Abstract
Background:
Perinatal mortality is one of the essential indicators of the health status of a country and by extension its state of development. Reduction in perinatal mortality rate is an important aspect of the MDGs.
Objectives:
To determine the perinatal mortality rate (PMR) in 2 tertiary institutions in Southern Nigeria and the factors responsible for the deaths.
Methods:
This was a retrospective, observational study conducted amongst 2 groups of subjects (A and B) located in 2 tertiary hospitals in Southern Nigeria over a 2-year period (1st Jan 2004 to 31st Dec. 2005). Variables such as maternal age, socio-economic status of the parents, sex, gestational age at delivery, mode of delivery, birth-weight, and age of baby before death and probable cause of death were recorded.
Results:
During the period, the perinatal mortality rate of 62.7/ 1000 live-births was recorded. The individual contributions to this rate were 22.1/1000 live births and 40.6/1000 live births for A and B respectively. The common causes of death in the study subjects were unbooked maternal status, fresh/macerated still births, low birth weight /premature babies and severe birth asphyxia. The mean gestational age for group A was 34.7 ± 6.50 wks and 33± 1.20 wks for group B, while the mean maternal ages were 27.3± 5.75yrs and 28.6 ± 5.1yrs respectively. Majority of the deliveries were by Spontaneous Vertex Delivery (SVD), accounting for 49.4% and 56% of the total deliveries in the two groups respectively. Furthermore, the male: female ratio was 0.85: 1.0 and 0.9: 1.0, the mean birth weights were 2.60 ± 1.87kg and 2.88 ±2.08kg and the unbooked cases were 61.9% and 70.6% respectively for group A and B.
Conclusion:
There is high rate of perinatal deaths in Southern Nigeria. This is associated with high rates of unbooked pregnancies resulting in difficult labours, ruptured uterus, chorio-amnionitis, preterm/low-birtthweight babies and severe neonatal asphyxia.
Keywords: Perinatal mortality, rate, causes, Southern Nigeria
Introduction
The perinatal period as defined by the World Health Organization (WHO) is the interval between 28 completed weeks of gestation (with babies weighing a minimum of 1000g) and the 1st completed week after birth.[1–3] It serves the dual purpose of being an indicator of the mother's health (and the care she received) during pregnancy/ delivery and a determinant of the baby's outcome later in life.[1] It is therefore a highly delicate period in the lives of both mother and baby. Death of a baby (including still births) within this period is referred to as perinatal mortality while perinatal mortality rate (PMR) is the number of such deaths (including still births) per 1000 live births. World-wide, about 7-9 million babies die annually, of which 98% occur in the tropics and developing countries where perinatal mortality rates are between 57 and 100 per 1000 birth.[1,2,12,13] These figures are about five times higher than those of developing countries.[30] These deaths are often linked to the absence of effective interventional efforts.
The perinatal mortality rate (PMR) in Nigeria varies from centre to centre ranging from 40 to above 80/1000 live births.[2] The National Demographic and Health Survey (2003) gave an estimated perinatal mortality rate (PMR) of 90/1000 live births in Nigeria.[4]. This figure is significantly high especially when compared to < 19/1000 live births obtained in developed countries of Europe, North America and Australia.[1,2] This high perinatal mortality rate (PMR) recorded in the country is also demonstrated by recent hospital-based studies which observed rates of 77.03, 50.9, and 133.9 per 1000 live births respectively.[5–7] Furthermore, a steady yearly increase in the rates was observed in these studies. Perinatal mortality rates in other African countries revealed that Ethiopia has 68 per 1000, South Africa 45 per 1000 and, Egypt 43 per 1000.[1]
Several factors are associated with high perinatal mortality rates. These include: low antenatal booking rates and poor antenatal clinic attendance during pregnancy, maternal age, late presentation at the hospitals during labour, multiple pregnancies and low birth weight babies.[5–7] Other factors such as too many closely spaced pregnancies and harmful practices such as inadequate cord care, letting the baby stay wet and cold, discarding colostrum and feeding other food, are deeply rooted in the cultural fabric of societies.[8] In many societies, perinatal deaths and stillbirths are not perceived as a problem, largely because they are very common.[8] Many communities have adapted to this situation by not recognizing the birth as complete, and by not naming the child, until the newborn infant has survived the initial period.[8]
The need to carry out this study was informed by the paucity of literature on perinatal mortality within the study areas in the recent past. The study is aimed at assessing the perinatal mortality rates and associated factors of perinatal deaths in the areas of study. It also hopes to make some recommendations towards significant reduction of these rates so that the attainment of the 4th MDG by the year 2015 will be realizable.
Methods
Study Design
Between January 2004 and December 2005, a retrospective, observational study was carried out in two tertiary institutions in Southern Nigeria, (A), Ebonyi State University Teaching Hospital Abakaliki (EBSUTH) and (B), University of Port Harcourt Teaching Hospital Port Harcourt (UPTH) on perinatal mortality. Study subjects were babies delivered in these hospitals that died from 28 weeks gestation to the first week of their birth (including still births).
Data Collection and Analysis
Data were collected from the birth records in the Labour Ward (LW), Antenatal ward (ANW), Accident and Emergency department and the New Born Special Care Unit (NBSCU) of both hospitals. These included variables such as maternal age, socio-economic status of the parents, sex, gestational age at delivery, mode of delivery, birth-weight, and age of baby before death and probable cause of death. The data collected were entered into the data editor of statistical package for social sciences (SPSS) software package version 11.0. Analysis was based on simple percentages, proportions and tables. The influences of the variables (sex, age, gestational age at delivery, mode of delivery, ANC attendance and birth-weight) on perinatal outcome were determined. Differences in Proportions were compared using the Chi square statistics. Statistical significance was set at p < 0.05.
Ethical clearance was gotten from the Ethics and Research Committee of both institutions.
Results
A total of 7678 deliveries were conducted in both institutions during the 24 month study period. Of these deliveries, 7225 were total live births with 453 perinatal deaths (including stillbirths), giving a perinatal mortality rate of 62.7/ 1000 live births and a male: female ratio of 0.9: 1.0.
Of the live births, 4020 were from EBSUTH and 3205 from UPTH, with perinatal deaths of 160 and 293, giving individual hospital's PMRs of 39.8 and 91.4/1000 live births, respectively.
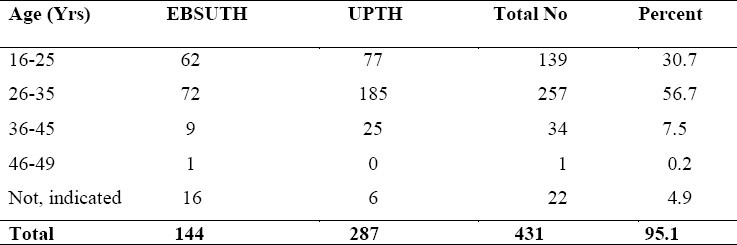
The maternal ages are shown in table 1. The ages ranged between 16 and 49 yrs while their mean ages were 27.3 ± 5.75yrs and 28.6 ± 5.1yrs for EBSUTH and UPTH respectively. Majority of the perinatal deaths occurred among women within the age group of 26-35yrs in both hospitals.
Table 1.
Maternal Age Distribution of Study Patients in Both Hospitals
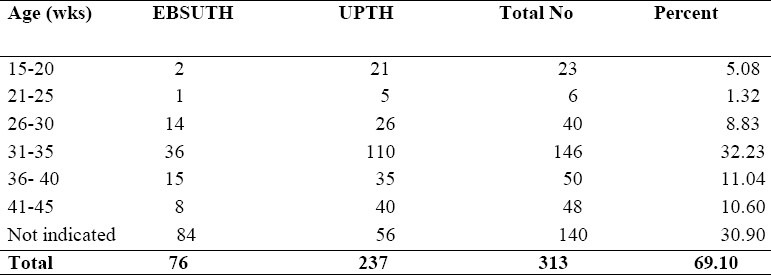
The gestational ages ranged from 19 to 42 wks with the mean gestational ages of 34.7 ± 6.50 wks in EBSUTH and 33.0± 1.20 wks in UPTH. Babies within the gestational age range of 31-35 wks were most affected accounting for 32% of the total. The gestational ages are shown in Table 2.
Table 2.
The Gestational Ages as seen in the Study Sites
The mode of delivery in both hospitals included emergency lower segment Cesarean section (32%), spontaneous vertex delivery (SVD) (54%) and vacuum extraction (14%). Spontaneous vertex delivery (SVD) was the major mode of delivery accounting for 49.4% and 56.0% of the deliveries in each of the hospitals respectively.
The birth weights of the babies were between 0.5kg and 4.2kg while their mean were 2.60 ± 1.87kg and 2.88 ±2.08kg in both hospitals.
Approximately 67.5% of the pregnant women were unbooked in both hospitals (i.e. did not register and never attended formal ANC). However, in each individual hospital the percentages of unbooked mothers were 61.9% and 70.6% respectively.
Table 3 shows associated maternal and fetal factors/causes for the perinatal deaths. Majority of the perinatal deaths were from maternal causes accounting 67.5% while the commonest causes include unbooked maternal status (48.6%), prematurity/low birth weight (10.8%), Fresh/macerated stillbirths (8.9%), and severe birth asphyxia (7.8%).
Table 3.
Maternal and neonatal causes of perinatal death.
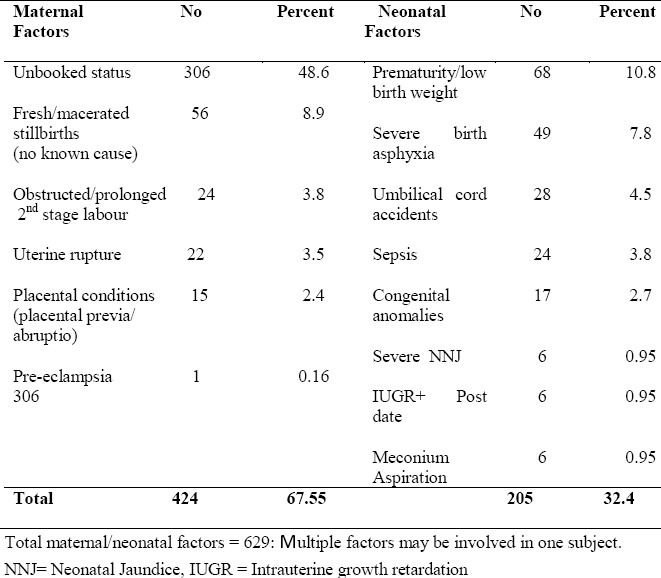
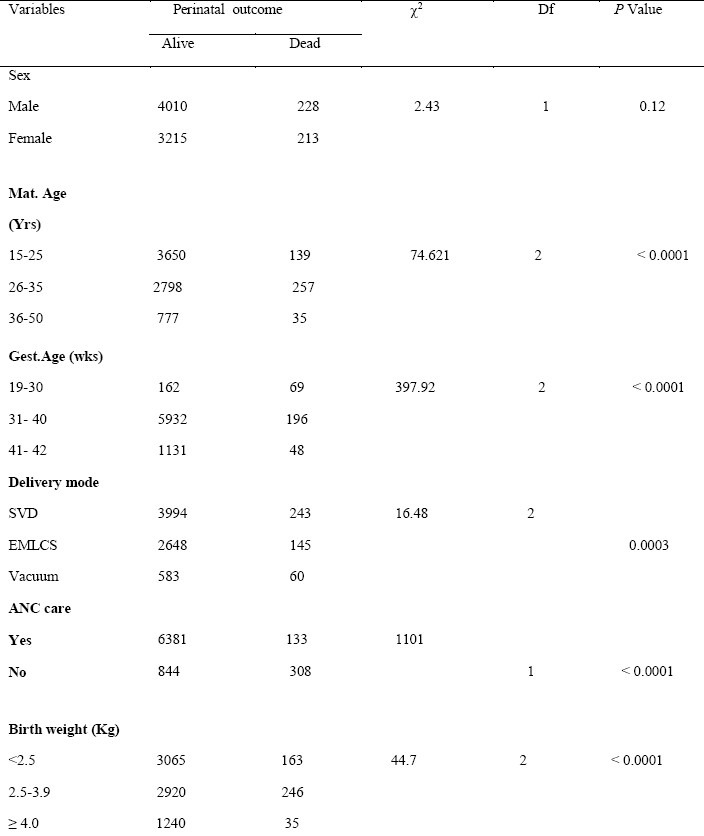
Table 4 shows the influence of certain variables on perinatal outcome in both hospitals. From the table, maternal age, unbooked maternal status, gestational age, birth weight of the babies and mode of delivery contributed significantly in the perinatal outcome.
Table 4.
The influence of certain variables on perinatal outcome in both hospitals
Discussion
The study revealed a perinatal mortality rate of 62.7/1000 live births in both institutions combined, with individual rates of 39.8 and 91.4/ 1000 live births for EBSUTH and UPTH respectively. The combined rate is lower than the national average of 90/1000 live births but much higher than 8.7/1000 in the UK[9] and <19.0/1000 live births obtained from developed countries of Europe, North America, Australia.[1,2] The combined rate is also lower than rates obtained in studies from other centres in Nigeria-133.94/1000 and 77.03/1000 live births obtained from the University of Nigeria Teaching Hospital, Enugu[7] and Wesley Guild hospital, Ilesa[5] respectively. It is however higher than 50.9/1000 live births obtained from Ogun State University Teaching Hospital, Sagamu.[6] The perinatal mortality rate in this study is still within the same range with other developing countries in Africa and Asia such as Cameroun and India with perinatal mortality rates of (60-79/1000livebirths).[10]
The causes of perinatal deaths were mostly related to maternal and neonatal factors. These include: unbooked maternal status, fresh/macerated still births, low birth weight /prematurity and severe birth asphyxia. Thus more deaths were recorded when mothers were either over-aged or under-aged, do not attend ANC during pregnancy, deliver prematurely, have low birth weight babies or are delivered by emergency Cesarean section. Bobzom and Unuigbe,1996[11] in their study conducted at the University of Benin Teaching Hospital, Benin, Nigeria demonstrated the important influence of booking status on the perinatal mortality rate. In the study, the perinatal mortality for unbooked patients was eight times that of the booked patients. Most of these deaths in addition to the other highlighted factors, revolved around the state of mother's health, nutrition, care during pregnancy, delivery, immediate post delivery period, which most often are poor.[1,2] It has been observed that perinatal outcome tended to be unfavourable in babies delivered before 35wks of gestation, had birth weight of <2.5kg, delivered by emergency cesarean section, or in babies born to under-aged or over-aged mothers, and also for mothers who were unbooked.[15–17] The figure from UPTH (91.4/ 1000 live births) is higher than the national average and much higher than EBSUTH figure. This may be related to some factors such as low booking maternal status. Only 29.4% of the pregnant mothers were actually booked for antenatal services in the centre. Other contributing factors may include the slightly higher maternal age (28.6 ± 5.1yrs) and lower gestational age (33.0± 1.20 wks) as opposed to 27.3 ± 5.75yrs and 34.7 ± 6.50 wks seen in EBSUTH.
The study shows that PNM has not declined and issues leading to its rise have not been fully addressed. However, it is retrospective and hospital based. A longitudinal, multicenter and community based study is critical to assess the exact magnitude of the problem. It is evident from this study, that the attainment of the 4th MDG before 2015 in this country may remain a mirage if major efforts are not made. Education of the public on the need for early booking(registration for antenatal care) when pregnant, proper antenatal care during pregnancy and supervised delivery, regular upgrading of neonatal intensive care facilities and regular retraining of health personnel on intrapartum care are areas that need emphasis. In the long term, it is the combination of education, improvement in the socioeconomic status of women and family planning information and services that will have the highest impact on perinatal mortality reduction.
References
- 1.Ibeziako NS. Perinatal and Neonatal mortalities. In: Azubuike JC, Nkangineme KEO, editors. Paediatrics and Child Health in a Tropical Region. Owerri: African Educational services; 2007. pp. 160–2. [Google Scholar]
- 2.Ugwu RO, Egri-Okwaji MTC. Perinatology in the tropics. In: Azubuike JC, Nkangineme KEO, editors. Paediatrics and Child Health in a Tropical Region. Owerri: African Educational services; 2007. pp. 157–60. [Google Scholar]
- 3.Cause- specific mortalities. Geneva: World Health Organization; 2003. The World Health Report. [Google Scholar]
- 4.National Demographic Health Survey. Federal Ministry of Health, Abuja Nigeria. 2003 [Google Scholar]
- 5.Kuti O, Orji EO, Ogunlola IO. Analysis of perinatal mortality in a Nigerian teaching hospital. J Obstet Gynaecol. 2003;23:512–4. doi: 10.1080/0144361031000153747. [DOI] [PubMed] [Google Scholar]
- 6.Njokanma OF, Olanrewaju DM. A study of neonatal deaths at the Ogun State University Teaching Hospital, Sagamu, Nigeria. J Trop Med Hyg. 1995;98:155–60. [PubMed] [Google Scholar]
- 7.Find-health.com. Perinatal mortality in University of Nigeria Teaching Hospital (UNTH) Enugu at the end of the last millennium - A review of research. 2007 [PubMed] [Google Scholar]
- 8.Mahy M. Childhood mortality in the developing world: a review of evidence from the Demographic and Health Surveys (DHS Comparative Reports, No.4) Calverton, MD: Macro International Inc; 2003. [Google Scholar]
- 9.Arulkumaran S. Perinatal Mortality. In: Arulkumaran S, et al., editors. Oxford Handbook of Obstetrics and Gynaecology. Oxford: University Press; 2007. p. 432. [Google Scholar]
- 10.Perinatal mortality. A listing of available information. 4th ed. 1996. World Health Organization. (WHO/FRH/MSM/95.7) [Google Scholar]
- 11.Bobzom DN, Unuigbe JA. Stillbirths and perinatal mortality at the University of Benin Teaching Hospital, Nigeria. J Obstet Gynaecol. 1996;16:8–9. [Google Scholar]
- 12.Maternal Care for the Reduction of Perinatal and Neonatal Mortality. Geneva: 1986. WHO/UNICEF; pp. 12–3. [Google Scholar]
- 13.Monterroso MS, Koglinsky M. Perinatal mortality: the uncounted millions. Mother care Matters. 1990;1:10–3. [Google Scholar]
- 14.World Health Organization. Maternal Health and Safe Motherhood Programme. Perinatal Mortality. WHO/FRH/MSH 96.7. [Google Scholar]
- 15.Anate M, Akeredolu P. Pregnancy outcome in elderly primigravida at the University of Ilorin Teaching Hospital, Nigeria. East African Medical Journal. 1995;73(8):548–51. [PubMed] [Google Scholar]
- 16.Oli JM, Osefo JJ, Okeke IC. Parity and perinatal mortality among diabetics in Nigerian Teaching Hospital. International Journal of Fertility. 1986;31:50–5. [PubMed] [Google Scholar]
- 17.Adedoyin MA, Adetoro OO. Pregnancy and its outcome among teenage mothers in Ilorin, Nigeria. East African Medical Journal. 1989;66:448–52. [PubMed] [Google Scholar]


