Abstract
Introduction:
Karimnagar District has consistently achieved highest rates of no-scalpel vasectomy (NSV) in the past decade when compared to state and national rates. This study was conducted to elucidate the underlying causes for higher acceptance of NSV in the district.
Materials and Methods:
A community-based, case control study was conducted. Sampling techniques used were purposive and simple random sampling. A semi-structured questionnaire was used to evaluate the socio-demographic, family characteristics, contraceptive history and predictors of contraceptive choice in 116 NSV acceptors and 120 other contraceptive users (OCUs). Postoperative complications and experiences were ascertained in NSV acceptors.
Results:
Age (χ2=11.79, P value = 0.008), literacy (χ2=17.95, P value = 0.03), duration of marriage (χ2=14.23, P value = 0.008) and number of children (χ2=10.45, P value = 0.01) were significant for acceptance of NSV. Among the predictors, method suggested by peer/ health worker (OR = 1.5, P value = 0.01), method does not require regular intervention (OR = 1.3, P value = 0.004) and permanence of the method (OR = 1.2, P value = 0.031) were significant. Acceptors were most satisfied with the shorter duration required to return to work and the most common complication was persistent postoperative pain among 12 (10.34%) of the acceptors.
Conclusion:
Advocating and implementing family planning is of high significance in view of the population growth in India and drawing from the demographic profile, predictors, pool of trainers and experiences in Karimnagar District, a similar achievement of higher rates of this simple procedure with few complications can be replicated.
Keywords: Karimnagar District, no-scalpel vasectomy, predictors of acceptance
INTRODUCTION
In contrast to female sterilization in India which has been adopted by 37.3% of couples practicing contraception, only 1% of the couples opt for male sterilization[1] as per National Family Health Survey III (NHFS III) data. This is in spite of male sterilization being a shorter, simpler procedure fraught with lesser complications, having a shorter recovery time and being more cost-effective. The barriers to adoption of male sterilization in India are profound with reasons ranging from unfounded fears among males characterizing vasectomy with physical weakness, loss of virility, manhood and inability to enjoy intercourse. Additionally, there is a traditional desire for more children, especially of male gender to carry on the family name, lack of adequate contraceptive knowledge, and the monetary and time costs of obtaining contraception.[2] Anecdotally, methods of family planning involving sterilization in India have been associated with coercion due to improper political foresight in the past and a cautious approach needs to be adopted to promote sterilization and to provide couples a contraceptive choice with informed consent.
No-scalpel vasectomy (NSV) is a surgical technique pioneered by Dr. Li Shunqiang to reduce the fear of incision, popularized in the West by Dr. Marc Goldstein of Cornell University and is currently the gold standard for male sterilization in several countries.[3] NSV has been proven in several multi-center, randomized trials to have lower risk of postoperative hematoma, pain during surgery, postoperative scrotal pain, and wound infection.[3–5] The NSV technique uses a sharp forceps-like instrument to puncture the skin contrary to traditional vasectomy which uses a scalpel for incision, thereby reducing bleeding, infection and pain. NSV is consistently associated with faster recovery and a shorter duration of hospital stay due to the lack of use of sutures.[6]
There is political commitment to promote NSV and the government of India has launched a national NSV project in 1998 in collaboration with the United Nations Population Fund, the impetus of which was continued in the National Population Policy of 2000 which focuses on long-term methods of family planning including male sterilization. Under the programs, over 4000 national-level master trainers (service providers), state master trainers and district master trainers have been trained to conduct vasectomy camps, train medical officers in primary health centers and to promote the acceptance of NSV. A monetary incentive of Rs. 1500/- in accredited private health facilities is provided for vasectomy acceptors in Andhra Pradesh under the National Rural Health Mission (NRHM) program[7]
Karimnagar District in Andhra Pradesh has had the highest rates for male sterilization through NSV from the years 2002–08 as per the District Level Household and Facility Survey[8,9] and the current study evaluated the underlying causes for this higher rate of acceptance in the district to be able to replicate and promote the acceptance of NSV on a wider scale.
MATERIALS AND METHODS
A community-based case control study was conducted over a period of three months in Karimnagar District. A questionnaire devised after a focus group discussion was administered via a face to face interview to the sample respondents. The questionnaire consisted of both open and closed-ended questions. The purpose of the study was explained and informed consent was obtained from the respondents. The questionnaire was explained in lay language and responses were recorded by interviewers. Complete privacy and confidentiality was ensured during the process.
Two groups were sampled: i) Cases who were NSV acceptors ii) Controls were men from eligible couples using contraceptive methods for family planning other than NSV i.e. other contraceptive users (OCUs). Non-random purposive sampling was employed to obtain NSV acceptors who had undergone NSV in Karimnagar District in the previous year and were traced retrospectively until a sample size of 116 was obtained. OCUs were obtained through simple random sampling from the eligible couples register in the field practice area of a teaching hospital to obtain a 1:1 ratio among cases and controls.
The questionnaire administered consisted of five parts:
Socio-demographic profile of the respondents including age, literacy, total family monthly income, and duration of married life. Literacy and income were classified into groups for data analysis based on the 2008 revision of the Kuppuswamy scale for socioeconomic status.[10]
Family characteristics including the number of children and ever use of other methods of contraception apart from vasectomy.
Predictors of contraceptive choice were evaluated on seven domains which were permanence of the contraceptive method, failure rate, side-effects and complications, recommendation by peers and health workers, availability and usability, whether it required regular intervention and monetary incentive provided. Responses were obtained on a five-point Likert scale on how important each predictor was in deciding a particular method of contraception. The responses were graded from ‘Not at all’ to ‘Very much’ with higher scores assigned to greater importance of the predictor in decision-making during analysis. NSV acceptance was coded as the dependent variable and predictors were used to perform a binary logistic regression analysis and odds ratio and significance values were obtained.
Satisfaction with the procedure among NSV acceptors was obtained on a five-point Likert scale, on a range of 1–5 with higher scores corresponding to greater satisfaction and lower scores corresponding to non-satisfaction. Satisfaction was measured on the following domains, duration of the procedure, pain involved, time required to return to work after the procedure, satisfaction with the postoperative counseling provided and availability of the service provider when required. Likert scales are psychometric scales and have been used to measure patient satisfaction regarding vasectomy in similar studies.[11]
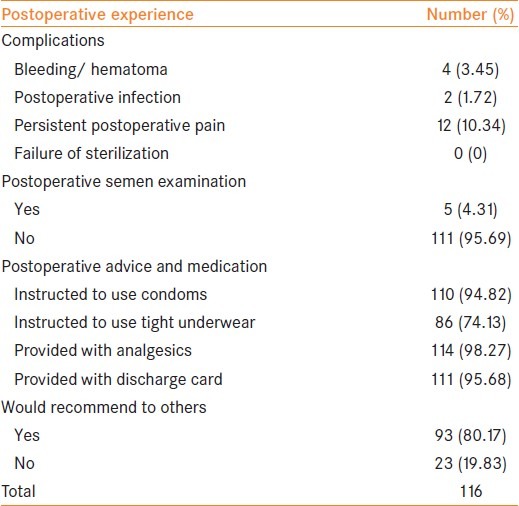
Postoperative experiences and complications were recorded among NSV acceptors. The occurrence of postoperative complications including excessive bleeding or hematoma formation, infection, persistent pain and failure of contraception were recorded. Information on postoperative advice and medications provided by health workers was obtained including the instructions to use condoms for three months postoperatively, to wear tight underwear to provide support and prevent bleeding, provision of analgesics and a properly documented discharge card. Respondents were asked whether they would recommend NSV to others.
Statistical analysis was done by using PASW 18 (SPSS) and statistical measures obtained were percentages, means, confidence intervals, proportions significance test, and binary logistic regression.
RESULTS
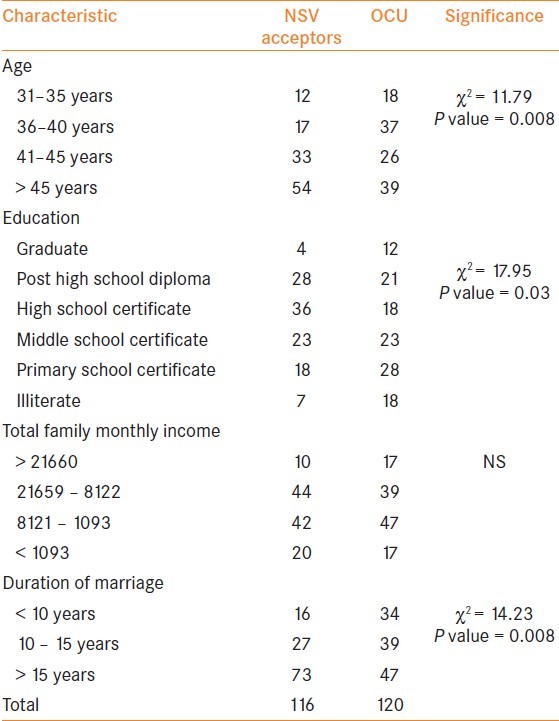
A sample size of 236 was obtained which included 116 NSV acceptors and 120 OCUs. The age of the respondents ranged from 31—55 years with the mean age in NSV acceptors being 44.51 years and the mean age in OCUs being 42.45 years. A proportions test showed a significant association between increasing age and acceptance of NSV as a contraceptive choice (χ2 = 11.79, P value = 0.008). Literacy was also significant for NSV acceptance and Chi square test values were χ2 = 17.95 and P value = 0.03. There was no significant association between total family monthly income and acceptance of NSV. A longer duration of married life was found to be associated with NSV acceptance (χ2 = 14.23, P value = 0.008). The age groups, education classes, total family monthly income and duration of marriage are presented in Table 1.
Table 1.
Socio-demographic characteristics of the respondents
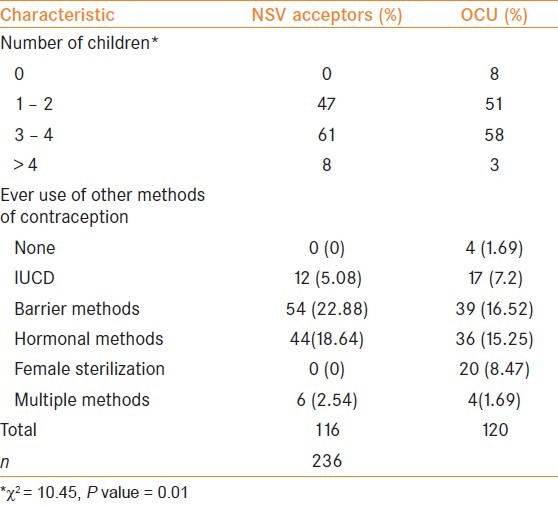
The number of children per couple were obtained for both NSV acceptors and OCUs and this was significant for an outcome of NSV with a Chi square value of 10.45 and P value of 0.01. Other contraceptive methods ever used in married life apart from male sterilization were obtained. The predominant method in NSV acceptors was barrier method (n=54, 22.88%) whereas both barrier methods (n=39, 16.52%) and hormonal methods (n=36, 15.25%) were used by OCUs. This information is depicted in Table 2.
Table 2.
Family characteristics and contraceptive history of the respondents
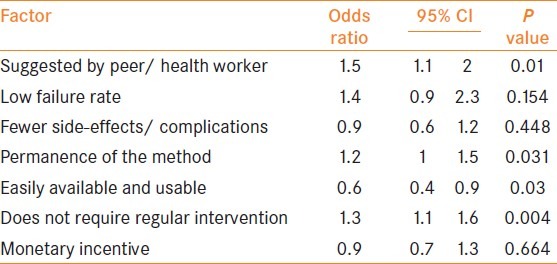
A binary logistic regression analysis was performed for factors affecting contraceptive choice and predicting an outcome of NSV acceptance. Odds ratio of more than one and significant P values were obtained for the following factors: method suggested by peer/ health worker (OR = 1.5, P value = 0.01), method does not require regular intervention (OR = 1.3, P value = 0.004) and permanence of the method (OR = 1.2, P value = 0.031). An odds ratio of less than one was obtained for availability and usability of the method (OR = 0.6, P value = 0.03). Failure rate, side-effects and complications and monetary incentive were not significant in predicting an outcome of NSV acceptance. The regression analysis results are depicted in Table 3.
Table 3.
Predictors influencing contraceptive choice
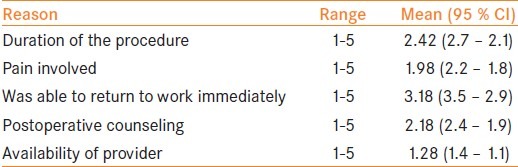
The predominant source of information regarding NSV among the NSV acceptor group was from previous acceptors (n=86, 74.13%). In the group, the domain with the highest satisfaction was the time required to return to work after the procedure with a mean score of 3.18 (3.5–2.9) while the domain with the least satisfaction was the availability of the service provider when required with a mean of 1.28 (1.4–1.1). The mean values for duration of the procedure, pain involved and postoperative counseling received are depicted in Table 4.
Table 4.
Satisfaction with the procedure
The commonest postoperative complication in the sample was persistent postoperative pain (n=12, 10.34%) followed by bleeding/hematoma occurrence (n=4, 3.45%) and infection (n=2, 1.72%). Most respondents (n=111, 95.69%) did not undergo a postoperative semen examination. Most people (98.27%) received analgesics and discharge cards (95.68%) after the procedure while postoperative instructions such as wearing of tight underwear to prevent bleeding (74.13%) were received by a lesser number of acceptors; 80.17% of the respondents would recommend the procedure to others. These values are presented in Table 5.
Table 5.
Postoperative experience and complications of NSV acceptors
DISCUSSION
The low acceptance of male sterilization in comparison to the number of women undergoing sterilization has been continuing despite attempts through National health programs providing health manpower and training, political commitment and more effective surgical techniques. To ensure voluntary and informed acceptance of NSV requires understanding of the interplay of the social and medical factors involved.
In the current study, rising age was significant for acceptance of NSV. Most acceptors of NSV were aged above 40 years. A similar trend was observed by Khokar et al.,[12] who studied acceptance of NSV in a public sector hospital in Delhi. While this reflects a desire for hassle-free contraception after completion of the family, the lesser acceptance among men in the reproductive age group suggests that there is still a need to promote acceptance in a younger age group. Literacy was significant for acceptance of NSV whereas total family income was not. A similar proportion was obtained by Khokhar et al.,[12] with increasing acceptance of NSV in people who had completed higher secondary education. This may be explained by a greater health awareness and better understanding and adoption of advice from health workers in general among groups with higher literacy. A longer duration of marriage was also significant for acceptance of NSV and again this can be explained by a desire for a hassle-free contraceptive after completion of the family.
All vasectomy acceptors had more than one child and there was a significant association between the number of children and acceptance of vasectomy. However, a similar trend was also seen in OCUs. This suggests that even after completion of the family, there is equal use of both terminal and non-terminal methods of contraception. NSV acceptors were more likely to have used barrier methods of contraception, hormonal methods and multiple methods of contraception before undergoing terminal contraception whereas intrauterine devices (IUDs) were more popular among OCUs when compared to the NSV group. A study by Murthy et al.,[13] found a similar high use of barrier methods by NSV acceptors before sterilization in Andhra Pradesh. However, Khokar et al.,[12] obtained a higher use of barrier methods and IUDs among NSV acceptors. This suggests regional differences between usage of contraceptive methods before undergoing sterilization and requires further study.
There are a multitude of factors that interplay and determine the acceptance of a contraceptive method. The most important factors determining contraceptive choice were selected based on a focus group discussion, and predictors of NSV acceptance were determined in logistic regression analysis. The significant predictors in order of odds ratio obtained were method suggested by peer/health worker, method does not require regular intervention, and lastly, permanence of the method. Ease of availability and usability was significant on regression analysis, but with an odds ratio of less than one indicating its higher importance in the OCU group. Failure rate, side-effects and complications, and monetary incentive were not significant in predicting an outcome of NSV acceptance. This indicates a less informed choice regarding contraceptive method adoption and most people relying on the suggestion by the health worker /peer for choosing a method of contraception. Ample usage can be made of this finding to promote acceptance of NSV by utilizing health worker services for health education and communication through the community of past adopters of NSV. More information should be provided by health workers prior to sterilization so that users can make an informed choice.
NSV acceptors were most satisfied with the aspect that they could immediately return to work after the procedure and no work days were lost. Duration of the procedure too played an important role in satisfaction followed by postoperative counseling. Users were least satisfied by availability of service providers implying a possible lack of trained personnel.
Few complications were reported, the commonest being persistent postoperative pain. Instances of bleeding or hematoma formation and postoperative infection were minimal as consistent with the improved surgical technique in NSV.[14,15] Few acceptors underwent a semen examination after the procedure, however, a high proportion received postoperative instructions, analgesics and documented discharge cards reflecting on the quality of services provided which can promote acceptance through word of mouth publicity through past acceptors. The satisfaction is also reflected among the numbers that most would recommend the procedure to their peers.
CONCLUSION
Acceptance of NSV increases with age, literacy, duration of marriage and number of children. Suggestion by a health worker or peer is a motivating factor in obtaining vasectomy and most acceptors are satisfied with the short duration of the procedure and rapid recovery. There are few complications with the procedure and a majority would recommend the procedure to others. Increased availability of trained personnel who can perform NSV is desirable.
Advocating and implementing family planning is of high significance in view of the population growth in India and drawing from the demographic profile, predictors, pool of trainers and experiences in Karimnagar District, similar achievement of higher rates of this simple procedure with few complications can be replicated elsewhere.
Limitations
Contraceptive history obtained from respondents may have been subject to recall bias, satisfaction regarding NSV was solely the respondent's subjective perception. Further analysis in future studies needs to be done comparing each contraceptive method versus NSV.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mumbai, India: International Institute for Population Sciences (IIPS) and Macro International; 2005-06. [Last cited on 2011 Aug 30]. Key Indicators for India from National Family Health Survey – 3. Available from: http://www.nfhsindia.org/pdf/India.pdf . [Google Scholar]
- 2.Santhya KG. Changing family planning scenario in India: An overview of recent evidence. New Delhi: Population Council; 2003. p. 52. (South and East Asia regional working paper no. 17) [Google Scholar]
- 3.Sokal D, McMullen S, Gates D, Dominik R. A comparative study of the no scalpel and standard incision approaches to vasectomy in 5 countries. The Male Sterilization Investigator Team. J Urol. 1999;162:1621–5. [PubMed] [Google Scholar]
- 4.Cook LA, Pun A, van Vliet H, Gallo MF, Lopez LM. Scalpel versus no-scalpel incision for vasectomy. Cochrane Database Syst Rev. 2007;18:CD004112. doi: 10.1002/14651858.CD004112.pub3. [DOI] [PubMed] [Google Scholar]
- 5.Christensen P, al-Aqidi OA, Jensen FS, Dørflinger T. Vasectomy. A prospective, randomized trial of vasectomy with bilateral incision versus the Li vasectomy. Ugeskrift Laeger. 2002;164:2390–4. [PubMed] [Google Scholar]
- 6.Kumar V, Kaza RM, Singh I, Singhal S, Kumaran V. An evaluation of the no-scalpel vasectomy technique. BJU Int. 1999;83:283–4. doi: 10.1046/j.1464-410x.1999.00934.x. [DOI] [PubMed] [Google Scholar]
- 7.Xiaozhang L. The WHO Reproductive Health Library. Geneva: World Health Organization; Scalpel versus no-scalpel incision for vasectomy: RHL commentary [Last revised on 2009 July 27] [Google Scholar]
- 8.District Level Household and Facility Survey (DLHS-3), 2007-08: India. Andhra Pradesh: Mumbai: IIPS; 2010. International Institute for Population Sciences (IIPS), 2010. [Google Scholar]
- 9.Center for Operations Research and Training (CORT) and UNFPA. Non-Scalpel Vasectomy and client satisfaction in Andhra Pradesh, 2007: New Delhi [Google Scholar]
- 10.Parashar SS. Principles of Sociology in Health Care. In: Bhalwar R, editor. Textbook of public health and community medicine. 1st ed. Pune: Gayo Enterprises; 2009. pp. 608–12. [Google Scholar]
- 11.Moses S, Oloto E. A community-based vasectomy service in Leicestershire and Rutland - The patients’ perspective. Eur J Contracept Reprod Health Care. 2010;15:17–23. doi: 10.3109/13625180903414483. [DOI] [PubMed] [Google Scholar]
- 12.Khokhar A, Sachdeva TR, Talwar R, Singh S, Rasania SK. Determinants of acceptance of No-scalpel vasectomy among men attending the NSV clinic in a public sector hospital of Delhi. Health Popul Perspect Issues. 2005;28:197–204. [Google Scholar]
- 13.Murthy SR, Rao MD. An analysis of factors influencing the acceptability of vasectomy in Andhra Pradesh. Health Popul Perspect Issues. 2003;26:162–82. [Google Scholar]
- 14.Pant PR, Sharma J, Subba S. Scrotal haematoma: The most common complication of no-scalpel vasectomy. Kathmandu Univ Med J (KUMJ) 2007;5:279–80. [PubMed] [Google Scholar]
- 15.Lara-Ricalde R, Velázquez-Ramírez N, Reyes-Muñoz E. No-scalpel vasectomy. Profile of acceptance and results. Ginecol Obstet Mex. 2010;78:226–31. [PubMed] [Google Scholar]


