Abstract
Background:
Obesity in pregnancy has continued to attract global attention due to its contribution to maternal morbidity and mortality. However, this attention appears to be concentrated on developed countries with little or no attention to developing countries, resulting in very little statistics from developing countries on the subject matter.
Objectives:
To determine the prevalence and characteristics of obesity during pregnancy, in South-east Nigeria.
Method:
Women who registered for antenatal care in their first trimester of pregnancy were interviewed and requisite data collected. Fischer exact test, t-test and bivariate correlation analysis were carried out as appropriate at the 95% confidence level. P-values less than 0.05 were considered significant.
Results:
A total of 3,167 pregnant women were recruited. The prevalence of obesity in pregnancy was 10.7%. Obesity was significantly more prevalent amongst women residing in urban areas. Only 15.1% of participants knew their pre-pregnancy weight. Education, employment, parity and age did not have significant relations with obesity in pregnancy.
Conclusion:
Obesity in pregnancy exists in appreciable proportion in south-eastern Nigeria and majority of women in this setting do not know their pre-pregnancy weights. There is need to begin to consider obesity in pregnancy as a problem that does exist in resource-poor settings and specific guidelines on the management of obese pregnant women in resource-poor settings would be needed. Nigerian women need to be encouraged to check their weights periodically especially before planning pregnancy.
Keywords: Obesity, pregnancy, Nigeria
Introduction
Obesity is globally a public health issue. In recent times, the prevalence of obesity has been adjudged by the world health organization as having reached pandemic proportions. Obesity in pregnancy is also an increasing problem, especially in high income countries. The clinical importance of obesity in pregnancy lies mainly in its associated complications. The associated adverse effects of obesity in pregnancy include, higher incidences of miscarriages, congenital anomalies, thrombo-embolism, pregnancy induced hypertension macrosomia, operative deliveries as well as higher incidences of wound disruption and infection following cesarean delivery.[1–5] These effects confer a high risk status to pregnant obese women. Antenatal care is mainly preventive and anticipatory health care. Obesity is a risk factor that can be modified to improve outcome.
Researches have continued in all aspects of obesity in pregnancy in high income countries. Guidelines for management of obese women in pregnancy have also been developed and instituted in many high income countries.
In low-income countries, studies on obesity in pregnancy are scarce. No specific guidelines exist in most African countries for the management of obesity in pregnancy, highlighting the inadequate attention being paid to the problem of obesity in pregnancy. The problems of maternal and perinatal mortalities appear to have overshadowed obesity in pregnancy. Furthermore, obesity characterized by many as a disorder of the affluent, may not have received the desired attention in resource poor settings with known higher prevalence of under-nutrition. Knowledge of the prevalence and pattern of obesity among pregnant women would help to stimulate interest in this contemporary global issue in resource-poor settings. It would help to assess the burden and magnitude of the problem in this setting and may stimulate the institution of appropriate interventional guidelines that might help to reduce the prevalence of obesity and its complications in pregnancy. Allocation of scarce resources to the prevention and management of obesity in pregnancy would be more meaningful and purposeful if the prevalence is known. A medical literature search yielded very few publications on obesity in pregnancy from the African continent. The very few previous studies on obesity in Africa were limited by design and/or sample size. A large study from Tanzania studied only pregnant women from an urban setting.[2] Another study from Nigeria studied only 300 women scheduled for cesarean delivery.[1] Yet another study from Benin was limited by its retrospective design and small sample size of 323.[3]
This study is a prospective cohort study designed to capture both urban and rural pregnant populations in a resource poor setting in Nigeria, Africa.
Methods
The study population included women attending antenatal clinic at 3 maternity care facilities in Enugu state, southern Nigeria between April 2009 and January 2010. The total population of this state is 3.257 million according to the 2006 national population census. The health facilities were University of Nigeria teaching hospital, Ituku Ozalla Enugu, Mother of Christ specialist hospital, Enugu and Odugu memorial hospital, Mpamute in Igboeze North local government area, Enugu state. University of Nigeria teaching hospital serves a mix of urban and rural populations and also serves as a referral centre for the southern Nigerian states of Enugu, Imo, Anambara, Abia, Ebonyi and Benue; mother of Christ hospital serves mainly urban population, Odugu memorial hospital serves predominantly rural populations. Together, the three study centers serve a combined catchment population of 20.3 million people according to the 2006 Nigerian national population census. The study population comprises consecutive pregnant women who registered for antenatal care within the first 13 weeks of pregnancy within the study period at the study sites. Informed oral consent and was obtained from each participant before recruitment. Ethical clearance was also sought from our institutions ethical committee. A pre-designed structured data pro forma was used to obtain information. The information obtained included age of the participant, employment status of participant and husband, education status of participant and husband, parity, gestational age at booking, pre-pregnancy weight, maternal weight at booking, height, gestational age, family/personal history of diabetes and hypertension, multiple gestation, and place of residence. Women with multiple pregnancies, HIV positive women and those who had hyperemesis gravidarum were excluded.
The weight was measured using a Harson weighing scale while the height was measured using pre-calibrated wall height measurements. Obesity was defined as a body mass index (BMI) of ≥ 30 according to the cut off criteria set by the world health organization.[6]
The data were analyzed using SPSS version 12.0. Fischer exact test, t-test and bivariate correlation analysis were carried out as appropriate at the 95% confidence level. P-values less than 0.05 were considered significant.
Results
A total of 3,167 pregnant women were recruited. The maternal mean age was 29.8 ± 5.2 (Range: 17 - 49) years.
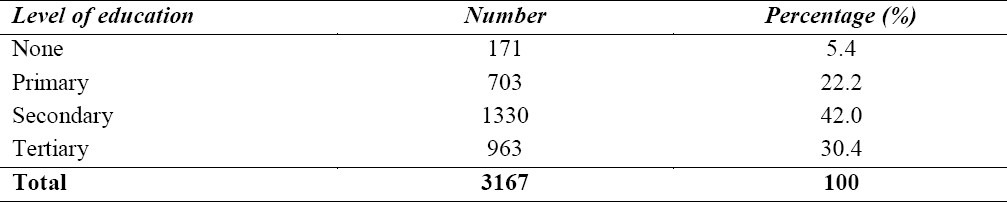
The parity distribution is as shown in Table 1 while Table 2 shows the distribution of participants according to educational status. One thousand, two hundred and ninety-eight (41.0%) participants were employed while 1869 (59.0%) were unemployed.
Table 1.
Parity distribution
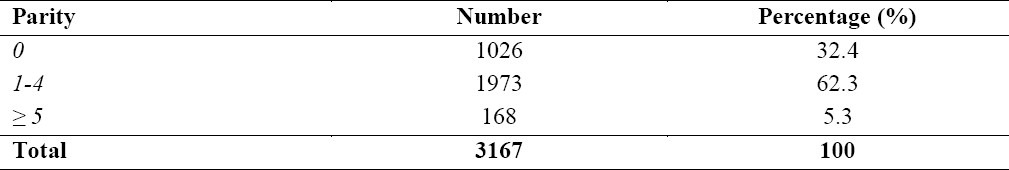
Table 2.
Education status of participants
The mean gestational age at first antenatal visit was 11.0 ± 2.2 (Range: 5 - 13) weeks.
Two thousand and twenty participants (63.8%) live in urban areas while 1147 (36.2%) live in rural areas.
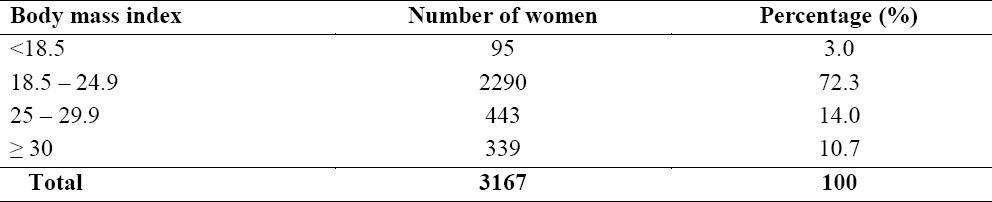
A total of 339 women had body mass index of ≥30 and were classified as obese. This gave a prevalence of 10.7%. Four hundred and forty-three participants (14.0%) had body mass index of between 25.0 and 29.9 and were classified as overweight (Table 3).
Table 3.
Body mass index of 3167 pregnant women in south eastern Nigeria.
The proportion of women residing in urban areas who were obese was significantly higher than the proportion residing in rural areas (15.4% vs. 2.4%; P= 0.0001).
There difference between the proportions of women with tertiary education who were obese and those without tertiary education who were obese did not reach statistical significance (9.1% vs. 11.4%, P=0.06). There was also no significant difference between the proportions of employed women were obese and that of unemployed women (10.6% vs. 10.8 %, P = 0.095).
Bivariate correlation analyses showed no significant correlation between body mass index and age of participants (Pearson's correlation coefficient = 0.023, P = 0.13). There was also no significant correlation between body mass index and parity of participants (Pearson's correlation coefficient = – 0.022, P = 0.78).
Only 478 (15.1%) women knew their pre-pregnancy weight. Analysis of women who knew their pre-pregnant weights showed a mean weight gain of 0.12 ± 0.24 (Range: –1.5 to 2.0) Kg and a mean gain in BMI of 0.07 ± 0.10 (Range: –0.41 to 0.71) within the first 13 weeks of pregnancy. There was no significant difference between the mean pre-pregnancy weight and the mean weight in the first 13 weeks of pregnancy (70.1 ± 11.7 vs. 70.4 ± 10.9, P=0.7). There was also no significant difference between the mean body mass index before pregnancy and the mean body mass index in the first trimester of pregnancy (26.4 ± 1.3 vs. 26.5 ± 1.7, P=0.3). All the women (100%) who knew their pre-pregnancy weight had university education and resided in urban areas.
Discussion
The study captured a mixed population of rural and urban dwellers in a low-income setting. Although body mass index is not reliable in pregnancy, the inclusion of only women in their first trimester of pregnancy took care of this limitation. Maternal weight gain in the first trimester of pregnancy is negligible and sometimes there could be weight loss due to nausea and vomiting associated with early pregnancy. First trimester maternal weight could be taken as a reasonable representation of maternal pre-pregnancy weight. The results of the analysis of women in this study who knew their pre-pregnancy weight supports this assertion. A previous study reported good correlation between maternal weights recorded at first antenatal visit and independently reported pre-pregnancy weights.[7] This becomes even more relevant in the setting of most low-income countries where majority of the pregnant population are unaware of their pre-pregnant weights as was the case in this study population. Only 15.1% of the study population was aware of their pre-pregnancy weight, indicating a lack of weight consciousness amongst the female population in this setting. It is instructive to note that, the prevalence of obesity of 10.7% in this study is quite high and surprising considering the previously-held idea that obesity a problem of affluent societies. This is similar to findings from Australia.[8] Furthermore 14 % of women in this study were over-weight. In a previous report from Nigeria, an incidence of 50.7% was reported.[1] This very large incidence may have resulted from the sample population of only pregnant women in their third trimester of pregnancy scheduled for cesarean in a University Teaching Hospital, the small sample size of 300 women and the use of body mass index in defining obesity in the third trimester of pregnancy. These limitations were taken care of in this study. The prevalence of obesity in this study is similar to the 9.1% reported from Tanzania in 2006.[2]
Significantly more women who resided in urban areas were obese when compared to those who resided in rural areas. One may be tempted to relate this to the possible difference in income between the two groups. However, the employment status and educational status which relate positively with individual income did not appear to affect the prevalence of obesity in this study population. The reasons for the difference in prevalence of obesity between urban and rural populations in this study may lie in the dietary and activity pattern. The staple food in most rural populations in Southeast Nigeria consists mainly of traditional high fiber foodstuffs and complex carbohydrates. Women in these rural populations are mainly subsistence farmers who intensely and manually work the agricultural fields, hence they are very less likely to be obese than women in urban areas who eat more of processed, commercial foodstuff and snacks and are engaged in more sedentary occupations. This supports the age-long known weight-modifying factors namely dietary and physical activity pattern. Physical inactivity was identified as a risk factor for obesity among blacks in South Africa.[9]
There was no significant correlation between parity and body mass index. This is contrary to findings from a recent study in Saudi Arabia.[10]
The proportion of women who were aware of their pre-pregnancy weight (15.1%) is instructive. This implies that any program aimed at reducing or halting the increase in the prevalence of obesity in pregnancy needs to include raising weight-consciousness amongst the female population. A woman who does not care to know her weight is unlikely to be interested in any weight-reducing policy or program. The medical problems associated with obesity in the pregnant and non-pregnant woman make it impossible for this subject to remain ignored in developing countries. It is known that obesity is a modifiable determinant of adverse pregnancy outcome. The problem of obesity in pregnancy is here with us in low-income countries. This implies a need to begin to draw up strategies for the prevention and management of obesity in pregnancy in Nigeria and other African countries. Prevention strategies would entail raising weight consciousness on the population, encouragement of healthy dieting and exercise. Future studies should focus on outcome of pregnancies in obese women in low-income countries and effective strategies to reduce the incidence of obesity in pregnancy in low-income countries.
In conclusion, obesity in pregnancy exists in appreciable proportion in south-eastern Nigeria and majority of women in this setting do not know their pre-pregnancy weights. There is need to begin to consider obesity in pregnancy as a problem that does exist in resource-poor settings and specific guidelines on the management of obese pregnant women in resource-poor settings would be needed. Nigerian women need to be encouraged to check their weights periodically especially before planning pregnancy.
References
- 1.Callaway LK, Prins JB, Chang AM, McIntyre HD. The prevalence and impact of overweight and obesity in an Australian obstetric population. Med J Aust. 2006;184(2):56–59. doi: 10.5694/j.1326-5377.2006.tb00115.x. [DOI] [PubMed] [Google Scholar]
- 2.Colatrella A, Braucci S, Festa C, Bianchi P, Fallucca F, Mattei L, et al. Hypertensive Disorders in Normal/Over-weight and Obese Type 2 Diabetic Pregnant Women. Exp Clin Endocrinol Diabetes. 2009;17(8):373–7. doi: 10.1055/s-0029-1220763. [DOI] [PubMed] [Google Scholar]
- 3.Djrolo F, Megnigbeto OA, De Souza J, Takpara I, Santos P, Alihonou E. Influence of maternal weight on pregnancy outcome in Cotonou (Benin) J Gynecol Obstet Biol Reprod. 2002;31(3):243–7. [PubMed] [Google Scholar]
- 4.Edomwonyi NP, Osaigbovo PE. Incidence of obesity in Parturients scheduled for cesarean section, intra-operative complications, management and outcome. East Afr Med J. 2006;83(4):112–9. doi: 10.4314/eamj.v83i4.9425. [DOI] [PubMed] [Google Scholar]
- 5.Kruger HS, Venter CS, Vorster HH, Margetts BM. Physical inactivity is the major determinant of obesity in black women in the North West Province, South Africa: the THUSA study. Transition and Health during Urbanization of South Africa. Nutrition. 2002;18:422–7. doi: 10.1016/s0899-9007(01)00751-1. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organisation Global Database on Body Mass Index. [Assessed on 2011; Nov 04]; Available at http://apps.who.int/bmi/index.jsp?introPage=intro_3.html .
- 7.Mamun AA, Lawlor DA, O’Callaghan MJ, Williams JM, Najman JM. Family and early life factors associated with changes in overweight status between ages 5 and 14 years: findings from the Mater University Study of Pregnancy and its outcomes. Int J Obes. 2005;29:475–82. doi: 10.1038/sj.ijo.0802922. [DOI] [PubMed] [Google Scholar]
- 8.Satpathy HK, Fleming A, Frey D, Barsoom M, Satpathy C, Khandalavala J. Maternal obesity and pregnancy. Postgrad Med. 2008;120(3):E01–9. doi: 10.3810/pgm.2008.09.1920. [DOI] [PubMed] [Google Scholar]
- 9.Villamor E, Msamanga G, Urassa W, Petraro P, Spiegelman D, Hunter DJ, et al. Trends in obesity, underweight, and wasting among women attending prenatal clinics in urban Tanzania, 1995–2004. Am J Clin Nutr. 2006;83(6):1387–94. doi: 10.1093/ajcn/83.6.1387. [DOI] [PubMed] [Google Scholar]
- 10.El-Gilany A, Hammad S. Body mass index and obstetric outcomes in pregnant in Saudi Arabia: a prospective cohort study. Ann Saudi Med. 2010;30:376–80. doi: 10.4103/0256-4947.67075. [DOI] [PMC free article] [PubMed] [Google Scholar]


