Abstract
Background and Objectives:
Optic neuritis (ON) and nonarteritic anterior ischemic optic neuropathy (NAION) have some overlapping clinical profiles. We evaluated the usefulness of B-scan ultrasonography in distinguishing ON from NAION by measuring diameter of the optic nerve.
Materials and Methods:
Consecutive patients with an acute noncompressive unilateral optic neuropathy with relative afferent pupillary defect and onset of visual loss during the last 2 weeks were included. Diagnosis of ON was based on age ≤ 35 years, orbital pain associated with eye movement, and no disk edema, and diagnosis of NAION was based on age ≥ 60 years, no orbital pain associated with eye movement, and presence of disk edema. Age- and gender-matched subjects without ocular disease were selected for comparison. The diameter of the optic nerve was measured by a single radiologist with B-scan ultrasonography.
Results:
In ON patients, the mean diameter of the affected nerve was significantly larger than that of the unaffected nerve and also larger than that of the right nerve of young controls; P < 0.05. In NAION patients, however, there was no significant difference between the mean diameter of the affected nerve and of the unaffected nerve or the right nerve of elderly controls; P > 0.05. Also, the diameter of the affected nerve was significantly larger in ON than in AION patients; P < 0.05.
Conclusion:
B-scan ultrasonography is helpful in the early stages of optic neuropathy to distinguish ON from NAION in those cases for which the diagnosis is still uncertain after clinical evaluation.
Keywords: Anterior ischemic optic neuropathy, echography, optic neuritis, optic neuropathy, ultrasonography
INTRODUCTION
Optic neuritis (ON) and nonarteritic anterior ischemic optic neuropathy (NAION) are the two most prevalent optic neuropathies presented with acute visual loss. ON usually affects young adults between the ages of 20 and 45 years and has been reported to be associated with multiple sclerosis in up to 85% of the cases.[1] In contrast, NAION occurs generally in the sixth or seventh decades and is associated with systemic vascular diseases, chiefly hypertension and diabetes mellitus.[2]
Despite remarkable advances in neuroimaging and electrophysiologic techniques, the diagnosis of ON and NAION still depends on clinical presentations. Differentiation between ON and NAION has prognostic and therapeutic implications for clinicians. They can usually be differentiated clinically, based on several key features. Patients with ON are generally younger, usually experience pain on eye movement, and have progressive visual loss over several days. Conversely, patients with NAION are older, visual loss is usually painless and is most often maximal at onset.[3] During the acute stage, altitudinal or pallid disk edema, hemorrhage, and retinal arterial attenuation are more characteristic of NAION, whereas a normal-colored optic disk without hemorrhage is more characteristic of ON.[4] Also, certain visual field defects are characteristic of either ON (e.g., central scotoma) or NAION (e.g., altitudinal loss).[3,5] However, in occasional cases, there is an overlap of the presenting clinical features between these two entities that causes difficulties in distinguishing them, especially in the acute stage.[6,7] In these cases, imaging studies like computed tomography (CT) scan and magnetic resonance imaging (MRI) are helpful in differentiating various causes of optic neuropathy. According to Gerling et al. study, the diameter of the optic nerve, measured by B-scan ultrasonography, is enlarged in ON but not in NAION.[8] Considering ultrasonography as a readily accessible and inexpensive imaging method, we compared the diameter of the optic nerve among ON, NAION, and control subjects, using B-scan ultrasonography to evaluate if this method could be distinctive.
MATERIALS AND METHODS
This cross-sectional study was done in Neuro-Ophthalmology Clinic of Farabi Hospital, Tehran University of Medical Science (TUMS). Patients with an acute noncompressive unilateral optic neuropathy with a relative afferent pupillary defect and with onset of visual loss during the last 2 weeks were included. Diagnosis of ON and NAION was established primarily with clinical criteria during the acute stage by an experienced neuro-ophthalmologist. Diagnosis of ON was based on age ≤ 35 years, orbital pain associated with eye movements, and no disk edema, and diagnosis of NAION was based on age ≥ 60 years, no orbital pain associated with eye movements, and presence of disk edema. Paraclinical evaluations like MRI, visual evoked potential, and perimetry were also used for confirming the diagnosis. Cases with giant cell arteritis, borreliosis, and toxoplasmosis were excluded. Regarding the difference between ON and NAION patients in age, young, and elderly age- and gender-matched individuals without ocular disease were selected from persons accompanying with patients as the control group for comparison. Calculated sample size per group was 10, considering α = 0.05, study power = 80%, and effect size = 0.5 mm according to the previous reports.[8] The Human Studies Committee at the TUMS approved the ethical appropriateness of the study and informed consent was obtained from all participants before participation.
Ultrasonography
The diameter of the optic nerve was measured using B-scan ultrasonography (SIMENS ANTARES, 13 MHz) by a single radiologist who was not aware of the diagnosis or the side of the lesion. The probe was placed on the closed upper eyelid while the patient looked up temporally by 40--45°. The diameter of the optic nerve was measured immediately behind the globe. An electronic caliper was used to measure the horizontal diameter of the optic nerve. Three measurements, with readjustment of the probe after each measurement, were done for each eye and the mean value was considered as the final measure.
Statistics
Considering the normal distribution of the data, the paired samples test was used for comparison of parametric data between the two groups. For comparison between the four groups, the one-factor ANOVA and Benferroni test were used. Data were analyzed using SPSS software for Windows (Version 16).
RESULTS
As presented in Table 1, in ON patients, the mean diameter of the affected nerve was significantly larger than that of the unaffected nerve; P = 0.017. In NAION patients, however, there was no significant difference between the mean diameter of the affected nerve and that of the unaffected nerve; P = 0.785.
Table 1.
Diameter of the optic nerve (mm) in ON, NAION, and controls
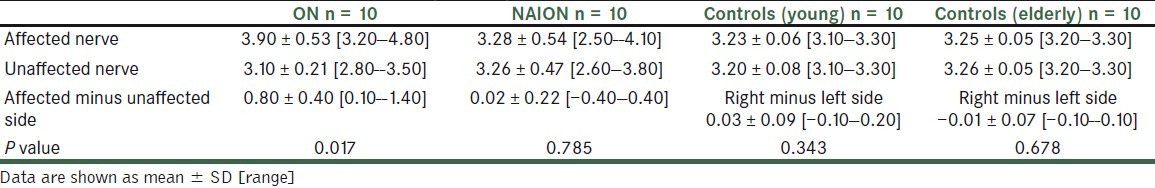
There was no significant difference between the right and left nerves in young or elderly controls; P = 0.343 and 0.678, respectively. Also, the mean diameter of the right and left nerves were the same in young and elderly controls; P = 0.47. But comparison of ON and NAION nerves with the corresponding nerve of the controls showed that in ON, the diameter of the affected nerve was significantly larger than that of the young controls; P = 0.002. However, in NAION, the diameter of the affected nerve did not differ from that of the elderly controls; P = 1.0 [Figure 1].
Figure 1.
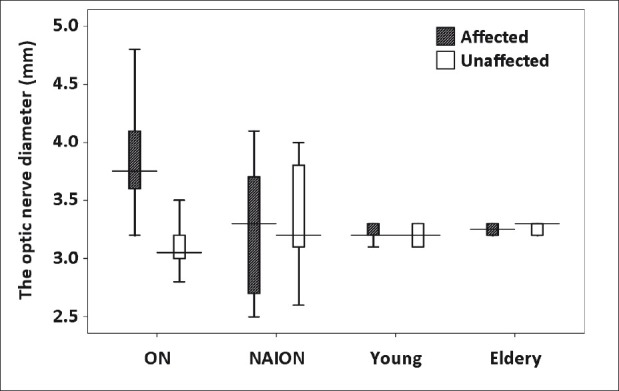
Comparison of the diameter of the affected and unaffected nerves among the study groups
Comparison between ON and NAION showed that the diameter of the affected nerve was significantly larger in ON than in NAION; P = 0.006. But, there was no significant difference between ON and NAION in the diameter of the unaffected nerve; P = 1.0. Also, the difference between affected and unaffected nerves was significantly larger in ON than that in NAION; P < 0.001 [Figure 1].
DISCUSSION
The initial clinical features of ON may resemble those of NAION with regard to age of onset, pattern of visual field loss, and optic disk appearance.[6,7] It is reported that up to 23% of patients with NAION are younger than 50[9,10] and up to 12% do experience ocular pain or headache.[11,12] Also, some studies reported a considerable overlap of the visual field defects between ON and NAION and the value of diagnosis on the basis of visual field defects is limited to cases with pathognomonic defects.[5,13] Therefore, in certain cases, other tests are needed to differentiate between ON and NAION.
The results of the present study showed that in ON patients the diameter of the affected optic nerve (measured by B-scan ultrasonography) is significantly larger than that of the unaffected nerve and also larger than normal. This finding is not present in patients with NAION. The results of the study by Gerling et al.[8] also showed that in ON patients (especially those with disk swelling), the diameter of the affected nerve is much larger than in NAION. Therefore, in addition to clinical features, the diameter of the optic nerve measured by B-scan ultrasonography can be used as a criterion to differentiate between ON and NAION. Other studies in which ultrasonography, CT scan, and MRI have been used separately in patients with ON or NAION showed the same results.[14–18]
In the study by Gerling et al.,[8] the diameter of the affected optic nerve in ON patients with and without disk swelling were 5.4 mm and 4.4 mm, respectively, which was significantly larger than what we found in our study (3.9 mm). This difference, however, is not observed in the diameter of the unaffected nerve or controls and therefore it seems not to be due to technical errors and/or equipment. As Figure 1 shows, there was an overlap of the diameter of the affected optic nerve between the ON and AION patients in our study, which was not present in the study by Gerling et al. Since significant variation in the measured diameter of the optic nerve can occur in the general population, it is better to compare the diameters in both eyes and not to calculate deviation from a normal value.[19] In our study, the difference between affected and unaffected sides was more than 0.5 mm in 80% (8/10) of ON patients and less than 0.5 mm in all NAION patients. In Gerling et al.'s study, this difference was more than 0.5 mm in all ON patients and less than 0.5 mm in all NAION patients. According to these results as well as other reports,[19] a difference of 0.5 mm between the eyes could be indicative of an abnormal thickness in one eye and distinguish ON from NAION. However, further investigation is needed to define a more accurate value.
In recent years, the use of ultrasonography in the diagnosis of orbital diseases has been overthrown by other imaging modalities like CT and MRI. In fact, ultrasonography is less useful in demonstrating inflammatory changes of the orbital portion of the optic nerve, which is better shown on MRI after injection of enhancing agents. Studies have shown that MRI scanning of the optic nerve demonstrates significantly different results in patients clinically diagnosed as either ON or NAION.[20] Although ultrasonography is a noninvasive and inexpensive form of imaging, its usefulness in both A and B modes is limited to the anterior portion of the orbit. It is of the greatest value in the hands of the clinician-ultrasonographer capable of interpreting real-time images.[21] However, the results of the present study along with the previous ones[8] showed that ultrasonography as a readily accessible, noninvasive, and inexpensive imaging method can assist in the early distinction between ON and NAION. It could be helpful in situations in which other imaging methods (MRI and CT) are not readily accessible and rapid diagnosis is needed for treatment.
CONCLUSION
B-scan ultrasonography can be used early in the course of optic neuropathy to distinguish ON from NAION in those cases for which the diagnosis is still uncertain after clinical examination. Further studies are needed to evaluate the efficacy of B-scan ultrasonography in distinguishing ON from NAION when there are important overlapping profiles, like in patients with NAION who are young or have pain with eye movements and in patients with ON who are elderly or do not have pain with eye movements. Comparison between B-scan ultrasonography and other imaging modalities in distinguishing ON from NAION also warrants further investigations.
ACKNOWLEDGMENTS
Our greatest thanks go to patients who participated in this study. This study was financially supported by Tehran University of Medical Sciences. We are also thankful to Isfahan Eye Research Center for scientific support and Ali Gholamrezaei (MD, Isfahan University of Medical Sciences) who helped us preparing this report.
Footnotes
Source of Support: Tehran University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Smith CH. Optic neuritis. In: Miller NR, Newman NJ, Biousse V, et al., editors. Walsh and Hoyt's Clinical Neuro-Ophthalmology. Philadelphia: Lippincott Williams and Wilkins; 2004. pp. 294–347. [Google Scholar]
- 2.Arnold AC. Ischemic Optic Neuropathy. In: Miller N R, Newman NJ, Biousse V, editors. Walsh and Hoyt's Clinical Neuro-Ophthalmology. Philadelphia: Lippincott Williams and Wilkins; 2004. pp. 350–83. [Google Scholar]
- 3.Purvin V, Kawasaki A. Neuro-ophthalmic emergencies for the neurologist. Neurologist. 2005;11:195–233. doi: 10.1097/01.nrl.0000159981.73413.2e. [DOI] [PubMed] [Google Scholar]
- 4.Warner JE, Lessell S, Rizzo JF, 3rd, Newman NJ. Does optic disc appearance distinguish ischemic optic neuropathy from optic neuritis? Arch Ophthalmol. 1997;115:1408–10. doi: 10.1001/archopht.1997.01100160578009. [DOI] [PubMed] [Google Scholar]
- 5.Gerling J, Meyer JH, Kommerell G. Visual field defects in optic neuritis and anterior ischemic optic neuropathy: Distinctive features. Graefes Arch Clin Exp Ophthalmol. 1998;236:188–92. doi: 10.1007/s004170050062. [DOI] [PubMed] [Google Scholar]
- 6.Rizzo JF, 3rd, Lessell S. Optic neuritis and ischemic optic neuropathy.Overlapping clinical profiles. Arch Ophthalmol. 1991;109:1668–72. doi: 10.1001/archopht.1991.01080120052024. [DOI] [PubMed] [Google Scholar]
- 7.Optic Neuritis Study Group. The clinical profile of optic neuritis.Experience of the Optic Neuritis Treatment Trial. Arch Ophthalmol. 1991;109:1673–8. doi: 10.1001/archopht.1991.01080120057025. [DOI] [PubMed] [Google Scholar]
- 8.Gerling J, Janknecht P, Hansen LL, Kommerell G. Diameter of the optic nerve in idiopathic optic neuritis and in anterior ischemic optic neuropathy. Int Ophthalmol. 1997;21:131–5. doi: 10.1023/a:1026422819404. [DOI] [PubMed] [Google Scholar]
- 9.Preechawat P, Bruce BB, Newman NJ, Biousse V. Anterior ischemic optic neuropathy in patients younger than 50 years. Am J Ophthalmol. 2007;144:953–60. doi: 10.1016/j.ajo.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 10.Hayreh SS, Joos KM, Podhajsky PA, Long CR. Systemic diseases associated with nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol. 1994;118:766–80. doi: 10.1016/s0002-9394(14)72557-7. [DOI] [PubMed] [Google Scholar]
- 11.Ischemic Optic Neuropathy Decompression Trial Study Group. Characteristics of patients with nonarteritic anterior ischemic optic neuropathy eligible for the Ischemic Optic Neuropathy Decompression Trial. Arch Ophthalmol. 1996;114:1366–74. doi: 10.1001/archopht.1996.01100140566007. [DOI] [PubMed] [Google Scholar]
- 12.Swartz NG, Beck RW, Savino PJ, Sergott RC, Bosley TM, Lam BL, et al. Pain in anterior ischemic optic neuropathy. J Neuroophthalmol. 1995;15:9–10. doi: 10.3109/01658109509044588. [DOI] [PubMed] [Google Scholar]
- 13.Keltner JL, Johnson CA, Spurr JO, Beck RW. Baseline visual field profile of optic neuritis.The experience of the optic neuritis treatment trial. Optic Neuritis Study Group. Arch Ophthalmol. 1993;111:231–4. doi: 10.1001/archopht.1993.01090020085029. [DOI] [PubMed] [Google Scholar]
- 14.Gass A, Moseley IF, Barker GJ, Jones S, MacManus D, McDonald WI, et al. Lesion discrimination in optic neuritis using high resolution fatsuppressed fast spin echo MRI. Neuroradiology. 1996;38:317–21. doi: 10.1007/BF00596577. [DOI] [PubMed] [Google Scholar]
- 15.Dees C, Buimer R, Dick AD, Atta HR. Ultrasonographic investigation of optic neuritis. Eye. 1995;9:488–94. doi: 10.1038/eye.1995.113. [DOI] [PubMed] [Google Scholar]
- 16.Miller DH, Newton MR, van der Poel IC, du Boulay EP, Halliday AM, Kendall BE, et al. Magnetic resonance imaging of the optic nerve in optic neuritis. Neurology. 1988;38:175–9. doi: 10.1212/wnl.38.2.175. [DOI] [PubMed] [Google Scholar]
- 17.Gans MS, Byrne SF, Glaser JS. Standardized A-Scan echography in optic nerve disease. Arch Ophthalmol. 1987;105:1232–6. doi: 10.1001/archopht.1987.01060090090035. [DOI] [PubMed] [Google Scholar]
- 18.Howard CW, Osher RH, Tomsak RL. Computed tomography features in optic neuritis. Am J Ophthalmol. 1980;89:699–702. doi: 10.1016/0002-9394(80)90290-1. [DOI] [PubMed] [Google Scholar]
- 19.Lystad LD, Hayden BC, Singh AD. Optic nerve disorders. Ultrasound Clin. 2008;3:257–66. [Google Scholar]
- 20.Rizzo JF, 3rd, Andreoli CM, Rabinov JD. Use of magnetic resonance imaging to differentiate optic neuritis and nonarteritic anterior ischemic optic neuropathy. Ophthalmology. 2002;109:1679–84. doi: 10.1016/s0161-6420(02)01148-x. [DOI] [PubMed] [Google Scholar]
- 21.Hayden BC, Kelley L, Singh AD. Ophthalmic ultrasonography: Theoretic and practical considerations. Ultrasound Clin. 2008;3:179–83. [Google Scholar]


