Abstract
Frontotemporal degeneration (FTD) and amyotrophic lateral sclerosis (ALS) are related but distinct neurodegenerative diseases. The identification of a hexanucleotide repeat expansion in a noncoding region of the chromosome 9 open reading frame 72 (C9ORF72) gene as a common cause of FTD/ALS, familial FTD, and familial ALS marks the culmination of many years of investigation. This confirms the linkage of disease to chromosome 9 in large, multigenerational families with FTD and ALS, and it promotes deeper understanding of the diseases' shared molecular FTLD-TDP pathology. The discovery of the C9ORF72 repeat expansion has significant implications not only for familial FTD and ALS, but also for sporadic disease. Clinical and pathological correlates of the repeat expansion are being reported but remain to be refined, and a genetic test to detect the expansion has only recently become clinically available. Consequently, individuals and their families who are considering genetic testing for the C9ORF72 expansion should receive genetic counseling to discuss the risks, benefits, and limitations of testing. The following review aims to describe genetic counseling considerations for individuals at risk for a C9ORF72 repeat expansion.
Introduction
Frontotemporal degeneration (FTD) is a common cause of presenile dementia, affecting 15 to 20 per 100,000 individuals between ages 45 and 64 years [1]. FTD is a clinical syndrome with three primary subtypes [2,3]. One subtype, behavioral variant FTD (bvFTD), is characterized by marked changes in behavior and personality. Disinhibition and apathy are prominent, and patients with bvFTD frequently display loss of insight, diminished empathy, repetitive motor behaviors, and eating dysregulation. Primary progressive aphasia (PPA) comprises the other two subtypes, known as nonfluent variant PPA and semantic variant PPA. Nonfluent variant PPA features loss of grammar with effortful or labored speech, while semantic variant PPA manifests as loss of knowledge of words and objects. Clinical and pathologic features of FTD may also overlap with the atypical Parkinsonian conditions corticobasal syndrome and progressive supranuclear palsy. About 15% of patients with FTD have co-occurring amyotrophic lateral sclerosis (ALS) [4].
ALS is an upper and lower form of motor neuron disease, affecting 4 to 8 per 100,000 individuals [5,6]. ALS leads to progressive weakness, muscle wasting, spasticity, and eventual paralysis and death due to degeneration of motor neurons in the cerebral cortex, brainstem, and spinal cord. Clinical diagnosis of ALS is rendered by criteria that exclude other causes of progressive upper and lower motor neuron dysfunction [7]. ALS phenotypes include primary lateral sclerosis, progressive muscular atrophy, and progressive bulbar palsy, each involving different spinal or bulbar segments at onset but with variable progression to widespread disease [8]. About 15% of patients with ALS have FTD, while up to 50% exhibit frontal lobe impairment but fail to meet strict criteria for FTD [4,9,10].
Approximately 40% of individuals with FTD have a family history of dementia [11], and in 10% the history is suggestive of an autosomal dominant inheritance pattern [5,6]. Up to 10% of individuals with ALS have a family history of ALS, usually suggestive of an autosomal dominant pattern. An expanded review of family histories considering both syndromes previously suggested that approximately 60% of individuals with co-occurring FTD/ALS have a family history of FTD and/or ALS, with almost 40% of these histories suggesting an autosomal dominant pattern [12].
In addition to the co-occurrence of disease in an individual or family, ALS and a significant proportion of patients dying with FTD share a common pathology, TDP-43 [13,14], which aggregates within cortical, brainstem, and spinal cord neurons. The recent discovery of the chromosome 9 open reading frame 72 (C9ORF72) gene as a common cause of FTD/ALS, familial FTD, and familial ALS [15,16] should lead to a better understanding of the connection between these two diseases.
C9ORF72 and frontotemporal degeneration/ amyotrophic lateral sclerosis
Familial FTD has been associated with mutations in genes encoding microtubule-associated protein tau [17] and progranulin [18,19] - and infrequently valosin-containing protein [20] and charged multivescular body protein 2B [21,22]. Familial ALS has been associated with mutations in genes encoding copper/zinc superoxide dismutase 1 [23,24], transacting response DNA binding protein [25,26], and fused in sarcoma [27,28] - and infrequently angiogenin [29], optineurin [30], and ubiquilin 2 [31]. Clinical testing is available for all listed genes with the exception of charged multivescular body protein 2B and ubiquilin 2. Most families with the clinical combination of FTD and ALS display linkage to chromosome 9.
The underlying genetic cause of chromosome 9-linked FTD and ALS was recently identified [15,16], and the mutation is an expansion of a hexanucleotide repeat (GGGGCC) in a noncoding region of the C9ORF72 gene. Function of the normal gene product is not currently known, but pathogenesis has been proposed to involve a combination of mechanisms: partial loss of function with reduced mRNA transcript and toxic gain of function with aggregation of long mRNA transcript into abnormal RNA foci [15]. Index families with a C9ORF72 expansion present with bvFTD, ALS, or both. Parkinsonism is common, and various ALS phenotypes may be observed [15,16,32]. Expansions associated with disease are estimated to have a size range of 700 to 1,600 repeats, as compared with less than 23 repeats in healthy individuals [15]. One study suggested a disease allele size of more than 30 repeats, as compared with a normal allele size of fewer than 20 repeats [16]. C9ORF72 expansions appear to be the most common cause of familial FTD, familial ALS, and sporadic forms of each [15,16].
Since the initial discovery of the C9ORF72 mutation, other FTD and ALS cohorts have been described - suggesting that the frequency of expansion in worldwide sampling is 3 to 12% among individuals with FTD and is 7 to 36% among individuals with ALS, depending on the population studied [15,33-40]. About two-thirds of expansion carriers have a positive family history of dementia of any etiology or motor neuron disease, with up to 85% exhibiting an autosomal dominant pattern [34,38]. About 4 to 7% of sporadic FTD or ALS cases are associated with an expansion [15,41]. FTD cases with family histories featuring only one first-degree relative with dementia onset at or after age 65 years are rarely (4.5%) associated with an expansion [38]. When the first-degree relative has dementia onset before age 65 years, the chance of detecting an expansion almost doubles (8%). Less than one-half of FTD cases having two other relatives with unspecified dementia, suggesting familial aggregation but not an autosomal dominant pattern, are associated with an expansion.
The frequency of the C9ORF72 expansion is highest in individuals with co-occurring FTD/ALS, as compared with pure bvFTD and ALS phenotypes. About 20 to 40% of persons with FTD/ALS carry the expansion [34,37,38,40], a proportion that significantly increases to up to 50% when there is a positive family history. Clearly, a family history of FTD and/or ALS raises the possibility of the presence of a C9ORF72 expansion, with FTD/ALS being most suggestive. Yet not all such familial cases carry the expansion.
The phenotype of individuals carrying a C9ORF72 expansion is similar to that of noncarriers. The most common presentation is bvFTD, which is frequently accompanied by motor neuron involvement. Up to 40% of expansion carriers with bvFTD had upper or lower motor neuron signs [34]. A small subset of patients with nonfluent variant PPA carries the expansion [37-39]. Semantic variant PPA, corticobasal syndrome, and progressive supranuclear palsy have not been associated with C9ORF72 expansions. Individuals with ALS may have motor neuron involvement of any segment at onset, and may even present with rare ALS phenotypes, including monomelic ALS and progressive muscular atrophy [15].
Men and women are equally likely to carry the C9ORF72 expansion. Mean age of onset is about 55 years, with a range of 30 to 70 years [33-40]. The disease duration ranges from 1 to 22 years, with an average of 7 years from symptom onset and with the ALS phenotype associated with shorter survival [34]. Individuals with a slowly progressive bvFTD phenotype, sometimes referred to as phenocopies, may harbor the expansion [42]. An interesting feature of the C9ORF72 expansion is its association with delusions. Often having a paranoid or somatoform quality, delusions occur in 20 to 40% of expansion carriers [33,34,40]. Hallucinations are also reported [34,39]. Symptoms may thus be attributed to primary psychiatric disease instead of to a neuro-degenerative condition.
Among individuals with a C9ORF72 expansion, magnetic resonance imaging shows bilateral, symmetrical frontal atrophy, with grey matter loss in orbitofrontal, medial, and dorsolateral regions, as well as anterior temporal atrophy. In contrast to other bvFTD-associated gene mutations, cerebellar atrophy appears to be uniquely associated with the expansion, despite the absence in carriers of frank cerebellar signs. Thalamic atrophy may also be uniquely associated with the expansion [33,43]. The C9ORF72 expansion displays TDP-43 neuropathology - in most cases consistent with harmonized FTLD-TDP type B, but in some cases type-A pathology is evident [34,38,40].
Risk of C9ORF72 expansion in frontotemporal degeneration/amyotrophic lateral sclerosis
The recent C9ORF72 gene discovery has created momentum towards greater understanding of FTD and ALS, allowing refinement of the phenotypes conferred by the expansion and fostering insight into the mechanism that results in overlapping symptomatology and shared TDP-43 pathology. At the same time, families living with the illnesses now have many considerations, particularly in the face of many unknowns.
While the a priori chance of a C9ORF72 expansion among individuals with an autosomal dominant family history is significant, the risk for individuals with no family history of dementia or motor neuron disease is only 4 to 7% [15,41,44]. For individuals whose family history includes relatives with dementia or other psychiatric or neurodegenerative disorder that has not been well phenotyped, the likelihood of an expansion is difficult to quantify. In addition, for individuals with a family history of relatives with mid-life onset of psychiatric symptoms that have been inadequately phenotyped, questions arise about whether or not FTD could have been overlooked in a relative, thereby complicating genetic risk assessment.
Risk assessment is also complicated by the occurrence of the C9ORF72 expansion in sporadic cases of FTD and ALS. Refinement of clinical, neuroimaging [37], and neuropathological [45,46] parameters will probably improve the ability to predict the presence of a mutation in sporadic cases, but careful attention to patients in whom the family history appears negative is critical. True sporadic cases should be distinguished from apparently sporadic ones, in which various reasons may explain the lack of a family history: unknown or incomplete information, misdiagnoses, early death, false paternity, or undisclosed adoption. Early death of a relative may be a confounder because of reports of reduced penetrance associated with the expansion, as in the report of a C9ORF72-positive family with one obligate carrier who died at age 35 years without symptoms and another obligate carrier who died at age 72 years without symptoms [34]. A large cross-sectional study suggested that 50% of individuals with an expansion are symptomatic by age 58 years, while nearly 100% are affected by age 80 years. Disease onset before age 35 years appears to occur rarely [41].
True sporadic cases may reflect the occurrence of de novo expansions, as supported by the observation that a particular 9p21 risk haplotype is over-represented in individuals with an expansion [41]. One explanation for this finding is the possibility that the haplotype may provide a predisposing genetic background for the mutation to occur randomly in sporadic cases [15]. In contrast, some data suggest that the expansion is about 1,500 years old and arises from a common founder of Finnish origin [47]. Irrespective of origins, the possibility to detect an expansion in an individual without a family history, although small, may raise concerns among families facing disease.
At the time of writing this article, C9ORF72 genetic testing has only recently become clinically available in the US, following the development of a test with Clinical Laboratory Improvement Amendments (CLIA) certification. The C9ORF72 gene test also has limited availability worldwide [48]. Although a CLIA test exists, one of the barriers to its widespread clinical utility is the unknown minimum number of repeats that confer a phenotype [15,16]. The repeat unit is large at six nucleotides, and in affected individuals the unit expands to more than several hundred in number, whereas in healthy individuals it remains at fewer than 20 to 23. The role of intermediate repeat sizes (23 to 700 repeats) is not known [15,44,46]. Because the repeat unit is large in size, GC rich, and unstable, the number of repeats cannot be quantified precisely by PCR. Southern blotting, the current method used to quantify repeat number, is labor intensive and may have difficulty discriminating repeat sizes at the smaller end of the intermediate spectrum. To date, the largest US laboratory that offers a CLIA test employs only semiquantification by PCR, and will not offer the test to asymptomatic individuals. International laboratories that perform the C9ORF72 test may also adopt similar practices. Until quantification by Southern blotting is first investigated in a large patient series [44] and later incorporated into the CLIA test, families should approach clinical genetic testing with careful consideration.
In addition, until the minimum number of pathogenic repeats is known, the suggestion that anticipation may be associated with the C9ORF72 expansion cannot be confirmed. Studies have observed that the most recent generation of affected individuals in some families had symptoms at least a decade earlier than those in the previous generation [34,36]. Better correlation of clinical patterns to exact repeat size is needed before claims of decreasing age of onset and increasing severity of symptoms are associated with larger numbers of repeats across successive generations. is scenario may create uncertainty for expansion-positive families with at-risk individuals considering genetic testing.
While a sizeable proportion of familial FTD and familial ALS is caused by the C9ORF72 expansion, there remain familial cases in which no expansion is found [34]. In these cases, the absence of a mutation in other known FTD and ALS genes suggests that there are still other unidentified causal genes implicated in FTD and/or ALS. Families left with no identifiable causal gene, despite a suggestive family history, may struggle with persistent uncertainty.
Genetic counseling
The growing but limited body of knowledge about the C9ORF72 expansion has important implications for genetic counseling of families. Genetic counseling is a communication process about the occurrence or risk of an inherited disease. Genetic counseling aims to educate individuals about disease, including the nature of inheritance; to facilitate understanding of genetic testing options for confirmation of disease or prediction of future disease onset; and to promote adaptation to the presence of or risk for disease [49]. The last aim is particularly important because of the devastating impact of FTD and/or ALS on families and the absence of prevention or treatment. Individuals who wish to learn the potential cause of FTD and/or ALS in their family should be offered genetic counseling, irrespective of but especially in the presence of a suggestive family history (Table 1).
Table 1.
Key features of C9ORF72 genetic counseling
| Feature | Salient characteristics |
|---|---|
| Family history assessment | A three-generation pedigree should document FTD, ALS, other dementia, Parkinsonism, psychiatric disease. |
| Medical records, autopsy studies may clarify diagnoses. | |
| Incomplete information, misdiagnoses, early death, false paternity, undisclosed adoption may complicate family history. | |
| An autosomal dominant pattern is most suggestive of the expansion, but a mutation cannot be ruled out completely in sporadic cases. | |
| Discussion of risks, benefits, and limitations of C9ORF72 genetic testing | Diagnostic testing should be considered in both sporadic and familial cases. Predictive genetic testing should be given careful consideration. |
| Presence of the expansion cannot predict age of onset or symptom expressivity. | |
| Limited information is known about anticipation, penetrance, and intermediate alleles. | |
| Predictive genetic testing should be offered via a modified Huntington disease protocol, which includes pre-test and post-test genetic counseling; neurologic and cognitive assessment; psychological evaluation; and in-person disclosure with a support person. | |
| Some families with an autosomal dominant history of FTD and/or ALS will have no identifiable expansion. Another genetic etiology is likely. Family members remain at risk. DNA banking is a viable option for such families. | |
| DNA banking is a viable option for families who are not ready for clinical diagnostic testing. | |
| Anticipatory guidance for at-risk families | Communication about family members' motivation to seek genetic testing may identify concerns or expectations for clinicians to address. |
| Communication about the psychological burden of disease and impact of caregiving may help clinicians identify family members' need for support or other resources. | |
| Pre-test communication about the psychosocial impact of genetic testing may help families prepare for possible outcomes and/or uncertainty. | |
| Pre-test communication about genetic privacy and discrimination concerns may help families make future care or financial plans. |
ALS, amyotrophic lateral sclerosis; C9ORF72, chromosome 9 open reading frame 72; FTD, frontotemporal degeneration.
Assessing family history is a key component of genetic counseling. The clinician should obtain a detailed three-generation pedigree that captures the presence of FTD, ALS, other dementias, Parkinsonism, and psychiatric conditions. The pedigree should include ages of disease onset, diagnoses, and ages at death. Medical records, including autopsy studies if available, are essential to clarify diagnoses. In the absence of a family history, the likelihood of detecting an expansion is small but not insignificant [41]. Genetic counseling should include a discussion of 50% risk to offspring of an expansion carrier, regardless of whether or not this expansion is de novo. Pre-test genetic counseling should help individuals appreciate the risks, benefits, and limitations of testing. At this time, predictive or presymptomatic testing should be undertaken with caution. Little is known about anticipation, penetrance, or the meaning of intermediate length expansion repeats.
Pre-test genetic counseling should help individuals anticipate the impact of genetic testing on themselves, family members, and their interpersonal relationships. For the individual who is cognitively or behaviorally impaired, genetic counseling should involve a healthcare proxy, legal guardian, or next of kin. If the proxy is an at-risk offspring or sibling, genetic counseling should address any conflicting motivations among family members for testing, while fostering a decision that best serves the family rather than the individual only. Families should consider the limitations of genetic testing, including the fact that detection of an expansion will resolve neither issues of reduced penetrance nor clinical heterogeneity. The expansion cannot predict exact age of onset or symptom expressivity. Why some individuals develop FTD or ALS or both is unclear, but there are probably other, as yet unidentified, genetic and possible environmental modifiers involved. In the context of diagnostic testing, detecting an expansion cannot predict the exact disease course. Moreover, the absence of an expansion may not reduce risk for other family members, particularly if there is an autosomal dominant family history. There remain as yet unidentified causal genes, compelling families to confront risk of disease without knowing the exact cause. Genetic counseling should focus on helping families anticipate and begin to adapt to the uncertainty that may remain after clinical genetic testing. Families who are not ready to pursue diagnostic genetic testing may consider DNA banking for future testing purposes [48].
When available, predictive genetic testing should only be offered after a mutation has been identified in a family by clinical testing. In the absence of a known C9ORF72 expansion in an affected family member, a negative predictive test result is uninformative, as it cannot discriminate someone who is a true negative for the C9ORF72 expansion from someone with another known or as yet unknown pathogenic familial mutation. At-risk family members nonetheless may have many reasons for pursuing predictive genetic testing: to reduce uncertainty, to plan for the future, to make health or lifestyle changes, and to plan a family [49]. Genetic counseling should address these motivating factors and the limitations of predictive testing, including the fact that no proven health or lifestyle behaviors can reduce risk of C9ORF72-caused FTD and/or ALS. At-risk individuals should consider future financial or care planning irrespective of predictive testing.
Many at-risk individuals are motivated to pursue genetic testing because of their experience with illness in the family. Issues of caregiver distress and psychological burden should be a focus of genetic counseling. International guidelines for medical ethics recommend that predictive genetic testing should be offered according to a modified Huntington's disease protocol and akin to guidelines about genetic testing for Alzheimer's disease [50-52]. is protocol involves a pre-test genetic counseling session, baseline neurologic and cognitive assessment, psychological evaluation, in-person disclosure, the presence of a support person, and post-test genetic counseling or follow-up. Predictive genetic testing should not be offered to asymptomatic minors. With the advent of clinical testing in a CLIA-approved laboratory, prenatal diagnosis and pre-implantation genetic diagnosis will soon become available.
Another potential risk that should be discussed during genetic counseling for predictive testing involves genetic privacy. Although studies suggest that at-risk individuals' concern for insurance and employment discrimination based on genetic information is disproportionate to documented instances, the fear of genetic discrimination persists [53-55]. In the US, the Genetic Information Nondiscrimination Act (GINA) - a federal law that took effect in 2009 to prohibit discrimination in health insurance and employment based on genetic information [56] - should be discussed during genetic counseling. At-risk individuals may also be reassured that in addition to federal legislation many US states also have anti-genetic discrimination laws [57,58]. However, none of the current federal or state legislation encompasses long-term care, life, or disability insurance, which should also be discussed during genetic counseling.
At-risk individuals should consider the potential risk of psychological distress as the result of predictive genetic testing. Although the risk for adverse psychological effects cannot be ruled out completely, studies suggest that increased post-test distress among at-risk individuals, who electively pursue predictive testing and who first receive pre-test genetic counseling, is usually transient and not clinically significant [59]. There is also evidence that baseline distress is a better predictor of post-test counseling distress than the genetic test result itself [60]. Predictive genetic testing may have a profound impact not only on the at-risk individual but also on spouses and partners [61,62]. This may greatly influence patterns of disclosure and nondisclosure within families [63]. Consequently, clinicians should be prepared to address the needs of both the patient and family members.
Case example
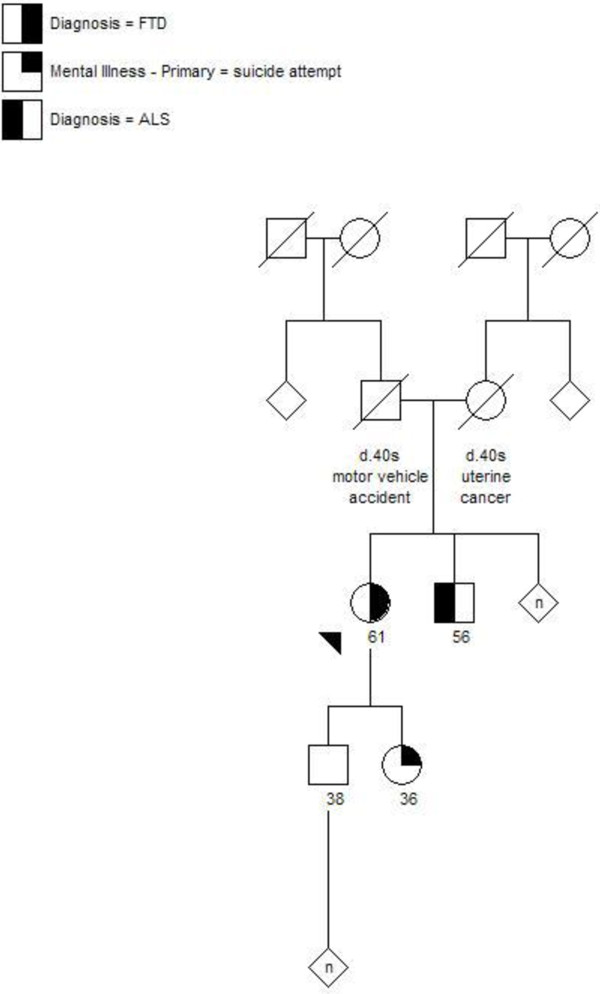
A 61-year-old patient and her husband were referred for genetic counseling due to a possible diagnosis of FTD. The patient had a 3-year history of apathy, personality changes, a decline in executive function, and some repetitive motor behaviors. More recently she had developed motor speech problems and a shuffling gait with a few falls. Her neurologic examination was notable for a dysexecutive syndrome and Parkinsonism with dysarthric speech, masked facies, a pronounced stare, subtle vertical saccade abnormalities, increased muscle tone, and gait instability. The patient's father died in his 40s in a motor vehicle accident, and her mother died in her 40s of uterine cancer. None of the patient's siblings had any known neurodegenerative or psychiatric disease. The patient's 36-year-old daughter had a suicide attempt in her 20s, but had no other psychiatric disturbances since then. The remainder of her family history was noncontributory, although little was known about her grandparents (Figure 1). At the time, the patient and her husband were counseled about the low likelihood that the illness was inherited.
Figure 1.
Case example pedigree. The proband was referred for genetic counseling with a clinical diagnosis of probable frontotemporal degeneration (FTD). The proband's father died in his 40s in a motor vehicle accident. Her mother died in her 40s of uterine cancer. Neither had any known neurodegenerative or psychiatric disease. The proband's daughter had a history of attempted suicide in her 20s, but no known longstanding psychiatric illness. No information is known about the proband's grandparents. At the time of the initial visit, the remainder of the family history was noncontributory. Subsequent to the proband's visit, her brother was diagnosed with amyotrophic lateral sclerosis (ALS).
Six months later, the patient's 38-year-old son contacted the neurologist to inform him that the patient's 56-year-old brother was recently diagnosed with ALS. During the time that passed from the patient's initial visit to the news about the patient's brother, the C9ORF72 expansion was discovered and a clinical test was developed. The patient's husband and son were referred again for genetic counseling, but only the son pursued the appointment. The son was counseled about the high likelihood that, in light of his uncle's recent diagnosis, the illnesses in the family were due to a single shared cause. The patient's son was counseled about the possibility of a C9ORF72 mutation in his family, and he understood the benefits, risks, and limitations of genetic testing. The son understood that his risk of carrying the same, as yet unidentifiable, pathogenic mutation as his mother and uncle was up to 50%. Although a clinical test was readily available, the son was challenged with trying to convince his reluctant father, already burdened by the illness experience, of the value of diagnostic testing. Genetic counseling encouraged the son to consider how best to help his father view diagnostic testing as a means to identify risk for family members, while maintaining sensitivity about his father's perspective. The son would begin talking to his father about the value of autopsy planning to confirm the clinical diagnosis. The availability of postmortem tissue would also allow the family to pursue diagnostic genetic testing posthumously, if the CLIA test was not obtained during the patient's lifetime. The son was counseled about the alternative of DNA banking.
If his mother carried a pathogenic mutation, the son understood that he could pursue predictive genetic testing. However, he remained ambivalent about testing. He felt unprepared to consider learning a positive genetic test result without the hope of prevention in the immediate future. Genetic counseling encouraged him to consider how the relationship with his wife could change, if the two of them learned of his positive genetic test result years in advance of first symptoms. He worried about whether or not his marriage could endure an inevitable, devastating illness, particularly as he watched his father struggle to adapt to his mother's personality and behavior changes. He was counseled about how and to what extent to involve his young children in conversations about the family illness. Irrespective of his gene status, he had already purchased a life insurance policy, and planned to acquire long-term care insurance. He did not know his sister's perspective on the family illness, as his sister had been uninvolved in the mother's care. Genetic counseling encouraged the son to involve the entire immediate family, including his sister, in consideration of diagnostic genetic testing for the mother. The son was also counseled about the potential impact of his mother's genetic test results on the relationship with his sister, as the siblings might react differently to the information and consequently to the implications about their own health.
The family subsequently enrolled the patient in a research protocol approved by an institutional review board, and a blood sample was screened for pathogenic mutations in the microtubule-associated protein tau, progranulin, and C9ORF72 genes. An expansion in C9ORF72 was detected in the research sample. The result was clinically confirmed but awaits disclosure, because the family remains undecided about whether or not to learn the information.
Conclusion
The discovery of the C9ORF72 expansion marks a milestone in the long search for the underlying cause of chromosome 9-linked FTD and ALS. Future studies will undoubtedly improve understanding of disease penetrance and the range of clinical phenotypes. Another area that remains to be clarified is genotype-phenotype correlations, with the intriguing possibility of intermediate alleles and their as yet undetermined clinical correlates. Additional studies will surely elucidate the molecular mechanisms that lead to C9ORF72-related neurodegeneration. at the expansion frequency is 4 to 7% in sporadic FTD or ALS raises an interesting question about whether or not C9ORF72 screening should be considered in all patients [15,41,44]. Now that a clinical test is available, its accessibility to the public may be tempered by the cost of testing, variable health insurance coverage of the test, as well as genetic privacy concerns. With the arrival of a CLIA test, genetic testing for the C9ORF72 expansion should be offered with careful consideration and in the context of genetic counseling. Genetic counseling will remain an important component of the genetic testing process as clinical expansion testing is more broadly incorporated into neurology practice.
Abbreviations
ALS: amyotrophic lateral sclerosis; bvFTD: behavioral variant frontotemporal degeneration; C9ORF72: chromosome 9 open reading frame 72; CLIA: Clinical Laboratory Improvement Amendments; FTD: frontotemporal degeneration; FTLD-TDP: frontotemporal lobar degeneration with TDP-43-positive inclusions; GINA: Genetic Information Nondiscrimination Act; PCR: polymerase chain reaction; PPA: primary progressive aphasia.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
JCF was responsible for the conception and design of the review, and for drafting and revising the manuscript. AMK was responsible for revising the manuscript. JSG was responsible for the conception and design of the review, and for revising the manuscript. The figure and table included herein comprise original work.
Contributor Information
Jamie C Fong, Email: jfong@memory.ucsf.edu.
Anna M Karydas, Email: akarydas@memory.ucsf.edu.
Jill S Goldman, Email: jg2673@columbia.edu.
Acknowledgements
The authors thank Bruce Miller and Suzee Lee for their critical review of the manuscript. The authors thank Adam Boxer and Howie Rosen for their clinical and research evaluations of patients. The authors also thank Giovanni Coppola for hexanucleotide expansion analysis. The authors are indebted to patients and their families for participation in a research study. This work was supported by National Institutes of Health grant P50 AG008702-22 (JSG). The manuscript was an invited article that underwent external peer review.
References
- Bird T, Knopman D, VanSwieten J, Rosso S, Feldman H, Tanabe H, Graff-Raford N, Geschwind D, Verpillat P, Hutton M. Epidemiology and genetics of frontotemporal dementia/Pick's disease. Ann Neurol. 2003;54(Suppl 5):S29–S31. doi: 10.1002/ana.10572. [DOI] [PubMed] [Google Scholar]
- Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, van Swieten JC, Seelaar H, Dopper EG, Onyike CU, Hillis AE, Josephs KA, Boeve BF, Kertesz A, Seeley WW, Rankin KP, Johnson JK, Gorno-Tempini ML, Rosen H, Prioleau-Latham CE, Lee A, Kipps CM, Lillo P, Piguet O, Rohrer JD, Rossor MN, Warren JD, Fox NC, Galasko D, Salmon DP. et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134:2456–2477. doi: 10.1093/brain/awr179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, Ogar JM, Rohrer JD, Black S, Boeve BF, Manes F, Dronkers NF, Vendenberghe R, Rascovsky K, Patterson K, Miller BL, Knopman DS, Hodges JR, Mesulam MM, Grossman M. Classification of primary progressive aphasia and its variants. Neurology. 2011;76:1006–1014. doi: 10.1212/WNL.0b013e31821103e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lomen-Hoerth C, Anderson T, Miller B. The overlap of amyotrophic lateral sclerosis and frontotemporal dementia. Neurology. 2002;59:1077–1079. doi: 10.1212/WNL.59.7.1077. [DOI] [PubMed] [Google Scholar]
- Rohrer JD, Warren JD. Phenotypic signatures of genetic frontotemporal dementia. Curr Opin Neurol. 2011;24:542–549. doi: 10.1097/WCO.0b013e32834cd442. [DOI] [PubMed] [Google Scholar]
- Pickering-Brown SM, Rollinson S, Du Plessis D, Morrison KE, Varma A, Richardson AM, Neary D, Snowden JS, Mann DM. Frequency and clinical characteristics of progranulin mutation carriers in the Manchester frontotemporal lobar degeneration cohort: comparison with patients with MAPT and no known mutations. Brain. 2008;131:721–731. doi: 10.1093/brain/awm331. [DOI] [PubMed] [Google Scholar]
- Brooks BR. El Escorial World Federation of Neurology criteria for the diagnosis of amyotrophic lateral sclerosis. Subcommittee on Motor Neuron Diseases/Amyotrophic Lateral Sclerosis of the World Federation of Neurology Research Group on Neuromuscular Diseases and the El Escorial 'Clinical limits of amyotrophic lateral sclerosis' workshop contributors. J Neurol Sci. 1994;124(Suppl):96–9107. doi: 10.1016/0022-510x(94)90191-0. [DOI] [PubMed] [Google Scholar]
- Hardiman O, van den Berg LH, Kiernan MC. Clinical diagnosis and management of amyotrophic lateral sclerosis. Nat Rev Neurol. 2011;7:639–649. doi: 10.1038/nrneurol.2011.153. [DOI] [PubMed] [Google Scholar]
- Ringholz GM, Appel SH, Bradshaw M, Cooke NA, Mosnik DM, Schulz PE. Prevalence and patterns of cognitive impairment in sporadic ALS. Neurology. 2005;65:586–590. doi: 10.1212/01.wnl.0000172911.39167.b6. [DOI] [PubMed] [Google Scholar]
- Lomen-Hoerth C, Murphy J, Langmore S, Kramer JH, Olney RK, Miller B. Are amyotrophic lateral sclerosis patients cognitively normal? Neurology. 2003;60:1094–1097. doi: 10.1212/01.WNL.0000055861.95202.8D. [DOI] [PubMed] [Google Scholar]
- Chow TW, Miller BL, Hayashi VN, Geschwind DH. Inheritance of frontotemporal dementia. Arch Neurol. 1999;56:817–822. doi: 10.1001/archneur.56.7.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman JS, Farmer JM, Wood EM, Johnson JK, Boxer A, Neuhaus J, Lomen- Hoerth C, Wilhelmsen KC, Lee VM, Grossman M, Miller BL. Comparison of family histories in FTLD subtypes and related tauopathies. Neurology. 2005;65:1817–1819. doi: 10.1212/01.wnl.0000187068.92184.63. [DOI] [PubMed] [Google Scholar]
- Neumann M, Sampathu DM, Kwong LK, Truax AC, Micsenyi MC, Chou TT, Bruce J, Schuck T, Grossman M, Clark CM, McCluskey LF, Miller BL, Masliah E, Mackenzie IR, Feldman H, Feiden W, Kretzschmar HA, Trojanowski JQ, Lee VM. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314:130–133. doi: 10.1126/science.1134108. [DOI] [PubMed] [Google Scholar]
- Arai T, Hasegawa M, Akiyama H, Ikeda K, Nonaka T, Mori H, Mann D, Tsuchiya K, Yoshida M, Hashizume Y, Oda T. TDP-43 is a component of ubiquitinpositive tau-negative inclusions in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Biochem Biophys Res Commun. 2006;351:602–611. doi: 10.1016/j.bbrc.2006.10.093. [DOI] [PubMed] [Google Scholar]
- DeJesus-Hernandez M, Mackenzie IR, Boeve BF, Boxer AL, Baker M, Rutherford NJ, Nicholson AM, Finch NA, Flynn H, Adamson J, Kouri N, Wojtas A, Sengdy P, Hsuing GY, Karydas A, Seeley WW, Josephs KA, Coppola G, Geschwind DH, Wszolek ZK, Feldman H, Knopman DS, Petersen RC, Miller BL, Dickson DW, Boylan KB, Graff-Radford NR, Rademakers R. Expanded GGGGCC hexanucleotide repeat in noncoding region of C9ORF72 causes chromosome 9p-linked FTD and ALS. Neuron. 2011;72:245–256. doi: 10.1016/j.neuron.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renton AE, Majounie E, Waite A, Simon-Sanchez J, Rollinson S, Gibbs JR, Schymick JC, Laaksovirta H, van Swieten JC, Myllykangas L, Kalimo H, Paetau A, Abramzon Y, Remes AM, Kaganovich A, Scholz SW, Duckworth J, Ding J, Harmer DW, Hernandez DG, Johnson JO, Mok K, Ryten M, Trabzuni D, Guerreiro RJ, Orrell RW, Neal J, Murray A, Pearson J, Jansen IE. A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. Neuron. 2011;72:257–268. doi: 10.1016/j.neuron.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutton M, Lendon CL, Rizzu P, Baker M, Froelich S, Houlden H, Pickering-Brown S, Chakraverty S, Isaacs A, Grover A, Hackett J, Adamson J, Lincoln S, Dickson D, Davies P, Petersen RC, Stevens M, de Graaff E, Wauters E, van Baren J, Hillebrand M, Joosse M, Kwon JM, Nowotny P, Che LK, Norton J, Morris JC, Reed LA, Trojanowski J, Basun H. et al. Association of missense and 5'-splicesite mutations in tau with the inherited dementia FTDP-17. Nature. 1998;393:702–705. doi: 10.1038/31508. [DOI] [PubMed] [Google Scholar]
- Baker M, Mackenzie IR, Pickering-Brown SM, Gass J, Rademakers R, Lindholm C, Snowden J, Adamson J, Sadovnick AD, Rollinson S, Cannon A, Dwosh E, Neary D, Melquist S, Richardson A, Dickson D, Berger Z, Eriksen J, Robinson T, Zehr C, Dickey CA, Crook R, McGowan E, Mann D, Boeve B, Feldman H, Hutton M. Mutations in progranulin cause tau-negative frontotemporal dementia linked to chromosome 17. Nature. 2006;442:916–919. doi: 10.1038/nature05016. [DOI] [PubMed] [Google Scholar]
- Cruts M, Gijselinck I, van der Zee J, Engelborghs S, Wils H, Pirici D, Rademakers R, Vandenberghe R, Dermaut B, Martin J-J, van Duijn C, Peeters K, Sciot R, Santens P, De Pooter T, Mattheijssens M, Van den Broeck M, Cuijt I, Vennekens K, De Deyn PP, Kumar-Singh S, Van Broeckhoven C. Null mutations in progranulin cause ubiquitin-positive frontotemporal dementia linked to chromosome 17q21. Nature. 2006;442:920–924. doi: 10.1038/nature05017. [DOI] [PubMed] [Google Scholar]
- Watts GDJ, Wymer J, Kovach MJ, Mehta SG, Mumm S, Darvish D, Pestronk A, Whyte MP, Kimonis VE. Inclusion body myopathy associated with Paget disease of bone and frontotemporal dementia is caused by mutant valosin-containing protein. Nat Genet. 2004;36:377–381. doi: 10.1038/ng1332. [DOI] [PubMed] [Google Scholar]
- van der Zee J, Urwin H, Engelborghs S, Bruyland M, Vandenberghe R, Dermaut B, De Pooter T, Peeters K, Santens P, De Deyn PP, Fisher EM, Collinge J, Isaacs AM, Van Broeckhoven C. CHMP2B C-truncating mutations in frontotemporal lobar degeneration are associated with an aberrant endosomal phenotype in vitro. Hum Mol Genet. 2008;17:313–322. doi: 10.1093/hmg/ddm309. [DOI] [PubMed] [Google Scholar]
- Skibinski G, Parkinson NJ, Brown JM, Chakrabarti L, Lloyd SL, Hummerich H, Nielsen JE, Hodges JR, Spillantini MG, Thusgaard T, Brandner S, Brun A, Rossor MN, Gade A, Johannsen P, Sørensen SA, Gydesen S, Fisher EM, Collinge J. Mutations in the endosomal ESCRTIII-complex subunit CHMP2B in frontotemporal dementia. Nat Genet. 2005;37:806–808. doi: 10.1038/ng1609. [DOI] [PubMed] [Google Scholar]
- Deng HX, Hentati A, Tainer JA, Iqbal Z, Cayabyab A, Hung WY, Getzoff ED, Hu P, Herzfeldt B, Roos RP. Amyotrophic lateral sclerosis and structural defects in Cu,Zn superoxide dismutase. Science. 1993;261:1047–1051. doi: 10.1126/science.8351519. [DOI] [PubMed] [Google Scholar]
- Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, Hentati A, Donaldson D, Goto J, O'Regan JP, Deng HX. Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature. 1993;362:59–62. doi: 10.1038/362059a0. [DOI] [PubMed] [Google Scholar]
- Benajiba L, Le Ber I, Camuzat A, Lacoste M, Thomas-Anterion C, Couratier P, Legallic S, Salachas F, Hannequin D, Decousus M, Lacomblez L, Guedj E, Golfier V, Camu W, Dubois B, Campion D, Meininger V, Brice A. French Clinical and Genetic Research Network on Frontotemporal Lobar Degeneration/Frontotemporal Lobar Degeneration with Motoneuron Disease. TARDBP mutations in motoneuron disease with frontotemporal lobar degeneration. Ann Neurol. 2009;65:470–473. doi: 10.1002/ana.21612. [DOI] [PubMed] [Google Scholar]
- Borroni B, Bonvicini C, Alberici A, Buratti E, Agosti C, Archetti S, Papetti A, Stuani C, Di Luca M, Gennarelli M, Padovani A. Mutation within TARDBP leads to frontotemporal dementia without motor neuron disease. Hum Mutat. 2009;30:E974–983. doi: 10.1002/humu.21100. [DOI] [PubMed] [Google Scholar]
- Kwiatkowski TJ, Bosco DA, Leclerc AL, Tamrazian E, Vanderburg CR, Russ C, Davis A, Gilchrist J, Kasarskis EJ, Munsat T, Valdmanis P, Rouleau GA, Hosler BA, Cortelli P, de Jong PJ, Yoshinaga Y, Haines JL, Pericak-Vance MA, Yan J, Ticozzi N, Siddique T, McKenna-Yasek D, Sapp PC, Horvitz HR, Landers JE, Brown RH Jr. Mutations in the FUS/TLS gene on chromosome 16 cause familial amyotrophic lateral sclerosis. Science. 2009;323:1205–1208. doi: 10.1126/science.1166066. [DOI] [PubMed] [Google Scholar]
- Vance C, Rogelj B, Hortobagyi T, De Vos KJ, Nishimura AL, Sreedharan J, Hu X, Smith B, Ruddy D, Wright P, Ganesalingam J, Williams KL, Tripathi V, Al-Saraj S, Al-Chalabi A, Leigh PN, Blair IP, Nicholson G, de Belleroche J, Gallo JM, Miller CC, Shaw CE. Mutations in FUS, an RNA processing protein, cause familial amyotrophic lateral sclerosis type 6. Science. 2009;323:1208–1211. doi: 10.1126/science.1165942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenway MJ, Andersen PM, Russ C, Ennis S, Cashman S, Donaghy C, Patterson V, Swingler R, Kieran D, Prehn J, Morrison KE, Green A, Acharya KR, Brown RH Jr, Hardiman O. ANG mutations segregate with familial and 'sporadic' amyotrophic lateral sclerosis. Nat Genet. 2006;38:411–413. doi: 10.1038/ng1742. [DOI] [PubMed] [Google Scholar]
- Maruyama H, Morino H, Ito H, Izumi Y, Kato H, Watanabe Y, Kinoshita Y, Kamada M, Nodera H, Suzuki H, Komure O, Matsuura S, Kobatake K, Morimoto N, Abe K, Suzuki N, Aoki M, Kawata A, Hirai T, Kato T, Ogasawara K, Hirano A, Takumi T, Kusaka H, Hagiwara K, Kaji R, Kawakami H. Mutations of optineurin in amyotrophic lateral sclerosis. Nature. 2010;465:223–226. doi: 10.1038/nature08971. [DOI] [PubMed] [Google Scholar]
- Deng H-X, Chen W, Hong S-T, Boycott KM, Gorrie GH, Siddique N, Yang Y, Fecto F, Shi Y, Zhai H, Jiang H, Hirano M, Rampersaud E, Jansen GH, Donkervoort S, Bigio EH, Brooks BR, Ajroud K, Sufit RL, Haines JL, Mugnaini E, Pericak-Vance MA, Siddique T. Mutations in UBQLN2 cause dominant Xlinked juvenile and adult-onset ALS and ALS/dementia. Nature. 2011;477:211–215. doi: 10.1038/nature10353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boxer AL, Mackenzie IR, Boeve BF, Baker M, Seeley WW, Crook R, Feldman H, Hsiung GY, Rutherford N, Laluz V, Whitwell J, Foti D, McDade E, Molano J, Karydas A, Wojtas A, Goldman J, Mirsky J, Sengdy P, Dearmond S, Miller BL, Rademakers R. Clinical, neuroimaging and neuropathological features of a new chromosome 9p-linked FTD-ALS family. J Neurol Neurosurg Psychiatry. 2011;82:196–203. doi: 10.1136/jnnp.2009.204081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sha SJ TL, Rankin KP, Yokoyama JS, Rutherford N, Fong JC, Khan B, Karydas AM, Baker MC, DeJesus-Hernandez M, Pribadi M, Coppola G, Geschwind DH, Rademakers R, Lee SE, Seeley WW, Miller BL, Boxer AL. Frontotemporal dementia due to C9ORF72 mutations: clinical and imaging features. Neurology. 2012. in press . [DOI] [PMC free article] [PubMed]
- Boeve BF, Boylan KB, Graff-Radford NR, DeJesus-Hernandez M, Knopman DS, Pedraza O, Vemuri P, Jones D, Lowe V, Murray ME, Dickson DW, Josephs KA, Rush BK, Machulda MM, Fields JA, Ferman TJ, Baker M, Rutherford NJ, Adamson J, Wszolek ZK, Adeli A, Savica R, Boot B, Kuntz KM, Gavrilova R, Reeves A, Whitwell J, Kantarci K, Jack CR Jr, Parisi JE. et al. Characterization of frontotemporal dementia and/or amyotrophic lateral sclerosis associated with the GGGGCC repeat expansion in C9ORF72. Brain. 2012;135:765–783. doi: 10.1093/brain/aws004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chio A, Borghero G, Restagno G, Mora G, Drepper C, Traynor BJ, Sendtner M, Brunetti M, Ossola I, Calvo A, Pugliatti M, Sotgiu MA, Murru MR, Marrosu MG, Marrosu F, Marinou K, Mandrioli J, Sola P, Caponnetto C, Mancardi G, Mandich P, La Bella V, Spataro R, Conte A, Monsurrò MR, Tedeschi G, Pisano F, Bartolomei I, Salvi F, Lauria Pinter G. et al. Clinical characteristics of patients with familial amyotrophic lateral sclerosis carrying the pathogenic GGGGCC hexanucleotide repeat expansion of C9ORF72. Brain. 2012;135:784–793. doi: 10.1093/brain/awr366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper-Knock J, Hewitt C, Highley JR, Brockington A, Milano A, Man S, Martindale J, Hartley J, Walsh T, Gelsthorpe C, Baxter L, Forster G, Fox M, Bury J, Mok K, McDermott CJ, Traynor BJ, Kirby J, Wharton SB, Ince PG, Hardy J, Shaw PJ. Clinico-pathological features in amyotrophic lateral sclerosis with expansions in C9ORF72. Brain. 2012;135:751–764. doi: 10.1093/brain/awr365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiung G-YR, DeJesus-Hernandez M, Feldman HH, Sengdy P, Bouchard-Kerr P, Dwosh E, Butler R, Leung B, Fok A, Rutherford NJ, Baker M, Rademakers R, Mackenzie IR. Clinical and pathological features of familial frontotemporal dementia caused by C9ORF72 mutation on chromosome 9p. Brain. 2012;135:709–722. doi: 10.1093/brain/awr354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney CJ, Beck J, Rohrer JD, Lashley T, Mok K, Shakespeare T, Yeatman T, Warrington EK, Schott JM, Fox NC, Rossor MN, Hardy J, Collinge J, Revesz T, Mead S, Warren JD. Frontotemporal dementia with the C9ORF72 hexanucleotide repeat expansion: clinical, neuroanatomical and neuropathological features. Brain. 2012;135:736–750. doi: 10.1093/brain/awr361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon-Sanchez J, Dopper EGP, Cohn-Hokke PE, Hukema RK, Nicolaou N, Seelaar H, de Graaf JRA, de Koning I, van Schoor NM, Deeg DJH, Smits M, Raaphorst J, van den Berg LH, Schelhaas HJ, De Die-Smulders CE, Majoor-Krakauer D, Rozemuller AJ, Willemsen R, Pijnenburg YA, Heutink P, van Swieten JC. The clinical and pathological phenotype of C9ORF72 hexanucleotide repeat expansions. Brain. 2012;135:723–735. doi: 10.1093/brain/awr353. [DOI] [PubMed] [Google Scholar]
- Snowden JS, Rollinson S, Thompson JC, Harris JM, Stopford CL, Richardson AMT, Jones M, Gerhard A, Davidson YS, Robinson A, Gibbons L, Hu Q, DuPlessis D, Neary D, Mann DM, Pickering-Brown SM. Distinct clinical and pathological characteristics of frontotemporal dementia associated with C9ORF72 mutations. Brain. 2012;135:693–708. doi: 10.1093/brain/awr355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majounie E, Renton AE, Mok K, Dopper EG, Waite A, Rollinson S, Chio A, Restagno G, Nicolaou N, Simon-Sanchez J, van Swieten JC, Abramzon Y, Johnson JO, Sendtner M, Pamphlett R, Orrell RW, Mead S, Sidle KC, Houlden H, Rohrer JD, Morrison KE, Pall H, Talbot K, Ansorge O. Chromosome 9-ALS/FTD Consortium; French research network on FTLD/FTLD/ALS; ITALSGEN Consortium. Hernandez DG, Arepalli S, Sabatelli M. et al. Frequency of the C9orf72 hexanucleotide repeat expansion in patients with amyotrophic lateral sclerosis and frontotemporal dementia: a cross-sectional study. Lancet Neurol. 2012;11:323–330. doi: 10.1016/S1474-4422(12)70043-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan BK, Yokoyama JS, Takada LT, Sha SJ, Rutherford NJ, Fong JC, Karydas AM, Wu T, Ketelle RS, Baker MC, Hernandez MD, Coppola G, Geschwind DH, Rademakers R, Lee SE, Rosen HJ, Rabinovici GD, Seeley WW, Rankin KP, Boxer AL, Miller BL. Atypical, slowly progressive behavioural variant frontotemporal dementia associated with C9ORF72 hexanucleotide expansion. J Neurol Neurosurg Psychiatry. 2012;83:358–364. doi: 10.1136/jnnp-2011-301883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitwell JL, Weigand SD, Boeve BF, Senjem ML, Gunter JL, DeJesus-Hernandez M, Rutherford NJ, Baker M, Knopman DS, Wszolek ZK, Parisi JE, Dickson DW, Petersen RC, Rademakers R, Jack CR Jr, Josephs KA. Neuroimaging signatures of frontotemporal dementia genetics: C9ORF72, tau, progranulin and sporadics. Brain. 2012;135:794–806. doi: 10.1093/brain/aws001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rademakers R. C9orf72 repeat expansions in patients with ALS and FTD. Lancet Neurol. 2012;11:297–298. doi: 10.1016/S1474-4422(12)70046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Sarraj S, King A, Troakes C, Smith B, Maekawa S, Bodi I, Rogelj B, Al-Chalabi A, Hortobagyi T, Shaw CE. p62 positive, TDP-43 negative, neuronal cytoplasmic and intranuclear inclusions in the cerebellum and hippocampus define the pathology of C9orf72-linked FTLD and MND/ALS. Acta Neuropathol. 2011;122:691–702. doi: 10.1007/s00401-011-0911-2. [DOI] [PubMed] [Google Scholar]
- Murray ME, DeJesus-Hernandez M, Rutherford NJ, Baker M, Duara R, Graff- Radford NR, Wszolek ZK, Ferman TJ, Josephs KA, Boylan KB, Rademakers R, Dickson DW. Clinical and neuropathologic heterogeneity of c9FTD/ALS associated with hexanucleotide repeat expansion in C9ORF72. Acta Neuropathol. 2011;122:673–690. doi: 10.1007/s00401-011-0907-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mok K, Traynor BJ, Schymick J, Tienari PJ, Laaksovirta H, Peuralinna T, Myllykangas L, Chio A, Shatunov A, Boeve BF, Boxer AL, DeJesus-Hernandez M, Mackenzie IR, Waite A, Williams N, Morris HR, Simón-Sánchez J, van Swieten JC, Heutink P, Restagno G, Mora G, Morrison KE, Shaw PJ, Rollinson PS, Al-Chalabi A, Rademakers R, Pickering-Brown S, Orrell RW, Nalls MA, Hardy J. Chromosome 9 ALS and FTD locus is probably derived from a single founder. Neurobiol Aging. 2012;33:209.e3–8. doi: 10.1016/j.neurobiolaging.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GeneTests Medical Genetics Information Resource. http://www.genetests.org
- Williamson J, LaRusse S. Genetics and genetic counseling: recommendations for Alzheimer's disease, frontotemporal dementia, and Creutzfeldt-Jakob disease. Curr Neurol Neurosci Rep. 2004;4:351–357. doi: 10.1007/s11910-004-0081-x. [DOI] [PubMed] [Google Scholar]
- Guidelines for the molecular genetics predictive test in Huntington's disease. International Huntington Association (IHA) and the World Federation of Neurology (WFN) Research Group on Huntington's Chorea. Neurology. 1994;44:1533–1536. [PubMed] [Google Scholar]
- Genetic Testing for Huntington's Disease: It's Relevance and Implications. http://www.hdsa.org/images/content/1/1/11884.pdf
- Goldman JS, Hahn SE, Catania JW, LaRusse-Eckert S, Butson MB, Rumbaugh M, Strecker MN, Roberts JS, Burke W, Mayeux R, Bird T. Genetic counseling and testing for Alzheimer disease: joint practice guidelines of the American College of Medical Genetics and the National Society of Genetic Counselors. Genet Med. 2011;13:597–605. doi: 10.1097/GIM.0b013e31821d69b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong K, Weber B, FitzGerald G, Hershey JC, Pauly MV, Lemaire J, Subramanian K, Asch DA. Life insurance and breast cancer risk assessment: adverse selection, genetic testing decisions, and discrimination. Am J Med Genet A. 2003;120A:359–364. doi: 10.1002/ajmg.a.20025. [DOI] [PubMed] [Google Scholar]
- Clayton EW. Ethical, legal, and social implications of genomic medicine. N Engl J Med. 2003;349:562–569. doi: 10.1056/NEJMra012577. [DOI] [PubMed] [Google Scholar]
- Wertz DC. Genetic discrimination - an overblown fear? Nat Rev Genet. 2002;3:496. doi: 10.1038/nrg854. [DOI] [PubMed] [Google Scholar]
- Hudson KL, Holohan MK, Collins FS. Keeping pace with the times - the Genetic Information Nondiscrimination Act of 2008. N Engl J Med. 2008;358:2661–2663. doi: 10.1056/NEJMp0803964. [DOI] [PubMed] [Google Scholar]
- National Conference of State Legislatures, Genetic Employment Laws. 2008. http://www.ncsl.org/issues-research/health/genetic-employmentlaws.aspx
- National Conference of State Legislatures:Genetics and Health Insurance State Anti-Discrimination Laws. http://www.ncsl.org/issues-research/health/genetic-nondiscrimination-in-health-insurance-laws.aspx
- Lerman C, Croyle RT, Tercyak KP, Hamann H. Genetic testing: psychological aspects and implications. J Consult Clin Psychol. 2002;70:784–797. doi: 10.1037//0022-006x.70.3.784. [DOI] [PubMed] [Google Scholar]
- Kessler S. Predictive testing for Huntington disease: a psychologist's view. Am J Med Genet. 1994;54:161–166. doi: 10.1002/ajmg.1320540302. [DOI] [PubMed] [Google Scholar]
- Quaid KA, Wesson MK. Exploration of the effects of predictive testing for Huntington disease on intimate relationships. Am J Med Genet. 1995;57:46–51. doi: 10.1002/ajmg.1320570111. [DOI] [PubMed] [Google Scholar]
- Richards F, Williams K. Impact on couple relationships of predictive testing for Huntington disease: a longitudinal study. Am J Med Genet A. 2004;126A:161–169. doi: 10.1002/ajmg.a.20582. [DOI] [PubMed] [Google Scholar]
- Klitzman R, Thorne D, Williamson J, Chung W, Marder K. Disclosures of Huntington disease risk within families: patterns of decision-making and implications. Am J Med Genet A. 2007;143A:1835–1849. doi: 10.1002/ajmg.a.31864. [DOI] [PubMed] [Google Scholar]