Abstract
Background:
There are several problems militating against satisfactory residency training in Nigeria. These problems may not be effectively identified and resolved if the opinion of the trainee doctors is ignored.
Objectives:
To review surgical residents’ perspectives of their training program in South-eastern Nigeria, with the aim of suggesting evidence-based innovative changes to enable the programs meet global trends and standards.
Materials and Methods:
A total of 90 semi-structured and pre-tested questionnaires were evenly distributed (30 per hospital) to the surgical residents at three tertiary healthcare facilities in South-eastern Nigeria. Information sought included sociodemographic variables, level in the residency training, rating of program and different aspects, learning environments/opportunities, and suggestions on ways to improve either part or overall program.
Results:
Analysis of 56 properly completed questionnaires (response rate=62.2%) shows that the respondents were aged 29 to 53 years [mean(SD) = 35.3(1.7)], mostly males (91.1%) and junior residents (75%). A significant majority of residents (47 or 83.8%) rated the surgical residency training in their respective centers as inadequate. Grand rounds were roundly criticized as having misplaced objectives and tending toward fault-finding by Consultants. Suggested interventions for improvement included enhanced supervision/mentoring/teaching by senior colleagues, inclusion of didactic lecture sessions, research trainings, and foreign postings.
Conclusion:
There exist gaps between expectations of surgical residents and the training offered. These create needed support for an evidenced-based review of surgical residency training program to enable it meet the aspirations of trainees and the ever-changing trend in Medicine. More studies on surgical residents covering other regions of Nigeria, and including the trainers (Consultants), will be of immense value.
Keywords: Enugu, Medical, Nigeria, Resident doctors, Surgical training
Introduction
A resident doctor in Nigeria is a fully registered medical practitioner undergoing further training in an institution accredited by either the National Postgraduate Medical College of Nigeria and/or the West African Postgraduate Medical College.[1] In both Colleges, fellowship is awarded after passing a 3-stage examination (Primary, Part I and Part II) program during the training. Candidates for the residency program are expected to possess a registrable qualification by the Nigerian Medical and Dental Council (NMDC). The primary examination covers basic sciences and successful candidates (Junior resident) must then undergo training in principles and practice of general surgery and complete clinical posting rotations in the following departments; Casualty/Trauma/Orthopedics, General surgery, Urology, and Anesthesia for two years to qualify for the Part I final examination. Successful candidates (Senior residents) will then commence rotation for the last stage which is the Part II Final Examination in one of the following departments: General surgery, Orthopedics/Traumatology, Urology, Pediatrics Surgery, Cardiothoracic Surgery, Neurosurgery, or Plastic surgery. The expected learning environments include clinics/outpatient departments, ward/ground rounds, theatre sessions, accident and emergency units, clinical meetings/academic conferences, and other workshops/seminars all under the supervision of their Consultants/Trainers. The Postgraduate Colleges also arrange annual integrated courses for the candidates at the different stages of training.[1] Despite the associated stress,[2] poor structuring nature of the program,[3] and lack of facilities,[4] residents are expected to be proficient clinicians, educators, researchers, and administrators at the end of their training.[5] However, decreasing surgical skills and surgical experiences over the years by residents have been reported,[6] and thus, there is the need to constantly review the training program. This study therefore aimed to assess surgical residents’ perspectives of their training program in three accredited tertiary health institutions in South-Eastern Nigeria. The results are expected to serve as feedback for innovative changes to achieve overall training objectives and global trends.
Materials and Methods
This descriptive cross-sectional study was conducted at three accredited tertiary health institutions in South-eastern Nigeria. A total of 90 semi-structured pre-tested questionnaires were distributed equally (30 per center) to the surgical residents at National Orthopedic Hospital Enugu (NOHE), University of Nigeria Teaching Hospital (UNTH) Enugu, and Nnamdi Azikiwe University Teaching Hospital (NAUTH) Nnewi. The questionnaires were distributed and collected physically during weekly clinical meetings in the above-named institutions.
The inclusion criteria were as follows
The resident must have been in the training for at least a year
The resident must not be rotating through the institution from an institution outside the south-eastern Nigeria
Informed consent.
Indices sought were sociodemographic variables and stage in the residency training, frequency of learning opportunities, rating of entire/components of the program, perceptions and evaluations of exposed learning environments, and suggested improvements for either components or entire surgical training program.
Responses were collated and analyzed using SPSS version 18.
Results
Sociodemographic variables
Seventy-two (80%) of questionnaires were returned, but only 56 (62.2%) were returned properly filled from residents aged between 29 to 53 years [mean(SD) = 35.3(1.7)]. Also, 51 (91.1%) of respondents were males and 42 (75%) were junior residents with the rest 14 (25%) senior residents. Only three (5.4%) admitted to rarely attendance of academic programs with the rest attending either most 38 (67.9%) or when possible 15 (26.8%).
Frequency of learning opportunities
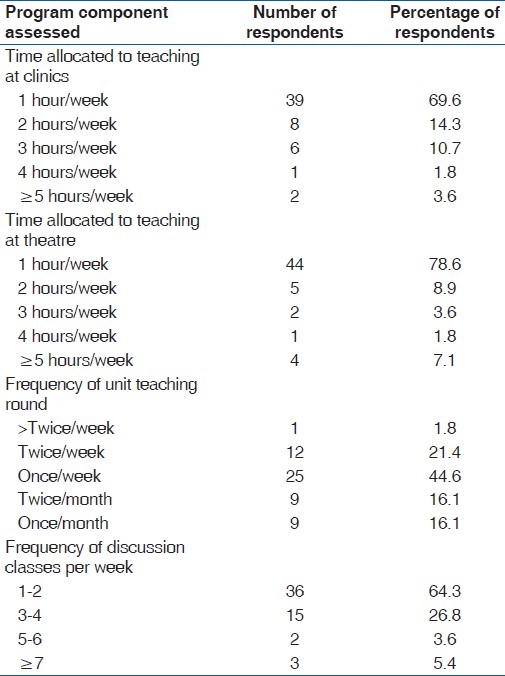
Table 1 shows that only two (3.6%) respondents/residents had up to 5 hours per week of clinic teaching environment, while significantly more residents 39 (69.6%) had an average of one hour/week. For time allocated to teaching during theatre sessions, 44 (78.6%) considered it to be about one hour/week, while only four (7.2%) had up to 5 hours/week. Also, average frequency of surgical unit's rounds for 25 (44.6%) was once/week, nine (16.1%) had it once/month, while only one (1.8%) of residents had teaching round more than twice/week.
Table 1.
Frequency of learning opportunities/environments
Rating of entire/components of the program
Most residents/respondents (28, 67.9%) rated grand rounds to be beneficial to the training program. Thirty (53.6%) perceived study either with other residents (24, 42.9%) or personal study (16, 28.6%) as the most valuable in perceived acquired knowledge in their training. However, 30 (53.6%) rated their percentage of skill acquisition commensurate with their status and number of years in training as ≥50% with only two persons (1.8%) scoring themselves above 80%.
On overall assessment of surgical training, 31 (53.3%) of respondents rated the program as inadequate, and another 17 (30.4%) rated it as grossly inadequate.
Poor ratings were due to perceived shortcoming in the following areas:
Inadequate teaching and supervision by trainers.
Absence of foreign training exposures.
No period of time dedicated strictly for research training.
Unclear structuring of training program.
Lack of adequate practical exposure with paucity of surgical skills.
Lack of surgical equipment and paucity of facilities.
Suggested interventions
Suggested improvements for either components or entire surgical training program in decreasing scale of preference included the following:
Incorporation of didactic lectures and enhanced teaching by Consultants during ward rounds – 50 (89.2%).
Compulsory overseas training program – 48 (85.7%).
Training should be more inclined to surgical skill acquisition – 44 (78.6%).
Commence research trainings programs – 44 (78.6%).
Support research by Residents through grants and sponsorships – 43 (76.7%).
Procurement of modern diagnostic and surgical equipments – 40 (71.4%).
Improved remuneration – 34 (60.7%).
A closer and cordial trainer and trainee relationship – 34 (60.7%).
Discussion
The mean age (35.1±1.7) of residents/respondents in this study was similar to those found in other studies in Nigeria.[2,7] This finding might support the views of Issa et al. 2009 that entry into residency training programs has become very competitive with some applicants having to wait for a long period before entrance, thus making it difficult to find residents in the twenties age range. The male predominance in this study is similar to findings of Ndom and Makanjuola 2004 but differs from Cohen and Patten 2005 and may be related to reported associated stress such that females may tend to avoid residency training because of the additional involvements with keeping a family.[2–4] Another possible reason might be that more males graduate from Nigerian medical schools[2] and subsequently enroll for residency training. Almost three-quarter of respondents were lower status (junior) residents representing similar to report by Issa et al.[2] and this may be due to delays in passing of Part 1 finals examinations, and may also be implicated in the finding of residents aged up to 53 years in training programs. These factors may have contributed to the low rating of the program by the most residents. Attendance to academic programs among residents is fair with over 67% attending regularly and only 5.4% of respondents rarely attending. This few may represent those gradually losing interest due to stress and frustrations from multiple attempts in the examinations. The lackadaisical attitude of these few may also contribute to perceived lack of commitment by the consultants leading to less mentoring and reduced teaching at clinics, ward rounds, and theatre sessions.
The time apportioned for teaching either at clinics, wards, or theatre is poor [Table 1], thus the residents depend almost entirely on self effort or on fellow residents for most of their learning experiences. The finding that inter-personal study with fellow residents was of greatest value to acquired knowledge in 42.9% of residents assert this and partly demonstrates the perceived low level of commitment of consultants to teaching and mentoring. These issues may have been contributory to earlier reports of declining quality of educational system and low prospect of professional development by doctors in Nigeria as part of factors that cause high rate of migration of Nigerian doctors to other countries.[8] A likely contributory factor to the low perception of the contribution of Consultants to teaching and skill acquisition may also be the lopsided “Consultant: Resident ratio.”
A majority (53.4%) of our respondents rated their training as inadequate and this supports earlier reports of unsatisfactory working condition and lack of professional equipment/tools by Nigerian doctors.[8] However, 53.6% of the residents rated their percentage of skill acquisition commensurate with their status and number of years in training as above 50% and another 1.8% rated it as above 80%.
It is clear from our study that residents want more attention from their Consultants, evidenced by the number of respondents that recommended the inclusion of formal didactic lectures and, despite their dissatisfaction with the Grand rounds, majority rated it as beneficial for the program. Criticisms of grand rounds bordered on its misplaced objectives, tendency toward finding faults, and apportioning blame rather than being educative, and in some surgical specialties, it is not existent. This perception is not unusual considering that more than 75% of residents responding to a survey on “experiences” in Alberta have earlier reported intimidation and harassment from many members of the healthcare team.[5] Thus, we believe that improvements in the quality of grand rounds will be of immense value to the entire training program. The results clearly show that Residents’ desire inclusion of additional training on research in their program. Also, exposure to leadership training is reportedly limited, confirming the earlier reports that traditional focus of residency training has been on development of clinical judgment and technical skills.[9,10] The transition from a resident to a consultant with its attending responsibilities is often abrupt and it is imperative that a resident inculcates the needed managerial and leadership traits while still training.[11] Also, 73.2% of residents desire the inclusion of foreign postings supporting earlier view that exposure to modern surgical training in better-endowed centers should be incorporated into the residents’ training program.[3] In managing patients, the resident/trainee needs to demonstrate a good grasp of “options” of proven efficacy and this calls for regular sharing of ideas and experiences with colleagues from other centers.[11] We believe this will provide resources to improve the knowledge base and mentoring skills by the trainees who will in future become consultants, in agreement with Sutherland's 2007 suggestion on development of positive role models and more educational activities for surgical residents.[12] These reported perceived short comings in the training program may be responsible for assertion by Sutherland 2007 that “many people today add additional years to their training with research years or ‘super’ fellowships.”
Conclusion
Gaps exist between expectations of surgical residents to the training being offered in major centers in South-eastern Nigeria. Residents expect more teaching and supervision from their consultants under a friendlier environment. A more extensive study involving other regions of Nigeria, and including the trainers (Consultants), is recommended.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.West African College of Surgeons. Prospectus, College secretariat Ibadan, Nigeria. 1995 [Google Scholar]
- 2.Issa BA, Yussuf AD, Olanrewaju GT, Oyewole AO. Stress in residency training as perceived by resident doctors in a nigerian university teaching hospital. Eur J Sci Res. 2009;30:253–9. [Google Scholar]
- 3.Adebamowo CA, Ezeome ER, Ajuwon AJ, Adekunle OO. Job stress associated with surgical training in Nigeria. Afr J Med Med Sci. 1998;27:233–7. [PubMed] [Google Scholar]
- 4.Woloschuk W, Harasym P, Mandin H. Implementing a clinical presentation curriculum: Impact on student stress and workload. Teach Learn Med. 1998;10:44–50. [Google Scholar]
- 5.Cohen JS, Patten S. Well-being in residency training: A survey examining resident physician satisfaction both within and outside of residency training and mental health in Alberta. BMC Med Educ. 2005;5:21. doi: 10.1186/1472-6920-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sorosky JI, Anderson B. Surgical experiences and training of residents: Perspective of experienced gynecologic oncologists. Gynecol Oncol. 1999;75:222–3. doi: 10.1006/gyno.1999.5570. [DOI] [PubMed] [Google Scholar]
- 7.Ndom RJ, Makanjuola AB. Perceived stress factors among resident docors in a Nigerian teaching hospital. West Afr J Med. 2004;23:232–5. doi: 10.4314/wajm.v23i3.28128. [DOI] [PubMed] [Google Scholar]
- 8.Ike SO. The health workforce crisis: The brain drain scourge. Niger J Med. 2007;16:204–11. [PubMed] [Google Scholar]
- 9.Bowen JL. Adapting residency training. Training adaptable residents. West J Med. 1998;168:371–7. [PMC free article] [PubMed] [Google Scholar]
- 10.Shwartz RW. Physician leadership: A new imperative for surgical educators. Am J Surg. 1998;176:38–40. doi: 10.1016/s0002-9610(98)00091-9. [DOI] [PubMed] [Google Scholar]
- 11.Omisanj AO. The ideal resident doctor: a resident's perspective. Ann Ibadan Postgrad Med. 2005;3:67–71. [Google Scholar]
- 12.Sutherland MJ. A young surgeon's perspective on alternate surgical training pathways. Am Surg. 2007;73:114–9. [PubMed] [Google Scholar]


