Abstract
Background:
Failure to ventilate patients by mask leads to serious complications especially if associated with difficult intubation. Previous studies have used subjective and indirect measures to evaluate difficulty in mask ventilation, which are associated with high inter-observer discrepancies. In this study, we have defined and used efficiency of mask ventilation (EMV) as an objective and direct surrogate for ease of mask ventilation in patients undergoing GA and mask ventilation using neuromuscular relaxation.
Materials and Methods:
1050 adult patients prospectively were evaluated with respect to different patients demographic and physical factors and EMV. EMV was defined as the ratio of minute ventilation via anesthesia mask to that via tracheal tube expressed as percentage. Edentolous patients were ventilated using lip-over-mask techniques. Separate analyses were done for edentolous and non-edentolous patients.
Results:
EMV in edentolous patients (n=269) using the lip-over-mask method was relatively high (90.9 ± 14.3%, 60.14–128.57 range). The result of multiple regression analysis in patients with normal denture determined receded chin, presence of beard, male gender, high Mallampati classes, high neck circumference, low inter-incisors gap, and old age as independent factors for estimating EMV. A regression formula for predicting EMV was developed which had an acceptable R-square value with a good model fit.
Conclusions:
Using EMV is an easy and reliable tool for measuring efficiency of mask ventilation. Based on the result of this study, EMV can be estimated from patient's demographic and physical factors. In edentolous patients, using the lip-over-mask method results in adequate ventilation of lungs.
Keywords: Anesthesia complications, difficult mask ventilation, efficiency of mask ventilation, multiple regression analysis
INTRODUCTION
Airway management of anesthetized patients is one of the most important responsibilities of anesthesiologist. Using mask ventilation is the primary means of maintaining airway and providing adequate ventilation and oxygenation before attempting tracheal intubation. Should the later proves difficult or impossible, ability to provide adequate ventilation via a face mask will be the most important factor in preventing hypoxia development and subsequent neurological damage.[1] In spite of many progress in anesthesia practice, difficult airway continues to be the most common factor associated with patient mortality and morbidity related to the airway problems.[2,3] Difficulty in establishing an adequate airway manifests either as difficult intubation (DI), difficult mask ventilation (DMV), or both. Patients factors used for prediction of DMV in most studies have nearly been the same as those associated with difficult intubation, including Mallampati score of pharyngeal view, degree of mouth opening, ability to protrude mandible, receding chin, head extension over atlanto-occipital joint, upper incisors protrusion, thyromental distance, body weight, history of snoring, and chronic obstructive pulmonary diseases.[4,5] In addition, there are factors specific to the prediction of difficult mask ventilation which include the presence of beard, edentulous, and old age.[6]
Current physical and demographic predictors still have a high rates of inaccuracies specially those of false positive.[4–8] Part of the problem is related to confusion in perception of what actually a DMV is. Lack of an standard objective definition for DMV makes a comparison of studies related to DMV more difficult.[9] In addition, in the previous studies on mask ventilation, researchers invariably looked for indirect surrogates of mask ventilation such as cyanosis, low oxygen saturation, low exhaled CO2, breath sounds, chest movement, gastric dilatation, need for more fresh gas flow, inadequate mask seal, excessive gas leak, increased resistance to flow and need for additional operators.[1,4–7] All of these factors are subjective with large inter-observer variability which together with low incidence of DMV make the necessary sample size for studying its incidence and its predisposing factors relatively large. Objective measures on the other hand are independent of observers’ judgment and seem to be associated with more predictable result, which lowers the necessary sample size. To our best knowledge, no previous study has attempted to define and study the efficiency of mask ventilation (EMV) in terms of measured post-induction tidal volume and predicting its value based on the patients characteristics. In this study, a simple and objective measurement for adequacy of mask ventilation based on measurement of exhaled tidal volume has been defined and studied in a sample of adult patients undergoing general anesthesia for elective operations.
MATERIALS AND METHODS
After institutional approval and informed written consent, 1050 adult patients undergoing general anesthesia and tracheal intubation for elective surgical procedures have been studied prospectively.
Sample size was determined by the proposed formula by Cohen:[10]
N = (L(1 – R2)/R2) + u + 1
Where N = total sample size
L = effect size index
R2 = estimated coefficient of variation
u = number of independent variables
A value of 35.7 for L was obtained from statistical tables[10] using a significance level of 0.05, a study power of 80% and total number of independent variables of 17. A value of 0.0346 for R2 was obtained by a pilot study on a sample of 50 patients. Number of independent variables was 17. Substituting the values in the sample size formula
N = (35.7(1 – 0.0346)/0.0346) + 17 + 1 = 1049.7919 = 1050
Patients scheduled for non-conventional modes of intubation (awake, fiberoptic, retrograde, etc), those with face trauma or airway pathology, and patients with acute respiratory problems were excluded. The study lasted 1 year in which all eligible cases from any of three university hospitals were managed by the second author during his third year of anesthesiology residency course (a 4 year course). Patients with abnormal occlusion due to significant loss of teeth, who did not have artificial denture, were excluded from the study. During pre-anesthesia visit before entering the operating room, patients were evaluated and different demographic and physical characteristics possibly associated with difficult mask ventilation or intubation were recorded.[4–8] These included age, weight, height, gender, presence of beard, Mallampati score, upper lip bite test, thyromental distance, chin receding, inter-incisors gap, head extension, and neck circumference. In addition, history of chronic obstructive pulmonary diseases, bronchial asthma, and snoring in sleep were recorded. Thyromental distance was measured as the distance from tip of the chin and thyroid notch in millimeter with the head in extension. Inter-incisors gap was measured in millimeter as the gap between upper and lower incisors with moth full open. Neck circumference was measured as the circumference of the neck at the level of cricoid cartilage with the head in the neutral position.
Patients were anesthetized using intravenous induction. Non-depolarizing muscle relaxants and short-acting narcotics were used to facilitate mask ventilation and tracheal intubation. After loss of consciousness and apnea, mask ventilation was started via a fitted anesthesia mask using two-hand method. Ventilation was controlled mechanically by anesthesia machine ventilator, using oxygen 8 L/min, a tidal volume of 10 mL/kg and a respiratory rate of 20/min with an I: E ratio of 1:2. Maximum allowed inspiratory pressure (i.e. pressure limit) was set to 25 cmH2O. Anesthesia machines and ventilators were inspected and calibrated every 4 months by a professional from vendor companies. Edentolous patients were ventilated without artificial denture in place, using a lip-over-mask technique as described by Racine and coworkers.[11]
Maximum exhaled minute volume by mask ventilation and through the tracheal tube were recorded using the same ventilatory settings. Maximum inspiratory pressure and positive end-expiratory pressure associated with these maximum minute volumes were also recorded. Volumes and pressures were measured by the anesthesia ventilator.
EMV was defined as the ratio of maximum minute volume with mask ventilation to the one with tracheal tube, expressed as a percentage value.
No airway adjunct was used with mask ventilation, except in cases of difficult mask ventilation where pulse oxymetric saturation dropped below 94%. In these cases, after recording the best values for minute volume and its associated airway pressures, other necessary devices or techniques were used to prevent further drop in oxygen saturation. Difficulty of mask ventilation was graded using the method described by Han and coworkers.[12]
Statistical analysis
Data were reported as Mean ± SD or n(%) where appropriate. Pearson and Spearman correlation analysis was used to correlate EMV with quantitative and qualitative characteristics of the patients respectively. Multiple regression analysis with the forward conditional method was used to predict the EMV based on demographic and physical characteristics of patients. A P value less than 0.05 was considered as statistically significant. The values for correlation coefficients of 0.1, 0.3, and 0.5 were considered as small, medium, and large, respectively.[13] Data were analyzed using R statistical software.[14]
RESULTS
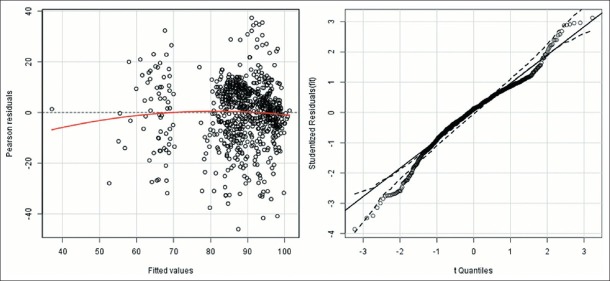
A total of 1050 cases were studied, 269 of them were edentolous. Because the EMV in edentolous patients using the lip-over-mask method was relatively high (90.9 ± 14.3, 60.14 – 128.57 range) and since some difficult airway indices were not measurable in them (upper lip bite test and inter-incisors gap), we decided to separate statistical analysis of edentolous patients, but due to their relatively small sample size no significant regression model was obtained. Therefore, final statistical analysis presented only for patients with normal denture (n=781). Figure 1 displays the frequency distribution for EMV. There was no patient with impossible mask ventilation. Proportion of patients with EMV less than 60% was 45 (5.8, 4.3–7.7 CI 95%). The lowest value for EMV was 19%. Post-intubation minute volume decreased in 95 (12.2%) patients, which resulted in an EMV more than 100%. These patients had higher values for maximum inspiratory pressure after intubation (21.4 ± 3.5 vs. 20.2 ± 3.5 in EMV less than 100% subjects, P=0.003).
Figure 1.
Frequency distribution for efficiency of mask ventilation
EMV had significant correlations with age, weight, thyromental distance, neck-circumference, beard, gender, chin receding, Mallampati class, neck-circumference and inter-incisors gap [P<0.01, Table 1]. Mean values for EMV were significantly higher in patients with beard, receding chin, high Mallampati classes, and in male patients [Table 2]. Multiple linear regression analysis showed that chin receding, beard, gender, Mallampati classes, neck-circumference, inter-incisors gap, and age are independent predictors of EMV in order of importance. The resulted regression model had a good fit (F=60, P=0.000) and a medium to strong predicting power (R=0.6, R-squared=0.36, P=0.000). Analysis of residuals revealed appropriate provision of model assumptions [Figure 2]. Using the produced model, EMV can be predicted using following regression formula:
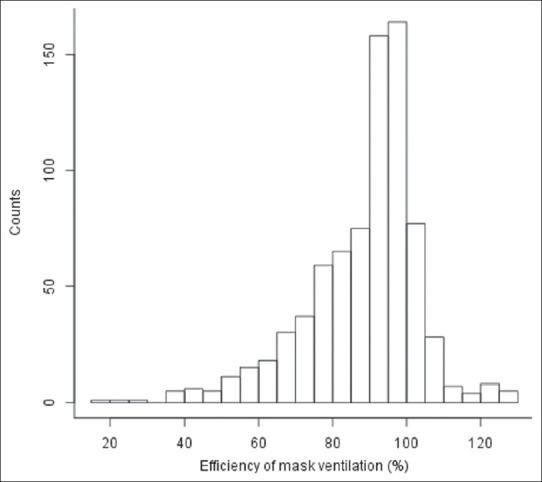
Table 1.
Demographic and physical characteristics of patients (n=781). Data are mean±sd or n (%), ranges for quantitative data, ci 95% for frequency data. The last column is coefficients of correlation between each independent factor and efficiency of mask ventilation
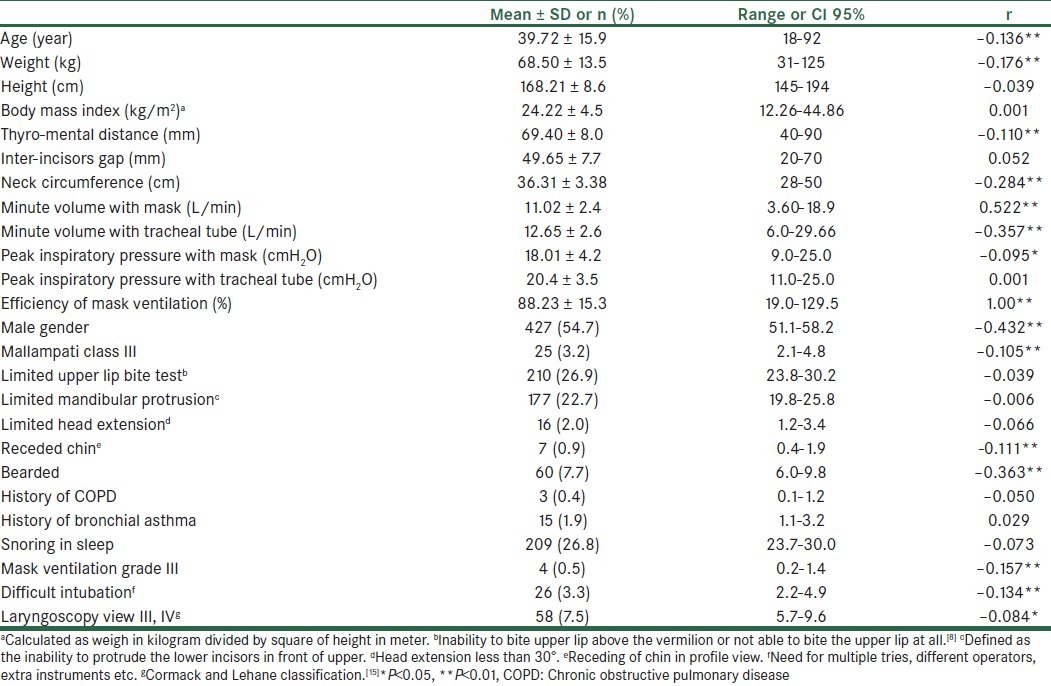
Table 2.
efficiency of mask ventilation compared among levels of independent factors, grades of mask ventilation, and difficulty of intubation

Figure 2.
Residual plots for the regression model
EMV = 113.5 – 26.7 × C – 19.5 × B – 8 × G – 2.8 × M – 0.55 × N + 0.15 × I – 0.06 × A
Where:
EMV = Efficiency of mask ventilation as percentage of ventilation by tracheal tube
C = Chin (0 = normal, 1 = receded)
B = Beard (0 = no beard, 1 = bearded)
G = Gender (0 = female, 1 = male)
M = Mallampati class (1, 2, 3, 4)
N = Neck circumference in cm
I = Inter-incisors gap in mm
A = Age in year
No patient had difficult mask ventilation grade 4 and only four patients had grade 3 difficult mask ventilation, in whom the minimum and maximum values for EMV were 24.7 and 43.8, respectively.
Mean values of EMV were significantly lower in patients with higher grades of difficult mask ventilation (II and III), and in those with difficult intubation. The correlations between difficulty of mask ventilation and tracheal intubation on one side and EMV on the other side although were significant but less than medium in size (r = –0.27 and –0.18 for difficult mask ventilation and difficult intubation respectively, P<0.01), and no significant predicting model existed between them.
DISCUSSION
In this study, we developed a model for predicting EMV following induction of general anesthesia and start of mask ventilation. EMV is a simple and objective tool for defining and studying relative ease of mask ventilation. It is estimated that about 6% of patients undergoing general anesthesia and mask ventilation have an EMV of less than 60%. Patients’ characteristics associated with a decrease in EMV in order of importance are receded chin, presence of beard, male gender, high Mallampati classes, high neck-circumference, low inter-incisors gap, and old age.
The association between EMV and difficult mask ventilation may not be as strong as expected, which imply different assumptions for each. EMV is a pure quantitative and direct surrogate for measuring ease of tidal volume delivery via anesthesia mask. The difficult mask ventilation scale on the other hand is subjective, indirect, and qualitative in nature[12] and cannot be finely enumerated for the degree of difficulty in mask ventilation. In addition, the usage direction for EMV is tailored toward the ease of mask ventilation, whereas the domain of difficult mask ventilation scale is mainly limited to the detection of difficulty in mask ventilation and its consequences. Since EMV compares the minute volume via mask to that of the tracheal tube, it has its own internal validity and is relatively independent of the measurement device errors.
Although patients with difficult intubation have lower values for EMV, their relationship is not sufficiently strong to define a fitted model, which denotes relative independence of these two outcome measures from each other.
From the regression equation presented in this study, one may predict the lowest possible value for EMV as low as 10% or less, depending on the particular combination of patients factors. Combination of beard and chin receding in a male patients will account for about 30% reduction in EMV, compared to an otherwise matched female patients with normal mandible.
In some patients, EMV were higher than 100%. The exact cause of this phenomenon is unknown. One possible explanation may be the lower values for post-intubation minute volume (the denominator of EMV) in these patients, due to decreased dynamic compliance after intubation, as evidenced by higher peak inspiratory pressure.[16]
The minimum EMV for edentolous patients was about 60%. Contrary to previous report, lack of teeth is a beneficial factor for EMV, provided the lip-over-mask method is used.[11]
In this study, incidence of grade III mask ventilation was lower than previous studies and there was no case of grade IV mask ventilation,[3–6,9,17] which is due to lower sample size of the present study and also reflect the subjectivity of definitions for detecting difficult mask ventilation cases.[18]
To our best knowledge, no previous studies have used EMV or a similar measure. Therefore, the results of this study are not directly comparable to those which studied difficult mask ventilation.
It should be noted that all cases in this study have been managed by a third-year anesthesiology resident, and therefore, the results must be cautiously used for patients managed by more experienced anesthesiologists.
In conclusion, the results of this study have presented receded chin, presence of beard, male gender, high Mallampati classes, high neck-circumference, low inter-incisors gap, and old age as the main factors for estimating EMV in patients undergoing general anesthesia who received non-depolarizing muscle relaxant. In addition, the results of this study indicate that lack of denture facilitates mask ventilation by the lip-over-mask method. To predict EMV based on patients factors in edentolous patients, further studies with larger sample sizes are required.
Footnotes
Source of Support: Faculty of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran
Conflict of Interest: None declared.
REFERENCES
- 1.American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–77. doi: 10.1097/00000542-200305000-00032. [DOI] [PubMed] [Google Scholar]
- 2.Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW. Management of the Difficult Airway: A closed claims analysis. Anesthesiology. 2005;103:33–9. doi: 10.1097/00000542-200507000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Asai T, Koga k, Vaughan RS. Respiratory complications associated with tracheal intubation and extubation. Br J Anaesth. 1998;80:767–75. doi: 10.1093/bja/80.6.767. [DOI] [PubMed] [Google Scholar]
- 4.Kheterpal S, Han R, Tremper KK, Shanks A, Tait AR, O’Reilly M, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006;105:885–91. doi: 10.1097/00000542-200611000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–36. doi: 10.1097/00000542-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Yildiz TS, Solak M, Toker K. The incidence and risk factors of difficult mask ventilation. J Anaesth. 2005;19:7–11. doi: 10.1007/s00540-004-0275-z. [DOI] [PubMed] [Google Scholar]
- 7.Saghaei M, Safavi MR. Prediction of prolonged laryngoscopy. Anaesthesia. 2001;56:1198–201. doi: 10.1046/j.1365-2044.2001.02084-5.x. [DOI] [PubMed] [Google Scholar]
- 8.Khan ZH, Maleki A, Makarem J, Mohammadi M, Khan RH, Zandieh A. A comparison of the upper lip bite test with hyomental/thyrosternal distances and mandible length in predicting difficulty in intubation: A prospective study. Indian J Anaesth. 2011;55:43–6. doi: 10.4103/0019-5049.76603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rose DK, Cohen MM. The incidence of airway problems depends on the definition used. Can J Anaesth. 1996;43:30–4. doi: 10.1007/BF03015954. [DOI] [PubMed] [Google Scholar]
- 10.Cohen J. Hilsdale, New Jersey: Lawrence Erlbaum Associates; 1987. Statistical power analysis for the behavioral sciences (rev.ed) pp. 407–44. [Google Scholar]
- 11.Racine SX, Solis A, Hamou NA, Letoumelin P, Hepner DL, Beloucif S, et al. Face mask ventilation in edentulous patients: A comparison of mandibular groove and lower lip placement. Anesthesiology. 2010;112:1190–3. doi: 10.1097/ALN.0b013e3181d5dfea. [DOI] [PubMed] [Google Scholar]
- 12.Han R, Tremper KK, Kheterpal S, O’Reilly M. Grading scale for mask ventilation. Anesthesiology. 2004;101:267. doi: 10.1097/00000542-200407000-00059. [DOI] [PubMed] [Google Scholar]
- 13.Cohen J. 2nd ed. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1988. Statistical Power Analysis for the Behavioral Sciences; pp. 79–80. [Google Scholar]
- 14.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2011. [Last accessed on 2012 Jan 24]. ISBN 3-900051-07-0, URL Available from: http://www.R-project.org .
- 15.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–11. [PubMed] [Google Scholar]
- 16.Kil HK, Rooke GA, Ryan-Dykes MA, Bishop MJ. Effect of prophylactic bronchodilator treatment on lung resistance after tracheal intubation. Anesthesiology. 1994;81:43–8. doi: 10.1097/00000542-199407000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Kheterpal S, Martin L, Shanks AM, Tremper KK. Prediction and Outcomes of Impossible Mask Ventilation A Review of 50,000 Anesthetics. Anesthesiology. 2009;110:891–7. doi: 10.1097/ALN.0b013e31819b5b87. [DOI] [PubMed] [Google Scholar]
- 18.El-Orbany M, Woehlck HJ. Difficult Mask Ventilation. Anesth Analg. 2009;109:1870–80. doi: 10.1213/ANE.0b013e3181b5881c. [DOI] [PubMed] [Google Scholar]