain. If not treated properly, TB can be fatal. It is spread through the air from one person to another. The TB bacteria are released into the air when a person with TB in the lungs or throat coughs, sneezes, speaks, or sings. People nearby may inhale the bacteria and become infected.
One-third of the world’s population is thought to have been infected with M. tuberculosis (5,6), and new infections occur at a rate of about one per second (5). In 2007 there were an estimated 13.7 million chronic active cases (6), and in 2010 an estimated 8.8 million new cases, and 1.45 million deaths; mostly in developing countries (7). The absolute number of tuberculosis cases has been decreasing since 2006 and the number of new cases has been decreasing since 2002 (8). More people in the developing world contract tuberculosis because their immune systems are more likely to be compromised by AIDS (9). China has achieved particularly dramatic progress in controlling TB, with an 80% decline in the national TB case-fatality rate (10). The distribution of tuberculosis is not uniform across the globe; about 80% of the population in many Asian and African countries test positive in tuberculin tests, while only 5-10% of the United States population test positive (11).
In developed countries, tuberculosis is less common and mainly an urban disease. In the United Kingdom, the national average prevalence rate was 15 per 100,000 in 2007, and the highest incidence rate in Western Europe was 30 per 100,000 in Portugal and Spain. These rates compare with 98 per 100,000 in China and 48 per 100,000 in Brazil. In the United States, the overall tuberculosis prevalence rate was 4 per 100,000 persons in 2007 (Figure 5). In Canada, tuberculosis is still endemic in some rural areas.
Figure 5.
In 2007, the prevalence of TB per 100,000 people was highest in sub-Saharan Africa, and was also relatively high in Asia. This figure is from Wikimedia commons.
Diagnosis
Tuberculosis is definitively diagnosed by identifying the causative organism (M.tuberculosis) in a clinical sample (for example, sputum or pus) (Figure 6). When this is not possible, a probable—although sometimes inconclusive—diagnosis may be made using imaging (X-rays or scans), a tuberculin skin test (Mantoux test) (6), or an Interferon Gamma Release Assay (IGRA).
Figure 6.

Photomicrograph of a sputum sample containing M. tuberculosis. This figure is from Wikimedia commons.
The main problem with tuberculosis diagnosis is the difficulty in culturing this slow-growing organism in the laboratory (it may take 4-12 weeks for blood or sputum culture). New TB tests have been developed that are fast and accurate. These include polymerase chain reaction assays for the detection of bacterial DNA (12). One such molecular diagnostic test gives results in 100 minutes and is currently being offered to 116 low- and middle-income countries at a discount with support from the World Health Organization (WHO) and the Bill and Melinda Gates Foundation (13).
Treatment of TB disease
Medications are the cornerstone of tuberculosis treatment. However, treating TB takes much longer than treating other types of bacterial infections. It takes antibiotics for at least six to nine months. The exact drugs and length of treatment depend on age, overall health, possible drug resistance, the form of TB (latent or active) and its location in the body.
The standard “short” course treatment of TB is isoniazid, rifampicin, pyrazinamide, and ethambutol for two months, then isoniazid and rifampicin for a further four months. The patient is considered cured at six months (although there is still a relapse rate of 2-3%). For latent tuberculosis, the standard treatment is six to nine months of isoniazid alone. If the organism is known to be fully sensitive, then treatment is with isoniazid, rifampicin, and pyrazinamide for two months, followed by isoniazid and rifampicin for four months. Ethambutol need not be used.
Although significant achievements have been made in controlling TB in China over the last decade (14), multidrug-resistant (MDR) and extensively drug-resistant tuberculosis (XDR-TB) cases have been widespread, causing a public health problem in China and worldwide in recent years. XDR-TB, a severe form of TB disease, is defined as TB that is resistant to at least rifampin and isoniazid (MDR), as well as to any member of the quinolone family and at least one second-line anti-TB injectable drug: kanamycin, capreomycin, or amikacin (15). According to WHO, XDR-TB has been reported in 58 countries up to January 2010 and is a major concern for global health (16).
The treatment of patients with MDR- or XDR-TB is more complex, toxic and costly, and less effective than treatment of other forms of TB. We applied percutaneous lung puncture to perfuse anti-TB drugs directly to the lung lesion, and the subsequent septum smear and TB culture results all were negative during 4 years of follow-up. To our knowledge, we reported the first case of XDR pulmonary tuberculosis cured by percutaneous lung puncture.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Yang SH, Chen JF, Nie Y, et al. chronic cavitary pulmonary tuberculosis cured by percutaneous lung puncture. Chi Clinic Med J 2001;55:3425-7 [Google Scholar]
- 2.Yang SH, Mao WJ, Shi XD, et al. Multidrug-resistant tuberculosis cured by percutaneous lung puncture. Chi J Tuberc Respir Dis 2006;29:131-2 [Google Scholar]
- 3.Yang SH, Li XM, Shi XD, et al. The effectiveness and security of 34 patients with pulmonary tuberculoma cured by percutaneous lung puncture. Jiangsu Med J 2008;34:414-5 [Google Scholar]
- 4.Tang S, Zhang Q, Yu J, et al. Extensively drug-resistant tuberculosis at a tuberculosis specialist hospital in Shanghai, China: clinical characteristics and treatment outcomes. Scand J Infect Dis 2011;43:280-5 [DOI] [PubMed] [Google Scholar]
- 5.“Tuberculosis Fact sheet N°104". World Health Organization. November 2010. Retrieved 26 July 2011.
- 6.Jasmer RM, Nahid P, Hopewell PC. Clinical practice. Latent tuberculosis infection. N Engl J Med 2002;347:1860-6 [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization (2009). “Epidemiology”. Global tuberculosis control: epidemiology, strategy, financing. pp. 6-33. ISBN 9789241563802. Retrieved 12 November 2009.
- 8.“The sixteenth global report on tuberculosis”.2011. Available online: http://www.who.int/tb/publications/global_report/2011/gtbr11_executive_summary.pdf
- 9.Lawn SD, Zumla AI. Tuberculosis. Lancet 2011;378:57-72 [DOI] [PubMed] [Google Scholar]
- 10.Global Tuberculosis Control, World Health Organization, 2011. Available online: http://www.who.int/tb/publications/global_report/en/index.html
- 11.Kumar V, Abbas AK, Fausto N, Mitchell RN (2007). Robbins Basic Pathology (8th ed.). Saunders Elsevier. 2007:516–522.ISBN 978-1-4160-2973-1. [Google Scholar]
- 12.Reddy JR, Kwang J, Lechtenberg KF, et al. An immunochromatographic serological assay for the diagnosis of Mycobacterium tuberculosis. Comp Immunol Microbiol Infect Dis 2002;25:21-7 [DOI] [PubMed] [Google Scholar]
- 13.“WHO says Cepheid rapid test will transform TB care”. Reuters. 8 December 2010.
- 14.Wang L, Liu J, Chin DP. Progress in tuberculosis control and the evolving public-health system in China. Lancet 2007;369:691-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wright A, Zignol M, Van Deun A, et al. Epidemiology of antituberculosis drug resistance 2002-07: an updated analysis of the Global Project on Anti-Tuberculosis Drug Resistance Surveillance. Lancet 2009;373:1861-73 [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Multidrug and extensively drug-resistant TB (M/XDR-TB): 2010 global report on surveillance and response. WHO/HTM/TB/2010.3. Geneva, Switzerland: WHO; 2010. [Google Scholar]