Abstract
Background:
Depression is a common psychiatric disorder in epilepsy patients. A bidirectional interaction is thought to be present between epilepsy and depression. There are few studies of this relationship in Nigerian Africans.
Objectives:
This was a cross-sectional study of the frequency and pattern of depression in a cohort of epilepsy patients in Enugu, South East Nigeria.
Materials and Methods:
Adult patients with epilepsy seen at the University of Nigeria Teaching Hospital, Enugu, from May to September 2009 were assessed for depression using the Becks Inventory for Depression. Informed consent was obtained from each patient. Clinical data obtained were analyzed using Statistical Package for the Social Sciences, version 15. The hospital's ethical review committee approved the study.
Results:
I0 n all, 83 subjects were studied (50 males and 33 females). They were aged from 18 to 75 years, with an average of 29.87 years. Most subjects were <25 years of age, single (53, 64%) and had at least secondary school education (65, 78%). Depression was present in 71 (85.5%) subjects – minimal 57 (68.7%), mild 10 (12%), and moderate 4 (4.8%). No case of severe depression was seen. Patients <25 years of age were the most affected. Depression was not significantly associated with age, gender, seizure type, or educational level.
Conclusion:
A significant proportion of Nigerian African epilepsy patients have depression, which may be easily overlooked, with far-reaching consequences on patients’ quality of life, morbidity, and mortality rates. There is need to regularly assess for and manage epilepsy-related depression in this population.
Keywords: Depression, Epilepsy, Nigerian Africans
Introduction
Depression is one of the most prevalent psychiatric disorders occurring in patients with epilepsy.[1] Most of the time it is underrecognized and has a huge impact on their quality of life.[1–3] Patients with epilepsy have a higher prevalence of depression than the general population and studies estimate the incidence to range between 20 and 54%.[4–6]
A bidirectional interaction is thought to be present between epilepsy and depression. Studies have shown that newly diagnosed epilepsy patients were up to 3.7–6 times more likely to have depression preceding the epilepsy than controls.[7,8] In people with epilepsy, depression can be a psychosocial reaction to having the condition or being treated differently because of it. The bidirectional interaction between depression and epilepsy is believed to be multifactorial and includes genetic, iatrogenic, endogenous, and adaptive/maladaptive processes.[9] These studies appear to suggest an interaction between epilepsy and depression, which is not restricted to the chronic epilepsies. Factors thought to be responsible include the use of some anticonvulsants like phenobarbitone, primidone, frequency and type of seizure, gender, and socioeconomic status.
There is a general consensus that the psycho-social problems of epilepsy are often more disabling than the seizure episodes.[10]
In this study, we sought to determine the prevalence of depression in patients with epilepsy in South East Nigeria and the factors, if any, which may be associated with it.
Materials and Methods
This was a cross-sectional, descriptive, preliminary study involving epileptic patients aged 16 years and above who were attending the adult Neurology Clinic of the University of Nigeria Teaching Hospital, Enugu, from May to September 2009. The patients were selected using a table of random numbers. Informed consent was obtained from all participants. Ethical clearance was obtained from the hospital's ethical review board. Patients who were mentally subnormal or who had other neurological problems apart from epilepsy were excluded. Also excluded were the patients who had epilepsy in addition to other chronic medical conditions like hypertension, diabetes mellitus, and bronchial asthma.
Data obtained included age, gender, highest level of education, marital status, occupation, and seizure type. Depression was assessed using the Beck's Inventory of Depression (BID) and patients with depression were classified as follows: Minimal with score 0–13, mild with score 14–19, moderate with score 20–28, and severe with score 29–63. Data obtained was analyzed using Statistical Package for the Social Sciences (SPSS), version 15. Normally distributed variables were expressed as simple frequencies and percentages. Tests of significance for the discreet variables were done using chi square.
Results
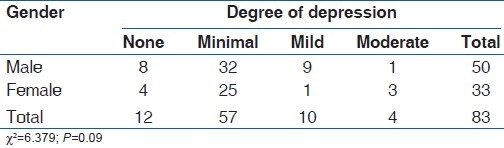
In all, 83 patients were recruited for the study, made up of 50 males and 33 females with a male: female ratio of 1.5:1. Among the males, 8 patients did not have evidence of depression, 32 had minimal depression, 9 had mild depression, and 1 patient had moderate depression. None of the patients had severe depression. Among the female patients, 4 did not have evidence of depression, 25 had minimal depression, 1 patient had mild depression, and 3 had moderate depression. None of the females had severe depression. There was no statistically significant difference between depression and gender. Table 1 shows these findings.
Table 1.
Degree of depression across the genders
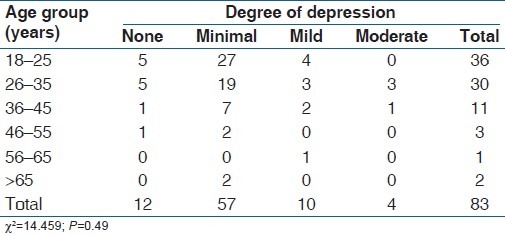
The age of the subjects ranged from 18 to 75 years, with an average of 29.87 years. Most of the patients (36, 43.4%) were in the age group 18–25 years. In this group, 5 patients did not have depression, 27 had minimal depression, 4 had mild depression, and none had moderate depression. Among the 26–35 year olds, 5 did not have depression, 19 had minimal depression, 3 each had mild and moderate depression, and none had severe depression. Among the subjects aged 36–45 years, one did not have depression, seven had minimal depression, two had mild depression, and one had moderate depression. None of the subjects in this age range had severe depression. In the patients aged 46–55 years, one did not have depression, two had minimal depression, while no patient had mild, moderate, or severe depression. Among the subjects within the 56–65 years age group, one patient had mild depression and none had minimal or moderate depression. In patients aged ≥65years, only two patients had minimal depression. There was no significant difference between age range and degree of depression (P=0.49). This is further illustrated in Table 2.
Table 2.
Age groups and levels of depression
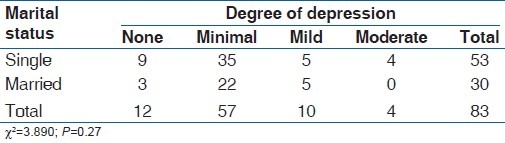
In the study, 53 (64%) subjects were single while 30 (36%) were married. Among the single subjects, 9 did not have depression, 35 had minimal depression, 5 had mild depression, while 4 had moderate depression. Among the married subjects, 3 did not have depression, 22 had minimal depression, and 5 had mild depression. None of the subjects had severe depression. There was no significant difference between marital status and degree of depression (P=0.27). This is shown in Table 3.
Table 3.
Relationship between marital status and degree of depression
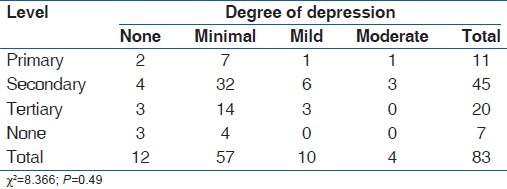
In terms of level of educational attainment, 7 patients were unschooled, while 11, 45, and 20 patients had primary, secondary, and tertiary level education, respectively. Among those with primary education, two did not have depression; seven subjects had minimal depression while one subject each had mild and moderate depression. Out of the 45 subjects with secondary education, 4 did not have depression, 32 had minimal depression, 6 had mild depression while 3 had moderate depression. Out of the 20 subjects who had tertiary education, 3 did not have depression, 14 had minimal depression, 3 had mild depression while none had moderate depression. Of the seven subjects with no educational attainment, three did not have depression, four had minimal depression, and none had either mild or moderate depression. No significant association was found between educational attainment and degree of depression [Table 4].
Table 4.
Relationship between level of education and degree of depression
Discussion
This study found the frequency of depression among epilepsy patients in Enugu to be 85.5%. This is higher than earlier documented estimates[4–6] and may be due to the fact that this study was hospital based.
Depression was commoner in the younger age, with the age group 18–25 years accounting for 31 (43.6%) out of the total of 71 patients with depression. This is similar to reports from Benin Republic, a neighboring West African country where depression occurred in epileptics with a mean age of 32 years.[9] The reason may be because these are young people who may have encountered very early in life the burden of social stigma from epilepsy and may not be able to carry on their normal life as a result of this.
This study did not show any significant relationship between depression and age in this patient population. A similar finding was obtained in the Benin study.[9] However, Lee and co-workers in their study found that age predicted depression in people with epilepsy.[11]
There was no significant relationship between gender and depression in people with epilepsy, even though females had a higher burden of depression. This finding is similar to earlier findings from West Africa which showed that age, gender, and living environment did not significantly influence depression among patients with epilepsy even though higher frequency of depression was found in females.[9]
Equally not significant in this study was the relationship of both marital status and level of educational attainment in people with epilepsy and depression. The Benin study had the same conclusion.[9] However, Lee and colleagues found that level of stress, social support, employment status, and self-efficacy predicted depression in people with epilepsy.[11]
In epilepsy patients, factors related to seizures, such as the type of the seizure, frequency of the seizures, age of onset, the duration of the illness, whether the illness is controlled or not, the number of medications used, additional neurological deficits, psychosocial factors, and socio-demographic factors including age and gender, may be related to the development of psychopathology.[12–14] This study was unfortunately not powered to study the effect of seizure type, frequency, and control on depression.
Could there be socio-cultural, racial, genetic, or other environmental reasons to explain the seemingly different findings from these West African studies from other non-African studies in terms of factors associated with epilepsy-related depression? More large-scale, multicenter studies will be necessary to help unravel these questions.
What this study has helped to demonstrate is that a large majority of epilepsy patients in Africa could have the added morbidity of depression. Depression is amenable to effective treatment when diagnosed early and the effect of appropriate treatment could be tremendous in giving these patients a new lease of life. Equally so is the sequel to non-recognition and treatment of epilepsy-related depression, especially given the increased risk of suicidal tendency in such doubly affected individuals.
Conclusion
Depression is very common in Nigerian African epilepsy patients. If unrecognized, it could significantly affect the morbidity and mortality of such patients. Given the possibility of effective management of the condition, once diagnosed, there is a need for clinicians caring for epilepsy patients to routinely screen for depression. The use of simple bedside screening instruments may be revealing and beneficial.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Seminario NA, Farias ST, Jorgensen J, Bourgeois JA, Seyal M. Determination of prevalence of depression in an epilepsy clinic using DSM-IV based self- report questionnaire. Epilepsy Behav. 2009;15:362–6. doi: 10.1016/j.yebeh.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 2.Kanner AM. Depression in epilepsy: A review of multiple facets of their close relation. Neurol Clin. 2009;27:865–80. doi: 10.1016/j.ncl.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Adewuya AO, Oseni SB. Impact of psychiatric morbidity on parent rated quality of life in Nigerian adolescents with epilepsy. Epilepsy Behav. 2005;7:497–501. doi: 10.1016/j.yebeh.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 4.Kanner AM, Palac S. Depression in epilepsy: A common but often unrecognized co-morbid malady. Epilepsy Behav. 2000;1:37–51. doi: 10.1006/ebeh.2000.0030. [DOI] [PubMed] [Google Scholar]
- 5.Okubadejo NU, Danesi MA, Aina OF, Ojini FI, Adeyemi JD, Olorunshola DA. Prospective case – control study of interictal depression and suicidal ideation in Nigerians with epilepsy. Niger Postgrad Med J. 2007;14:204–8. [PubMed] [Google Scholar]
- 6.Boylan LS, Flint LA, Labovitz DL, Jackson SC, Starner K, Devinsky O. Depression but not epilepsy predicts quality of life in treatment resistant epilepsy. Neurology. 2004;62:258–61. doi: 10.1212/01.wnl.0000103282.62353.85. [DOI] [PubMed] [Google Scholar]
- 7.Forsgren L, Nystrom L. An incident case referent study of epileptic seizures in adults. Epilepsy Res. 1990;6:66–81. doi: 10.1016/0920-1211(90)90010-s. [DOI] [PubMed] [Google Scholar]
- 8.Hesdorffer DC, Hauser WA, Annegers JF, Cascino G. Major depression is a risk factor for seizures in older adults. Ann Neurol. 2000;47:246–9. [PubMed] [Google Scholar]
- 9.Nubukpo P, Houinato D, Preux PM, Avode G, Clement JP. Anxiety and depression among the epileptics in general population in Benin (Western Africa) Encephale. 2004;30:214–9. doi: 10.1016/s0013-7006(04)95432-2. [DOI] [PubMed] [Google Scholar]
- 10.Olley BO, Osinowo HO, Brieger WR. Psycho-educational therapy among Nigerian adult patients with epilepsy. Patient Educ Couns. 2001;42:25–33. doi: 10.1016/s0738-3991(00)00087-2. [DOI] [PubMed] [Google Scholar]
- 11.Lee SA, Lee SM, No YJ. Factors contributing to depression in patients with epilepsy. Epilepsia. 2010;51:1305–8. doi: 10.1111/j.1528-1167.2009.02387.x. [DOI] [PubMed] [Google Scholar]
- 12.Ayhan B, Savaş Y, Serap T, Gülhis D, Emine ZK. Depression and anxiety symptom severity in a group of children with epilepsy and related factors. Turk J Psych. 2006;17:165–72. [PubMed] [Google Scholar]
- 13.Davies S, Heyman I, Goodman R. A Population survey of mental health problems in children with epilepsy. Dev Med Child Neurol. 2003;45:292–5. doi: 10.1017/s0012162203000550. [DOI] [PubMed] [Google Scholar]
- 14.Mensah SA, Beavis JM, Thapar AK, Kerr M. The presence and clinical implications of depression in a community population of adults with epilepsy. Epilepsy Behav. 2006;8:213–9. doi: 10.1016/j.yebeh.2005.09.014. [DOI] [PubMed] [Google Scholar]


