Abstract
Objectives
To evaluate the association between stress-induced hyperglycemia and infectious complications in non-diabetic orthopaedic trauma patients admitted to the Intensive Care Unit (ICU).
Design
Retrospective review.
Setting
Academic Level-1 Trauma Center.
Patients
One hundred and eighty-seven consecutive trauma patients with isolated orthopaedic injuries.
Intervention
Blood glucose values during initial hospitalization were evaluated. The admission blood glucose (BG) and Hyperglycemic Index (HGI) were determined for each patient.
Main Outcome Measures
Perioperative infectious complications: pneumonia, urinary tract infection (UTI), surgical-site infection (SSI), sepsis.
Results
An average of 21.5 BG values was obtained for each patient. Mean ICU and hospital length of stay was 4.0±4.9 and 10.0±8.1 days, respectively. Infections were recorded in 43/187 patients (23.0%) and SSI’s specifically documented in 16 patients (8.6%). Open fractures were not associated with SSI (8/83, 9.6% vs. 8/104, 7.7%). There was no difference in admission BG or HGI and infection. However, there was a significant difference in HGI when considering SSI alone (2.1±1.7 vs. 1.2±1.1). Patients with an SSI received a greater amount of blood transfusions (14.9±12.1 vs. 4.9±7.6). No patient was diagnosed with a separate infection (i.e. pneumonia, UTI, bacteremia) prior to SSI. There was no significant difference in Injury Severity Score among patients with an SSI (11.1±4.0 vs. 9.6±3.0). Multivariable regression testing with HGI as a continuous variable demonstrated a significant relationship (OR: 1.8, 95% CI: 1.3–2.5) with SSI after adjusting for blood transfusions (OR: 1.1, 95% CI: 1.1–1.2).
Conclusions
Stress-induced hyperglycemia demonstrated a significant independent association with SSI’s in non-diabetic orthopaedic trauma patients who were admitted to the ICU.
Keywords: hyperglycemia, orthopaedic trauma, surgical site infection, non-diabetic, intensive care unit
Introduction
Acute hyperglycemia following traumatic injury is common. Studies have shown that 20–30% of trauma patients present following injury with blood glucose values greater than 200 mg/dL, and that a majority of patients demonstrate values greater than 150 mg/dL.1 The immediate physiologic response to traumatic injury is thought to result in certain autonomic and endocrine adaptations, such as increased catecholamine and glycogen levels, which may be deleterious to immune function.2–5 Elevated blood glucose at admission and persistent hyperglycemia are risk factors for infectious complications, longer hospital and intensive care unit (ICU) length of stay, and increased risk of death.6 Recent investigations have demonstrated that this significant relationship is independent from a history of diabetes mellitus.7, 8
Based on the results from the general trauma literature, 1, 9–13 it would appear intuitive that the relationship of acute hyperglycemia and outcome in orthopaedic trauma patients would be of significant value to the treating surgeon. Karunakar and Staples demonstrated that stress-induced hyperglycemia in a population of non-diabetic orthopaedic trauma patients was a significant risk factor for infectious complications.14 However, there has been little discussion in the orthopaedic trauma literature regarding the relationship of acute hyperglycemia and potential complications following musculoskeletal injury. The purpose of this study was to evaluate the association of stress-induced hyperglycemia and infectious complications in a population of non-diabetic orthopaedic trauma patients who were admitted to the ICU.
Patients and Methods
We performed a retrospective investigation at a university-based Level-1 trauma center. Following approval by the Institutional Review Board, the institution’s Trauma Registry of the American College of Surgeons (TRACS) database was queried from a period of January 1, 2004 through October 1, 2009 to identify patients admitted with isolated orthopaedic injuries requiring acute operative intervention. Baseline demographic information, medical co-morbidities, injury characteristics, hospital and ICU length of stay (LOS) were obtained from the database. Inclusion criteria were age ≥18 years, isolated orthopedic injuries, ICU stay≥1 day, and a pelvis and/or extremity Abbreviated Injury Scale (AIS) score ≥2. Patients with diabetes mellitus, an AIS score in any other body region other than pelvis and/or extremity, or a history of corticosteroid use were excluded. Because hemoglobin A1C was not routinely obtained on every patient during the study period, patients with occult diabetes mellitus were included in the study cohort.
Patient-specific variables identified from the TRACS database included age, sex, race, medical co-morbidities, history of recent tobacco use, Injury Severity Score (ISS), units of blood transfusion, open fractures, and acute renal failure. The total number of medical co-morbidities for each patient was calculated and included coronary artery disease, hypertension, chronic obstructive pulmonary disease, rheumatoid arthritis, and alcohol abuse. ISS was calculated as defined by Baker et al.15 as the sum of the squares of the highest AIS scores in each of the most severely injured body regions. Open fractures were documented according to the Gustilo and Anderson classification system and were determined by review of the initial operative report describing the degree of injury to the open wound.16
During the study period, institutional protocol required that prophylactic antibiotics, consisting of a first generation cephalosporin, or clindamycin for penicillin -sensitive patients, begin within 30 minutes prior to surgical incision and be discontinued within 24 hours postoperatively for all closed fractures. Patients with open fractures received a first generation cephalosporin or vancomycin, with the addition of levaquin or ceftriaxone for open Type III fractures, upon admission to the emergency department. Open fractures were thoroughly irrigated and debrided of devitalized tissue in the operating room within 24 hours of admission. Subsequently, further irrigation and debridement was repeated at the discretion of the treating surgeon until a clean soft tissue bed was obtained. Antibiotics were discontinued 24 hours after definitive wound closure in patients with open fractures. Tetanus prophylaxis was administered in the emergency department, as necessary.
All blood glucose (BG) values were prospectively recorded in the patient’s electronic medical record and included both fingerstick and serum levels. Fingerstick glucose measurements were performed by trained nurses using the SureStep® Pro Professional Blood Glucose Monitoring System (OneTouch®, Lifescan, Inc., Milpitas, CA). Enteral nutrition was initiated as soon as possible. We were unable to determine whether patients had recent oral intake prior to the laboratory draw, therefore all glucose values were considered random.
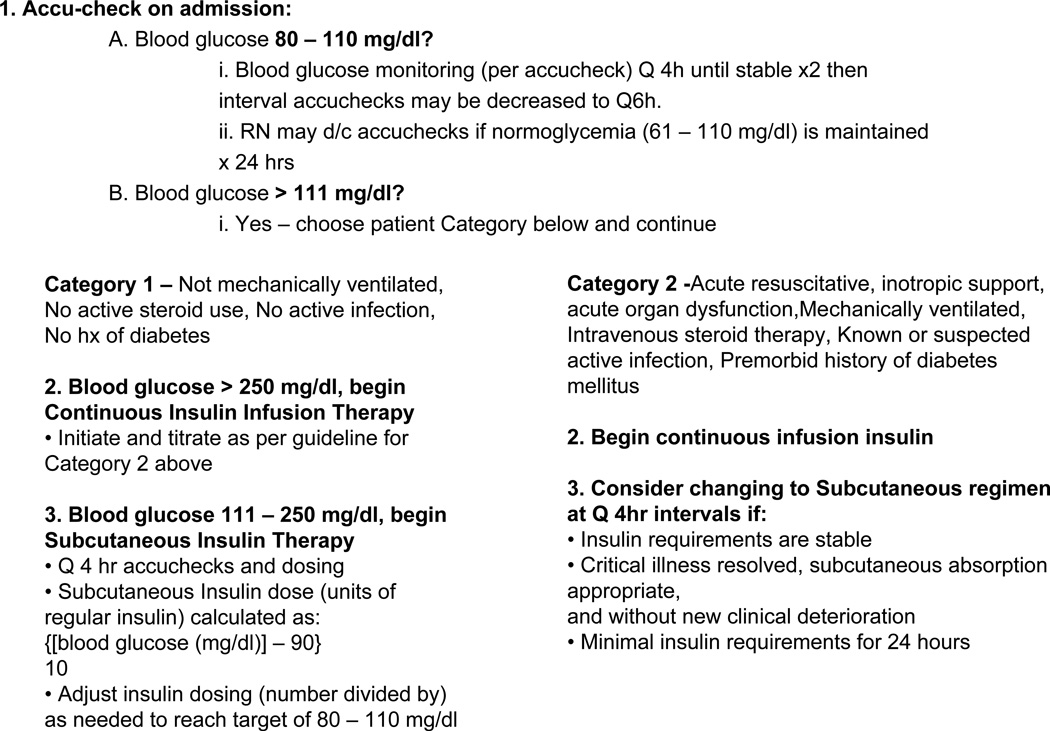
Glycemic control in the ICU consisted of a protocol with a target BG of 80–110 milligrams/deciliter (mg/dL). BG values were obtained by fingerstick and insulin administration was determined by computerized protocol-driven management algorithms (Figure 1)12. Patients who remained on the general surgery trauma service after discharge from the ICU were managed by similarly published guidelines (if blood glucose >110 mg/dL administer subcutaneous insulin according to the formula: insulin= (BG-100)/10; and adjust denominator to reach target 80–110 mg/dL). However, in certain instances patients with isolated musculoskeletal injuries were transferred to the orthopaedic trauma service for the remainder of the hospitalization following discharge from the ICU. There was no protocol for the orthopaedic trauma service during the investigation period for routine BG monitoring and glycemic control. In this scenario, a majority of glucose values were gathered from basic metabolic panel profiles, which included serum BG laboratories, and were obtained at the discretion of the attending orthopaedic surgeon.
Figure 1.
Definition of hyperglycemia
Hyperglycemia was defined in multiple ways. Previous literature has considered admission BG as a predictor of outcome following trauma.9, 10 BG values obtained in the emergency department at initial presentation were evaluated for each patient. Secondly, we defined hyperglycemia as more than 1 random blood glucose level ≥ 200 mg/dL. Thirdly, we used the Hyperglycemic Index (HGI) to describe multiple glucose measurements taken at irregular sampling intervals over a prolonged period of time. The index represents the mean glucose level above 108 mg/dL and yields a better estimate of overall glucose control than a single value at admission or the highest value during the day.17, 18 To calculate the HGI, the area under the curve of all glucose values over the entire hospital stay is plotted. HGI is independent of hospital LOS, and is expressed as millimoles/liter (mmol/L), with the normal glucose range at a cutoff of 6.0, the equivalent of 108 mg/dL. The HGI for each patient in our investigation was calculated. We also considered an HGI >1.72 (equivalent to 139 mg/dL) as a potential marker of stress-induced hyperglycemia. Blood glucose values obtained after the diagnosis of infection (including pneumonia, urinary tract infection (UTI), sepsis, or surgical-site infection) were excluded from analysis, in order to eliminate potential bias that hyperglycemia was a result of the infection rather than a contributing risk factor.
Definition of outcomes
Peri-operative infectious complications were categorized as pneumonia, urinary tract infection (UTI), sepsis, and surgical site infections. Pneumonia was considered in the presence of fever, leukocytosis, chest radiograph with a pneumonic infiltrate, Gram stain of sputum with a predominant organism, and a quantitative sputum culture via bronchoalveolar lavage demonstrating a pathogen ≥ 105 colony forming units per milliliter. UTI was documented when a clean voided or catheter urine specimen that was leukocyte esterase or nitrate-positive and demonstrated ≥ 10 white blood cells per high powered field. Sepsis was defined as a temperature ≥39°C, white blood cell count > 10,000 per cubic millimeter, and positive blood cultures. Surgical-site infection was defined as any case that required reoperation for an infection at the site of the index operation and was confirmed by the presence of either positive intra-operative cultures, pathology specimens with microbiologic pathogens, or visible gross purulence at the operative site. Superficial infections requiring only oral or topical antibiotics were not considered.
Statistical Analysis
Normally distributed continuous variables were summarized by reporting the mean and standard deviation and compared using Analysis of Variance (ANOVA) testing. Continuous variables that were not normally distributed were presented by reporting the median and standard deviation (SD) and compared using the Kruskal Wallis test. Differences in proportions were compared using a χ2 test, and reported as percent frequency. Multivariable logistic regression modeling was constructed to determine the association of hyperglycemia on the risk of surgical-site infection, adjusting for potential confounding variables. Results are reported as the odds ratio (OR) and 95% confidence interval (CI). Statistical analysis was conducted using STATA version 11.0 (Stata Corp, College Station, TX). A two-sided p value of <0.05 indicated statistical significance.
Results
One hundred and eighty-seven consecutive patients were identified for study inclusion. Four-thousand and eighteen BG values were collected and the mean number of values for each patient was 21.5 (SD: 28.8, median: 12). On average each patient had at least 2 BG values obtained daily.
Population demographics and injury characteristics are described in Table 1. Orthopaedic injuries included 62 upper extremity injuries, 36 pelvic or acetabular fractures, 86 femur fractures, 56 tibia fractures, and 20 foot injuries. The most frequent co-morbidity was hypertension (56/187, 30.0%); and the mean number of co-morbidities per patient was 0.7 (SD: 0.9, median: 0). Average BG at hospital admission was 140.5 ± 45.0 mg/dL and 33/187 patients (17.6%) had 2 or more BG values ≥200 mg/dL during the entire hospital stay. Mean HGI was 1.2±1.2 and 41/187 patients (22.0%) had an HGI>1.72.
Table 1.
Baseline Demographics and Injury Characteristics
| N=187 | ||
|---|---|---|
| Age, mn (SD) | 47.7 (23.2) | |
| Male Sex, n (%) | 121 (67.7) | |
| Race, n (%) | ||
| White | 150 (80.2) | |
| Non-white | 37 (19.8) | |
| Number of co-morbidities, mn (SD) | 0.7 (0.9) | |
| ISS, mn (SD) | 9.8 (3.1) | |
| ICU days, mn (SD) | 4.0 (4.9) | |
| Hospital days, mn (SD) | 10.0 (8.1) | |
| Open fracture, n (%) | 83 (44.4) | |
| Type I | 6 (7.2) | |
| Type II | 13 (15.7) | |
| Type IIIA | 37 (44.6) | |
| Type IIIB | 9 (10.8) | |
| Type IIIC | 18 (21.7) | |
| Blood Transfused, mn (SD) | 5.7 (8.5) | |
| Admission BG (mg/dL), mn (SD) | 140.5 (45.0) | |
| More than 1 BG ≥200 mg/dL, n (%) | 33 (17.6) | |
| HGI, mn (SD) | 1.2 (1.2) | |
| HGI >1.72, n (%) | 41 (21.9) | |
Results reported as mean (mn) and Standard Deviation (SD), or frequency (n) and percentage (%).
ISS: Injury Severity Score; ICU: Intensive Care Unit; BG: Blood Glucose; mg/dL: milligrams/deciliter; HGI: Hyperglycemic Index
Of the entire study population, there were 51 peri-operative infectious complications in 43 patients, consisting of 22 pneumonia, 7 UTI, 6 sepsis, and 16 surgical-site infections, for an overall infection rate of 23.0%. Five patients with a surgical-site infection had wound cultures which were positive for methicillin-resistant Staphylococcus aureus. Patients with an infectious complication were older (55.4, SD: 21.8 years vs. 45.4, SD: 23.1 years; p=0.006) and received greater amounts of blood (9.1, SD: 9.4 units vs. 4.7, SD: 8.0 units; p=0.0001). Mean ISS was greater, but not clinically significant, in patients with an infection (10.6, SD: 3.7 vs. 9.5, SD: 2.8; p=0.03). There were no differences in admission BG (p=0.35), 2 BG values ≥ 200 mg/dL (p=0.10), or HGI (p=0.08) and the presence of an infection. However, when surgical-site infections were considered alone there was a significant difference in HGI (2.1, SD: 1.7 vs. 1.2, SD: 1.1; p=0.006). There was no difference in admission BG (p=0.65) or 2 BG ≥200 mg/dL (p=0.21) and surgical-site infection. When evaluated separately from surgical-site infections, there was no significant difference between HGI and other infectious complications (1.2±0.9 vs. 1.3±1.2, p=0.67).
The overall rate of surgical-site infection was 16/187 (8.6%). No patient with a surgical-site infection had a prior infection (i.e. pneumonia, UTI, or bacteremia). There were no differences in age, race, history of tobacco use, or ISS and the presence of a surgical-site infection (Table 2). Male patients were significantly more likely to have a surgical-site infection; however, male gender was not associated with HGI (1.2±1.3 vs. 1.3±1.4, p=0.61). Eighty-three patients had open fractures: 9 Type I, 13 Type II, 37 Type IIIA, 9 Type IIIB, and 18 Type IIIC. Open fractures were not more likely to develop a surgical-site infection (8/83, 9.6% vs. 8/104, 7.7%; p=0.64) and all infections in open fractures occurred in Type III fractures: 3/34, 8.8% Type IIIA; 1/9, 11.1% Type IIIB; and 4/18, 22.2% Type IIIC). Of the 41 patients with an HGI >1.72, eight patients (19.5%) developed a surgical-site infection (p=0.005). The unadjusted risk for a surgical-site infection in patients with an HGI >1.72 was 4 times greater than in patients with an HGI ≤1.72 (OR: 4.2, 95% CI: 1.5–12.0). Patients with an HGI >1.72 were significantly older (57.8, SD: 22.3 years vs. 44.8, SD: 22.7 years; p=0.008), however, there were no differences in sex, number of co-morbidities, ISS, or hospital and ICU LOS (Table 3).
Table 2.
Variables by Surgical-Site Infection
| SSI (n=16) | No-SSI (n=171) | p-value | ||
|---|---|---|---|---|
| Age, mn (SD) | 41.7 (17.2) | 48.3 (23.6) | 0.38 | |
| Male Sex, n (%) | 14 (87.5) | 107 (62.6) | 0.05 | |
| Race, n (%) | 0.6 | |||
| White | 12 (75) | 138 (80.7) | ||
| Non-white | 4 (25) | 33 (19.3) | ||
| Number of co-morbidities, n (%) | 0.4 (0.6) | 0.7 (0.9) | 0.31 | |
| History tobacco use, n (%) | 0 (0) | 16 (100) | 0.2 | |
| ISS, mn (SD) | 11.1 (4.0) | 9.6 (3.0) | 0.06 | |
| ICU days, mn (SD) | 5.6 (5.3) | 3.9 (4.8) | 0.2 | |
| Acute Renal Failure, n (%) | 0 (0) | 7 (4.1) | 0.24 | |
| Open fracture, n (%) | 8 (50) | 75 (43.9) | 0.6 | |
| Blood Transfused, mn (SD) | 14.9 (12.1) | 4.9 (7.6) | <0.0001 | |
| Admission BG, mn (SD) | 135.7 (25.4) | 141.0 (46.5) | 0.7 | |
| More than 1 BG ≥200 mg/dL, n (%) | 1 (6.25) | 32 (18.7) | 0.2 | |
| HGI, mn (SD) | 2.1 (1.7) | 1.2 (1.1) | 0.006 | |
| HGI >1.72, n (%) | 8 (50) | 33 (19.3) | 0.005 | |
SSI: Surgical-Site Infection; mn: mean; SD: Standard Deviation; ISS: Injury Severity Score; ICU: Intensive Care Unit; BG: Blood Glucose; mg/dL: milligrams/deciliter; HGI: Hyperglycemic Index
Table 3.
Demographic and Injury Variables by Hyperglycemic Index >1.72
| HGI >1.72 (n=41) | HGI ≤1.72 (n=146) | p-value | ||
|---|---|---|---|---|
| Age, mn (SD) | 57.9 (22.2) | 44.8 (22.7) | 0.001 | |
| Male Sex, n (%) | 29 (70.7) | 92 (63.0) | 0.4 | |
| Race, n (%) | 0.3 | |||
| White | 35 (85.4) | 115 (78.8) | ||
| Non-white | 6 (14.6) | 31 (21.2) | ||
| Number of co-morbidities, n (%) | 0.8 (0.9) | 0.6 (0.9) | 0.4 | |
| History tobacco use, n (%) | 1 (2.4) | 16 (11.0) | 0.1 | |
| ISS, mn (SD) | 9.8 (2.5) | 9.8 (3.2) | 0.99 | |
| ICU days, mn (SD) | 5.2 (8.5) | 3.7 (3.2) | 0.09 | |
| Hospital days, mn (SD) | 11.0 (11.1) | 9.7 (7.0) | 0.4 | |
| Open fracture, n (%) | 21 (51.2) | 62 (42.5) | 0.3 | |
| Blood Transfused, mn (SD) | 5.0 (4.6) | 5.9 (9.3) | 0.6 | |
HGI: Hyperglycemic Index; mn: mean; SD: Standard Deviation; ISS: Injury Severity Score; ICU: Intensive Care Unit
A multivariable logistic regression model was constructed (Table 4) adjusting for potential confounding variables, to test the association between HGI and surgical-site infection. Variables significant by univariate analysis were considered for potential inclusion in the multivariable model. Due to the rather limited number of surgical-site infections (n=16), clinically and statistically significant continuous variables (HGI and total units of blood transfused) were inserted in the model. After adjusting for units of blood transfusion (OR: 1.1, 95% CI: 1.0–1.2), HGI remained a significant independent risk factor for surgical-site infections (OR: 1.8, 95% CI: 1.3–2.5).
Table 4.
Multivariable Logistic Regression for Risk Factors of Surgical-Site Infection
| Odds Ratio | 95% Confidence Interval | p-value | |
|---|---|---|---|
| Hyperglycemic Index | 1.8 | 1.2–2.6 | 0.001 |
| Units of Blood Transfusion | 1.1 | 1.0–1.2 | 0.001 |
Discussion
Acute hyperglycemia following traumatic injury has received significant attention in the critical care literature throughout the last decade. Yendamuri and colleagues demonstrated that admission blood glucose may represent a clinically useful predictor of mortality and infectious outcome in traumatically injured patients.9 The relative ease with which such laboratory values are obtained and the applicability to immediate bedside practice has contributed greatly to the management of critically-ill patients. Few topics have garnered as substantial of an influence in the surgical critical care community. We therefore evaluated the relationship of hyperglycemia and potential infectious complications in a population of non-diabetic orthopaedic trauma patients admitted to the ICU.
Laird and colleagues reported that more than half of trauma patients demonstrated blood glucose values greater than 150 mg/dL and that levels ≥200 mg/dL were significantly associated with infectious morbidity, longer ICU and hospital stay, and an increased risk of mortality.1 Scalea et al. demonstrated that achieving normoglycemia in the early post-traumatic period reduced infectious complications and mortality, after adjusting for potential confounding variables.19 These results, and the topic of stress-induced hyperglycemia, have also been described in orthopaedic trauma patients. Bochicchio and colleagues reported that admission blood glucose ≥200 mg/dL was an accurate predictor of postoperative infection in trauma patients who required immediate operative intervention.11 The authors commented that orthopaedic injuries were the most common indication for operative intervention in the study cohort. A subsequent investigation in orthopaedic trauma patients identified that an HGI ≥3.0 was a significant independent risk factor for post-traumatic infectious complications, after controlling for age and injury severity.14
This investigation describes a population of patients with isolated musculoskeletal injuries who were admitted to the ICU and demonstrates that a continuous measure of hyperglycemia represented an independent association with surgical-site infection, after controlling for units of blood transfusion. Previous literature has demonstrated that HGI represents a more accurate reflection of overall glycemic control in trauma patients than a single isolated glucose value or the overall mean glucose.18 Patients with a surgical-site infection had a significantly greater HGI (equivalent to 145.8 mg/dL). Hyperglycemia was also considered as a dichotomous variable by an HGI >1.72 (equivalent to 139 mg/dL), in accordance with a recent consensus statement which stated that inpatient hyperglycemia was defined as BG values above 140 mg/dL.20 The unadjusted risk for a surgical-site infection was four times greater in patients with an HGI >1.72. Furthermore, this study found no significant associations with admission blood glucose or 2 random BG values ≥200 mg/dL and surgical-site infections. A possible explanation for this finding was the implementation of a tight glycemic control protocol upon admission to the ICU, which may have attenuated the fluctuations in BG levels. This may also explain why there was no significant relationship with hyperglycemia and other in-hospital infectious complications, such as UTI, pneumonia, and sepsis; as has been suggested by Sperry and colleagues.21 An exact reason why hyperglycemia demonstrated a significant relationship with surgical-site infections and not other infectious complications is not precisely known; however, considering that the mean time to identification of surgical-site infection in our population was 14 days, whereas mean hospital stay was nearly 10 days, there may be underlying hyperglycemic pathophysiologic mechanisms which continue after operative stress and beyond hospital discharge.22
There are also several important limitations to consider. This was a retrospective investigation, which contains inherent bias. Our data was unable to provide whether patients were managed by the general surgery trauma service or the orthopaedic trauma service following ICU discharge. Throughout the study period there was no standard protocol for routine BG monitoring once patients were discharged from the ICU and transferred to the orthopaedic trauma service. We were also unable to determine the amount of insulin administered both while patients were in the ICU and at post-ICU transition. The overall number of surgical-site infections was low (n=16), for which we limited our multivariable regression analysis to clinically appropriate and continuous variables, and may contribute to Type II error.
Additional variables, or even yet undefined factors, that were not extrapolated from the data may also be confounding our results. While we identified that male patients were significantly more likely to have an infection, male gender was not associated with hyperglycemia. With regard to lack of a significant univariate association with open fractures and SSI, this finding was also reported in the recent study by Karunakar and Staples.14 While not described in the final multivariable model due to the small sample size, open fractures were tested as a potential confounder, after adjusting for HGI and blood transfusion. The results of the regression analysis were unchanged and open fractures did not represent a significant association with SSI. This should be considered with caution as it may represent an over-fit of the multivariable model. The HGI is well-described in the literature and is shown to be a better predictor of outcome than other glucose control metrics.17 However, ease of interpretation and translation of HGI values into useful bedside data in routine daily clinical care are potential drawbacks of the index.23 Last, the purpose of our investigation was to evaluate hyperglycemia in orthopaedic patients without a history of diabetes. A recent prospective study demonstrated that nearly five percent of trauma patients were diagnosed with occult diabetes mellitus by hemoglobin A1C blood levels.24 Such laboratory values are not routinely collected at our institution, and therefore, patients with occult diabetes could not be identified from this investigation.
Intense blood glucose management has received a considerable degree of attention in the critical care literature; however, application of this practice in isolated traumatic orthopaedic injuries has not been well described. It is important to consider that this study does not provide recommendations for a target range of glucose control but rather suggests that the relationship between hyperglycemia and infectious complications may significantly influence post-operative outcome in non-diabetic orthopaedic patients. Large prospective, randomized studies are necessary to further delineate the relationship of stress-induced hyperglycemia and surgical-site infections following orthopaedic surgery and implement potential therapeutic interventions.
Acknowledgments
Dr. Kauffmann is supported by an NIH training grant in Diabetes and Endocrinology: 5T32DK007061-35
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no conflict of interest, monetary or otherwise, for the duration of this study.
They have received nothing of value in return for the completion of this investigation.
All devices mentioned in this study have been approved for use by the United Sates Food and Drug Administration.
Presented as a podium presentation at the Thirty-first Annual Scientific Meeting of the Surgical Infection Society of North America, May 11–14, 2011, Palm Beach, FL; and the Twenty-seventh Annual Meeting of the Orthopaedic Trauma Association, October 12–15, 2011, San Antonio, TX.
References
- 1.Laird AM, Miller PR, Kilgo PD, et al. Relationship of early hyperglycemia to mortality in trauma patients. J Trauma. 2004;56:1058–1062. doi: 10.1097/01.ta.0000123267.39011.9f. [DOI] [PubMed] [Google Scholar]
- 2.McCowen KC, Malhotra A, Bistrian BR. Stress-induced hyperglycemia. Crit Care Clin. 2001;17:107–124. doi: 10.1016/s0749-0704(05)70154-8. [DOI] [PubMed] [Google Scholar]
- 3.Dungan KM, Braithwaite SS, Preiser JC. Stress hyperglycaemia. Lancet. 2009;373:1798–1807. doi: 10.1016/S0140-6736(09)60553-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Losser MR, Damoisel C, Payen D. Bench-to-bedside review: Glucose and stress conditions in the intensive care unit. Crit Care. 2010;14:231. doi: 10.1186/cc9100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smiley DD, Umpierrez GE. Perioperative glucose control in the diabetic or nondiabetic patient. South Med J. 2006;99:580–589. doi: 10.1097/01.smj.0000209366.91803.99. quiz 90–1. [DOI] [PubMed] [Google Scholar]
- 6.Umpierrez GE, Isaacs SD, Bazargan N, et al. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87:978–982. doi: 10.1210/jcem.87.3.8341. [DOI] [PubMed] [Google Scholar]
- 7.Ramos M, Khalpey Z, Lipsitz S, et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg. 2008;248:585–591. doi: 10.1097/SLA.0b013e31818990d1. [DOI] [PubMed] [Google Scholar]
- 8.Ata A, Lee J, Bestle SL, et al. Postoperative hyperglycemia and surgical site infection in general surgery patients. Arch Surg. 2010;145:858–864. doi: 10.1001/archsurg.2010.179. [DOI] [PubMed] [Google Scholar]
- 9.Yendamuri S, Fulda GJ, Tinkoff GH. Admission hyperglycemia as a prognostic indicator in trauma. J Trauma. 2003;55:33–38. doi: 10.1097/01.TA.0000074434.39928.72. [DOI] [PubMed] [Google Scholar]
- 10.Sung J, Bochicchio GV, Joshi M, et al. Admission hyperglycemia is predictive of outcome in critically ill trauma patients. J Trauma. 2005;59:80–83. doi: 10.1097/01.ta.0000171452.96585.84. [DOI] [PubMed] [Google Scholar]
- 11.Bochicchio GV, Salzano L, Joshi M, et al. Admission preoperative glucose is predictive of morbidity and mortality in trauma patients who require immediate operative intervention. Am Surg. 2005;71:171–174. doi: 10.1177/000313480507100215. [DOI] [PubMed] [Google Scholar]
- 12.Collier B, Diaz J, Jr, Forbes R, et al. The impact of a normoglycemic management protocol on clinical outcomes in the trauma intensive care unit. JPEN J Parenter Enteral Nutr. 2005;29:353–358. doi: 10.1177/0148607105029005353. discussion 9. [DOI] [PubMed] [Google Scholar]
- 13.Bochicchio GV, Bochicchio KM, Joshi M, et al. Acute glucose elevation is highly predictive of infection and outcome in critically injured trauma patients. Ann Surg. 2010;252:597–602. doi: 10.1097/SLA.0b013e3181f4e499. [DOI] [PubMed] [Google Scholar]
- 14.Karunakar MA, Staples KS. Does stress-induced hyperglycemia increase the risk of perioperative infectious complications in orthopaedic trauma patients? J Orthop Trauma. 2010;24:752–756. doi: 10.1097/BOT.0b013e3181d7aba5. [DOI] [PubMed] [Google Scholar]
- 15.Baker SP, O'Neill B, Haddon W, Jr, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 16.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–746. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Vogelzang M, van der Horst IC, Nijsten MW. Hyperglycaemic index as a tool to assess glucose control: a retrospective study. Crit Care. 2004;8:R122–R127. doi: 10.1186/cc2840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vogelzang M, Nijboer JM, van der Horst IC, Zijlstra F, et al. Hyperglycemia has a stronger relation with outcome in trauma patients than in other critically ill patients. J Trauma. 2006;60:873–877. doi: 10.1097/01.ta.0000195715.63978.80. discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 19.Scalea TM, Bochicchio GV, Bochicchio KM, et al. Tight glycemic control in critically injured trauma patients. Ann Surg. 2007;246:605–610. doi: 10.1097/SLA.0b013e318155a789. discussion 10–2. [DOI] [PubMed] [Google Scholar]
- 20.Moghissi ES, Korytkowski MT, DiNardo M, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Diabetes Care. 2009;32:1119–1131. doi: 10.2337/dc09-9029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sperry JL, Frankel HL, Nathens AB, et al. Characterization of persistent hyperglycemia: what does it mean postinjury? J Trauma. 2009;66:1076–1082. doi: 10.1097/TA.0b013e31817db0de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thorell A, Nygren J, Ljungqvist O. Insulin resistance: a marker of surgical stress. Curr Opin Clin Nutr Metab Care. 1999;2:69–78. doi: 10.1097/00075197-199901000-00012. [DOI] [PubMed] [Google Scholar]
- 23.Badawi O, Yeung SY, Rosenfeld BA. Evaluation of glycemic control metrics for intensive care unit populations. Am J Med Qual. 2009;24:310–320. doi: 10.1177/1062860609336366. [DOI] [PubMed] [Google Scholar]
- 24.Kopelman TR, O'Neill PJ, Kanneganti SR, et al. The relationship of plasma glucose and glycosylated hemoglobin A1C levels among nondiabetic trauma patients. J Trauma. 2008;64:30–33. doi: 10.1097/TA.0b013e318161b0ab. discussion 3–4. [DOI] [PubMed] [Google Scholar]