Abstract
Background:
Umbilical cord blood analysis may give a clue to the state of health of both pregnant mothers and their neonates. However, there is paucity of literature on some of these indices from our area.
Objectives:
This present study determined the red blood indices of maternal and umbilical cord blood in Owerri, Nigeria.
Methods:
Pregnant mothers aged 18 - 42 years who booked and received antenatal care until vaginal delivery at the antenatal clinics of two tertiary health care centres in Owerri, Nigeria were divided into five age groups I – V. Maternal blood samples were obtained immediately after delivery of the baby. The umbilical blood samples were collected from the umbilical cord of the baby at the end of the second stage of labour. The haemoglobin (Hb) concentration and packed cell volume (PCV) were determined using standard procedures. The mean corpuscular haemoglobin concentration (MCHC) was calculated mathematically.
Results:
The result of the cord blood haemoglobin concentration and packed cell volume were significantly higher than the maternal values (14.22 ± 1.25 g/dl versus 11.20 ± 0.92g/d and 42.6 9± 3.80% versus 33.67 ± 2.71% respectively; (P < 0.0001).However, there was no significant differences between cord blood and maternal mean corpuscular haemoglobin concentration (33.24 ±0.23% versus 33.29 ± 0.45 % ;P = 0.310). Furthermore, a positive linear Pearson's correlation was observed between the mean Hb and PCV of cord blood and maternal blood (r=1.11 and r=1.15 respectively <0.0001).
Conclusion:
This result provides a baseline data for further studies on establishing a reference value for maternal and umbilical cord packed cell volume and haemoglobin concentration in our locality.
Keywords: Umbilical cord blood, maternal blood, haemoglobin concentration, packed cell volume, red cell indices
Introduction
Hopper and Seyler in 1864 first used the term haemoglobin (Hb) to describe the red pigments found inside the red blood cells (RBC), and a lot of studies have been carried out on its significance.1 It has been well documented that certain differences exist between haemoglobin types and packed cell volume of the newborn babies and adults, and this was attributed to the embryonic development and extra uterine life adaptation.2 Previous studies have reported on the variation of haematological indices between Negroes (Africans) and Caucasians.3–7 The suggested reasons for the racial variations included genetic factors,8 dietary factors,9–11 infections, parasites and gravidity.10 The concentration of foetal haemoglobin (Hb-F) in the umbilical cord blood for full term infants were shown to vary from 77% to 90% due to the persistence of erythrocytes in the circulation for a period of four mouths notwithstanding the switch-off in the polypeptide chain production.12 Published reports of haemorheological values of umbilical cord blood in Nigerian newborns are relatively scanty.13 The red blood cell count of full term newborns was shown to be very high compared to adult values,8 with Hb levels ranging from 11.2 to 26.6g/100ml, with 95% of the values between 13.7 to 20.2g/100ml.14,15 A previous study in Americans reported a cord blood haemoglobin concentration range of 16.6–17.9g/100ml.12
In Nigeria, various studies from other different locations have reported different values for Jos, North Central; an umbilical cord Hb concentration of 12.3g/100ml was obtained in 2003,16 while an earlier study in 1990 reported a cord Hb concentration of 17.1g/100ml.6 In Port Harcourt, South South Nigeria, it was 13.7g/100ml13,17 and in Benin City in the same geographical location, it was 15.4g/100ml.18 The mean umbilical cord blood PCV reported for Port Harcourt was 41.28 +/- 6.57 % while the PCV for neonates in Northern Nigeria was 42%.19
Another study conducted on 600 apparently healthy neonates indicated that the PCV was highest at 24hours after birth.20 It has been stressed that each population must establish normal reference values for use in clinical assessment.21 There is paucity of literature on these indices in cord and maternal blood for this locality. Consequently, the present study was designed to determine basic haematological indices in the umbilical cord blood of Nigerian neonates and in the venous blood of their respective mothers in Owerri. Furthermore, it also aimed to determine if there are any significant differences or correlations in these haematological indices between maternal and umbilical cord blood.
Subjects and Methods
Subjects
A total of two hundred (200) apparently healthy pregnant women at term, aged 18–42 years resident within Owerri municipality who were booked, received antenatal care at the ante natal clinics of the Federal Medical Centre, Owerri and General Hospital Owerri, Nigeria until vaginal delivery and who delivered within the eighteen (18) months period of this study were randomly selected by using a lucky dip of yes or no. Subjects who showed any sign of anaemia from the routine laboratory tests including positive malaria parasitaemia, or had premature delivery, history of haemorheological, cardiovascular, endocrine, metabolic or neurological diseases were excluded from this study.
All our subjects were screened for HIV at the first booking for antenatal clinic and repeated at mid-third trimester respectively22 and only those who tested negative on the two occasions were included. They all belonged to the same socioeconomic class. Ethical clearance was obtained from the ethical committees of the two hospitals and ‘informed’ verbal consent was obtained from the subjects before blood sample collection. The subjects were divided into five age group ranges designated I – V to determine effects of age and parity on the red cell indices.
Sample Collection
Blood samples were collected from the umbilical cord of the babies at the end of the second stage of labour (immediately after delivery) by clamping and cutting the babies’ end of the cord. The blood samples were also collected from the antecubital fossa of the mothers by venepuncture inside the labour room immediately after delivery of the babies. These collections were done under high aseptic conditions. Blood samples were collected into sample bottles containing EDTA anticoagulant adequate for 2mls of blood. The samples were analysed within two hours of collection.
Laboratory Investigations
Haemoglobin Estimation
The cyanmethaemoglobin method as described by Dacie and Lewis (1993)23 was employed using the Dabkin‟s solution and the absorbance of the supernatant colour was measured at 540nm in a spectrophotometer (Spectron 20+, Bush and Lomb, England). The Hb concentration was estimated from a standard normogram.
Determination of Packed Cell volume
The packed cell volume was measured using the microhaematocrit capillary tube-centrifuge-reader method.23 Samples were collected into capillary tubes by capillary action, sealed off at one end with plasticine, placed inside the microhaematocrit centrifuge for spinning for five minutes at 1500 revolutions per minute. The spun sample was read off to determine the packed cell volume in percentages.
Estimation of Mean Corpuscular Haemoglobin Concentration (MCHC)
The MCHC was determined from the values of haemoglobin concentrations and the packed cell volumes using standard formula.23
Statistical and Data Analysis
The results are presented as mean ± SD and SEM. The data was statistically analysed by using the software, EPI – INFO version 6. The means were compared using the One-way Analysis of Variance (ANOVA) and the student t-test where appropriate. A Pearson's correlation was obtained between the mean Hb and PCV of cord blood and maternal blood. The probability value (P -value) of less than 0.05 was considered statistically significant
Results
A total of 200 maternal and umbilical cord blood samples were analysed. Table 1 shows the age distribution range, range frequency and mean age values of the women. The ages of the mothers ranged from 18 – 42 years with a mean value of 30.18 ± 1.39 years. The age range with the highest frequency was 23 - 27 years.
Table 1.
Age distribution, Ranges and Frequency of the Mothers
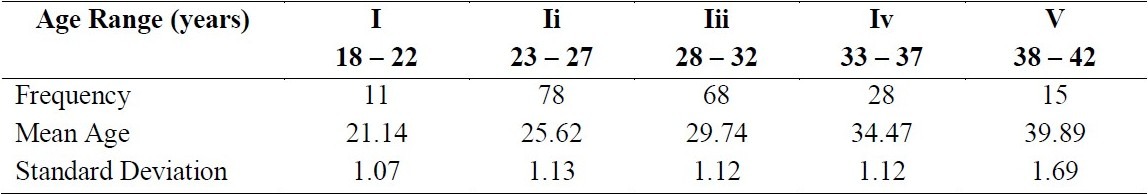
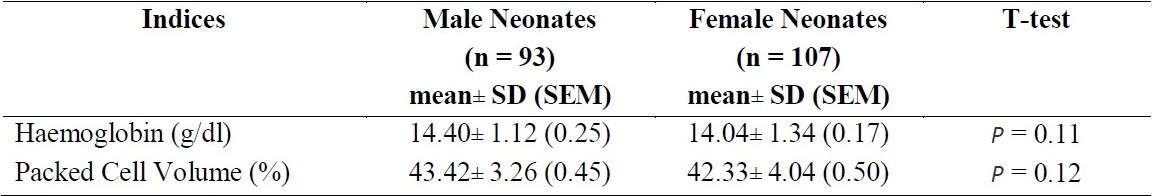
Table 2 shows certain red cell indices of the maternal and cord blood. This indicates a significant difference between the haemoglobin concentration and packed cell volume (P < 0.0001) while the MCHC (P = 0.31) was not significant. Table 3 shows the age distribution of the delivered mothers and their PCV, and haemoglobin concentration. The mean Hb concentration was 11.20g/dl ± 0.92 and mean PCV was 33.67% ± 2.71. No significant difference was observed between the age ranges and the indices (P = 0.24 and 0.28 respectively). Table 4 shows the red cell indices among the sexes of the neonates. No significant difference was observed (P = 0.11 and 0.12 respectively). A positive linear Pearson‟s correlation was obtained between the mean Hb concentration of cord blood and maternal blood (r = 1.11) on one hand and between PCV of cord blood and maternal blood (r = 1.15). P <0.0001.
Table 2.
Certain Red Cell Indices of Maternal and Umbilical Cord Blood
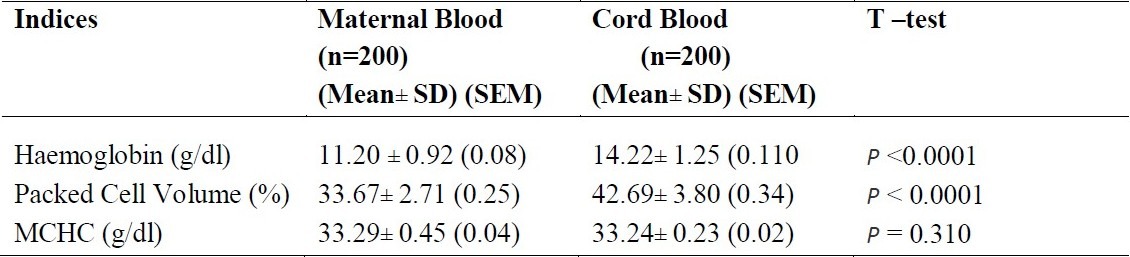
Table 3.
Certain Red Cell Indices of Maternal Blood According to Age Distribution
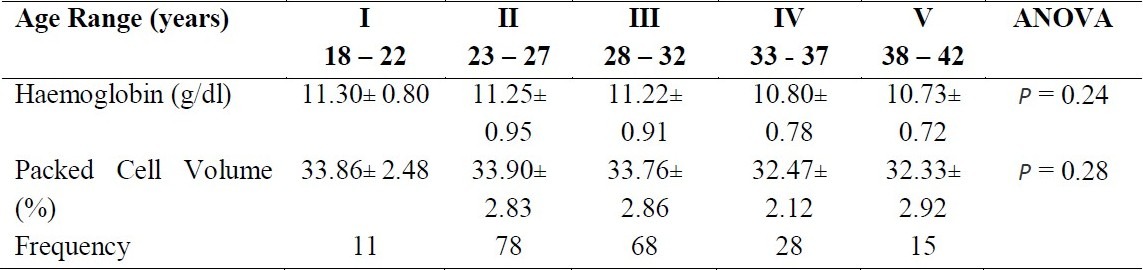
Table 4.
Certain Red Cell Indices of Umbilical Cord Blood According to Sex
Discussion
Previous studies by various workers on haematological data of maternal and umbilical cord blood have been reported for several locations in Nigeria.5,13,16,17,18,19 This present study carried out in Owerri obtained a higher value for cord blood Hb (14.22g/dl) when compared with others (11.2g/dl),12 (12.3g/dl),16 (13.29g/dl)17 and (10.8 – 12.6g/dl).11 However, certain workers recorded higher values for Hb than was obtained herein (15.46g/dl),18 (15.2 – 19.0g/dl)6 and (16.6 – 17.9g/dl).15 The mean PCV(33.67%) of umbilical cord blood was higher than in one previous study,12 but lower than other reports for Northern Nigeria (42%),19 Jos (45%),6 Benin (45%)18 and Ibadan (60%).24
Though, some of these previous reports were not specific for cord blood but included neonates irrespective of age. The suggested reasons for the differences observed in the previous studies in various locations were environmental and dietary factors.8,9,25 Others include time of clamping of the umbilical cord before blood samples were collected7,26,27 and the different methods of delivery employed.7,28 This present study utilised the vaginal delivery of full term pregnancy and clamping of the cord at the end of second stage of labour. This is known to have no adverse effect on the studied indices26,27,29 hence the decreased PCV and Hb attributed to caesarean delivery25 and late clamping29 could not have been the case in this study. Furthermore, nutrition30 could not have influenced our study as the mothers were maintained on routine prophylactic iron and folic acid. This study showed that both the Hb and PCV of the cord blood were significantly higher than the maternal blood samples hence corroborates an earlier study8.
A positive linear correlation was obtained for the Hb and PCV of cord and maternal blood which agreed with previous reports in other environments.5,6,13,30 This explains a dependence of foetal Hb level on certain maternal factors such as ferritin5 and hepcidin levels.31 Understandably, the relatively lower values of Hb and PCV observed in the maternal blood than in cord blood may be due to plasma volume expansion leading to haemodilution in pregnancy.32,33 Indeed, key physiological changes in pregnancy, which modifies the chemical constitution of blood, amplifies transfer of some haematopoietic micronutrients, and increased utilisation of some of these micronutrients as defence mechanisms against pregnancy induced oxidative stress may lead to maternal depletion and low haematological values.
In this study, maternal age had no significant effect on the blood indices and this agrees with a similar observation in Karachi, Pakistan.25 Also, no sex difference was observed among the cord blood and thus collaborate an earlier American survey.7,26.
The results of this present study substantiate the existence of variations in the red cell indices of umbilical cord blood reported for different locations in Nigeria. This provides a baseline data for further studies on establishing a reference value for umbilical cord PCV and Hb concentration in pregnant women in our locality. This is of clinical importance considering the new concept of umbilical cord blood banking; which serves as a reservoir for harvesting stems cells needed for stem cell transplant. However, the study is limited by the fact that the deliveries occurred at different times of the day, mainly in the night and one could not always be present to collect the samples except when the researchers are around. Also, some mothers would not consent to the collection of their blood samples from the cord of their new born babies because of their beliefs. Further studies to include a complete full blood count and to determine the effect of maternal anaemia on these umbilical cord parameters are advocated.
Acknowledgments
We wish to thank the Management of the Federal Medical Centre and General Hospital Owerri. Our gratitude goes to the Chief Nursing Officer in-charge of the Maternity ward at Federal Medical Centre, Mrs. Irene O. Nwoko, and that of General Hospital, Mrs. Obrieze and their nurses for their assistance.35
References
- 1.Hoffbrand AV, Petit JE, Moss PAH. Essential Hematology. 4 edn. England: Blackwell Science; 2001. Hemoglobin; pp. 12–27. [Google Scholar]
- 2.Elias S, Francis M. Hematology of the Newborn. In: Williams H, et al., editors. Hematology. England: McGraw Hill book Company; 1983. pp. 37–43. [Google Scholar]
- 3.Harrison KA. Blood Volume of Nigerian women. West Afri Med J. 1966;46:680–685. [PubMed] [Google Scholar]
- 4.Ezeilo GC. A Comparison of the hematological values of cord blood of African, European and Asian neonates. Afri J Med. 1978;7:163–169. [PubMed] [Google Scholar]
- 5.Onwukeme KE, Uguru VE. Hematological values in pregnancy in Jos. West Afri J Med. 1990;9:770–775. [PubMed] [Google Scholar]
- 6.Onwukeme KE, Olomu IN, Nnanna OU. Hematological indices of healthy Nigerian neonates. Nig Med Pract. 1993;23:9–12. [Google Scholar]
- 7.Alur P, Devapatia SS, Super DM, Danish ED, Stern T, Inagandla R, et al. Impact of Race and Gestational age on Red Blood Cell Indices in Very Low Birth Weight Infants. Pediatr. 2000;106(2):306–310. doi: 10.1542/peds.106.2.306. [DOI] [PubMed] [Google Scholar]
- 8.Ezeilo GC. Hematological Values in pregnant Zambian women. Trop Geogr Med J. 1972;24:252–258. [PubMed] [Google Scholar]
- 9.Ezeilo GC. Neutropenia in Africans. Trop Geogr Med. 1971;23:264–267. [PubMed] [Google Scholar]
- 10.Ezeilo GC. The Etiology of neutropenia in Healthy Africans. East Afr Med J. 51:936–941. [PubMed] [Google Scholar]
- 11.Ogunranti JO. Non-genetic leuco-neutropenia is related to dietary cholesterol, an experimental model with rat. Acta Haematol. 1994;92:61–65. doi: 10.1159/000204176. [DOI] [PubMed] [Google Scholar]
- 12.Andrews EF, Willet GP. Fetal Hemoglobin and Packed Cell Volume Concentration in the Newborn. Am J Obstet Gynecol. 1965;16:58–88. [PubMed] [Google Scholar]
- 13.Dapper DV, Didia BC. Haemorheological parameters of umbilical cord blood of Nigerian newborns: Correlations with maternal parameters. W Afr J Med. 2006;25(1):226–230. doi: 10.4314/wajm.v25i3.28283. [DOI] [PubMed] [Google Scholar]
- 14.Oski FA, Naiman JC. Hematological problems in Newborn. 3 edn. Philadelphia: WB Saunders Company; 1972. Hematology; pp. 12–13. [Google Scholar]
- 15.Jeliffe DB, Stanfield JP. Diseases of children in the sub - tropics and Tropics. 3 edn. England: ELBS and Edward Arnold Ltd; 1981. Umbilical cord blood; pp. 573–84. [Google Scholar]
- 16.Odey SO, Ibu JO. Levels of Hemoglobin concentration and Packed Cell Volume in umbilical cord blood in Jos, Nigeria. Nig J Physiol Scis. 2003;18(1-2):1–3. [Google Scholar]
- 17.George I, Korma L, Dapper DV. Haemorheological parameters of maternal and umbilical cord blood in Port Harcourt, Nigeria. Nig J Physiol Scis. 2004;19(1-2):114–115. [Google Scholar]
- 18.Scott Emuakpor AB, Okolo AA, Omene JA, Ukpe SI. Normal hematological values of the African Neonate. Blut. 1985;51(1):11–18. doi: 10.1007/BF00320595. [DOI] [PubMed] [Google Scholar]
- 19.Abdurrahman MB, Adekoje MA. Hematological values in Northern Nigerian neonates. Trans R Soc Trop Med Hyg. 1983;77(6):786–788. doi: 10.1016/0035-9203(83)90289-4. [DOI] [PubMed] [Google Scholar]
- 20.Virginia DB, Lula OL. Neonatal polycythemia and hyperviscosity. Paed Clin Amer. 1982:1137–1148. doi: 10.1016/s0031-3955(16)34251-1. [DOI] [PubMed] [Google Scholar]
- 21.El-Hazmi WAF, Warsy AS. Normal Reference values for Hematological Parameters, Red cell indices, HBA2 and HB-F from early childhood through adolescence in Saudis. Ann Saudi Med. 2001;21(3-4):165–169. doi: 10.5144/0256-4947.2001.165. [DOI] [PubMed] [Google Scholar]
- 22.Nneli RO. Retrospective and Prospective Studies on the epidemiology of HIV/AIDS in pregnancy and children in Enugu, South Eastern Nigeria. PhD Thesis. Uturu, Nigeria: Abia State University; 2003. [Google Scholar]
- 23.Dacie JV, Lewis SM. Practical Hematology. 3 edn. London: Churchill – Livingstone Medical Division of Pearson Professional Ltd; 1993. Hemoglobin Estimation; pp. 227–228. [Google Scholar]
- 24.Effiong CE, Taiwo O, Odeniyi OO, Mellitus ED. Hematological values in healthy full term Nigerian newborn infants. Bio Neonate. 1976;28:336–346. [Google Scholar]
- 25.Qaiser DH, Sandila MP, Kazmi T, Ahmed ST. Influence of maternal factors on hematological parameters of healthy newborns of Karachi. Pak J Physiol. 2009;5(2):34–37. [Google Scholar]
- 26.Shohat M, Merlob P, Reisner SH. Neonatal polycythemia. Early diagnosis and influence relating to time of sampling. Pediatric. 1984;73(7):7–10. [PubMed] [Google Scholar]
- 27.Ramamurthy RS, Berlinga M. Postnatal alteration in haematocrit and viscosity in normal and polycythaemic infants. J Pediatric. 1987;11:929–934. doi: 10.1016/s0022-3476(87)80417-1. [DOI] [PubMed] [Google Scholar]
- 28.Gairdner D, Marks J, Roscoe JD, Brettel RO. The fluid shift from the vascular compartments immediately after. Arch Dis Child. 1958;33:489–498. doi: 10.1136/adc.33.172.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abalos E. The WHO Reproductive Health Library. Geneva: World Health Organization; Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes: RHL Commentary 29 March 2009. http://apps.who.int/rhl/pregnancy_childbirth/childbirth/3rd_stage/cd004074_abalose_com/12/7/2010 . [Google Scholar]
- 30.Vobecky JS, Vobecky J, Shapcott D, Demers PP, Cloutier D, Blanchard R, et al. Biochemical indices of nutritional status in maternal, cord, and early neonatal blood. Am J Clin Nutr. 36:630–632. doi: 10.1093/ajcn/36.4.630. [DOI] [PubMed] [Google Scholar]
- 31.Rehu M, Punnonen K, Ostland V, Heinonen S, Westerman M, Pulkki K, et al. Maternal serum hepcidin is low at term and independent of cord blood iron status. Eur J Haematol. 2010;85(4):345–352. doi: 10.1111/j.1600-0609.2010.01479.x. [DOI] [PubMed] [Google Scholar]
- 32.Abudula OO, Sofola OA. Relationship between Red cell mass and packed cell volume in Nigerian Primigavidae. Nig J Physiol Scis. 1994;10(1-2):13–21. [Google Scholar]
- 33.Bahi N, Tuan N, Ali K. Maternal Physiology. In: Hacker NF, Muore JG, editors. Essentials of Obstetrics and Gynecology. Philadelphia: WB Saunders Company; 1992. pp. 85–86. [Google Scholar]
- 34.Dejmek J, Ginter E, Solansky I, Podrazilova K, Benes I, Sram RJ. Vitamin C, E, and A levels in Maternal and fetal blood for Czech and Gypsy ethnic group in the Czech Republic. Int J vitam Res. 2002;72(3):183–190. doi: 10.1024/0300-9831.72.3.183. [DOI] [PubMed] [Google Scholar]
- 35.Pressman EK, Cavanangh JL, Mingione M, Norkus EP, Woods JR. Effects of maternal antioxidants supplementation on Maternal and fetal antioxidant levels: a randomized double blind study. Am J Obstet Gynecol. 2003;189(6):1720–1725. doi: 10.1016/s0002-9378(03)00858-5. [DOI] [PubMed] [Google Scholar]


