Abstract
Objective
To examine the modern epidemiology of abdominal aortic aneurysm (AAA) rupture and short-term AAA-related mortality after the introduction of endovascular aneurysm repair (EVAR).
Background
Prior epidemiologic studies have demonstrated stable rates of AAA repair, repair mortality, and AAA rupture. Recently, EVAR has been introduced as a less invasive treatment method and its use has expanded to over 75% of elective AAA repairs.
Methods
We identified Medicare beneficiaries undergoing AAA repair and those hospitalized with a ruptured AAA during the period 1995–2008 and calculated standardized annual rates of AAA-related deaths due to either elective repair or rupture.
Results
338,278 patients underwent intact AAA repair over the study period. There were 69,653 patients with AAA rupture of whom 47,524 underwent repair. Intact repair rates increased substantially in those over age 80 (57.7 to 92.3 per 100,000, P<0.001), but decreased in those aged 65–74 (81.8 to 68.9, P<0.001). A decline in ruptures with and without repair was seen in all age groups. By 2008, 77% of all intact repairs and 31% of all rupture repairs were performed with EVAR (P<0.001). Operative mortality declined over the study period for both intact (4.9% to 2.4%, P<0.001) and ruptured (44.1% to 36.3%, P<0.001) AAA repair. Short-term AAA-related deaths decreased by more than half (26.1 to 12.1 per 100,000, P<0.001) with the greatest decline occurring in those over age 80 (53.7 to 27.3, P<0.001).
Conclusions
A recent decline in AAA rupture and short-term AAA-related mortality is demonstrated and likely related in part to the introduction and expansion of EVAR. This is due to decreased deaths from ruptures (with and without repair) and decreased mortality with intact repairs, particularly in patients over age 80.
Introduction
Elective abdominal aortic aneurysm (AAA) repair is undertaken in order to prevent future rupture with its accompanying high mortality rate.1,2 Minimally invasive endovascular AAA repair (EVAR), FDA approved in 1999, has lower perioperative mortality and morbidity compared to open surgical repair in 3 randomized trials 3–5 and the US Medicare population.6 Most elective AAA repairs in the US are now performed using EVAR.7,8 The introduction of EVAR has changed the risks and benefits of elective aneurysm repair as it now may be offered to patients considered too high risk for traditional open repair.7 Moreover, because of increased rates of advanced abdominal imaging,9,10 more AAAs are being detected incidentally than in the past. Thus, the introduction of EVAR combined with increased detection may be responsible for an increasing number of intact AAA repairs in the US, which should ultimately result in lower mortality from AAA rupture.
There has been concern, however, that EVAR may not be as effective in preventing late rupture leading to potentially increased late mortality after repair.11 Additionally, the benefit of a prophylactic procedure in the most elderly patients is unproven because many of these patients will soon die from competing causes. Consequently, the population level acute mortality impact of this increase in elective repairs following the introduction of EVAR is unknown. To understand the impact of these trends on a population level, we analyzed data on elective AAA repair and AAA rupture between 1995 and 2008 within the US Medicare population, which accounts for over 70% of elective repairs and most deaths. We hypothesized that increased rates of detection and elective repair along with the introduction and increasing use of EVAR would be associated with decreased short-term AAA-related mortality over time.
Methods
Study Population
We identified all traditional Medicare beneficiaries undergoing repair of intact AAA as well as those hospitalized with a diagnosis of ruptured AAA during the period 1995–2008 using administrative data from the Medicare program. We used the time period of 1995–2008 because this allowed us to investigate AAA repair and rupture rates beginning several years prior to FDA approval of EVAR. Those enrolled in Medicare Advantage health plans were excluded from both the study population and the population estimates because claims data are not available for these enrollees. Patients were categorized based on hospitalizations with a diagnosis of intact (ICD-9-CM code 441.4) or ruptured (ICD-9-CM code 441.3) AAA. For intact AAA, we only included those who had either EVAR (39.71) or open repair (38.44 or 39.25) during the same admission because the presence of a diagnostic code without an accompanying procedure might not indicate a clinically relevant AAA. Rupture patients were only included in the analysis if a diagnosis code for AAA rupture was their primary diagnosis as this is likely the reason for their index admission. Patients with diagnosis codes for AAA rupture in other diagnosis fields (fields other than the primary field) were excluded as these might be miss-coded or indicate a history of AAA rupture not relevant to the index admission. Rupture patients were further divided into those undergoing repair (EVAR or open) or no repair. The ICD-9 code for endovascular repair was introduced in October 2000 so we used the code for stent placement (39.90) linked to a primary diagnosis of AAA for the preceding time period. In order to limit the study population to those with pure AAA, we excluded patients with concomitant codes for aortic dissection (441.00–441.03), fenestration of dissection (39.54), thoracoabdominal aneurysm (diagnosis 441.1, 441.6, 441.2, 441.7, or repair 38.45, 39.73) or visceral/renal bypass (38.46). Demographic characteristics were obtained from the Medicare enrollment files.
Outcomes
We define short-term mortality as the combined mortality related to elective repair, rupture repair, and death due to rupture without repair. Mortality related to elective repair was defined as death within 30 days of a repair procedure or within the repair hospitalization if greater than 30 days. Mortality related to rupture was defined as all deaths within the primary hospitalization or within 30 days of a repair procedure for cases with a repair; or within 30 days of admission for persons with a diagnosis of rupture who did not undergo repair. We note that many people with ruptured AAA die prior to arriving at a hospital, so these deaths are not counted in our analyses.
Analyses
We calculated the annual incidence and mortality rates of intact AAA repair, ruptured AAA repair, and rupture without repair per 100,000 Medicare Beneficiaries. Standardized rates were calculated using the 2008 traditional Medicare enrollee data as our standard population. We first calculated standardized rates for males and females stratified by age group (65–74, 75–79, ≥80) for each year (1995–2008). We then calculated standardized rates that were gender and age adjusted per year. Rates were analyzed overall and within subgroups stratified by age and gender. In descriptive analyses, we used linear regression models with two-sided t-tests to test whether the slope of the time trend was different from 0 and to detect significant changes in rates over time. We used the Chi-square test to compare mortality rates between EVAR and open repair for various populations. All statistical analyses were performed using SAS 9.1 (SAS Institute, Cary, NC). The study was approved by the Institutional Review Board at Harvard Medical School.
Results
A total of 338,278 patients underwent repair of intact AAA over the 14 year period. Total annual intact repairs increased slightly from 23,186 in 1995 to 24,334 in 2008. There were 69,653 AAA ruptures presenting to a hospital of which 47,524 were repaired, with the annual total number of ruptures decreasing from 6,535 in 1995 to 3,298 in 2008. All results reported are statistically significant at the P<0.001 level unless otherwise stated.
Demographic and clinical characteristics of the US Medicare beneficiaries undergoing intact or ruptured AAA repair are shown in 3-year increments in Table 1 (data are available by year, see Table, Supplemental Digital Content 1, which also includes data on non-operative rupture patients). The mean age of patients undergoing intact AAA repair increased from 73.7 years in 1995 to 75.5 years in 2008. Similarly, the mean age of patients undergoing ruptured AAA repair (open or EVAR) increased from a mean of 75.3 years in 1995 to 76.4 years in 2008. Patients receiving open repair of intact AAA had a higher prevalence of comorbid conditions in 2008 as compared to 1995.
Table 1.
Demographic and comorbidity characteristics of US Medicare beneficiaries undergoing open repair and EVAR of intact and ruptured AAAs showing significant trends across time from 1995–2008 (in 3 year increments).
| Intact Repairs
|
Trends Across All Years (1995–2008) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1995–1997 | 1998–2000 | 2001–2003 | 2004–2006 | 2007–2008 | ||||||||||
|
|
||||||||||||||
| Annual number of repairs | Open | EVAR | Open | EVAR | Open | EVAR | Open | EVAR | Open | EVAR | Open | EVAR | ||
|
| ||||||||||||||
| 24347 | 363 | 21756 | 1320 | 15507 | 10102 | 10568 | 16018 | 6518 | 19181 | T-statistic | P value | T-statistic | P value | |
| Age (mean) | 73.9 | 75.3 | 74.3 | 75.4 | 74.3 | 75.7 | 74.2 | 75.9 | 74.0 | 76.0 | 1.81 | 0.10 | 6.99 | < 0.001 |
| < 65 | 3% | 3% | 3% | 2% | 4% | 3% | 4% | 3% | 5% | 3% | 6.31 | < 0.001 | 1.04 | 0.32 |
| 65–69 | 22% | 19% | 19% | 17% | 19% | 16% | 21% | 16% | 22% | 17% | −1.29 | 0.22 | 1.78 | 0.11 |
| 70–74 | 31% | 27% | 29% | 26% | 28% | 24% | 26% | 23% | 26% | 22% | −11.34 | < 0.001 | −7.13 | < 0.001 |
| 75–79 | 26% | 26% | 28% | 27% | 28% | 28% | 27% | 26% | 26% | 25% | 0.84 | 0.42 | −5.48 | < 0.001 |
| 80–84 | 13% | 17% | 15% | 18% | 16% | 20% | 16% | 20% | 15% | 20% | 4.66 | < 0.01 | 1.46 | 0.18 |
| ≥ 85 | 4% | 9% | 5% | 9% | 5% | 9% | 6% | 11% | 6% | 13% | 4.80 | <0.001 | 8.32 | < 0.001 |
| Gender (%Male) | 77% | 86% | 76% | 85% | 74% | 84% | 73% | 82% | 70% | 81% | −9.66 | < 0.001 | −9.27 | < 0.001 |
| Race | ||||||||||||||
| White | 95% | 97% | 95% | 96% | 94% | 95% | 93% | 94% | 93% | 94% | −7.73 | < 0.001 | −3.79 | < 0.01 |
| Black | 3% | 0% | 3% | 2% | 4% | 3% | 4% | 3% | 4% | 4% | 2.91 | 0.01 | 5.61 | < 0.001 |
| Other | 2% | 3% | 2% | 2% | 2% | 2% | 3% | 3% | 3% | 2% | 4.36 | < 0.01 | −0.42 | 0.69 |
| Comorbidities | ||||||||||||||
| CHF | 13% | 9% | 12% | 11% | 12% | 9% | 13% | 9% | 10% | 8% | −1.63 | 0.13 | −2.70 | 0.02 |
| Valvular disease | 6% | 5% | 6% | 5% | 6% | 6% | 8% | 7% | 6% | 6% | 3.16 | < 0.01 | 0.02 | 0.98 |
| PVD | 20% | 25% | 20% | 24% | 22% | 21% | 23% | 21% | 26% | 23% | 6.35 | < 0.001 | 2.49 | 0.03 |
| Hypertension | 44% | 46% | 49% | 53% | 54% | 58% | 55% | 62% | 51% | 61% | 6.06 | < 0.001 | 3.15 | 0.01 |
| COPD | 34% | 25% | 34% | 30% | 38% | 31% | 41% | 33% | 35% | 31% | 3.81 | < 0.01 | 0.40 | 0.70 |
| Obesity | 2% | 3% | 2% | 3% | 2% | 3% | 3% | 4% | 3% | 5% | 4.56 | < 0.01 | 8.20 | < 0.001 |
| Renal Disease | 0% | 1% | 0% | 0% | 0% | 0% | 1% | 1% | 1% | 0% | 2.55 | 0.03 | 0.57 | 0.58 |
| CVD | 5% | 7% | 5% | 5% | 5% | 4% | 5% | 4% | 5% | 5% | −1.11 | 0.29 | 2.06 | 0.07 |
| Diabetes | 8% | 10% | 9% | 12% | 10% | 13% | 12% | 15% | 12% | 17% | 12.58 | < 0.001 | 10.82 | < 0.001 |
|
| ||||||||||||||
| Rupture Repairs | ||||||||||||||
|
| ||||||||||||||
| Annual number of repairs | Open | EVAR | Open | EVAR | Open | EVAR | Open | EVAR | Open | EVAR | Open | EVAR | ||
|
| ||||||||||||||
| 4713 | 4038 | 3172 | 260 | 2205 | 401 | 1619 | 616 | T-statistic | P value | T-statistic | P value | |||
|
| ||||||||||||||
| Age (mean) | 75.5 | 76.0 | 76.0 | 76.9 | 76.1 | 77.1 | 76.1 | 77.1 | 5.03 | < 0.001 | 1.41 | 0.20 | ||
| < 65 | 3% | 3% | 3% | 2% | 3% | 4% | 3% | 4% | 1.60 | 0.14 | 1.60 | 0.15 | ||
| 65–69 | 19% | 17% | 17% | 16% | 17% | 14% | 18% | 16% | −1.82 | 0.09 | −0.52 | 0.62 | ||
| 70–74 | 27% | 25% | 23% | 20% | 22% | 20% | 22% | 18% | −8.32 | < 0.001 | −0.96 | 0.37 | ||
| 75–79 | 25% | 26% | 25% | 24% | 25% | 21% | 22% | 19% | −0.87 | 0.40 | −2.90 | 0.02 | ||
| 80–84 | 17% | 18% | 19% | 22% | 20% | 23% | 21% | 21% | 7.15 | < 0.001 | −0.49 | 0.64 | ||
| ≥85 | 11% | 12% | 13% | 17% | 13% | 18% | 14% | 22% | 3.97 | < 0.01 | 4.28 | < 0.01 | ||
| Gender (%Male) | 78% | 78% | 76% | 74% | 74% | 76% | 74% | 77% | −7.12 | < 0.001 | 1.21 | 0.27 | ||
| Race | ||||||||||||||
| White | 94% | 94% | 93% | 92% | 93% | 90% | 92% | 89% | −6.19 | < 0.001 | −3.21 | 0.02 | ||
| Black | 3% | 4% | 4% | 6% | 4% | 8% | 4% | 7% | 2.62 | 0.02 | 1.27 | 0.25 | ||
| Other | 3% | 2% | 3% | 2% | 3% | 2% | 4% | 4% | 3.31 | < 0.01 | 2.42 | 0.05 | ||
| Comorbidities | ||||||||||||||
| CHF | 18% | 18% | 17% | 20% | 17% | 18% | 11% | 13% | −3.29 | < 0.01 | −3.57 | < 0.01 | ||
| Valvular disease | 3% | 3% | 4% | 5% | 4% | 6% | 3% | 4% | 0.66 | 0.52 | −0.64 | 0.54 | ||
| PVD | 9% | 9% | 9% | 12% | 9% | 15% | 12% | 15% | 1.63 | 0.13 | 1.54 | 0.17 | ||
| Hypertension | 27% | 31% | 32% | 37% | 31% | 40% | 28% | 38% | 2.22 | 0.05 | −0.28 | 0.79 | ||
| COPD | 31% | 33% | 35% | 33% | 35% | 37% | 26% | 29% | 0.47 | 0.65 | −1.88 | 0.10 | ||
| Obesity | 2% | 2% | 3% | 2% | 3% | 2% | 2% | 3% | 2.75 | 0.02 | 1.27 | 0.24 | ||
| Renal Disease | 0% | 0% | 1% | 1% | 1% | 2% | 1% | 1% | 3.63 | < 0.01 | 0.63 | 0.55 | ||
| CVD | 4% | 4% | 3% | 4% | 3% | 4% | 4% | 5% | −1.31 | 0.21 | 0.57 | 0.58 | ||
| Diabetes | 6% | 6% | 7% | 9% | 8% | 9% | 7% | 12% | 4.67 | < 0.01 | 3.46 | 0.01 | ||
CHF = congestive heart failure; PVD = peripheral vascular disease; COPD = chronic obstructive pulmonary disease; CVD = cerebral vascular disease
Rates of Repair of Intact and Ruptured AAA
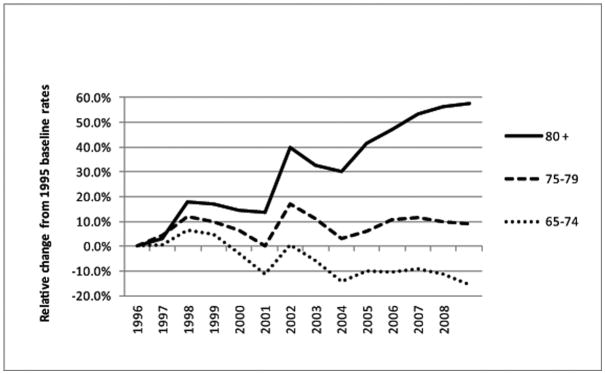
The overall rate of intact repair (age and gender adjusted) increased slightly (yet still significant statistically) from 79.9 to 85.0 per 100,000 Medicare beneficiaries over the period 1995 to 2008. Intact repair rates decreased in those aged 65–74 (81.8 to 68.9), but increased in all other age groups, with the largest increase in those aged 80 and older (57.7 to 92.3). Figure 1 shows changes in intact repair rates over time within these age groups relative to the baseline year (1995). Although the majority of intact repairs were in men, the increase in repairs was greater in women (10.2% increase in repairs in women vs. a 5.4% increase in men).
Figure 1.
Changes in intact AAA repair rates subsequent to 1995 by age and year (gender adjusted)
The rate of AAA ruptures presenting to a hospital (age and gender adjusted) decreased from 33.4 to 16.8 per 100,000 Medicare Beneficiaries between 1995 and 2008, while the proportion of ruptures undergoing repair changed little over the same time period (70% in 1995 vs. 65% in 2008).
The proportion of intact repairs using EVAR increased steadily over time, reaching 77% in 2008 for all age groups and 83% for those over age 80 (see Figure, Supplemental Digital Content 2, which shows proportion of EVAR for intact and ruptured AAA). Men were more likely to undergo EVAR compared to women for all age groups in 2008; 79% vs.67% (data not shown). Although EVAR utilization for rupture repair has lagged behind that for intact repair, it grew to 31% in 2008.
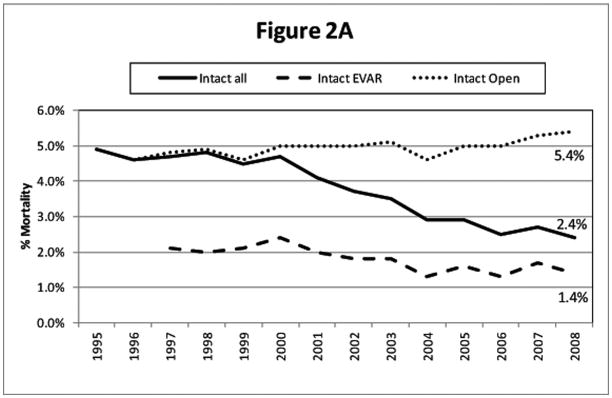
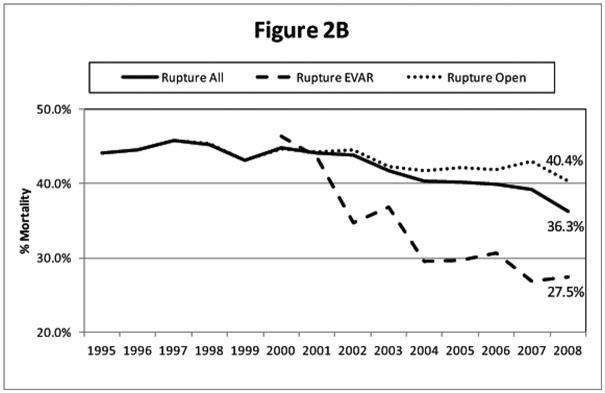
Operative Mortality
Operative mortality with intact repair declined over time after the introduction of EVAR (Figure 2a). Operative mortality with open repair remained fairly constant near 5%, so most of this decrease was due to the adoption of EVAR. The reduction in mortality with intact repair was greatest for those over age 80 (9.6% in 1995 to 3.3% in 2008). Patients aged 65–74 had a smaller absolute reduction in mortality (3.3% to 1.5%). Operative mortality was higher for women than men for both endovascular repair (2.1% vs. 1.3% in 2008) and open repair (7.0% vs. 5.2% in 2008, p<0.01) and this difference has changed little over time. Similarly, after the introduction of EVAR, the overall operative mortality with ruptured AAA repair declined from 44.1% in 1995 to 36.3% in 2008 (Figure 2b).
Figure 2.
Operative mortality for EVAR, open repair, and total AAA repairs for US Medicare beneficiaries, 1995–2008 A) Intact AAA B) Ruptured AAA
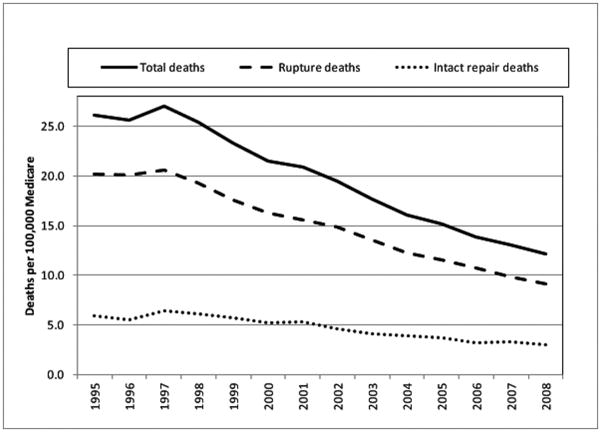
Short-term AAA-related deaths
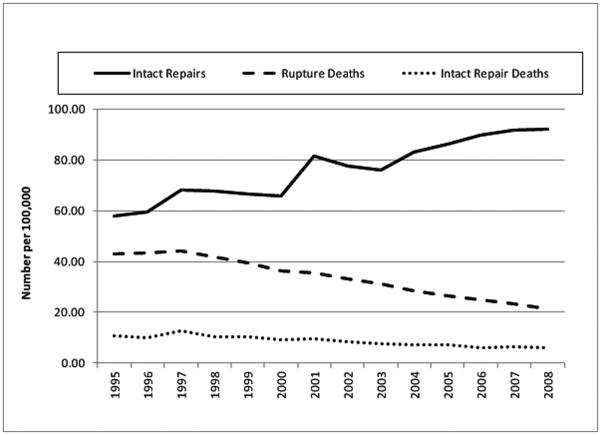
Between 1995 and 2008, the overall rate of short-term AAA-related deaths for those presenting to a hospital (age and gender adjusted) per 100,000 Medicare beneficiaries declined from 26.1 to 12.1 (Figure 3). This is due mostly to a 50% decline in the rate of ruptures and resulting deaths, which decreased from 20.2 to 9.1 per 100,000 beneficiaries. In addition, despite the increase in intact repairs, there was a decline in the rate of deaths related to intact repair from 5.9 to 3.0 per 100,000 beneficiaries (age and gender adjusted). The decline in all short-term AAA-related deaths was seen for both men and women and across all age groups with the greatest decline seen in those aged 80 and older (see Figure, Supplemental Digital Content 3, which shows all short-term AAA-related deaths per age group). Similarly, the decline in intact repair deaths and rupture deaths (with and without repair) was greatest in those aged 80 and older (see Figures, Supplemental Digital Content 4 and 5, which show intact repair deaths and rupture deaths per age group respectively). Figure 4 shows that as the rate of intact AAA repair increased for those aged 80 and older there was a concomitant 50% decrease in rupture-related deaths as well as a decrease in deaths due to intact AAA repair in that age group.
Figure 3.
Short-term AAA related deaths per 100,000 US Medicare beneficiaries (age and gender adjusted), 1995–2008
Figure 4.
Intact AAA repairs, rupture deaths (with and without repair), and intact repair deaths in patients aged 80 and older (gender adjusted, per 100,000 Medicare Beneficiaries), 1995–2008
Discussion
We studied trends in short-term AAA-related mortality over the period 1995–2008, which coincided with the period just prior to and following the introduction of EVAR, and calculated standardized rates to correct for population changes. By using complete data from the Medicare program, we were able to capture all deaths within 30 days of presentation in a large population encompassing most AAA repairs and deaths in the US. Our analysis has several key findings. First, rates of intact AAA repair increased dramatically in those over age 80 and decreased somewhat in those younger than 75 years. Despite the increase in intact repair rates in those over age 80, operative mortality decreased by 50% because of the adoption of EVAR with its lower (and decreasing) mortality rates. Second, the incidence of AAA rupture has decreased dramatically over time, with 50% fewer deaths due to rupture observed in 2008 compared with 1995. Because most ruptures occur in the oldest population, this finding is likely due to increasing rates of prophylactic elective repair in that population. Together, these trends have resulted in a marked decline in short-term AAA-related mortality over time, largely coinciding with the introduction and rise of EVAR.
In our previous work using the Nationwide Inpatient Sample, years 1993–2005, we previously demonstrated that the average annual number of deaths from intact and ruptured AAA decreased significantly after the introduction of EVAR.7 However, the analysis did not account for changes in the in the population over time, was limited to in-hospital mortality, and was based on a 20% sample of hospitalizations. In contrast, the current study includes all Medicare beneficiaries and also includes uniform data on short-term outcomes observed after discharge from the hospital. We now demonstrate substantial differences based on age and demonstrate changes occurring annually rather than 5 year averages.
Short-term AAA-related deaths in the US are decreasing due to both fewer deaths after intact repair (despite an increase in repair rates primarily in those over age 80) and decreased incidence of rupture. Another contributing factor to decreased mortality from AAA rupture is that there may have been a change in the underlying prevalence of AAA. Prior epidemiologic studies based on data through 2000 have suggested an increasing or at least stable rate of AAA incidence, 12–17 but these studies are now over 10 years old. The population most likely to show decreased incidence of AAA are the youngest Medicare beneficiaries who might have benefitted most from lower smoking rates, and other risk factor control.18 Our data also are consistent with this hypothesis. In younger patients (those aged 65–74) we observed a decrease in the rate of rupture despite a decrease in the rate of intact repair. The decline in repair rate in this age group also may be related in part to the UK Small Aneurysm Trial and the subsequent Aneurysm Detection and Management trial, both of which demonstrated the safety of deferring AAA repair until the diameter reaches 5.5cm.19,20 The fact that the rupture rate declined in this age group despite a decreasing rate of intact repair suggests that for the first time, the incidence of AAA may be declining in younger patients. In contrast to younger patients, we observed markedly increased rates of intact repair for those aged 80 and older along with a similar decrease in ruptures in that population. It is unlikely that we would have seen this dramatic increase if the prevalence of AAA was decreasing in this older population
Prior to the introduction of EVAR, rates of AAA rupture and intact repair were generally stable,1,14–17,21–23 although some more recent studies that include the early years after the introduction of EVAR showed a decreasing rate of intact repairs.7,8,24,25 For instance, Dillavou et al found a decrease in intact repairs from 1994–2003 in a 5% sample of Medicare patients24 whereas Nowygrod et al found a stable rate of intact repair from 1998–2003 using state and national hospital discharge data.25 We find that the increase in intact repairs likely coincided with the introduction of EVAR. Close inspection reveals a spike in intact repairs in 2001 after FDA approval of EVAR with a small decline in the years just before and after. It is likely that elective repair was deferred in those patients who were deemed most likely to benefit from EVAR in the years just before its introduction and that the small decline occurred after this backlog was eliminated. These overall trends, however, mask important differences by age group. Our analysis demonstrates that intact repair rates have been increasing dramatically in those over age 80 since 1995 but that this increase is partially offset by a decrease in repair rates in those under age 75.
Although EVAR has expanded access to repair, particularly for the oldest patients, we cannot confirm that life expectancy has been prolonged meaningfully because although rupture may have been prevented, these patients may have died from other competing causes soon afterward. Thus, the benefit in reduction of short-term AAA-related mortality may not persist when examining the long-term benefits of EVAR. What is unambiguous, however, is that we observe fewer ruptures in this population. The recent EVAR 2 trial suggests that EVAR for unfit patients does not prolong survival.26 We did not evaluate “fitness” and have simply noted trends based on age alone. We previously demonstrated that although operative mortality increases with age, a low mortality can be achieved even in Medicare patients 85 years of age and older (inhospital mortality of only 2.7%).6 Operative mortality in EVAR 2 was 9% suggesting that these patients were substantially less “fit”. In addition to age, comorbid conditions can be used to more precisely predict the operative risk with EVAR and open surgery for all age groups to help select those who may be at reasonable risk for EVAR even if they are high risk for open repair.27,28
We found a lower operative mortality with EVAR when compared to open repair for ruptured AAA similar to others. 24,27,29 It has been suggested that only the most stable ruptured patients are chosen for EVAR and that mortality for EVAR and open repair of ruptured AAA may not be different.30,31 However, prior to the introduction of EVAR, rupture repair mortality had been stable.23 Our analysis demonstrates a reduction in overall rupture repair mortality after the introduction of EVAR providing the strongest argument in favor of a real reduction in operative mortality with EVAR for ruptures as well as intact AAA.
There are several limitations to this study. The administrative data we used is subject to coding errors and thus we might have missed some cases of repair. The trends we report, however, would not be subject to such a bias unless coding accuracy was changing over time. Similarly, we were only able to identify rupture-related deaths that reached a hospital and most rupture patients likely die prior to reaching the hospital. However, we have no reason to suspect that the proportion of ruptures reaching the hospital would be changing over time; if anything we would expect that more ruptures would be reaching the hospitals because of improvements in the emergency response system.32,33 We also do not have the ability to determine why the proportion of patients admitted with ruptured AAA who are not offered repair has not changed substantially. We would hypothesize that some patients present either with the expressed desire not to undergo repair or present with an unrecoverable situation and that the expansion of EVAR would not impact this. Our analysis is also limited by a lack of anatomic information. We do not know AAA diameter and therefore cannot comment on changes in practice over time related to diameter. However, based on the age related trends we observed, we suspect that the increased utilization of EVAR represents an increase in the treatment of the elderly (age 80 and older) with larger diameter AAAs rather than expansion to treatment of smaller diameter AAAs.
In summary, coincident with the introduction of EVAR, we observed large population level declines in short-term AAA-related mortality among elderly Medicare Beneficiaries. This is due to both decreased perioperative mortality and decreased deaths due to ruptures of untreated (and treated) aneurysms, particularly in older patients. Expansion of the Medicare screening program and others could be expected to provide further benefits in reducing the AAA rupture rate nationally. Utilization of EVAR continues to expand for both intact and ruptured AAA suggesting that these trends will likely continue. Our data also suggest that AAA incidence might be decreasing in younger patients, potentially due to less smoking and improved risk factor control, but this finding will need to be confirmed in other studies.
Supplementary Material
Acknowledgments
This work was supported by the NIH T32 Harvard-Longwood Research Training in Vascular Surgery grant HL007734, the NIH grant 1RC4MH092717-01 for comparative effectiveness research, and the NHLBI R01 grant HL105453.
Footnotes
The opinions expressed do not necessarily represent the views or policy positions of the Centers for Medicare and Medicaid Services.
Conflicts of Interest and Source of Funding: Marc L. Schermerhorn is on the Endologix Data Safety and Monitoring Board and is a Medtronic consultant. Bruce E. Landon has received a Gore Unrestricted Educational Grant. For the remaining authors none were declared.
References
- 1.Bengtsson H, Bergqvist D. Ruptured abdominal aortic aneurysm: a population-based study. J Vasc Surg. 1993;18:74–80. doi: 10.1067/mva.1993.42107. [DOI] [PubMed] [Google Scholar]
- 2.Bengtsson H, Bergqvist D, Sternby NH. Increasing prevalence of abdominal aortic aneurysms. A necropsy study. Eur J Surg. 1992;158:19–23. [PubMed] [Google Scholar]
- 3.Greenhalgh RM, Brown LC, Kwong GP, et al. Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial. Lancet. 2004;364:843–8. doi: 10.1016/S0140-6736(04)16979-1. [DOI] [PubMed] [Google Scholar]
- 4.Lederle FA, Freischlag JA, Kyriakides TC, et al. Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA. 2009;302:1535–42. doi: 10.1001/jama.2009.1426. [DOI] [PubMed] [Google Scholar]
- 5.Prinssen M, Verhoeven EL, Buth J, et al. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2004;351:1607–18. doi: 10.1056/NEJMoa042002. [DOI] [PubMed] [Google Scholar]
- 6.Schermerhorn ML, O’Malley AJ, Jhaveri A, et al. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med. 2008;358:464–74. doi: 10.1056/NEJMoa0707348. [DOI] [PubMed] [Google Scholar]
- 7.Giles KA, Pomposelli F, Hamdan A, et al. Decrease in total aneurysm-related deaths in the era of endovascular aneurysm repair. J Vasc Surg. 2009;49:543–50. doi: 10.1016/j.jvs.2008.09.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwarze ML, Shen Y, Hemmerich J, et al. Age-related trends in utilization and outcome of open and endovascular repair for abdominal aortic aneurysm in the United States, 2001–2006. J Vasc Surg. 2009;50:722–9. e2. doi: 10.1016/j.jvs.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 9.Federle MP. Current status and future trends in abdominal CT. Radiographics. 1998;18:1555–68. doi: 10.1148/radiographics.18.6.9821199. [DOI] [PubMed] [Google Scholar]
- 10.Levin DC, Rao VM, Parker L, et al. Recent trends in utilization rates of abdominal imaging: the relative roles of radiologists and nonradiologist physicians. J Am Coll Radiol. 2008;5:744–7. doi: 10.1016/j.jacr.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 11.Bernhard VM, Mitchell RS, Matsumura JS, et al. Ruptured abdominal aortic aneurysm after endovascular repair. J Vasc Surg. 2002;35:1155–62. doi: 10.1067/mva.2002.123758. [DOI] [PubMed] [Google Scholar]
- 12.Ashton HA, Buxton MJ, Day NE, et al. The Multicentre Aneurysm Screening Study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial. Lancet. 2002;360:1531–9. doi: 10.1016/s0140-6736(02)11522-4. [DOI] [PubMed] [Google Scholar]
- 13.Best VA, Price JF, Fowkes FG. Persistent increase in the incidence of abdominal aortic aneurysm in Scotland, 1981–2000. Br J Surg. 2003;90:1510–5. doi: 10.1002/bjs.4342. [DOI] [PubMed] [Google Scholar]
- 14.Blanchard JF. Epidemiology of abdominal aortic aneurysms. Epidemiol Rev. 1999;21:207–21. doi: 10.1093/oxfordjournals.epirev.a017997. [DOI] [PubMed] [Google Scholar]
- 15.Gillum RF. Epidemiology of aortic aneurysm in the United States. J Clin Epidemiol. 1995;48:1289–98. doi: 10.1016/0895-4356(95)00045-3. [DOI] [PubMed] [Google Scholar]
- 16.Melton LJ, 3rd, Bickerstaff LK, Hollier LH, et al. Changing incidence of abdominal aortic aneurysms: a population-based study. Am J Epidemiol. 1984;120:379–86. doi: 10.1093/oxfordjournals.aje.a113902. [DOI] [PubMed] [Google Scholar]
- 17.Wilmink AB, Quick CR. Epidemiology and potential for prevention of abdominal aortic aneurysm. Br J Surg. 1998;85:155–62. doi: 10.1046/j.1365-2168.1998.00714.x. [DOI] [PubMed] [Google Scholar]
- 18.Tynan M, Pechacek T, McKenna M, et al. Centers for Disease Control and Prevention. [Accessed November 4th, 2010];CDC Grand Rounds: Current Opportunities in Tobacco Control. 2010 Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5916a3.htm.
- 19.Mortality results for randomised controlled trial of early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. The UK Small Aneurysm Trial Participants. Lancet. 1998;352:1649–55. [PubMed] [Google Scholar]
- 20.Lederle FA, Wilson SE, Johnson GR, et al. Immediate repair compared with surveillance of small abdominal aortic aneurysms. N Engl J Med. 2002;346:1437–44. doi: 10.1056/NEJMoa012573. [DOI] [PubMed] [Google Scholar]
- 21.Drott C, Arfvidsson B, Ortenwall P, et al. Age-standardized incidence of ruptured aortic aneurysm in a defined Swedish population between 1952 and 1988: mortality rate and operative results. Br J Surg. 1992;79:175–9. doi: 10.1002/bjs.1800790228. [DOI] [PubMed] [Google Scholar]
- 22.Eickhoff JH. Incidence of diagnosis, operation and death from abdominal aortic aneurysms in Danish hospitals: results from a nation-wide survey, 1977–1990. Eur J Surg. 1993;159:619–23. [PubMed] [Google Scholar]
- 23.Heller JA, Weinberg A, Arons R, et al. Two decades of abdominal aortic aneurysm repair: have we made any progress? J Vasc Surg. 2000;32:1091–100. doi: 10.1067/mva.2000.111691. [DOI] [PubMed] [Google Scholar]
- 24.Dillavou ED, Muluk SC, Makaroun MS. A decade of change in abdominal aortic aneurysm repair in the United States: Have we improved outcomes equally between men and women? J Vasc Surg. 2006;43:230–8. doi: 10.1016/j.jvs.2005.09.043. [DOI] [PubMed] [Google Scholar]
- 25.Nowygrod R, Egorova N, Greco G, et al. Trends, complications, and mortality in peripheral vascular surgery. J Vasc Surg. 2006;43:205–16. doi: 10.1016/j.jvs.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 26.Greenhalgh RM, Brown LC, Powell JT, et al. Endovascular repair of aortic aneurysm in patients physically ineligible for open repair. N Engl J Med. 2010;362:1872–80. doi: 10.1056/NEJMoa0911056. [DOI] [PubMed] [Google Scholar]
- 27.Egorova N, Giacovelli JK, Gelijns A, et al. Defining high-risk patients for endovascular aneurysm repair. J Vasc Surg. 2009;50:1271–9. e1. doi: 10.1016/j.jvs.2009.06.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giles KA, Schermerhorn ML, O’Malley AJ, et al. Risk prediction for perioperative mortality of endovascular vs open repair of abdominal aortic aneurysms using the Medicare population. J Vasc Surg. 2009;50:256–62. doi: 10.1016/j.jvs.2009.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mureebe L, Egorova N, Giacovelli JK, et al. National trends in the repair of ruptured abdominal aortic aneurysms. J Vasc Surg. 2008;48:1101–7. doi: 10.1016/j.jvs.2008.06.031. [DOI] [PubMed] [Google Scholar]
- 30.Mastracci TM, Garrido-Olivares L, Cina CS, et al. Endovascular repair of ruptured abdominal aortic aneurysms: a systematic review and meta-analysis. J Vasc Surg. 2008;47:214–21. doi: 10.1016/j.jvs.2007.07.052. [DOI] [PubMed] [Google Scholar]
- 31.Hinchliffe RJ, Bruijstens L, MacSweeney ST, et al. A randomised trial of endovascular and open surgery for ruptured abdominal aortic aneurysm - results of a pilot study and lessons learned for future studies. Eur J Vasc Endovasc Surg. 2006;32:506–13. doi: 10.1016/j.ejvs.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 32.Farooq MM, Freischlag JA, Seabrook GR, et al. Effect of the duration of symptoms, transport time, and length of emergency room stay on morbidity and mortality in patients with ruptured abdominal aortic aneurysms. Surgery. 1996;119:9–14. doi: 10.1016/s0039-6060(96)80206-6. [DOI] [PubMed] [Google Scholar]
- 33.Haveman JW, Karliczek A, Verhoeven EL, et al. Results of streamlined regional ambulance transport and subsequent treatment of acute abdominal aortic aneurysms. Emerg Med J. 2006;23:807–10. doi: 10.1136/emj.2006.037879. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.