Abstract
Aims:
Detrusor muscle in initial transurethral resection of the bladder tumor (TURBT) may not be found in up to 50% of the cases. This study was done to assess the safety, feasibility and yield of detrusor muscle on en- bloc TURBT using a conventional electrocautery loop.
Materials and Methods:
Patients with bladder tumor of size 2-4 cm, from September 2007 to August 2010, who had en-bloc TURBT, were compared with patients who had conventional resection for the presence of detrusor muscle in the biopsy specimen on an initial resection. Tumor size was calculated on ultrasonography or contrast enhanced computerized tomography scan. Tumor with pedunculated base, more than 4 cm in size and tumor with hydroureteronephrosis were excluded. Conventional electrocautery loop was bent to 45° and periphery of the tumor was marked first and then the whole tumor was resected en bloc. The free-lying tumor was then cut into two or three pieces in the bladder for retrieval. Statistical analysis was done using SPSS software Version 13.
Statistical Analysis Used:
Statistical analysis was done using Pearson chi square test and P value of <.05 was considered significant.
Results:
A total of 25 patients in the control arm (with conventional TURBT) were compared with 21 patients who had en-bloc TURBT. En-bloc TURBT did not result in bladder perforation as vision was clear due to better hemostasis. Twenty of 21 (94.4%) patients had detrusor muscle but only 15 of 25 (60%) patients in the control arm had detrusor muscle on histopathological examination (P.001)
Conclusions:
En-bloc TURBT is safe and gives well-controlled resection of the whole tumor due to better visualization. Yield of detrusor muscle present in the specimen is significantly better with en-bloc TURBT.
Keywords: Non muscle invasive bladder cancer, Transurethral resection of the bladder tumor, en bloc
INTRODUCTION
The world over bladder cancer is the seventh most common malignancy in men and the eighth most common malignancy in females.[1] In India bladder cancer is the fifth most common cancer in men according to the Delhi-based registry with age-adjusted incidence rate of 5.8/100,000 person years.[2] In India it is predominantly the disease of the male population with a male to female ratio of 8.6:1 with median age at presentation of 60 years (range: 18-90 years).[3]
Transurethral resection of bladder tumor (TURBT) is the cornerstone in the management of bladder cancer. Goals of TURBT are to look for detrusor muscle invasion and complete resection of tumor. Even though conventional TURBT, where tumor is removed in piecemeal, has been in practice for many years, issues like absence of detrusor in histopathology report and incomplete resection continue to plague the adequacy of TURBT. Presence of detrusor is a surrogate for the completeness of resection[4] but various series have reported absence of detrusor musclein TURBT specimen in up to 50% of the cases.[5,6] Restaging TURBT has shown presence of residual disease in up to 76% of cases.[6] We aim to assess performance of en-bloc TURBT as compared to conventional TURBT for adequacy of initial resection of the tumor judged by the presence of the detrusor muscle in the specimen.
MATERIALS AND METHODS
In a prospective nonrandomized interventional design a pilot study was conducted between September 2007 and December 2010, to see the safety and efficacy of en-bloc TURBT as compared to the conventional TURBT. En-bloc TURBT was done by a single surgeon and to avoid bias towards deliberate attempt to resect the tumor completely two other urologists did the conventional TURBT. All three urologists were senior consultants with more than 10 years of experience. Clinical data on the size (measured by ultrasonography in 22 patients and by CECT in 24 patients) and the location of the tumor were recorded.
Inclusion criteria
Patients presenting for the first time with single tumor on imaging and with tumor size from 2-4 cm were included for the study.
Exclusion criteria
Patients with recurrences, multiple tumors and those with tumor size of less than 2 and more than 4 cm were excluded. Tumors with prior history of TURBT and pedunculated tumors were also excluded.
Technique of en-bloc TURBT
The usual Tungsten loop electrode and 26FR resectoscope (Storz, Germany) with 30° lens and monopolar cautery was used in all the cases under regional anesthesia and general anesthesia if tumor was located in the lateral wall. The angle of the loop electrode was changed manually from 90° to 45° [Figure 1] for en-bloc TURBT. The feasibility of en-bloc TURBT was initially tried in tumors less than 2 cm in size in six cases and then this study was started.
Figure 1.
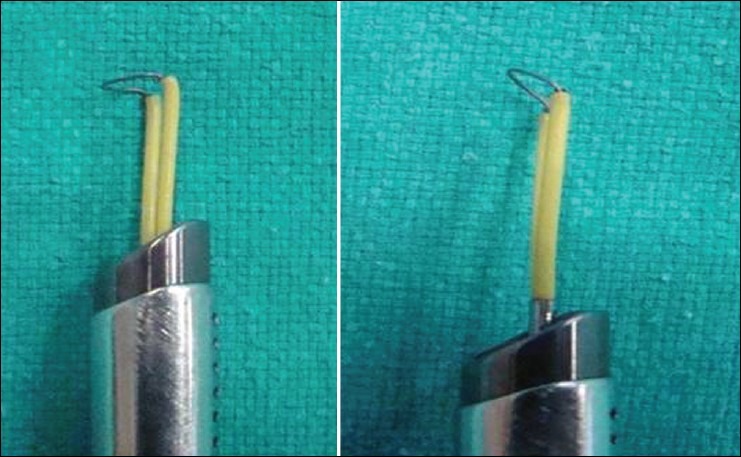
(a) Normal right-angled loop and (b) Electrocautery loop bent at 45° (for en-bloc TURBT)
After identifying the tumor, normal mucosa, 1 cm away from the tumor base was marked all around it by using coagulation current at setting 60-80W (Valley Lab, USA). Blood vessels entering the base of the tumor were coagulated before starting the procedure [Figure 2]. Glycine 1.5% was used as an irrigant during the resection.
Figure 2.
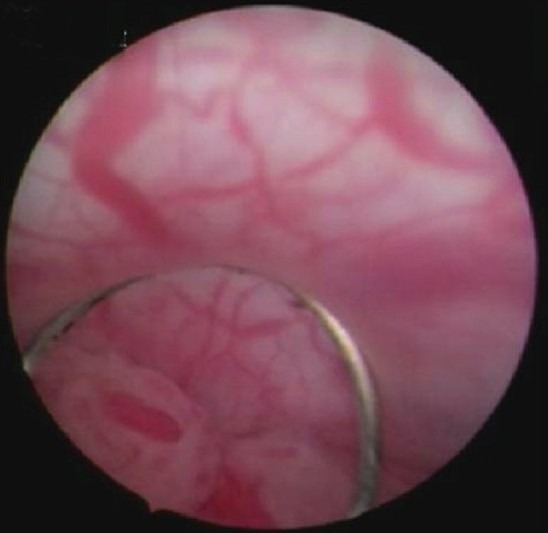
Marking the periphery of the tumor and at the same time coagulating the feeding blood vessels
By using cutting current setting at 100-115W, incision from the normal mucosa was deepened till detrusor muscle plane was reached and then retrograde resection was started in the deep layer of the detrusor seeing and coagulating the feeding vessels. Angle of the loop and beak of the resectoscope (not seen in the picture) helped in elevating the tumor and going deep to its base till the whole tumor was resected [Figure 3].
Figure 3.
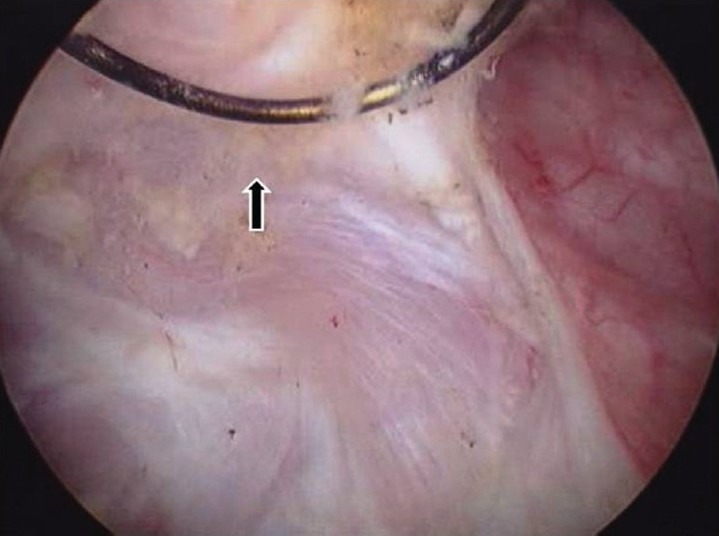
Angled loop helped in elevating the tumor and dissection at the base
Once the tumor was detached, then the larger tumors were cut into two to three pieces in the bladder itself. After stopping the inflow and resting the tumor in the trigone and base area the tumor was cut into pieces using cutting current. The largest tumor removed was 3 cm in size in a female [Figure 4]. Intravesical chemotherapy after TURBT was not used as per the practice at our institute. Histopathological examination was done according to the 2004 World Health Organization (WHO)–International Society of Urological Pathological grading system. The end point was presence or absence of detrusor muscle. Blood loss was calculated in terms of fall in hemoglobin levels measured before and a day after TURBT but it was not significant. Statistical analysis was done using Pearson chi square test and P value of <.05 was considered significant.
Figure 4.
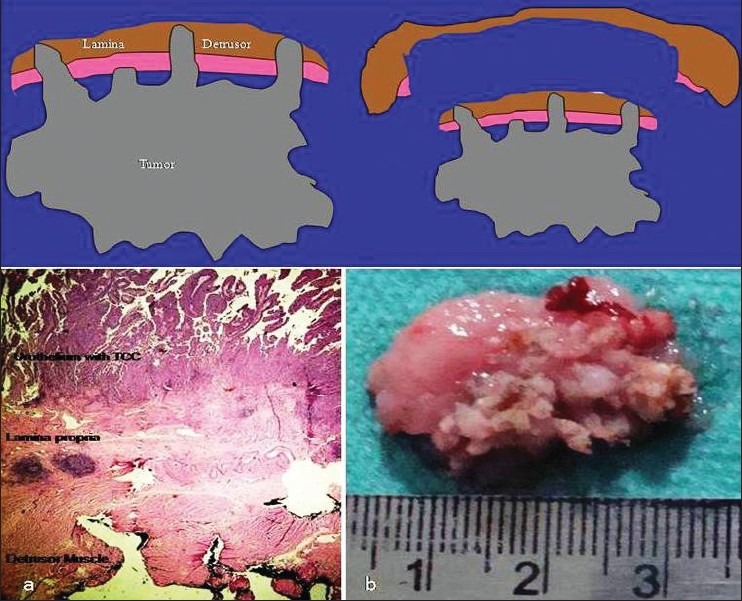
En bloc TURBT gives all three layers i.e. Detrusor muscle, lamina and urothelium in the tumor as one specimen. Photomicrograph showing all three layers with inked outer margin; H and E stain, ×20
RESULTS
A total of 49 patients were registered for this trial. Three patients had multiple tumors so were excluded from the study. Of 21 patients in the en-bloc group, 20 (94.4%) had detrusor muscle in their initial specimen. In the en-bloc group, the procedure could be completed without any bladder perforation as vision was much better due to better hemostasis. One patient who did not have detrusor muscle in the resected specimen, had TURBT in the initial part of the study. In conventional TURBT, only 15 of 25 (60%) had detrusor muscle in biopsy report. One patient had bladder perforation who had a 4-cm tumor on the lateral wall and was managed conservatively with a peritoneal drain. None of the patients in the en-bloc group had bladder perforation.
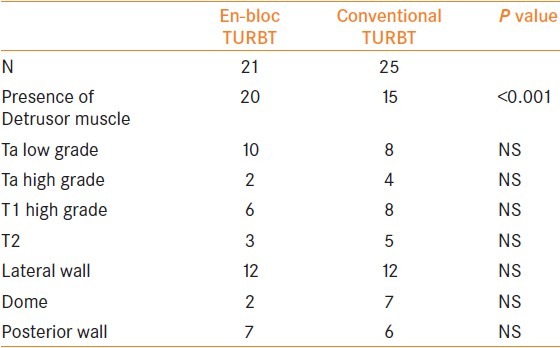
Location of the tumor, stage and grade were comparable in both the groups [Table 1].
Table 1.
Stage and grade of tumors in the two groups on first TURBT
Though there was no significant difference in the blood loss, hemostasis was better in the en-bloc group as it was easy to coagulate blood vessels at the base at the time of cutting and lifting the tumor up. The second advantage was that the depth of resection could easily be controlled in comparison to the conventional TURBT.
Of 10 patients who did not show muscle on an initial TURBT, three patients refused to undergo second-look TURBT, two had radical cystectomy for high-grade lamina-invasive Transitional cell carcinoma and out of five who had second look, one had muscle-invasive TCC and the remaining four had detrusor muscle free of tumor.
DISCUSSION
Transurethral resection of bladder tumor remains a surgery in which the end point is the presence of muscle but complete resection is not always achieved.
Transurethral resection of the bladder tumor bladder tumor is the most underrated surgery in urology. Its adequacy is a hallmark of a good local control but there is no yardstick available clinically to adjudge complete resection of the tumor. This is evident by the absence of the detrusor muscle in a significant number of patients in initial TURBT. There are some surrogate markers to assess adequate resection described in the literature and those are, presence of detrusor muscle in the specimen and the rate of subsequent recurrence.[7–9]
An ideal TURBT would mean complete resection of the visible tumor, resection of the surrounding healthy looking mucosa for up to 1 cm and then the removal of the detrusor muscle. Herr described three ways to measure the quality of a good TURBT, i.e. complete resection, presence of deep muscle in the specimen and the rate of recurrence at the site of previous TURBT.[10] He also suggested classifying tumor resection as R0, microscopic negative margin, R1 microscopic positive margin and R2 that is macroscopic positive margin. This kind of assessment is not practical in conventional TURBT but could be possible in en-bloc resection, where we can have a complete piece of tumor tissue including lamina propria and detrusor muscle with it. The innermost surface of the detrusor muscle could then be inked thereby examining all three layers in one piece that would give us a better understanding of the tumor stage and a true perspective of the level of resection i.e. R0-R1 [Figure 4].
Inadequate TURBT in a conventional way is not only judged by the absence of muscle in an initial specimen but also by the rate of recurrence at the same site. It is common knowledge that recurrence is seen in 50-80% of non-muscle-invasive bladder cancer mostly during the first year. Reasons that have been described for recurrences are incomplete resection, cell implantation or the tumor biology itself.[11] Incomplete resection seems to be the most important reason for recurrence. European organization for research and treatment of cancer on review of seven randomized controlled trials noted significant difference in the recurrence rate among different institutions and after controlling established factors for recurrence like tumor size, multiplicity, stage and grade, it was concluded that a wide range in the rate of recurrence i.e. 0-46%, is due to the difference in the quality of resection.[12] Inadequate resection leading to a higher rate of recurrence at the same site is supported by another study where 81% of recurred tumors occurred at the site of previous resection.[13]
There are many ways described in the literature to improve the quality of TURBT with the use of different kinds of loops and laser. En-bloc dissection has been described to have a better pathological evaluation for Ta and T1 tumors.[14] In that study a flat loop electrode was used to resect the tumors less than 2.5 cm in size.[14] Though the authors did not describe the presence or absence of the detrusor muscle, they concluded that invasion of the lamina was better delineated with en-bloc resection. A limitation of this technique described was the inability to use a flat loop for tumors located at the anterior and upper posterior wall. Another limitation was that tumor of more than 2.5 cm was considered a contraindication.
For a small-size papillary tumor it really does not make any difference whether an en bloc or conventional TURBT is done? but for doing en bloc for large tumors, there are indeed no reports in the literature. We used a 45° angle loop electrode with a 30° lens, that helped in scooping out the tumor in retrograde fashion. Removing a large tumor resected en bloc though the urethra would be a difficult proposition therefore once the tumor was free, it was cut into two to three pieces for the removal from the bladder.
The detrusor muscle has been described to be absent in 30-50% of TURBT specimens at an initial resection.[4,15] Absence of the detrusor muscle not only affects the recurrence rate as previously described but also brings in the need for second-look TURBT. The presence of the detrusor muscle lessens the rate of upstaging in second-look TURBT. In one study, tumors were upstaged by second resection in 15% of 421 patients who had detrusor muscle at initial resection as compared to 45% of 280 patients with no muscle.[16] Therefore with the present method a higher incidence of finding the detrusor muscle in the specimen of an initial TURBT would not only provide adequacy of the TURBT but also reduce the need for second-look TURBT. Second-look surgery is a significant deterrent on the part of the patients, which not only adds to the mental anguish but also increases the cost of the procedure.
Another possible advantage of en-bloc TURBT is that it could eliminate crush artefact of cold cup deep biopsy and diathermy artefacts are less likely to happen as the tissue piece obtained by it is too large to be affected by cautery.
Though the surgical expertise is an important denominator for the yield of detrusor muscle, even an experienced urologist did not fare well in getting complete removal of the bladder tumor with conventional TURBT.[17] The adequacy of an initial TURBT that is judged by the presence of the detrusor muscle in the initial specimen is much better with en-bloc TURBT than conventional TURBT. Thought no method described till date has resulted in the presence of detrusor muscle in 100% cases in initial TURBT, en-bloc TURBT helped in achieving adequate resection in 94% of cases.
We have not used intravesical mitomycin in our study protocol.
Though there is Level 1 evidence to suggest that intravesical Mitomycin C (MMC) should be used, its role in preventing recurrences in high-grade or multiple tumors is not clear. It does not change surveillance cystoscopic protocol and the cost of follow-up remains high.
CONCLUSION
The presence of the detrusor muscle which is considered as a surrogate marker for complete resection in TURBT determines the rate of recurrence. En-bloc TURBT is feasible and safe and has a better yield of the presence of the detrusor muscle in the initial resection specimen of non-muscle-invasive bladder cancer. Rate of presence of muscle with en bloc was significantly higher than the conventional TURBT. En-bloc TURBT provides a better hemostasis and vision to control the resection limits. Though our initial experience of en-bloc TURBT is small the results are encouraging and it can be extended to a larger number of patients. In future it will be interesting to see the effect of en-bloc TURBT on recurrence.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Grasso M. Bladder cancer: A major public health issue. Eur Urol Suppl. 2008;7:510–5. [Google Scholar]
- 2.Raina V, Tyagi BB, Manoharan N. Cancer incidence and mortality in Delhi UT-urban, 2002-2003. Delhi cancer registry, Dr. B.R. Ambedkar institute rotary cancer hospital, All India Institute of Medical Sciences, New Delhi [Google Scholar]
- 3.Gupta P, Jain M, Kapoor R, Muruganandham K, Srivastava A, Mandhani A. Impact of age and gender on the clinicopathological characteristics of bladder cancer. Indian J Urol. 2009;25:207–10. doi: 10.4103/0970-1591.52916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herr H, Donat S. A re-staging transurethral resection predicts early progression of superficial bladder cancer. BJU Int. 2006;97:1194–8. doi: 10.1111/j.1464-410X.2006.06145.x. [DOI] [PubMed] [Google Scholar]
- 5.Maruniak N, Takezawa K, Murphy W. Accurate pathological staging of urothelial neoplasms requires better cystoscopic sampling. J Urol. 2002;167:2404–7. [PubMed] [Google Scholar]
- 6.Herr HW. The value of a second transurethral resection in evaluating patients with bladder tumours. J Urol. 1999;162:74–6. doi: 10.1097/00005392-199907000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Mariappan P, Smith G, Lamb AD, Grigor KM, Tolley DA. Pattern of recurrence changes in noninvasive bladder tumours observed during 2 decades. J Urol. 2007;77:867–75. doi: 10.1016/j.juro.2006.10.048. [DOI] [PubMed] [Google Scholar]
- 8.Herr HW, Donat SM. A re-staging transurethral resection predicts early progression of superficial bladder cancer. BJU Int. 2005;97:1194–8. doi: 10.1111/j.1464-410X.2006.06145.x. [DOI] [PubMed] [Google Scholar]
- 9.Grimm M-O, Steinhoff C, Simon X, Spiegelhalder P, Ackermann R, Vogeli AT. Effect of routine repeat transurethral resection for superficial bladder cancer: A long-term observational study. J Urol. 2003;170:433–7. doi: 10.1097/01.ju.0000070437.14275.e0. [DOI] [PubMed] [Google Scholar]
- 10.Herr HW, Donat MS. Quality control in transurethral resection of bladder tumors. BJU Int. 2008;102:1242–6. doi: 10.1111/j.1464-410X.2008.07966.x. [DOI] [PubMed] [Google Scholar]
- 11.Kurth KH, Bouffioux C, Sylvester R, van der Meijden AP, Oosterlinck W, Brausi M members of the EORTC Genitourinary Group. Treatment of superficial bladder tumors: Achievements and needs. Eur Urol. 2000;37:1–9. doi: 10.1159/000052386. [DOI] [PubMed] [Google Scholar]
- 12.Brausi M, Collette L, Kurth K, van der Meijden AP, Witjes JA, Sylvester RJ. Variability in the recurrence rate at first follow-up cystoscopy after TUR in stage Ta T1 transitional cell carcinoma of the bladder: A combined analysis of seven EORTC studies. Eur Urol. 2002;41:523–31. doi: 10.1016/s0302-2838(02)00068-4. [DOI] [PubMed] [Google Scholar]
- 13.Grimm M-C, Ackermann R, Vogeli TA. Effect of routine repeat transurethral resection for superficial bladder cancer: A long-term observational study. J Urol. 2003;170:433–7. doi: 10.1097/01.ju.0000070437.14275.e0. [DOI] [PubMed] [Google Scholar]
- 14.Lodde M, Lusiardi L, Palermo S, Signorello D, Maier K, Hohenfellner R, et al. En bloc transurethral resection of bladder tumors: Use and limits. Urology. 2003;62:1089–91. doi: 10.1016/s0090-4295(03)00761-1. [DOI] [PubMed] [Google Scholar]
- 15.Mariappan P, Zachou A, Grigor KM for the Edinburgh Uro-Oncology Group. Detrusor muscle in the first, apparently complete transurethral resection of bladder tumour specimen is a surrogate marker of resection quality, predicts risk of early recurrence, and is dependent on operator experience. Eur Urol. 2010;57:843–9. doi: 10.1016/j.eururo.2009.05.047. [DOI] [PubMed] [Google Scholar]
- 16.Jesuraj MG, Harris M, Rogers A, Whiteway JE. Completeness of the first resection of bladder tumour depending on the seniority of the surgeon. Eur Urol Suppl. 2008;7:138. [Google Scholar]
- 17.Zurkirchen MA, Sulser T, Gaspert A, Hauri D. Second transurethral resection of superficial transitional cell carcinoma of the bladder: A must even for experienced urologists. Urol Int. 2004;72:99–102. doi: 10.1159/000075961. [DOI] [PubMed] [Google Scholar]


