Abstract
Endoscopic surgery first started as snare polypectomy and then progressed to endoscopic mucosal resection (EMR). In order to resect a lesion that is more than 2 cm, endoscopic submucosal dissection (ESD) was developed. ESD therapy has now been established and is being used for early stage neoplastic lesions in the stomach, colon, esophagus, larynx and pharynx. In ESD specimens, we deal with relatively small lesions; therefore, more meticulous and precise pathological diagnosis is required compared to that in surgically resected specimens. In addition, we should be expert in the eligibility criteria of the different organs for ESD therapy. Here, we explain the biopsy diagnosis, including the Japanese group classification as well as the Vienna classification, handling the specimen, including fixation, photography, cutting and paraffin embedding, histological type, depth, vascular invasion and evaluation of the surgical margins, based on the latest Japanese guidelines. Japanese histopathology diagnostic criteria for the stomach, colon and esophagus are also described. We also demonstrate some examples of those mentioned above.
Keywords: Esophagus, Stomach, Colon, Rectum, Biopsy, Endoscopic mucosal dissection, Surgical pathology, Diagnosis, Guideline, Immunohistochemistry
INTRODUCTION
Endoscopic surgery for gastrointestinal epithelial neoplasms such as protruding early gastric cancer or adenoma of the colon first took the form of polypectomy for polypoid lesions and then progressed to endoscopic mucosal resection (EMR) for flat type lesions[1]. However, the resection of these lesions by EMR was generally less precise than that in surgical excision. This was because the lesion could be no larger than approximately 2 cm in diameter for resection and had to be resected separately, not en bloc. In addition, local recurrence was often encountered. In order to solve these problems in the stomach, a new method called endoscopic submucosal dissection (ESD) was developed, enabling a lesion to be excised en bloc[2,3]. Nowadays, ESD has been used for early stage neoplastic lesions in the esophagus[4], colorectum[5], pharynx[6,7] and larynx[8]. The development of this technique enabled an accurate pathological diagnosis of the lesion to be made and the endoscopic operation became established as a form of therapy. ESD therapy has been established not only as a procedure of ESD, but also as a system composed of the endoscopic diagnosis of the lesion, the pathological diagnosis of the biopsy, ESD enforcement, the pathological diagnosis of the ESD specimen and additional surgical resections (if necessary). It was completed based on the data amassed by Japanese physicians, surgeons, radiologists and pathologists’ continuous efforts through more than 50 years of experience. Here, we describe the Japanese histopathology diagnostic criteria based on ESD treatment and the evaluation criteria of ESD specimens (especially in the esophagus, stomach and colorectum). In addition, critical points to be considered are also mentioned.
STOMACH
ESD treatment was first performed for early gastric cancer and nowadays ESD treatment can be utilized in other organs, including the esophagus and colon. Eligibility criteria for ESD therapy and pathological diagnosis by the Gastric Cancer Treatment Guidelines 2010 have been established.
According to the Gastric Cancer Treatment Guidelines 2010 (3rd edition) by the Japanese Gastric Cancer Association, the fundamental rule for ESD treatment is described as follows: the possibility of lymph node metastasis is extremely low and the tumor is of a size and location which enables it to be removed en bloc. The absolute indicative lesion for ESD is defined as follows: differentiated type adenocarcinoma which is diagnosed as macroscopically intramucosal carcinomas (cT1a) of 2 cm or less in diameter regardless of its macroscopic type, without ulcer/ulcer scar lesion. If the lesion has no vascular invasion, the pT1a lesion shows an extremely low risk of lymph node metastasis[9-13]. Since ESD treatment does not include lymph node dissection, it poses a greater risk for lymph node metastasis than surgical resection[14,15]. Recently, ESD has been performed for the lesions of “extended adaptation”. These lesions include (1) differentiated type adenocarcinoma (cT1a), more than 2 cm in diameter, without ulceration; (2) differentiated type adenocarcinoma (cT1a), 3 cm or less in diameter, with ulceration; and (3) undifferentiated type adenocarcinoma (cT1a), 2 cm or less, without ulceration[16-18]. All three lesions should not have lymphatic or vascular invasion. The pathological diagnosis of ESD is important to determine whether a case is a “usual adaptation lesion” or an “extended adaptation lesion”.
Biopsy diagnosis
Histological assessment of gastric and colorectal biopsy specimens is made in Japan by using the “group classification” system. This classification was originally made for epithelial neoplasm and is based on the grade of cellular and/or structural changes of the lesion. The group classification is not a diagnostic category and is used only for biopsy tissue diagnosis and not for resection materials. This classification consists of six groups (Table 1)[19,20]. Since there are very few esophageal glandular neoplasias in Japan, the group classification is not used in the esophagus. In other words, squamous epithelial lesions are just divided into three categories (normal, reactive atypia and neoplasia with low grade atypia and high grade atypia). In order to internationally standardize the pathological criteria, an international consensus meeting was held in Vienna and the “Vienna classification” was established[21]. Afterwards, the “group classification” was also revised by adding the concept of the “Vienna classification” (Table 1). However, a debatable portion between the “group classification” and the “Vienna classification” still remains. For example, intramucosal invasive lesions of the colon are not considered to be intramucosal carcinomas in the western point of view but they are in the Japanese point of view. We Japanese also think that the proliferation potency of the cancer differs between cancer with low grade atypia (low grade cancer) and cancer with high grade atypia (high grade cancer) and the grading of the cancer is recommended. Intraepithelial neoplasia of the esophagus and Group 3 lesions of the stomach and the colorectum are now considered to be eligible for polypectomy, EMR or ESD treatment in Japan. Considering the adaptation of future treatment, it is necessary to standardize the pathological nomenclature of intramucosal neoplasia internationally. For example, adenoma/dysplasia to carcinoma in situ with low grade atypia should be standardized to low grade intramucosal neoplasia and carcinoma in situ with high grade atypia to intramucosal invasive adenocarcinoma should be standardized to high grade intramucosal neoplasia.
Table 1.
Histological assessment of biopsy specimens of colon and rectum and comparison with Vienna classification
| Definition of group classification of Japan | Vienna classification |
| Group X: Inadequate material for histological diagnosis | |
| Group 1: Normal tissue and non-neoplastic lesion | Category 1 |
| Group 2: Lesions in which it is difficult to determine whether the lesion is tumorous or non-tumorous | Category 2 |
| Group 3: Adenoma (benign neoplasia) | Category 3 |
| Group 4: Neoplastic lesion suspected of being carcinoma | Category 4.1 |
| Group 5: Carcinoma | Category 4.1 to 5.2 |
Japanese classification is used only for biopsy tissue diagnosis (English edition of gastric carcinoma is now being prepared for publication).
Handling of endoscopic resection materials
In ESD materials, it is important to pathologically evaluate whether curative resection has been made or additional resection is required. Since specimens and lesions are both smaller than the surgical operation materials, careful and meticulous handling is desirable.
Fixation of the specimen: Just as with surgical materials, an endoscopically resected specimen is placed on a formalin board, cork or styrofoam and stretched out to approximate the length to what is in the living body. Then the full thickness (mucosa, muscularis mucosae and submucosa) of the specimen is pinned with rustproof pins to identify the horizontal margin. Overextension of the specimen should be avoided since it can cause destruction of the material. A filter paper placed between the resection specimen and the fixation board should prevent poor fixation.
Macroscopic observation: In order to identify the proximal side, distal side, tumor location, size of lesion and marginal side, communication between endoscopists and pathologists is essential. Especially if there is a possibility of submucosal invasion or ulcer scar, it is necessary for pathologists to confirm the possible site with endoscopists.
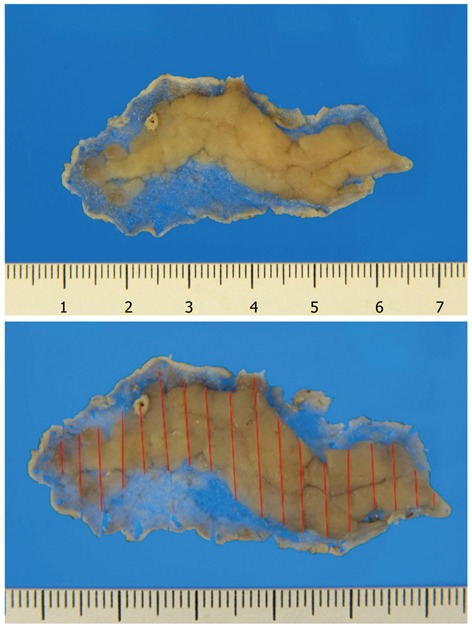
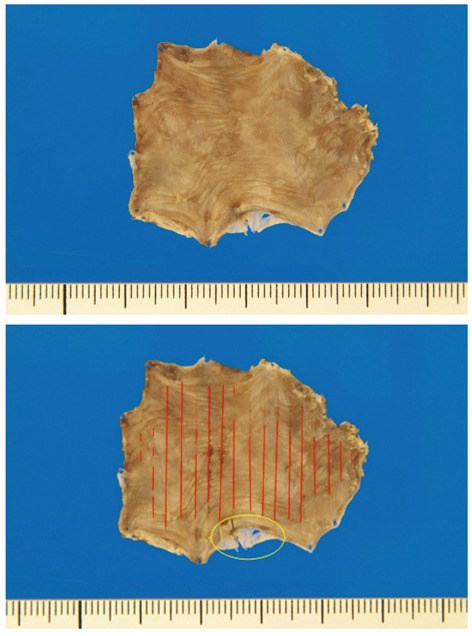
Photography: Photographs of the specimen should be taken both before and after formalin fixation. In general, when taking a picture, the resection materials are positioned with the proximal side to the right and the distal side to the left. However, in the case of ESD, the specimen can be positioned with the major axis direction horizontally for the photograph, as this allows for the highest resolution. The gross photograph with cutting lines is recommended to compare macroscopic and microscopic findings (Figure 1). It is also useful to map and rebuild the lesion. The mucosal lesion can be clearly identified if a photograph is taken of the specimen immersed in water after hematoxylin staining.
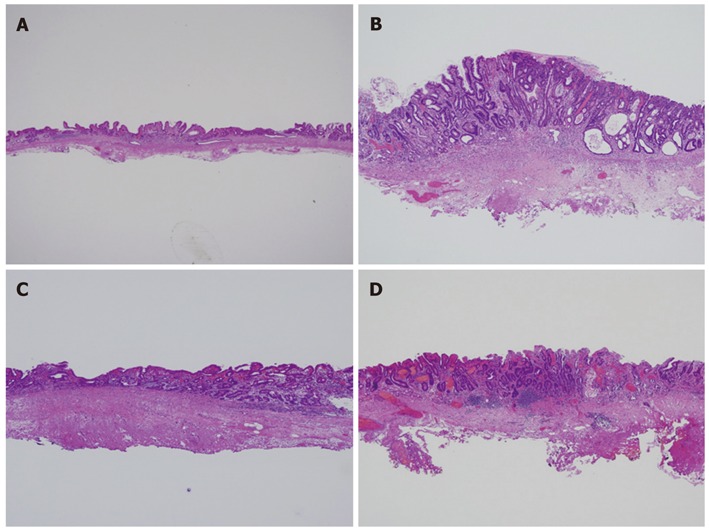
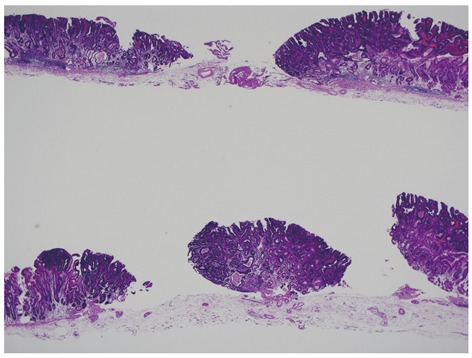
Figure 1.
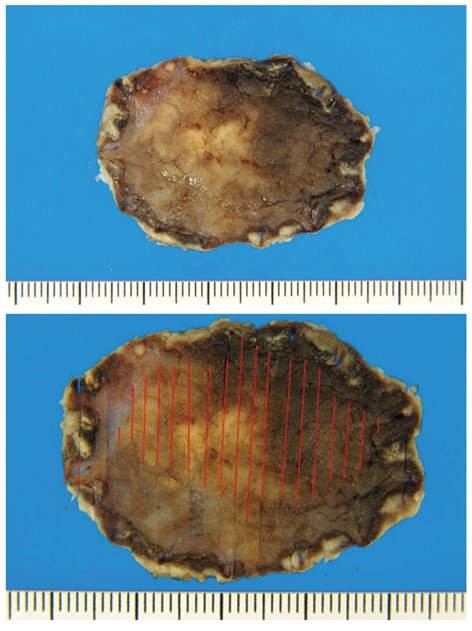
Endoscopic submucosal dissection materials with incidental lesions not found before treatment. These cases are found in a percentage of endoscopic submucosal dissection materials. The incidental lesion shows a positive margin. It should be kept in mind that a lesion may not be single but multiple in endoscopic submucosal dissection specimens. This accurate mapping of the lesion is helpful to make a treatment strategy after endoscopic submucosal dissection specimen.
Cutting: Importantly, the ESD specimen should be cut parallel to the closest margin direction (Figure 2A). When the negative margin is obvious, the specimens are step-sectioned along the minor axis of the specimen to obtain more information (Figure 2B).
Figure 2.
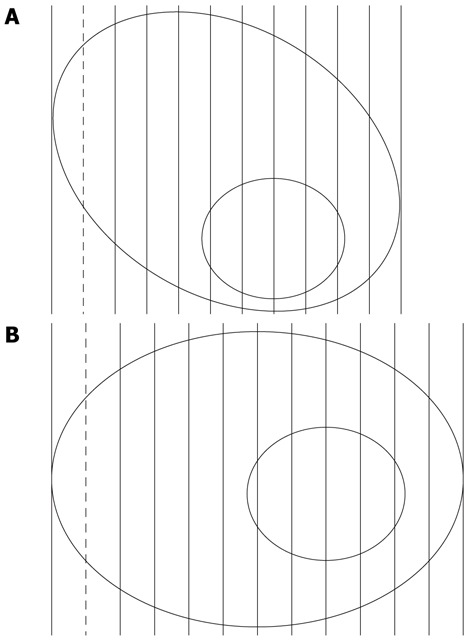
Cutting. A: General cutting of endoscopic submucosal dissection material. The final glass slide is of the reversed section of the solid line. Therefore, it is recommended that the tumor area should not be included in the portion of the dotted line; B: Cutting of endoscopic submucosal dissection material with a tumor close to the cut margin. Endoscopic submucosal dissection specimen should be cut in parallel sections which are perpendicular to the tangent of the closest margin.
The evidence of ESD treatment is based on the data of cases of surgically treated early gastric cancer in relation to lymph node metastases. In those cases, the lesion was step-sectioned at 4 mm to 5 mm intervals and then examined pathologically. Regarding the ESD material, the width of the sections is reduced to 2 mm intervals to allow for a more accurate diagnosis, as recommended by the Japanese Gastric Cancer Association. If any lesion is to be confirmed pathologically, tissue processing of the lesion should be performed.
Paraffin embedding: Larger tissue specimens should be divided properly. In such cases, care should be taken so that the divided portions do not contain the main lesion, a portion suspected of having invasion to the submucosa, or a site of an ulcer scar. Then, the tissues are put into the cassettes and the cassettes containing tissue are immersed in paraffin.
Histological evaluation
In Japan, the histological diagnosis of the ESD materials is made according to the gastric cancer handling rules. The most important thing in the pathological diagnosis of ESD is to evaluate the complete removal of the lesion[5,22]. Here, we will explain several important points for the pathological diagnosis in ESD specimens. These are the size of the lesion, histological type, depth of the lesion, vessel invasion, ulcer scar and surgical margin, each of which are described in detail below.
Histological type: Generally, the histological type of gastric cancer is divided into the differentiated type and undifferentiated type (so-called diffuse type in the Laurén classification)[23] and the major histological type within the tumor is taken as the final pathological diagnosis according to the gastric cancer handling rules in Japan[19]. If a lesion is composed of only the differentiated type, the chance of vascular invasion and lymph node metastasis is low. However, if there is some of the undifferentiated type mixed within the tumor, the risk becomes high. Therefore, it is recommended to write the presence of the undifferentiated type component in the pathology report. When submucosal invasion is present, the histological type of the invasive portion is important and it is necessary to mention whether the invasive part shows only the differentiated type component or if it includes the undifferentiated type component because the histological type will determine whether or not additional treatment may be required.
Depth: pT1b is classified into two categories, namely pT1b1 (tumor depth of less than 0.5 mm from the lower edge of muscularis mucosae) and pT1b2 (tumor depth of 0.5 mm or more from the lower edge of muscularis mucosae), because the risk of lymph node metastases is significantly higher in cases belonging to the latter category[16]. When the muscularis mucosae are obscure due to myofibroblastic proliferation, it is recommended to identify the muscularis mucosae by using the immunohistochemical staining of desmin.
There are several practical methods available for the measurement of 0.5 mm. These are: (1) putting a thin transparent ruler directly on the glass slide; (2) using a measurement device of a microscopic digital camera; (3) measuring with the micrometer of the eyepiece; and (4) using a scale loupe (Figure 3). The depth of invasion in the ESD specimen is only determined in cases of negative vertical margin. In cases of positive vertical margin, the findings should be described, for example, as follows: “at least pT1b2/SM2: 1200 micrometers from muscularis mucosae”.
Figure 3.
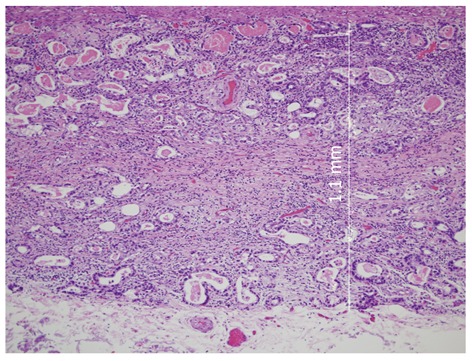
How to measure the depth in pT1b2 cases. Depth of a pT1b case indicates the distance from the lower edge of the muscularis mucosae to the invasive front of tumor.
Vessel invasion
The presence or absence of lymphatic permeation and vascular (vein) invasion is one of the important factors for the evaluation of additional therapy. In our institution, double staining with Victoria blue and hematoxylin-eosin (HE) for vascular invasion and immunohistochemistry of D2-40 for lymphatic invasion are routinely performed in all cases with submucosal invasion[24,25]. In addition, elastic Van Gieson stain and immunohistochemistry of CD31 or CD34 are widely used for the identification of vascular and lymphatic invasions (Figure 4)[26]. When special staining and immunohistochemistry are ordered, the lesion of vascular invasion may disappear due to a deeper cut. Therefore, caution should be made in cutting the block. In cases with obvious vascular invasion on HE-stained slides, we record its presence even if we cannot confirm such invasions by special staining or immunohistochemistry. Since lymphatic invasion can be present even in pT1a cases, careful microscopic examination is necessary (Figure 4).
Figure 4.
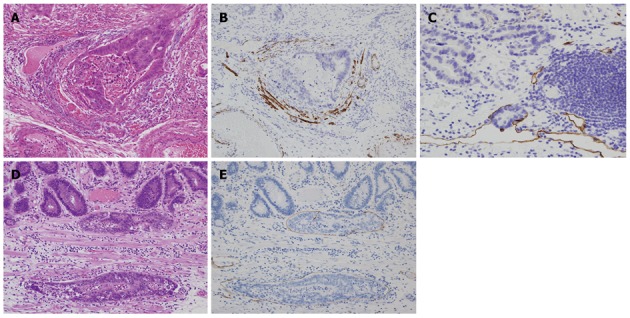
Evaluation of vessel invasion and lymphatic invasion. Venous invasion is evaluated by using a double staining with Victoria blue and hematoxylin-eosin (A) and immunohistochemistry of desmin (B). Lymphatic invasion is demonstrated by immunostaining of D2-40 (C). Lymphatic invasion is noted in the lamina propria (D: Hematoxylin-eosin stain; E: Immunohistochemistry of D2-40).
ULCER SCAR AND BIOPSY SCAR
The determination of curability of the lesion may be changed depending on the presence or absence of an ulcer or ulcer scar. An ulcer scar should be confirmed histologically, not endoscopically. Since a biopsy scar is not regarded as a real ulcer scar, it is necessary to confirm previous biopsy histories, including the biopsy site (Figures 5 and 6). Confirmation with endoscopists may be required, depending on the case.
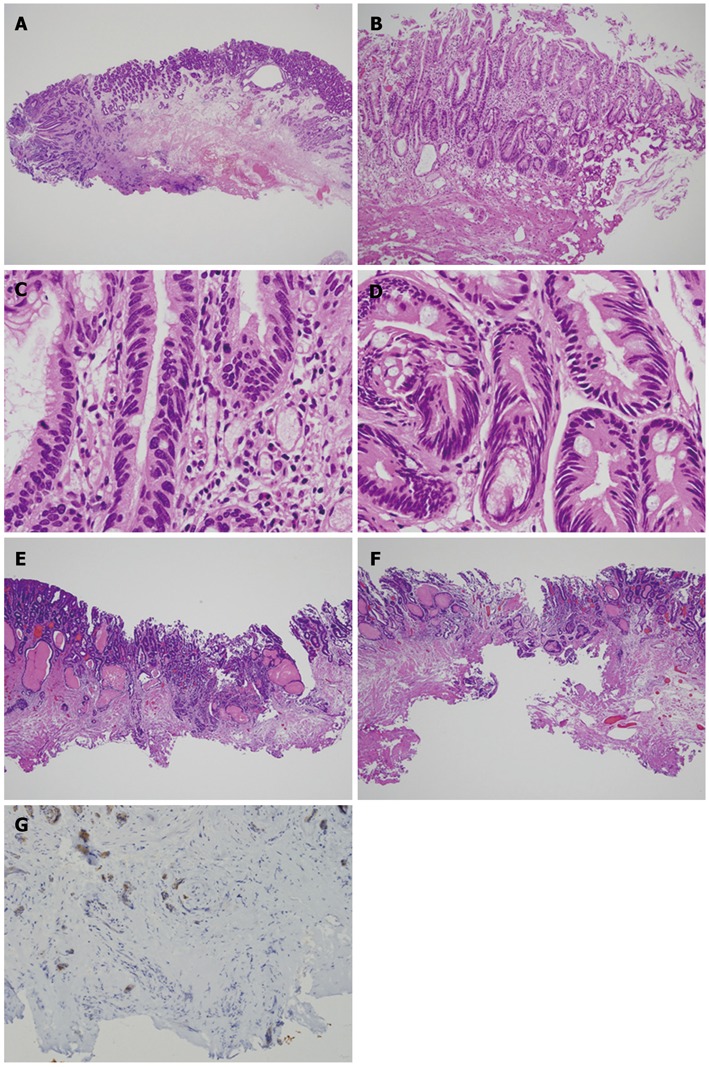
Figure 5.
Ulcer scar vs biopsy scar. Biopsy scar is a very localized lesion (A and B) and is noted at the site of biopsy. Therefore, clinical information is important. On the other hand, ulcer scar due to tumor is usually an expansive lesion (C and D). Clinical information of no history of biopsy is also useful.
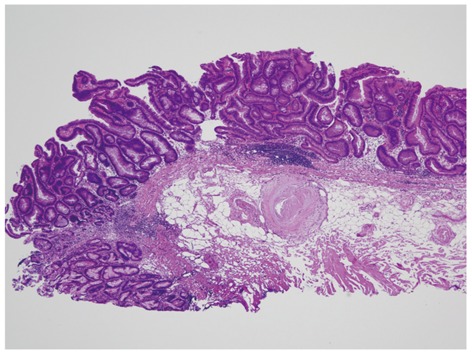
Figure 6.
Heterotopic submucosal glands (= gastritis cystica profunda). Heterotopic submucosal glands can be misdiagnosed endoscopically as an ulcer due to submucosal invasion. These lesions should be described in the pathology report and the lesional mapping diagram.
Evaluation of the surgical margins
Horizontal margin: To diagnose a negative horizontal margin, the first and last section should be free of cancer and both sides of all other sections should show no cancer. In the case of a negative horizontal margin, the distance (mm) to the margin should be recorded and in positive cases, it is recommended that the number of sections with positive margins be described. In cases with a cauterization effect, it is sometimes difficult to judge the horizontal margin (Figure 7). Although there is no conclusive solution in such cases, immunohistochemical staining of p53 and Ki-67 may be useful[27]. Detailed microscopic examination including nuclear and structural changes may be helpful in some cases. Recently, ESD has been performed for lesions measuring more than 5 cm. In such cases, an incidental lesion which was not detected preoperatively may be found and it may show a positive margin. Therefore, it should be kept in mind that multiple lesions may be present at the time of preoperative diagnosis.
Figure 7.
Cases of positive horizontal margin and vertical margin. In most cases, a positive margin is easily recognized (A); Some cases show marked degeneration by treatment (B); By careful microscopic examination, adenocarcinoma cells (C) can be distinguished from intestinalized epithelium (D). A positive vertical margin at the submucosal layer (E) or at the lamina propria (F) should be described in the pathology report. A positive vertical margin can be easily detected by using immunohistochemistry of keratin (G).
Vertical margin: When cancer cells are not exposed to an abrasion side in all sections, we make the diagnosis of a negative vertical margin and confirm the depth of invasion. In cases with positive vertical margins, as previously described in the section of the depth, both the positive site (either lamina propria or submucosa) and the distance from the lower edge of muscularis mucosae to the positive margin site should be recorded (Figure 7). When tumor cells are hard to identify due to cauterization, immunostains with keratin are useful. When the positive margin site shows no cauterization effect, the possibility of false positivity should be considered and recorded as such. Then, a more deeply cut section should be obtained. Since examination by re-embedding often does not work well, it is better to avoid such a preparation. In the case of a negative vertical margin, if tumor cells are close to the vertical margin, recording the distance from the abrasion margins to the tumor cells may be useful as information during follow-up.
COLON AND RECTUM
As for the endoscopic treatment of colorectal lesions, polypectomy is the main treatment since most lesions are pedunculated. ESD is performed for so-called lateral spread lesions[28]. The evaluation of ESD specimens follows that of polypectomy materials.
Biopsy diagnosis
The definition/diagnostic criteria of colorectal cancer are different in Japan and the west. High-grade intraepithelial neoplasia can be called carcinoma in Japan, while only submucosal invasive lesions can be called carcinoma in the west. Namely, intramucosal invasive lesions are included in high-grade dysplasia in the west. Therefore, the so-called western high-grade dysplasia can be a target for endoscopic treatment in Japan.
Characteristics of colonic ESD material
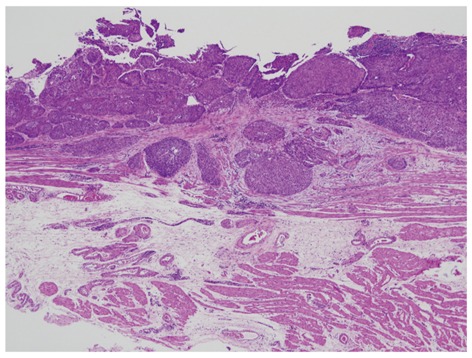
In the colon, pedunculated polypoid lesions are much more common compared to those in the stomach. However, some show sessile lesions, or so-called laterally spreading tumors (LSTs). LSTs are the most common target lesions in colonic ESD. Characteristics of large bowel ESD materials include predominantly polypoid lesions, often papillary or villous lesions with fragility, and thin walls compared to those in the stomach (Figure 8). It is desirable that all of the layers of the specimen should be examined microscopically. The rupture of the material by the excessive extension at fixation handling disturbs an accurate diagnosis (Figure 9).
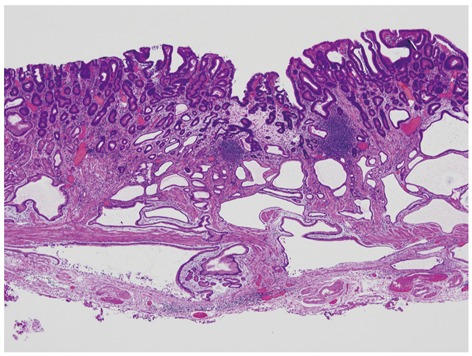
Figure 8.
Cutting of a sessile polypoid lesion. Non-tumor areas around the polypoid lesion are very thin. The submucosal layer of the tumor portion is also thin. Therefore, caution should be taken when preparing the specimen so that a false positive diagnosis of the vertical margin will not be made.
Figure 9.
Mucosal tears due to overextension during the tissue fixation.
Eligibility criteria for endoscopic treatment are based on the Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines (2010 edition). In the colorectal cancer treatment guidelines published in 2010, the principle of the endoscopic treatment is described as follows: “the size and the location of the lesion should be such that it can be excised en bloc, and there is a low risk of lymph node metastasis”. Eligibility criteria for endoscopic excision are (1) intramucosal carcinoma, or mildly invasive cancer into the submucosa; (2) less than 2 cm at the greatest diameter; and (3) macroscopic type is not taken into consideration[29,30]. In addition, the adaptation of colonic ESD for adenoma includes lesions which are 2 cm or more at the greatest diameter with lateral spread lesions or sessile lesions, lesions with an ulcer scar and recurrent lesions; while that for carcinoma is adenocarcinoma with cT1b1 (SM1) which is 2 cm or less at the greatest diameter.
Eligibility criteria for additional treatment after endoscopic excision
In cases with positive horizontal or vertical margins, additional surgical resection is recommended (Figure 10)[5]. In addition, surgical resection is considered if any one of the following factors is present: (1) pT1b1 (deeper than 1000 micrometers from the lower border of muscularis mucosae); (2) positive lymphovascular invasion (ly, v); (3) poorly differentiated adenocarcinoma, signet ring cell carcinoma and mucinous carcinoma; and (4) budding/sprouting at the invasive front showing Grade 2 to 3. Therefore, it is important to evaluate these factors in ESD materials of the colon[31-33].
Figure 10.
Positive horizontal margin in the colonic endoscopic submucosal dissection. In appropriate pathology specimens, the evaluation of the margin is relatively easy.
Pathological diagnosis specific to colonic lesions
Unlike gastric lesions, large intestinal lesions predominantly show pedunculated lesions. Therefore, special attention should be paid to submucosal invasion and the grading of budding/sprouting.
Evaluation of submucosal invasion
Most colorectal lesions are pedunculated or sub-pedunculated and are usually treated by polypectomy or EMR. In recent years, however, ESD has been used for the treatment of non-polypoid 0-IIc type lesions as well as LST type lesions. Regarding the evaluation of submucosal invasion, there are some differences between pedunculated lesions and non-pedunculated lesions in the colon. When it is possible to identify the muscularis mucosae, the depth of submucosal invasion is the distance from the deeper edge of the muscularis mucosae to the deepest invasive portion. When muscularis mucosae cannot be identified, the depth of submucosal invasion is the distance between the surface of the tumor and the deepest invasive portion. In polypoid tumors with disrupted muscularis mucosae, the depth of submucosal invasion is the distance between the deepest invasive site and the reference line, defined as the boundary between the tumor head and the pedicle. Migration of adenomatous glands (dysplastic glands in the west) should be differentiated from the true submucosal invasion[34].
Budding/sprouting grading
When cancer cells reveal an isolated or small cluster pattern in the invasive front in the large bowel pT1b cancer, it is most likely to be lymph node metastasis. Budding/sprouting is defined as a small cluster of cancer cells consisting of less than 5 tumor cells at the invasive front. When the most highly concentrated area is examined under × 200 magnification, 0-4 clusters can be graded as Grade 1, 5-9 clusters as Grade 2, and 10 or more clusters as Grade 3. Grade 2 and Grade 3 show a significantly higher risk of lymph node metastasis than Grade 1. Therefore, in cases with submucosal invasion, it is required to describe the budding/sprouting grading in the report[33,35-38].
ESOPHAGUS
Eligibility criteria for endoscopic treatment are based on Esophageal Cancer Diagnosis Treatment Guidelines (Second Edition, 2007).
The endoscopic ablative adaptation of esophageal cancer is as follows: carcinoma in situ [pT1a-EP (M1)], tumor-invaded lamina propria mucosa [pT1a-LPM (M2)], or tumor-invaded mucosa (pT1a). Since these lesions show extremely rare lymph node metastases, radical cure can be obtained by the ESD procedure. Because of the occurrence of cicatricial stenosis after ESD, adaptation of ESD is limited to the cases with less than two-thirds circumferential lesion. The lesions which have invaded the muscularis mucosa [pT1a-MM (M3)] or invaded the submucosa up to a depth of 200 micrometers or less from the lamina muscularis mucosa (pT1b-SM1 in ESD criteria) are a relatively indicative lesion because of the risk of lymph node metastasis. In addition, total circumferential lesion in pT1a-MM (M3) and pT1b-SM1 is a relative indicative lesion. The lesion invading the submucosa with a depth of more than 200 micrometers from the lamina muscularis mucosa (pT1b-SM2 in ESD criteria) has a 50% risk of lymph node metastasis[39]; therefore, these lesions are treated in accordance with the treatment of progressive cancer[40-42].
Characteristics of esophagus ESD materials
In esophageal ESD materials, the mucosal epithelium and lamina propria separates easily and the marginal portion is easily fragmented. Since a lesion can be recognizable by Lugol dispersion, cutting after Lugol staining is useful. Caution should be made to examine all of the layers microscopically (Figure 11). In cases of esophageal cancer with invasion deeper than the lamina propria mucosa, the invasive pattern should be recorded, since the risk of lymphovascular invasion differs depending on the invasive patterns, namely expansive pattern or infiltrating pattern (Figure 12)[43-45].
Figure 11.
Early esophageal cancer in endoscopic submucosal dissection specimen. The marginal portion (squamous epithelium) of the specimen is very thin. Therefore, it is difficult to make a section (yellow circle) and may cause false positivity of the surgical margin.
Figure 12.
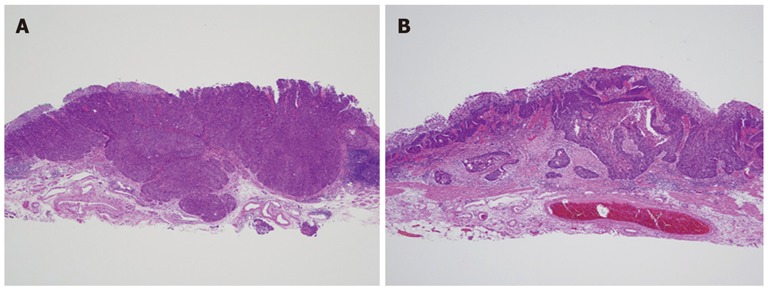
Invasive patterns in squamous cell carcinoma of the esophagus. Expansive pattern (A) and infiltrative pattern (B) should be described in the pathology report.
In cases of Barrett’s esophageal cancer, double layers of the muscularis mucosae is known[46]. Around the muscularis mucosae, vasculatures and lymphatic channels are well developed and there is the possibility of lymph node metastasis. However, the relationship between the depth of early stage Barrett’s esophageal cancer and lymph node metastasis is not clear in Japan. Therefore, cases with pT1a-MM (M3) are divided into pT1a-superficial muscularis mucosae, pT1a- LPM and pT1a-deep muscularis mucosae in Japan and we are now collecting these cases for evaluation (Figure 13). In cases with esophageal ESD, it is sometimes difficult to judge the horizontal margin and in such cases, immunohistochemical staining of p53 and Ki-67 may be useful (Figure 14).
Figure 13.
pT1a-superficial muscularis mucosae case. The lower portion of the picture shows two-layered muscularis mucosae. In esophageal cancers with pT1a-MM (M3), the depth of invasion is divided into three (pT1a-superficial muscularis mucosae, pT1a-lamina propria mucosae and pT1a-deep muscularis mucosae).
Figure 14.
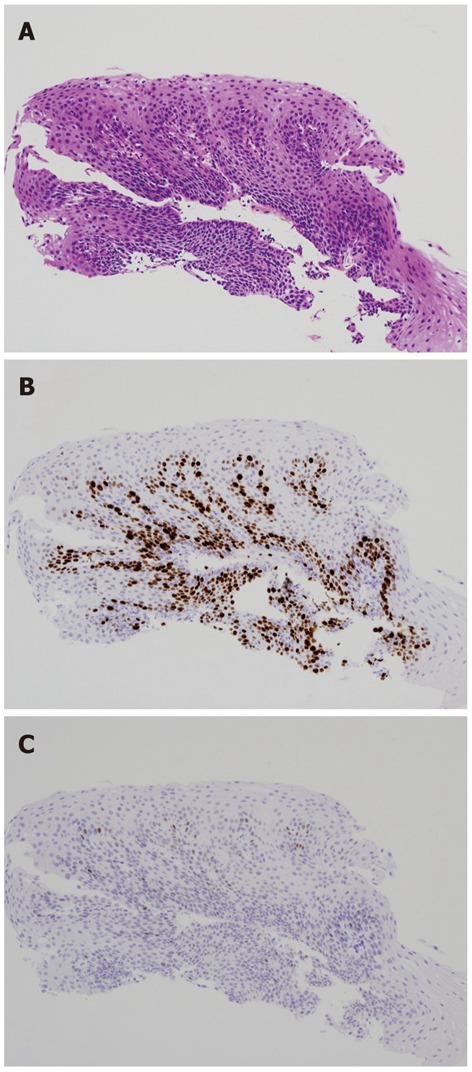
Evaluation of horizontal margin in the esophageal endoscopic submucosal dissection. Compared to hematoxylin-eosin stain (A); immunohistochemical stainings of Ki-67 (B) and p53 (C) highlight the lesion.
CONCLUSION
We described several important points to be considered in ESD materials. For accurate pathological diagnosis, it is essential to make appropriate pathology specimens, including HE glass slides. Furthermore, it is important for pathologists to understand the factors related to the prognosis and to communicate with endoscopists.
Footnotes
Peer reviewers: Wai-Keung Chow, Visiting Staff, Division of Gastroenterology, Department of Internal Medicine, China Medical University Hospital, Taichung 40001, Taiwan, China; Jochen Wedemeyer, MD, Department of Gastroenterology, Hepatology and Endocrinology, Medical School Hannover, Carl Neuberg Str. 1, 30625 Hannover, Germany
S- Editor Song XX L- Editor Roemmele A E- Editor Zhang DN
References
- 1.Kudo S. Endoscopic mucosal resection of flat and depressed types of early colorectal cancer. Endoscopy. 1993;25:455–461. doi: 10.1055/s-2007-1010367. [DOI] [PubMed] [Google Scholar]
- 2.Oyama T, Tomori A, Hotta K, Morita S, Kominato K, Tanaka M, Miyata Y. Endoscopic submucosal dissection of early esophageal cancer. Clin Gastroenterol Hepatol. 2005;3:S67–S70. doi: 10.1016/s1542-3565(05)00291-0. [DOI] [PubMed] [Google Scholar]
- 3.Ono H. Early gastric cancer: diagnosis, pathology, treatment techniques and treatment outcomes. Eur J Gastroenterol Hepatol. 2006;18:863–866. doi: 10.1097/00042737-200608000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Takahashi H, Arimura Y, Masao H, Okahara S, Tanuma T, Kodaira J, Kagaya H, Shimizu Y, Hokari K, Tsukagoshi H, et al. Endoscopic submucosal dissection is superior to conventional endoscopic resection as a curative treatment for early squamous cell carcinoma of the esophagus (with video) Gastrointest Endosc. 2010;72:255–264, 264.e1-2. doi: 10.1016/j.gie.2010.02.040. [DOI] [PubMed] [Google Scholar]
- 5.Tanaka S, Oka S, Chayama K. Colorectal endoscopic submucosal dissection: present status and future perspective, including its differentiation from endoscopic mucosal resection. J Gastroenterol. 2008;43:641–651. doi: 10.1007/s00535-008-2223-4. [DOI] [PubMed] [Google Scholar]
- 6.Kuwabara T, Hiyama T, Oka S, Urabe Y, Tanaka S, Yoshihara M, Arihiro K, Shimamoto F, Chayama K. Clinical features of pharyngeal intraepithelial neoplasias and outcomes of treatment by endoscopic submucosal dissection. Gastrointest Endosc. 2012:Epub ahead of print. doi: 10.1016/j.gie.2012.07.032. [DOI] [PubMed] [Google Scholar]
- 7.Hanaoka N, Ishihara R, Takeuchi Y, Suzuki M, Uemura H, Fujii T, Yoshino K, Uedo N, Higashino K, Ohta T, et al. Clinical outcomes of endoscopic mucosal resection and endoscopic submucosal dissection as a transoral treatment for superficial pharyngeal cancer. Head Neck. 2012:Epub ahead of print. doi: 10.1002/hed.23106. [DOI] [PubMed] [Google Scholar]
- 8.Fujishiro M. Perspective on the practical indications of endoscopic submucosal dissection of gastrointestinal neoplasms. World J Gastroenterol. 2008;14:4289–4295. doi: 10.3748/wjg.14.4289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abe N, Watanabe T, Suzuki K, Machida H, Toda H, Nakaya Y, Masaki T, Mori T, Sugiyama M, Atomi Y. Risk factors predictive of lymph node metastasis in depressed early gastric cancer. Am J Surg. 2002;183:168–172. doi: 10.1016/s0002-9610(01)00860-1. [DOI] [PubMed] [Google Scholar]
- 10.Kunisaki C, Takahashi M, Nagahori Y, Fukushima T, Makino H, Takagawa R, Kosaka T, Ono HA, Akiyama H, Moriwaki Y, et al. Risk factors for lymph node metastasis in histologically poorly differentiated type early gastric cancer. Endoscopy. 2009;41:498–503. doi: 10.1055/s-0029-1214758. [DOI] [PubMed] [Google Scholar]
- 11.Yamao T, Shirao K, Ono H, Kondo H, Saito D, Yamaguchi H, Sasako M, Sano T, Ochiai A, Yoshida S. Risk factors for lymph node metastasis from intramucosal gastric carcinoma. Cancer. 1996;77:602–606. doi: 10.1002/(SICI)1097-0142(19960215)77:4<602::AID-CNCR3>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 12.Mita T, Shimoda T. Risk factors for lymph node metastasis of submucosal invasive differentiated type gastric carcinoma: clinical significance of histological heterogeneity. J Gastroenterol. 2001;36:661–668. doi: 10.1007/s005350170028. [DOI] [PubMed] [Google Scholar]
- 13.Alvarez Herrero L, Pouw RE, van Vilsteren FG, ten Kate FJ, Visser M, van Berge Henegouwen MI, Weusten BL, Bergman JJ. Risk of lymph node metastasis associated with deeper invasion by early adenocarcinoma of the esophagus and cardia: study based on endoscopic resection specimens. Endoscopy. 2010;42:1030–1036. doi: 10.1055/s-0030-1255858. [DOI] [PubMed] [Google Scholar]
- 14.Japanese gastric cancer association. Gastric cancer treatment guidelines 2010. 3 ed. Tokyo: Kanehara; 2010. [Google Scholar]
- 15.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3) Gastric Cancer. 2011;14:113–123. doi: 10.1007/s10120-011-0042-4. [DOI] [PubMed] [Google Scholar]
- 16.Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, Kato Y. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–225. doi: 10.1007/pl00011720. [DOI] [PubMed] [Google Scholar]
- 17.Hirasawa T, Gotoda T, Miyata S, Kato Y, Shimoda T, Taniguchi H, Fujisaki J, Sano T, Yamaguchi T. Incidence of lymph node metastasis and the feasibility of endoscopic resection for undifferentiated-type early gastric cancer. Gastric Cancer. 2009;12:148–152. doi: 10.1007/s10120-009-0515-x. [DOI] [PubMed] [Google Scholar]
- 18.Hanaoka N, Tanabe S, Mikami T, Okayasu I, Saigenji K. Mixed-histologic-type submucosal invasive gastric cancer as a risk factor for lymph node metastasis: feasibility of endoscopic submucosal dissection. Endoscopy. 2009;41:427–432. doi: 10.1055/s-0029-1214495. [DOI] [PubMed] [Google Scholar]
- 19.Japanese gastric cancer association. Japanese classification of gastric cancer. Tokyo: Kanehara; 2010. [DOI] [PubMed] [Google Scholar]
- 20.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–112. doi: 10.1007/s10120-011-0041-5. [DOI] [PubMed] [Google Scholar]
- 21.Schlemper RJ, Riddell RH, Kato Y, Borchard F, Cooper HS, Dawsey SM, Dixon MF, Fenoglio-Preiser CM, Fléjou JF, Geboes K, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000;47:251–255. doi: 10.1136/gut.47.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yokoi C, Gotoda T, Hamanaka H, Oda I. Endoscopic submucosal dissection allows curative resection of locally recurrent early gastric cancer after prior endoscopic mucosal resection. Gastrointest Endosc. 2006;64:212–218. doi: 10.1016/j.gie.2005.10.038. [DOI] [PubMed] [Google Scholar]
- 23.Lauren P. The two histological main types of gastric carcinoma: Diffuse and so-called intestinal-type carcinoma. an attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 1965;64:31–49. doi: 10.1111/apm.1965.64.1.31. [DOI] [PubMed] [Google Scholar]
- 24.Sako A, Kitayama J, Ishikawa M, Yamashita H, Nagawa H. Impact of immunohistochemically identified lymphatic invasion on nodal metastasis in early gastric cancer. Gastric Cancer. 2006;9:295–302. doi: 10.1007/s10120-006-0396-1. [DOI] [PubMed] [Google Scholar]
- 25.Yonemura Y, Endou Y, Tabachi K, Kawamura T, Yun HY, Kameya T, Hayashi I, Bandou E, Sasaki T, Miura M. Evaluation of lymphatic invasion in primary gastric cancer by a new monoclonal antibody, D2-40. Hum Pathol. 2006;37:1193–1199. doi: 10.1016/j.humpath.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 26.del Casar JM, Corte MD, Alvarez A, García I, Bongera M, González LO, García-Muñiz JL, Allende MT, Astudillo A, Vizoso FJ. Lymphatic and/or blood vessel invasion in gastric cancer: relationship with clinicopathological parameters, biological factors and prognostic significance. J Cancer Res Clin Oncol. 2008;134:153–161. doi: 10.1007/s00432-007-0264-3. [DOI] [PubMed] [Google Scholar]
- 27.Sugai T, Inomata M, Uesugi N, Jiao YF, Endoh M, Orii S, Nakamura S. Analysis of mucin, p53 protein and Ki-67 expressions in gastric differentiated-type intramucosal neoplastic lesions obtained from endoscopic mucosal resection samples: a proposal for a new classification of intramucosal neoplastic lesions based on nuclear atypia. Pathol Int. 2004;54:425–435. doi: 10.1111/j.1440-1827.2004.01643.x. [DOI] [PubMed] [Google Scholar]
- 28.Kudo S, Kashida H, Tamura T, Kogure E, Imai Y, Yamano H, Hart AR. Colonoscopic diagnosis and management of nonpolypoid early colorectal cancer. World J Surg. 2000;24:1081–1090. doi: 10.1007/s002680010154. [DOI] [PubMed] [Google Scholar]
- 29.Japanese society for cancer of the colon and rectum. JSCCR guidelines 2010 for the treatment of colorectal cancer. Tokyo: Kanehara; 2010. [DOI] [PubMed] [Google Scholar]
- 30.Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol. 2012;17:1–29. doi: 10.1007/s10147-011-0315-2. [DOI] [PubMed] [Google Scholar]
- 31.Kitajima K, Fujimori T, Fujii S, Takeda J, Ohkura Y, Kawamata H, Kumamoto T, Ishiguro S, Kato Y, Shimoda T, et al. Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study. J Gastroenterol. 2004;39:534–543. doi: 10.1007/s00535-004-1339-4. [DOI] [PubMed] [Google Scholar]
- 32.Ueno H, Mochizuki H, Hashiguchi Y, Shimazaki H, Aida S, Hase K, Matsukuma S, Kanai T, Kurihara H, Ozawa K, et al. Risk factors for an adverse outcome in early invasive colorectal carcinoma. Gastroenterology. 2004;127:385–394. doi: 10.1053/j.gastro.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 33.Tateishi Y, Nakanishi Y, Taniguchi H, Shimoda T, Umemura S. Pathological prognostic factors predicting lymph node metastasis in submucosal invasive (T1) colorectal carcinoma. Mod Pathol. 2010;23:1068–1072. doi: 10.1038/modpathol.2010.88. [DOI] [PubMed] [Google Scholar]
- 34.Japanese society for cancer of the colon and rectum. Japanese classification of colorectal carcinoma. 2rd ed. Tokyo: Kanehara; 2009. [Google Scholar]
- 35.Nakamura T, Mitomi H, Kanazawa H, Ohkura Y, Watanabe M. Tumor budding as an index to identify high-risk patients with stage II colon cancer. Dis Colon Rectum. 2008;51:568–572. doi: 10.1007/s10350-008-9192-9. [DOI] [PubMed] [Google Scholar]
- 36.Okuyama T, Nakamura T, Yamaguchi M. Budding is useful to select high-risk patients in stage II well-differentiated or moderately differentiated colon adenocarcinoma. Dis Colon Rectum. 2003;46:1400–1406. doi: 10.1007/s10350-004-6757-0. [DOI] [PubMed] [Google Scholar]
- 37.Morodomi T, Isomoto H, Shirouzu K, Kakegawa K, Irie K, Morimatsu M. An index for estimating the probability of lymph node metastasis in rectal cancers. Lymph node metastasis and the histopathology of actively invasive regions of cancer. Cancer. 1989;63:539–543. doi: 10.1002/1097-0142(19890201)63:3<539::aid-cncr2820630323>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 38.Prall F. Tumour budding in colorectal carcinoma. Histopathology. 2007;50:151–162. doi: 10.1111/j.1365-2559.2006.02551.x. [DOI] [PubMed] [Google Scholar]
- 39.Eguchi T, Nakanishi Y, Shimoda T, Iwasaki M, Igaki H, Tachimori Y, Kato H, Yamaguchi H, Saito D, Umemura S. Histopathological criteria for additional treatment after endoscopic mucosal resection for esophageal cancer: analysis of 464 surgically resected cases. Mod Pathol. 2006;19:475–480. doi: 10.1038/modpathol.3800557. [DOI] [PubMed] [Google Scholar]
- 40.Kim DU, Lee JH, Min BH, Shim SG, Chang DK, Kim YH, Rhee PL, Kim JJ, Rhee JC, Kim KM, et al. Risk factors of lymph node metastasis in T1 esophageal squamous cell carcinoma. J Gastroenterol Hepatol. 2008;23:619–625. doi: 10.1111/j.1440-1746.2007.05259.x. [DOI] [PubMed] [Google Scholar]
- 41.Chiba T, Kawachi H, Kawano T, Kumagai J, Kitagaki K, Sekine M, Uchida K, Kobayashi M, Sugihara K, Eishi Y. Independent histological risk factors for lymph node metastasis of superficial esophageal squamous cell carcinoma; implication of claudin-5 immunohistochemistry for expanding the indications of endoscopic resection. Dis Esophagus. 2010;23:398–407. doi: 10.1111/j.1442-2050.2009.01023.x. [DOI] [PubMed] [Google Scholar]
- 42.Japan esophageal society. Japanese classification of esophageal cancer. 10th ed. Tokyo: Kanehara; 2008. [Google Scholar]
- 43.Miyata H, Yoshioka A, Yamasaki M, Nushijima Y, Takiguchi S, Fujiwara Y, Nishida T, Mano M, Mori M, Doki Y. Tumor budding in tumor invasive front predicts prognosis and survival of patients with esophageal squamous cell carcinomas receiving neoadjuvant chemotherapy. Cancer. 2009;115:3324–3334. doi: 10.1002/cncr.24390. [DOI] [PubMed] [Google Scholar]
- 44.Koike M, Kodera Y, Itoh Y, Nakayama G, Fujiwara M, Hamajima N, Nakao A. Multivariate analysis of the pathologic features of esophageal squamous cell cancer: tumor budding is a significant independent prognostic factor. Ann Surg Oncol. 2008;15:1977–1982. doi: 10.1245/s10434-008-9901-6. [DOI] [PubMed] [Google Scholar]
- 45.Roh MS, Lee JI, Choi PJ. Tumor budding as a useful prognostic marker in esophageal squamous cell carcinoma. Dis Esophagus. 2004;17:333–337. doi: 10.1111/j.1442-2050.2004.00436.x. [DOI] [PubMed] [Google Scholar]
- 46.Takubo K, Aida J, Naomoto Y, Sawabe M, Arai T, Shiraishi H, Matsuura M, Ell C, May A, Pech O, et al. Cardiac rather than intestinal-type background in endoscopic resection specimens of minute Barrett adenocarcinoma. Hum Pathol. 2009;40:65–74. doi: 10.1016/j.humpath.2008.06.008. [DOI] [PubMed] [Google Scholar]


