Abstract
Background:
Menopause alters the physiological, biochemical and psychological environment of a woman. Thus the knowledge and perception of its symptomatology is invaluable to enable appropriate adjustment to this natural phenomenon.
Objective:
The objective of this study was to determine the knowledge and perception of menopause and climacteric symptoms among a sample of women in Enugu, South East Nigeria.
Methods:
This was a cross sectional survey of 432 women aged 45-60 and above drawn from the general population of Enugu metropolis of Nigeria. These women were randomly selected from the gynaecology clinic attendees in a tertiary health care facility in Enugu. A self administered structured pre-tested questionnaire was designed. The data were analysed using SPSS software. The primary methods used were cross tabulation (with X2 or Mantel Haenszel trend tests as appropriate) and one way analysis of variance.
Results:
Majority of women in the population studied experienced climacteric symptoms but relatively few regarded these symptoms as a problem. For example hot flushes and night sweats were experienced by 70.0% but defined as a problem by only 30.0%. Out of 432 women studied, only 33.3% sought medical attention in hospital for their symptoms. 58.3% of the women did not regard them as a medical problem and took them as part of aging process.
Conclusion:
Physicians should be aware of climacteric symptoms among women in the population so as to offer appropriate counselling and support without undue recourse to wasteful clinical assessment and investigations. Public enlightenment would also help to improve awareness of the menopause and its symptoms that may often lead to misdiagnosis in gynaecological clinics.
Keywords: Knowledge, perception, women, menopause, climacteric, Enugu-Nigeria
Introduction
Menopause usually signifies the end of a woman's reproductive life. The mean age of menopause throughout the world today is 50 years.1 Menopause is a physiological process. A twelve month period of amenorrhoea confirms that menopause has set in. It is therefore a retrospective diagnosis.2 It is an oestrogenic deficiency period associated with a wide variety of physical and psychological symptoms including hot flushes, night sweat, dyspareunia, urinary frequency, sleep disturbance, tiredness, depression, anxiety, concentration difficulties and inability to cope.1,3–4 These symptoms may not be widely experienced by every woman or confined to a minority of women.
A lot of studies based on symptomatology have been criticised on methodological grounds, such as relying on selected populations like those who attend clinics or using unquantifiable measures of symptoms.6 Large scale studies on Nigerian women drawn from the general population are unavailable.6 Menopause and the postmenopausal period are very important landmarks in a woman's life since she will spend more than a third of her life during these periods without significant endogenous oestrogen production.7,8
This paper describes findings from a randomly selected population of women drawn from Enugu metropolis aged between 45-60 years and above. The aim of the survey is to determine the knowledge and perception of menopause and climacteric symptoms by women in this age group who reside in Enugu, South East Nigeria.
Methods
A sample of 432 women aged 45-60 and above living in Enugu metropolis of Nigeria was randomly selected (simple lucky dip of YES or NO) from UNTH gynaecology clinic attendees. Self administered pre-tested questionnaire was designed to cover background details, menstrual history, climacteric symptoms and the general health of the women.
In the analysis, symptoms were divided into ‘classic’ (e.g. hot flushes, night sweats, sleep disturbance and vaginal problems), ‘somatic’ (e.g. aches and pains, headaches, sore breasts, nocturia, palpitations and dizziness and ‘psychological’ (e.g. irritability, concentration/memory problems, anxiety, depression and feeling unable to cope).
The data were analysed using SPSS version12. Data was presented as simple descriptive statistics.
Results
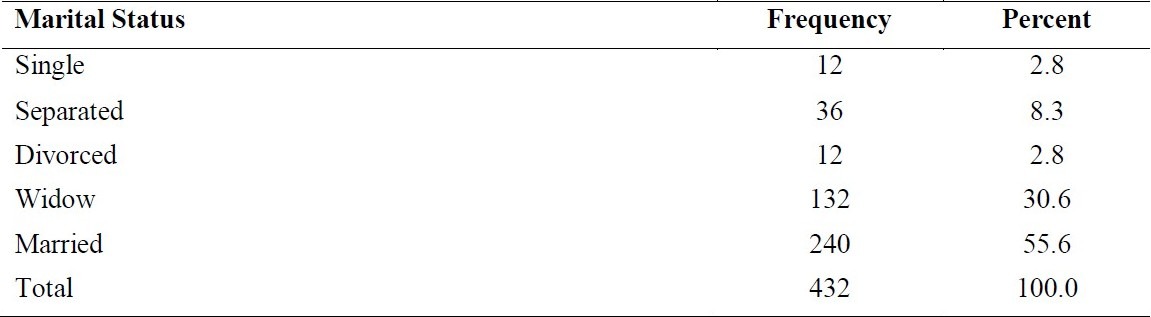
A total of 432 questionnaires were returned completed. The women studied were Igbo's who resides in Enugu. The response rate was 100%. While the age group 45-49 constitutes the highest in frequency, the age group 50-59 constitutes the least (38.9% versus 25% respectively). Single women were less than married women (2.8% versus 55.6%) as shown in tables 1 and 2.
Table 1.
(Age of Respondents)
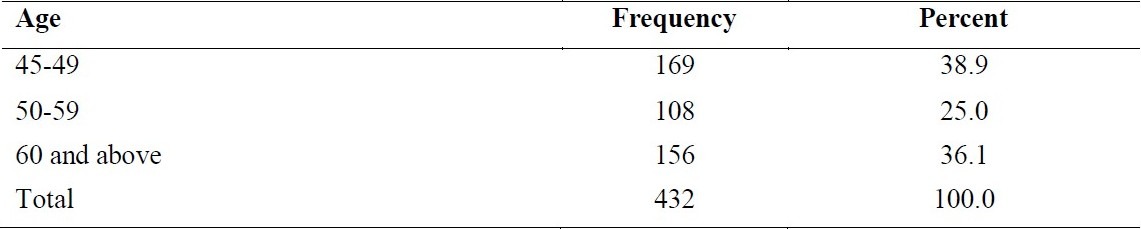
Table 2.
Marital Status of Respondents
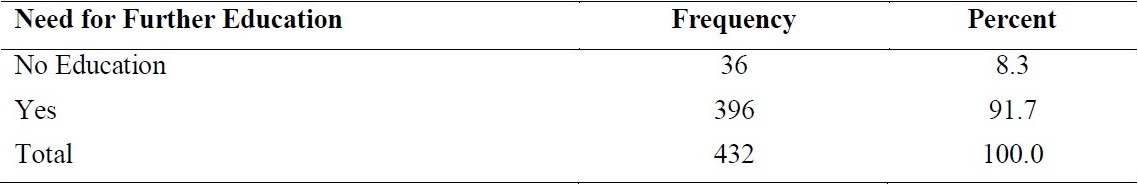
Out of 432 women studied, 372 (86.1%) had knowledge of menopause. Four hundred and eight (94.4%) had primary education and higher educational certificates. (Table 3). Three hundred and ninety six; 396 (91.7%) held the opinion that women should be educated more on menopause and its short and long-term effects. (Table 4). Educational level has a significant effect on perception of menopause. The illiterate ones never heard or recognised menopause and climacteric symptoms; rather they took it as part of their life.
Table 3.
The Level of Education/Knowledge of Menopause
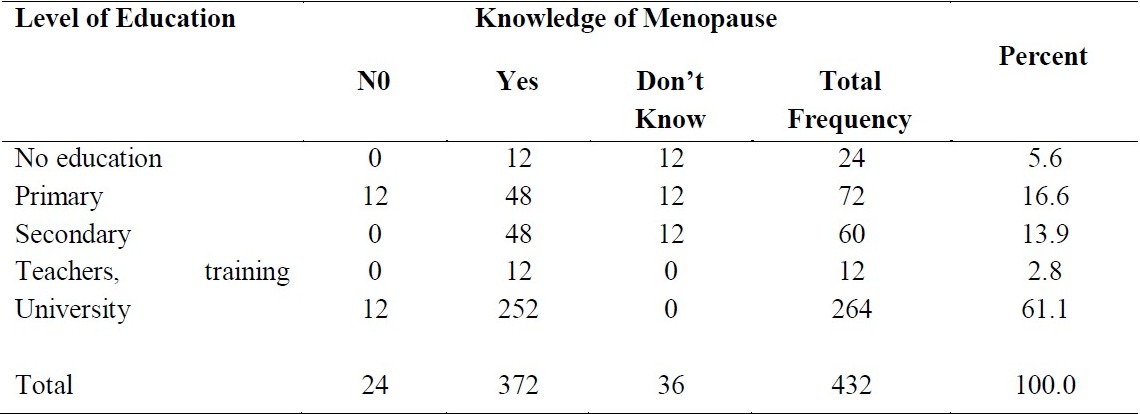
Table 4.
The Need for Further Education of Women on Menopause
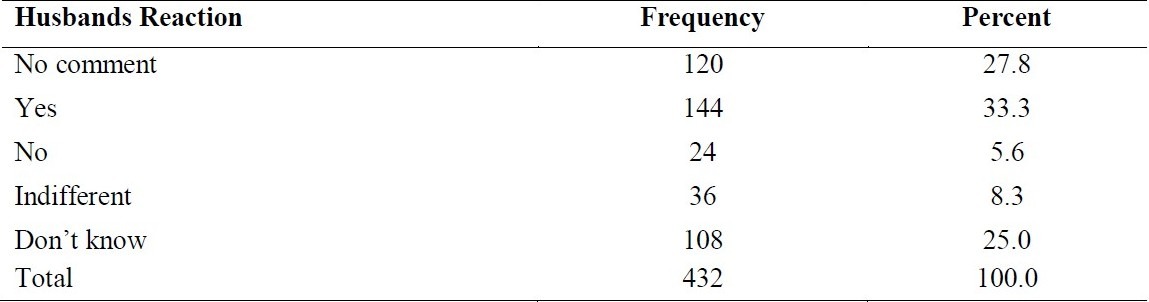
The study further showed that married women were more likely to respond to any questionnaire on menopause than single and separated women (55.6% vs. 2.8% and 8.3% respectively). The source of information was more from friends/mothers 180 (41.7%) and least from churches 12 (22.2%). Ninety six; 96 (22.2%) agreed that the climacteric symptoms affected their sex life as shown in table 5. One hundred and forty four; 144(33.3%) agreed that their husbands sympathised with them while 36(8.3%) revealed that their husbands were indifferent to their problems as shown in table 6.
Table 5.
The Effect of Menopause on Sex Life
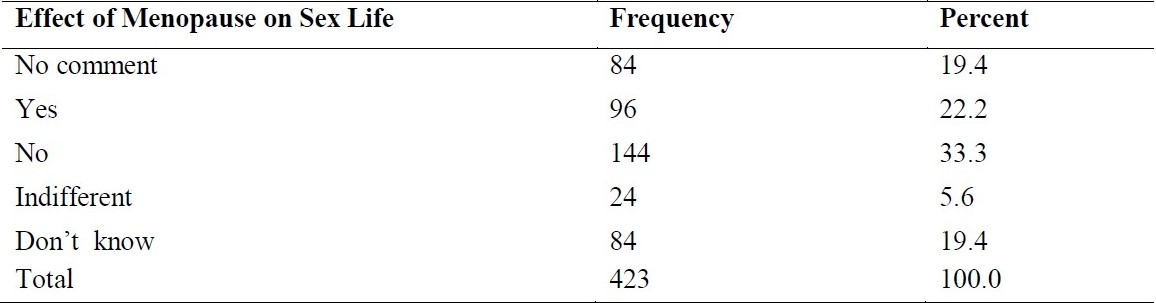
Table 6.
Husbands Reaction to Climacteric Symptoms on their Wives
Seventy two (16.7%) were unable to carry on with their job while 276 (63.9%) performed their normal duties without any problem.
Out of the 432 women studied, 144 (33.3%) sought for medical treatment while 252 (58.3%) did not take any medication but regarded climacteric symptoms as self limiting. Those who sought medical treatment made use of such facilities as gynaecology clinics, medical clinics, native doctor/sorcerer, priests and self administered prayers.
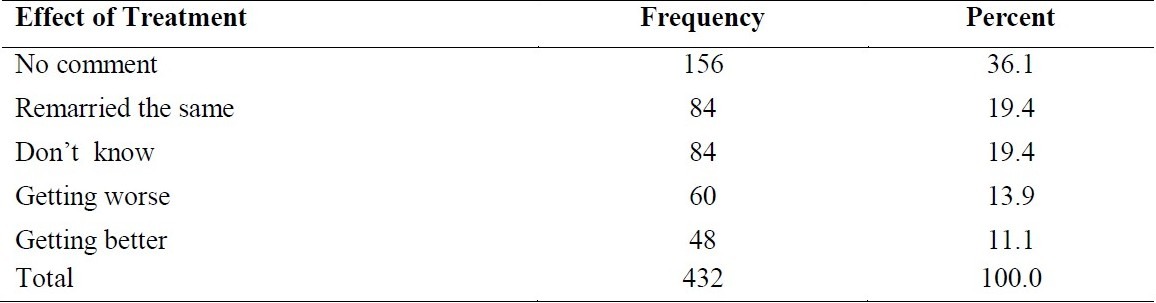
Ninety six (22.2%) consulted gynaecologists while 12 (2.8%) went to native doctor/sorcerer for assistance. Eighty four (19.4%) were of the opinion that the symptoms remained the same after treatment while 48 (11.1%) agreed that there was improvement in their condition, however 60 (13.9%) revealed that their condition became worse after treatment as shown in tables 7 and 8 respectively.
Table 7.
Facilities where medical advice was sought
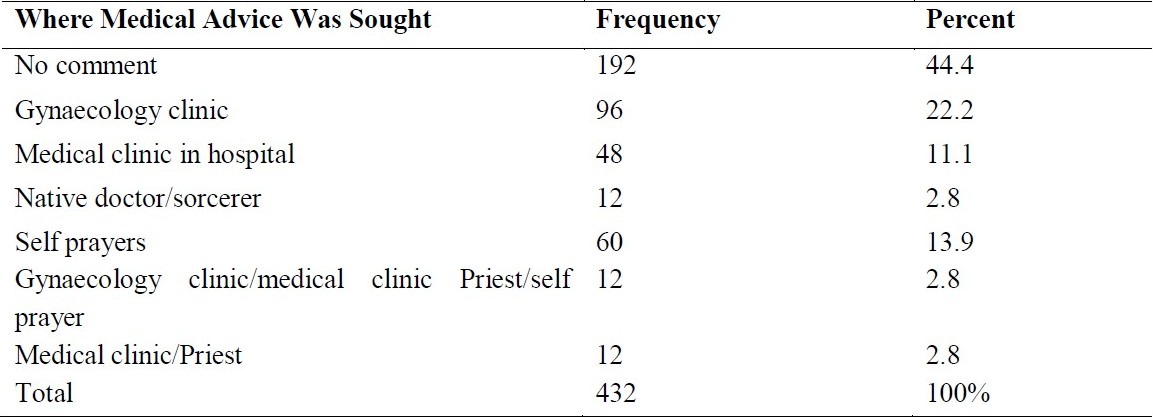
Table 8.
The Effect of Treatment on Climacteric Symptoms
Discussion
Menopause is the permanent cessation of menstruation resulting from the loss of ovarian follicular activity.7 This is recognised with certainty only in retrospect after 12 months of amenorrhoea without obvious pathologic or physiological cause.2,7 An adequate independent biologic marker for this event does not exist.7 The average age at menopause of 50 years has remained remarkably constant throughout the centuries, unaffected by improving nutrition and reduction of disease.1,7 However, certain chemotherapeutic agents, radiation, smoking and even hysterectomy, may contribute to an earlier onset of menopause.7
The vast majority of women will reach menopause and will spend one-third of their lives in this state.8 The long term metabolic problems of menopause are therefore becoming increasingly important. Oestrogen deficiency is the main pathology of menopause and is responsible for the numerous short and long-term symptoms.7 As a result of diminished ovarian oestrogen secretion and, ultimately, by sporadic ovarian activity, menstrual cycles are more likely to be anovulatory, with prolonged or erratic intermenstrual intervals and variable (at times excessive) menstrual flow.
The symptoms experienced by women randomly selected from Enugu metropolis are examined in this study. Single women and women in the lowest socioeconomic group were less likely to respond to questionnaire on menopause. The highly educated ones were aware of menopause and their response to it was high. The majority of women in the population studied experienced climacteric symptoms but relatively few regarded these symptoms as a problem. For example, hot flushes and night sweats were experienced by 70.0% but defined as a problem by only 30.0%. Out of 432 women studied, only 33.3% sought medical attention in hospital for their symptoms. Majority (58.3%) of the women did not regard them as a medical problem and took them as part of aging process. It suggests that menopausal symptoms are widely experienced by women in this age group, but they are not defined as problematic.
This study has shown that women's experience of the classic symptoms of hot flushes, night sweats among others, differed greatly according to menopausal status. Education had a significant effect on perception of menopause. Women with high educational level presented themselves to hospital for treatment and were keen to consult a doctor of any untoward effects of menopause. With this therefore, we necessitate more appropriate information dissemination to the less educated. The study is limited by the fact that recall of the women may have been incomplete. Furthermore lack of consensus on vernacular or tribal terminologies for terms related to menopause may have affected responses. Finally, level of education may have had an effect on perception of menopause.
In conclusion, education has a significant effect on the perception of menopause since a vast majority of women will reach menopause and spend one-third of their lives in this state8.
References
- 1.Beckmann CRB, et al., editors. Obstetrics and Gynecology. 2nd ed. Baltimore: Williams and Wilkins; 1995. Menopause; pp. 381–389. [Google Scholar]
- 2.Padubidri VG, Daftary SN. Howkins and Bourne Shaws Textbook of Gynecology. 13th ed. India: Elsevier; 2004. Menopause, Premature Menopause and Post menopausal bleeding; pp. 56–67. [Google Scholar]
- 3.Studd J, Watson N, Henderson A. Symptoms and metabolic sequelae of the Menopause. In: Drife J, Studd JWW, editors. Hormone Replacement therapy and Osteoporosis. London: Spring Verlag; 1990. pp. 23–33. [Google Scholar]
- 4.Neugarten B, Kraines R. Menopausal Symptoms in women of various ages. Psychosom Med. 1965;27:266–273. doi: 10.1097/00006842-196505000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Daly E, Gray A, Barlow D, Mcpherson K, Roche M, Vessey M. Measuring the impact of menopausal Symptoms on quality of life. BMJ. 1993;307:836–840. doi: 10.1136/bmj.307.6908.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Porter M, Panney GC, Russel D, Russel E, Templeton A. A population based survey of women's experience of the menopause. BJOG. 1996;103:1025–1028. doi: 10.1111/j.1471-0528.1996.tb09555.x. [DOI] [PubMed] [Google Scholar]
- 7.Ke RW. Management of Menopause. In: Ling FW, Duff P, editors. Obstetrics and Gynecology. Principles for Practice. 1st ed. New York: McGraw-Hill Companies Inc; 2001. pp. 1021–1040. [Google Scholar]
- 8.Peterson MEL. Menopause and Hormone Replacement Therapy. In: Luesley DM, Baker PN, editors. Obstetrics and Gynecology An evidence-based text for MRCOG. London: Arnold; 2004. pp. 600–605. [Google Scholar]


