Abstract
Purpose
To determine peripapillary retinal nerve fiber layer (RNFL) thickness values by three-dimensional optical coherence tomography (3D-OCT) in a normal Iranian population and to evaluate the concordance of these measurements with those obtained by the second generation of optical coherence tomography (OCT II).
Methods
In a cross-sectional observational study, 96 normal Iranian subjects 20-53 years old were enrolled. Peripapillary RNFL thickness in one randomly selected eye of each subject was measured by 3D-OCT and also by OCT II. Standard achromatic perimetry, corneal pachymetry and A-scan ultrasonographic biometry were also performed. Other study variables included age, gender, laterality (right versus left eye), refractive error, corneal diameter and disc area.
Results
Mean peripapillary RNFL thickness measured by 3D-OCT (75.50±8.38) μm was significantly less than that measured by OCT II (144.10±33.32 μm) (P<0.001). Using 3DOCT, no significant difference in peripapillary RNFL thickness was observed by gender (P=0.90) or laterality (P=0.17); RNFL thickness had no correlation with age (P=0.95), axial length (P=0.32), spherical equivalent refractive error (P=0.21), central corneal thickness (P=0.66) and disc area (P=0.31). However, a positive correlation was found between peripapillary RNFL thickness and corneal diameter (P=0.03).
Conclusion
3D-OCT seems to yield lower RNFL thickness values as compared to OCT II. It seems advisable to obtain separate baseline measurements when using different generations of OCT machines.
Keywords: Optical Coherence Tomography, Retinal Nerve Fiber Layer Thickness, Three-Dimensional Tomography
INTRODUCTION
Glaucomatous optic neuropathy is associated with accelerated apoptosis of retinal ganglion cells (RGCs) manifesting as thinning of the retinal nerve fiber layer (RNFL) and increased cupping of the optic nerve head (ONH). The diagnosis of glaucoma is currently based on the appearance of the ONH and RNFL, and standard achromatic perimetric findings.1,2 Over 60% of ocular hypertensive patients develop slowly progressive reduction in RNFL thickness , 5-6 years before the appearance of any visual field defect.3,4 Although clinical examination of the ONH is still considered to be the most sensitive method for identifying glaucomatous damage, ocular imaging technologies such as optical coherence tomography (OCT) are gaining popularity in the diagnosis of glaucoma.5–9 They enable clinicians to perform objective measurements of RNFL thickness and to obtain ONH topography.10
OCT is a high resolution imaging technology that has been widely used to evaluate RNFL thickness in patients with or without glaucoma. The device works on the principal of low coherence interferometry. Images are obtained by delivery of low coherence near infrared light (850 nm) from a superluminescent diode laser source and subsequent backscattering from the retina. RNFL thickness is measured by the number of pixels between the anterior and posterior reflections from the RNFL identified by an edge detection algorithm.10,11
Less than two decades since its introduction, OCT technology has evolved and several generations of the device such as OCT II, OCT III, and ultra high resolution/high speed OCT have been employed in the field of retinal disorders and glaucoma. One critical variable differentiating these instruments is the speed of imaging. Faster image acquisition avoids motion-induced artifacts and can yield more reproducible scans. One of the new generations of machines in this category is the 3-dimen-sional OCT (3D-OCT). Using Fourier domain instead of time domain, this instrument acquires more data in less time with higher resolution. In other words by taking advantage of internal spectrometry instead of mobile mirrors, the number of axial scans per second has increased from 400 in conventional OCT to 20,000 in 3D-OCT making the device 50–100 times faster than previous versions. With such higher number of scans the device is capable of reconstructing 3-dimensional images with point to point registration of the scanned area.12,13
This study was performed to determine the normal range of peripapillary RNFL thickness as determined by 3D-OCT in an Iranian population and to compare these values with similar measurements obtained by OCT II. We also evaluated the effect of age, gender, laterality, refractive error, axial length, central corneal thickness, corneal diameter and disc area on RNFL thickness measurements by 3D-OCT.
METHODS
This study included subjects over 18 years of age who accompanied patients in ophthalmology clinics at Labbafinejad Medical Center who were able and willing to make the required study visits. Each subject gave informed consent and the project was approved by the ethics committee of the Ophthalmic Research Center. Exclusion criteria were contraindications to pupil dilation, history of intolerance to topical anesthetics or mydriatics, previous intraocular surgery, history of any type of drug consumption, or use of photosensitizing agents during the last 14 days, best-corrected visual acuity (BCVA) less than 20/20, media opacity or any abnormal slitlamp finding, intraocular pressure (IOP)≥ 22 mmHg, any evidence of glaucoma, diabetic retinopathy, macular edema or other vitreoretinal disorders, optic nerve or RNFL abnormalities, unreliable visual fields (VF), and any reproducible VF defect.
Each subject underwent a complete ophthalmologic evaluation including refraction and BCVA measurement, slitlamp examination, IOP measurement (using Goldmann applanation tonometry) and dilated fundus examination. Threshold VF examinations were performed in all subjects using the Humphrey visual field analyzer (Carl Zeiss Meditec Inc., Dublin, USA). Axial length measurements were obtained using A-mode ultrasound biometry (US-2520, Nidek, Japan). Central corneal thickness (CCT) was determined by an ultrasonic pachymeter (Quantel Medical, Pocket, France). Corneal diameter was measured using a spectacle frame which was scaled horizontally and vertically with two plastic rulers (Fig. 1). The subjects wore the glasses and digital photographs were taken; horizontal and vertical corneal diameters were measured by another ruler on the computer screen, using the scaled frame as a reference.
Figure 1.
Scaled spectacle frame used for measuring corneal diameter.
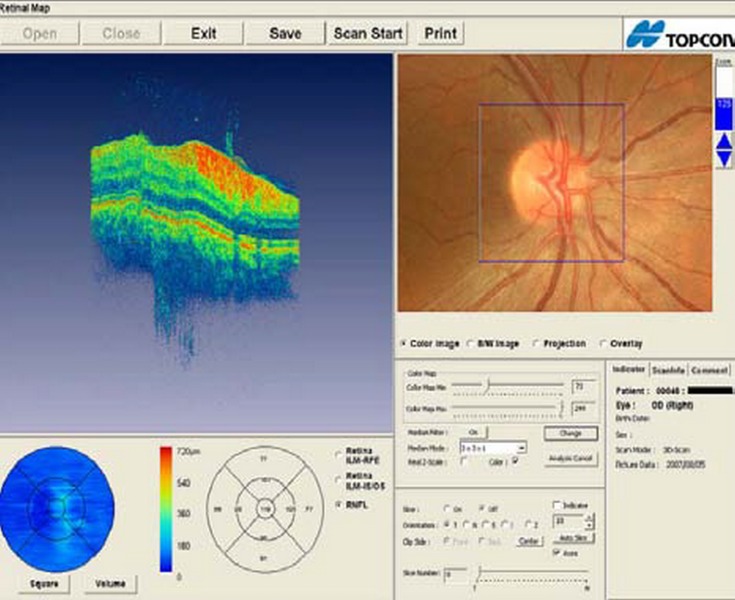
3D-OCT (Topcon Inc., Paramus, USA) and OCT II (Humphrey-Zeiss Meditec Inc., Dublin,USA) were performed in all subjects after pupil dilation to measure peripapillary RNFL thickness. The 3D-OCT peripapillary RNFL thickness (3 mm scan) printout (Fig. 2) has 3 circle scales around the optic nerve head, which include central, paracentral and peripheral circles; we used the peripheral circle for RNFL measurements. The 3.4 mm peripapillary scan mode of OCT II was used to measure peripapillary RNFL thickness. Optic disc photographs were captured from 3D-OCT images superimposing a 3x3 mm square used as a reference for disc area measurement. For this purpose, fundus photographs were enlarged on a computer screen and the optic disc boundary was traced with a mouse and a contour line was depicted by a computer engineer unaware of the results of RNFL measurements under supervision by an ophthalmologist. Using the 3x3 mm quadrangle as the reference, the area within this contour line was measured using AutoCAD 2007 software and the mean of 3 measurements was recorded. When the edge of the optic nerve was indistinct or uncertain because of anatomic variations such as tilting of the optic nerve or a broad scleral ring, the optic disc area was recorded as the median value of three measurements considered as most representative and reproducible.
Figure 2.
The scan type and printout of 3-dimensional optical coherence tomography used in the study.
SPSS-15 software was used for statistical analysis. Quantitative variables were described using mean and standard deviations or their relevant 95% confidence intervals (CI), whereas percentages and 95% CI were used to describe qualitative data. Univariate analysis such as t-test, analysis of variances and Pearson’s correlation coefficient were employed to determine the correlation between explanatory variables and RNFL thickness individually. A general linear model was utilized to evaluate the correlation between explanatory variables and RNFL thickness simultaneously while controlling for potential confounders.
RESULTS
Overall, 96 eyes (including equal numbers of right and left eyes) of 96 normal subjects including 49 (51%) men and 47 (49%) women with mean age of 32.9±9 (range, 20–53) years were enrolled in this study. Table 1 summarizes mean spherical equivalent (SE) refractive error, axial length, CCT, corneal diameter (average of horizontal and vertical) and optic disc area.
Table 1.
Basic characteristics
| Mean±SD | 95% CI | Range | |
|---|---|---|---|
| Age (years) | 33.0±9.0 | 31.1 to 34.8 | 20 to 53 |
| Spherical equivalent (diopters) | −0.3±0.7 | −0.5 to 0.2 | −3.0 to +1.6 |
| Axial length (mm) | 22.7±0.9 | 22.5 to 22.9 | 21.1 to 25.3 |
| Central corneal thickness (μm) | 528.0±35.1 | 520.9 to 535.1 | 442.0 to 649.0 |
| Corneal diameter (mm) | 10.9±0.2 | 10.8 to 11.0 | 10.1 to 11.5 |
| Disc area (mm2) | 2.6±0.5 | 2.5 to 2.7 | 1.4 to 4.0 |
SD, standard deviation; CI, confidence interval.
Using 3D-OCT mean peripapillary RNFL thickness was 75.50±8.38 μm and mean RNFL volume was 0.100±0.012 μm3. No difference in peripapillary RNFL thickness was observed between right and left eyes (P=0.17) or male and female subjects (P=0.90). There was no significant difference between men and women in terms of peripapillary RNFL volume (P=0.61, Table 2).
Table 2.
Mean retinal nerve fiber layer thickness and volume by gender using 3D-OCT
| RNFL | Gender | Mean±SD | 95% CI | Range |
|---|---|---|---|---|
| Thickness (Μm) | Male | 75.4±8.7 | 72.9 to 77.9 | 57.3 to 92.5 |
| Female | 75.6±8.1 | 73.2 to 78.0 | 58.3 to 93.3 | |
| Total | 75.5±8.4 | 73.8 to 77.2 | 57.3 to 93.3 | |
|
| ||||
| Volume (mm3) | Male | 0.10±0.01 | 0.096 to 0.103 | 0.08 to 0.12 |
| Female | 0.10±0.01 | 0.097 to 0.104 | 0.08 to 0.12 | |
| Total | 0.10±0.01 | 0.097 to 0.102 | 0.08 to 0.12 | |
3D-OCT, 3-dimensional optical coherence tomography; RNFL, retinal nerve fiber layer; SD, standard deviation; CI, confidence interval.
Mean peripapillary RNFL thickness was 75.50±8.38 μm using 3D-OCT and 144.10+33.32 μm using OCT II (P<0.001). Peripapillary RNFL thickness in different quadrants using 3D-OCT in descending order included: inferior (80.5 μm), superior (78.5 μm), nasal (77.1 μm), and temporal (63.2 μm) which follows the"ISNT rule". Peripapillary RNFL thickness in different quadrants using OCT II in descending order included: inferior (169.1 μm), superior (167.0 μm), nasal (129.4 μm), and temporal (107.7 μm) which also follows the "ISNT rule" (Table 3).
Table 3.
Retinal nerve fiber layer thickness and volume in different quadrants
| Quadrants | OCT II | 3D-OCT | ||||
|---|---|---|---|---|---|---|
| RNFL thickness (μm) | RNFL thickness (μm) | RNFL volume mm3 | ||||
| Mean±SD | 95% CI | Mean±SD | 95% CI | Mean±SD | 95% CI | |
| Inferior | 169.1±32.2 | 162.1–176.1 | 80.5±10.5 | 78.2–82.7 | 0.11±0.01 | 0.105–0.11 |
| Superior | 167.0±30.8 | 160.3–173.6 | 78.5±10.1 | 76.4–80.7 | 0.10±0.01 | 0.10–0.11 |
| Nasal | 129.4±37.6 | 121.2–137.6 | 77.1±13.9 | 74.1–80.1 | 0.10±0.02 | 0.10–0.11 |
| Temporal | 107.7±40.7 | 98.8–116.5 | 63.2±9.7 | 61.1–65.3 | 0.08±0.01 | 0.080–0.09 |
OCT, optical coherence tomography; 3D-OCT, 3-dimensional OCT; RNFL, retinal nerve fiber layer; SD, standard deviation; CI, confidence interval.
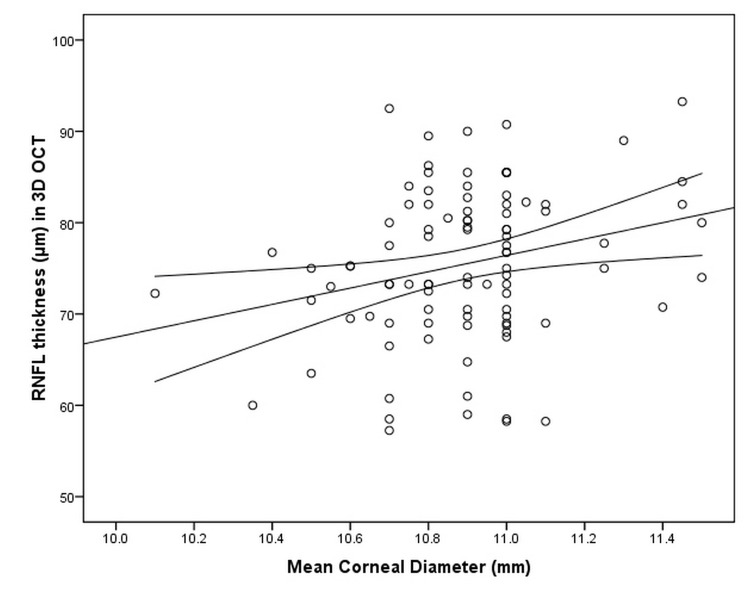
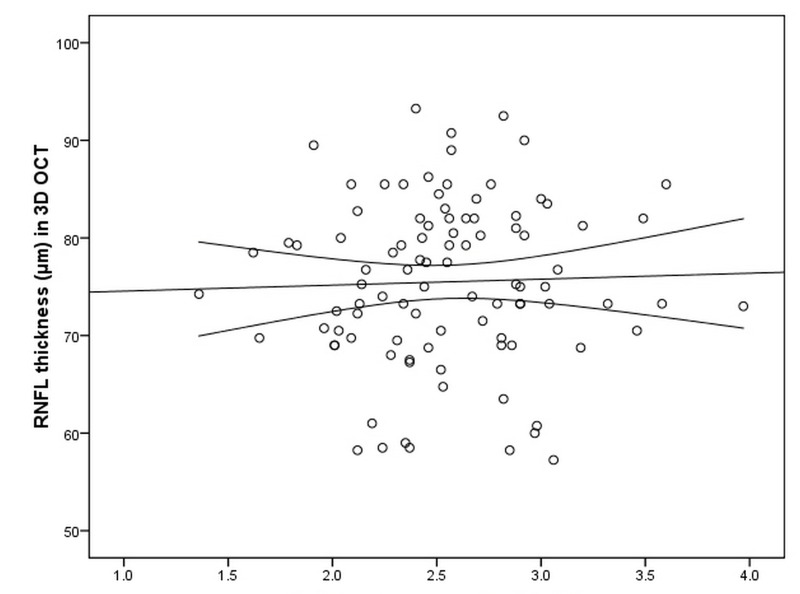
Peripapillary RNFL thickness measured by 3D-OCT had no correlation with age (P=0.95), axial length (P=0.32), SE (P=0.21), CCT (P=0.66) and disc area (P=0.31) but had a positive correlation with mean corneal diameter (P=0.03) such that with each millimeter increase in corneal diameter, RNFL thickness was thicker by approximately 8.11 μm (95% CI; 0.67 to 15.55) (Table 4,Fig. 3). There was a trend for mean RNFL thickness to increase with increasing optic disc area (r=2.02), however this was not statistically significant (P=0.31); for every square millimeter increase in optic disc area, mean RNFL thickness increased by approximately 2.02 μm. (95%CI; −1.88 to 5.93) (Fig. 4).
Table 4.
Multiple linear regression analysis of demographic and clinical variables in relation to mean retinal nerve fiber layer thickness measured by 3D-OCT
| Variable | Regression coefficient | Standard error | 95%CI | P-Value |
|---|---|---|---|---|
| Sex (male) | −0.24 | 1.77 | −3.75 to 3.27 | 0.893 |
| Eye (OD) | 2.35 | 1.70 | −1.04 to 5.73 | 0.171 |
| Age | −0.01 | 0.10 | −0.21 to 0.19 | 0.952 |
| Spherical equivalent | −1.56 | 1.24 | −4.01 to 0.89 | 0.211 |
| Axial length | −0.96 | 0.97 | −2.88 to 0.96 | 0.323 |
| Central corneal thickness | 0.01 | 0.03 | −0.04 to 0.06 | 0.658 |
| Corneal diameter | 8.11 | 3.74 | 0.67 to 15.55 | 0.033 |
| Disc area | 2.02 | 1.96 | −1.88 to 5.93 | 0.306 |
3D-OCT, 3-dimensional optical coherence tomography; CI, confidence interval; OD, right eye.
Figure 3.
Correlation between peripapillary retinal nerve fiber layer (RNFL) thickness and mean corneal diameter, plotted as a continuous variable.
Figure 4.
Correlation between retinal nerve fiber layer (RNFL) thickness and optic disc area.
DISCUSSION
This study on a normal Iranian population revealed that mean peripapillary RNFL thickness measured by 3D-OCT was significantly less than that obtained by OCT II (75.50±8.38 vs 144.10±33.32 μm, P<0.001). Table 5 summarizes other studies reporting mean peripapillary RNFL thickness in normal populations from different parts of the world using conventionalOCT (versions II or III).14–19 Average RNFL thickness in these studies ranges from 100 to 138 μm; all greater than the average value determined by 3D-OCT in our study. In another study on an Iranian population by Nilforoushan et al18 who measured RNFL thickness by OCT II, mean RNFL thickness was 137.56±16.79 μm which is comparable to our findings by OCT II (144.10±33.32 μm) but much greater than our 3D-OCT measurements.
Table 5.
Mean peripapillary RNFL thickness values in different studies
| Study | Country | Year | Number of eyes | Type of OCT | Mean RNFL thickness (μm) |
|---|---|---|---|---|---|
| Gramer et al14 | USA | 1998 | 104 | Not mentioned | 107±26 |
| Mok et al15 | Hong Kong | 2002 | 129 | Not mentioned | 120±28 |
| Varma et al16 | USA | 2003 | 312 | OCT II | 133±14 |
| Leung et al17 | China | 2004 | 107 | OCT II | 105±11 |
| Nilforoushan et al18 | Iran | 2004 | 45 | OCT II | 138±17 |
| Budenz et al19 | USA | 2007 | 328 | OCT III | 100.1±11.6 |
RNFL, retinal nerve fiber layer; OCT, optical coherence tomography.
3D-OCT uses a circular scan 3 mm in diameter, but OCT II utilizes a 3.4 mm circle; therefore one would expect that OCT II measurements be smaller. The reason for opposite findings in this study as well as other studies is not clearly understood and it remains unclear which one is more accurate. 3D-OCT is different from conventional OCT in the method of image acquisition due to utilizing an internal spectrometer instead of mobile mirrors which may be one source of differences. In a histopathological study by Jones et al,20 it was shown that conventional OCT may underestimate histological RNFL thickness by an average of 37%. Based on this study, one may assume that 3D-OCT could be farther from reality. However, tissue processing artifacts and consequent swelling should be considered as other possible causes of disparity.
This study demonstrated that RNFL thickness measured by 3D-OCT in different quadrants follows the so-called "ISNT rule" which is consistent with other studies.14–16,18,19 This sequence may be explained by the anatomical and histological structure of the eye. Due to the arcuate pattern of nerve fibers terminating in the inferior and superior poles of the optic nerve head, RNFL in these areas is thicker than nasal and temporal quadrants.3 Even with other RNFL imaging techniques such as OCT II in our study and scanning laser polarimetry in other studies, the same descending order of thickness has been shown.18,19,21,22
The current study demonstrated a weak negative correlation between peripapillary RNFL thickness and age, with a decline of approximately 0.06 micrometer in RNFL thickness per decade of age. Although this finding was not statistically significant, several other studies have reported a significant negative correlation. In a study on 100 healthy individuals, Alamouti et al22 demonstrated that both total retinal thickness and RNFL thickness significantly decreased with age with an average decrease of 0.44 μm per year. Budenz et al19 showed that RNFL thickness was significantly correlated with age; for each decade increase in age, mean RNFL decreased by approximately 2 μm. Other studies by Schuman, Gramer, Mok, and Varma have also noted a significant negative correlation between age and RNFL thickness.11,14–16 The small and statistically insignificant correlation we found between peripapillary RNFL and age may be due to the younger population in our study (mean age of 33; range, 20–53 years) as compared to other studies which focused on older people (mostly over 40 years of age).11,14,15,18,19,22 On the other hand, there are studies which have demonstrated no decrease in RNFL thickness with ageing. Repka and Quigly23 reported no decrease in RNFL thickness in older subjects and believed that this is similar to a stable cup/disc ratio throughout life. Nilforoushan and Ahadi18 also found no significant correlation between age and RNFL thickness. One histological study also demonstrated no significant correlation between age and the number of axons.23 But these types of studies typically include relatively few subjects. The large variation (7×105 to 1.4×106 fibers) in the number of RGC axons in normal individuals further complicates this correlation.23 To prove any correlation between peripapillary RNFL thickness and age, we need age-adjusted normal values for interpretation of RNFL thickness measurements.
The current study revealed no significant difference in RNFL thickness between male and female subjects which is compatible with many other reports.11,16,18,19,21 However, Wong et al24 reported significantly thicker RNFL in men suggesting their higher body mass index as the cause. We found no difference in RNFL thickness between right and left eyes which is similar to the study by Budenz et al.19 No significant correlation was found between RNFL thickness and CCT in our study which is consistent with the study by Lester and Mermoud.25
We observed no correlation between RNFL thickness and spherical equivalent refractive error which is in contrast to the study by Budenz et al19 who reported thinner RNFL in myopic eyes (0.9 μm less thickness for every diopter of myopia). In another study on Iranian subjects, Nilforoushan et al18 reported a similar correlation between RNFL thickness and myopia which was not statistically significant. The diversity of results reported by different studies could be due to differences in the range of refractive errors included; in the current study for instance, the range of refractive errors was narrow, from −3.00 to +1.63. We observed an inverse but statistically insignificant correlation between axial length (AL) and RNFL thickness, for every millimeter increase in AL, RNFL thickness decreased by approximately 0.96 μm. The corresponding figure in the study by Budenz et al19 was 2.2 μm which was also statistically significant.
Budenz et al19 reported a significant correlation between disc area and RNFL thickness such that one mm2 increase in optic disc area was associated with 3.3 μm increase in RNFL thickness. Although not significant, the corresponding figure in our study was close to the mentioned report: 2.02 μm increase in RNFL thickness for each mm2 increase in optic disc area. Savini et al10 have also shown that optic nerve fiber counts increase with ONH size. However, one may argue that the thicker RNFLin large optic nerves may be due to the shorter distance between the circular OCT scan and the optic disc. If a fixed diameter circular scan is employed, which is usually the case, the distance between the scan and the optic nerve head margin will obviously be reduced in the presence of a large ONH, thereby overestimating RNFL thickness.
In conclusion, this study on a normal group of Iranian individuals revealed that mean peripapillary RNFL thickness measured by 3D-OCT was 75.5±8.38 μm which is much less than the corresponding figure of 144.10± 33.32 μm measured by OCT II in the same population. It seems that peripapillary RNFL thickness measurements by 3D-OCT are thinner compared to measurements by older generations of OCT, therefore one should consider obtaining separate baseline measurements when using different imaging instruments. Further studies are warranted to determine which measurement is more accurate.
REFERENCES
- 1.Coleman AL. Epidemiology of glaucoma. In: Morrison JC, Pollack IP. Glaucoma: science and practice. New York: hieme; 2003. pp. 2–11. [Google Scholar]
- 2.Kanski JK, Callister JA, Salmon JF. A colour manual of diagnosis and treatment of glaucoma. 2nd ed. Oxford: Butterword, Heinemani; 1996. [Google Scholar]
- 3.Sommer A, Katz J, Quigley HA, Miller NR, Robin AL, Richter RC, et al. Clinically detectable nerve fiber atrophy precedes the onset of glaucomatous field loss. Arch Ophthalmol. 1991;109:77–83. doi: 10.1001/archopht.1991.01080010079037. [DOI] [PubMed] [Google Scholar]
- 4.Caprioli , Ortiz-Colberg R, Miller JM, Tressler C. Measurements of peripapillary nerve fiber layer contour in glaucoma. Am J Ophthalmol. 1989;108:404–413. doi: 10.1016/s0002-9394(14)73308-2. [DOI] [PubMed] [Google Scholar]
- 5.Pieroth L, Schumon JS, Hertzmark E, Hee MR, Wilkins JR, Coker J, et al. Evaluation of focal defects of the nerve fiber layer using optical coherence tomography. Ophthalmology. 1999;106:570–579. doi: 10.1016/s0161-6420(99)90118-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zangwill LM, Bowd C, Berry CC, Williams J, Blumenthal EZ, Sanchez-Galeana CA, et al. Discriminating between normal and glaucomatous eyes using the Heidelberg Retina Tomograph, GDx Nerve Fiber Analyzer, and Optical Coherence Tomograph. Arch Ophthalmol. 2001;119:985–993. doi: 10.1001/archopht.119.7.985. [DOI] [PubMed] [Google Scholar]
- 7.Schuman JS, Pedut-Kloizman T, Hertzmark E, Hee MR, Wilkins JR, Coker JG, et al. Reproducibility of nerve fiber layer thickness measurement using optical coherence tomography. Ophthalmology. 1996;103:1889–1898. doi: 10.1016/s0161-6420(96)30410-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guedes V, Schuman JS, Hertzmark E, Wollstein G, Correnti A, Mancini R, et al. Optical coherence tomography measurement of macular and nerve fiber layer thickness in normal and glaucomatous human eyes. Ophthalmology. 2003;110:177–189. doi: 10.1016/s0161-6420(02)01564-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greaney MJ, Hoffman DC, Garway-Heath DF, Nakla M, Coleman AL, Caprioli J. Comparison of optic nerve imaging methods to distinguish normal eyes from those with glaucoma. Invest Ophthalmol Vis Sci. 2002;43:140–145. [PubMed] [Google Scholar]
- 10.Savini G, Zanini M, Carelli V, Sadun AA, Ross-Cisneros FN, Barboni P. Correlation between retinal nerve fiber layer thickness and optic nerve head size: an optical coherence tomography study. Br J Ophthalmol. 2005;89:489–492. doi: 10.1136/bjo.2004.052498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schuman JS, Hee MR, Puliafito CA, Wong C, Pedut-Kloizman T, Lin CP, et al. Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch Ophthalmol. 1995;113:586–596. doi: 10.1001/archopht.1995.01100050054031. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg L. 3-D OCT 1000: A Fourier-domain system acquires more data in less time. 2007 [Google Scholar]
- 13.Topcon Great Britain Ltd. Topcon 3-D OCT 1000 specifications. 2007 [Google Scholar]
- 14.Gramer E, Tausch M. Measurement of the retinal nerve fiber layer thickness in clinical routine. Curr Opin Ophthalmol. 1998;9:77–87. doi: 10.1097/00055735-199804000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Mok KH, Lee VW, So KF. Retinal nerve fiber layer measurement of the Hong Kong Chinese population by optical coherence tomography. J Glaucoma. 2002;11:481–483. doi: 10.1097/00061198-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Varma R, Bazzaz S, Lai M. Optical tomography-measured retinal nerve fiber layer thickness in normal Latinos. Invest Ophthalmol Vis Sci. 2003;44:3369–3373. doi: 10.1167/iovs.02-0975. [DOI] [PubMed] [Google Scholar]
- 17.Leung CK, Yung WH, Ng AC, Woo J, Tsang MK, Tse KK. Evaluation of scanning resolution on retinal nerve fiber layer measurement using optical coherence tomography in normal and glaucomatous eyes. J Glaucoma. 2004;13:479–485. doi: 10.1097/01.ijg.0000138205.99424.24. [DOI] [PubMed] [Google Scholar]
- 18.Nilforoushan N, Ahadi M. Optical coherence tomography measurement of peripapillary retinal nerve fiber layer thickness in normal human eyes. Bina J Ophthalmol. 2005;10:473–480. [Google Scholar]
- 19.Budenz DL, Anderson DR, Varma R, Schuman J, Cantor L, Savell J, et al. Determinants of normal retinal nerve fiber layer thickness measured by Stratus OCT. Ophthalmology. 2007;114:1046–1052. doi: 10.1016/j.ophtha.2006.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones AL, Sheen NJ, North RV, Morgan JE. The Humphrey optical coherence tomography scanner: quantitative analysis and reproducibility study of the normal human retinal nerve fibre layer. Br J Ophthalmol. 2001;85:673–677. doi: 10.1136/bjo.85.6.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bowd C, Zangwill LM, Blumenthal EZ, Vasile C, Boehm AG, Gokhale PA, et al. Imaging of the optic disc and retinal nerve fiber layer: the effects of age, optic disc area, refractive error, and gender. J Opt Soc Am A Opt Image Sci Vis. 2002;19:197–207. doi: 10.1364/josaa.19.000197. [DOI] [PubMed] [Google Scholar]
- 22.Alamouti B, Funk J. Retinal thickness decreaseswith age: an OCT study. Br J Ophthalmol. 2003;87:899–901. doi: 10.1136/bjo.87.7.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Repka MX, Quigley HA. The effect of age on normal human optic nerve fiber number and diameter. Ophthalmology. 1989;96:26–32. doi: 10.1016/s0161-6420(89)32928-9. [DOI] [PubMed] [Google Scholar]
- 24.Wong AC, Chan CW, Hui SP. Relationship of gender, body mass index, and axial length with central retinal thickness using optical coherence tomography. Eye. 2005;19:292–297. doi: 10.1038/sj.eye.6701466. [DOI] [PubMed] [Google Scholar]
- 25.Lester M, Mermoud A. Retinal nerve fiber layer and physiological central corneal thickness. J Glaucoma. 2001;10:158–162. doi: 10.1097/00061198-200106000-00003. [DOI] [PubMed] [Google Scholar]