Abstract
OBJECTIVE
To evaluate the natural history of gastric emptying in diabetes.
RESEARCH DESIGN AND METHODS
Thirteen patients with diabetes (12, type 1; 1, type 2) had measurements of gastric emptying, blood glucose levels, glycated hemoglobin, upper gastrointestinal symptoms, and autonomic nerve function at baseline and after 24.7 ± 1.5 years.
RESULTS
There was no change in gastric emptying of either solids (% retention at 100 min) (baseline 58.5 ± 5% vs. follow-up 51.9 ± 8%; P = 0.35) or liquids (50% emptying time) (baseline 29.8 ± 3 min vs. follow-up 34.3 ± 6 min; P = 0.37). Gastric emptying of solid at follow-up was related to emptying at baseline (r = 0.56, P < 0.05). At follow-up, blood glucose concentrations were lower (P = 0.006), autonomic function deteriorated (P = 0.03), and gastrointestinal symptoms remained unchanged (P = 0.17).
CONCLUSIONS
In unselected patients with diabetes, gastric emptying appears remarkably stable over 25 years.
There is limited information about the natural history of gastric emptying in diabetes (1–3). We have reported that gastric emptying and symptoms changed little after 12 years of follow-up, possibly because a deterioration in autonomic function was counteracted by better glycemic control (4). We reexamined patients from the same cohort after 25 years.
RESEARCH DESIGN AND METHODS
We studied 13 patients (9 female) with diabetes (12, type 1; 1, type 2) in whom gastric emptying was measured in 1984–1989 (duration of follow-up 24.7 ± 1.5 years). Age was 61 ± 8 years at follow-up, and duration of known diabetes was 38 ± 8 years. Baseline (5,6) and longitudinal (4) measurements in this cohort have been reported. Fifty-three of the original 86 patients were known to be alive; 30 were contactable, and 13 of these patients agreed to participate. When compared with the other 73 patients, those who participated were younger at entry (36.4 ± 2.2 vs. 49.3 ± 1.7 years, P = 0.003), but did not differ in regard to BMI, duration of known diabetes, symptom or autonomic function scores, proportion who smoked, or rates of solid or liquid emptying at baseline. No subject was taking medication known to affect gastrointestinal motility, and smoking was forbidden on the day of the test. Written, informed consent was obtained, and the protocol was approved by the Royal Adelaide Hospital Research Ethics Committee (protocol 091221).
Gastric emptying was measured in the morning after an overnight fast, after administering the patient’s usual insulin dose, using a dual-isotope technique (100-g minced beef labeled with 20-mBq 99mTc sulfur colloid, and 150-mL 10% dextrose labeled with 25–37 mBq 113m indium-diethylenetriaminepentaacetic acid at baseline, and 8 mBq 67Ga-ethylenediaminetetraacetic acid at follow-up (4,6,7). Solid emptying was expressed as percentage remaining in the stomach at 100 min (T100min), and liquid emptying as 50% emptying time (T50%). Gastric emptying was classified as normal or abnormal using an established control range (solid T100min [12–61%] and liquid T50% [8–31 min]) (4,6).
At baseline and follow-up, glycated hemoglobin (HbA1c), plasma creatinine, and blood glucose were measured from an initial venous sample; blood glucose was also measured 30, 60, 90, and 120 min after meal ingestion (4).
Gastric and esophageal symptoms were assessed by a validated questionnaire (6), with a maximum score of 27.
Autonomic nerve function was evaluated by cardiovascular reflex tests (variation in heart rate during deep breathing; heart rate response and fall in systolic blood pressure after standing) (6,7). Each test was scored as 0 (normal), 1 (borderline), or 2 (abnormal). A total score ≥3 was taken to indicate definite autonomic neuropathy.
Statistical analysis
Data were normally distributed and comparisons between baseline and follow-up were evaluated using paired t tests and linear regression analysis, with the exception of autonomic function and symptom scores that were evaluated by Wilcoxon signed rank tests. The sample size of 13 had 80% power to detect a difference in solid emptying of one-third from the baseline value, at P < 0.05 significance. Data are mean ± SEM (or median [interquartile range] for nonparametric data).
RESULTS
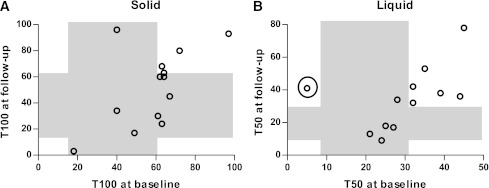
Gastric emptying of solids was abnormally slow in 8 of 13 patients at baseline, and 5 of 13 at follow-up. In one patient, gastric emptying of liquid was not evaluated at follow-up because 67Ga-ethylenediaminetetraacetic acid was unavailable. Liquid emptying was abnormally slow in 6 of 12 patients at baseline and 8 of 12 at follow-up. There was no change in gastric emptying of either solid (P = 0.35) or liquid (P = 0.37), and the rate of solid emptying at baseline was related to emptying at follow-up (r = 0.56, P < 0.05), with a trend for the liquid component (r = 0.49, P = 0.11), which became significant (r = 0.82, P = 0.002) on excluding one subject with abnormally rapid emptying at follow-up (Fig. 1).
Figure 1.
Measurements of gastric emptying of (A) solid (r = 0.56, P < 0.05, n = 13) and (B) liquid (r = 0.49, P = 0.11, n = 12) components at baseline and follow-up. The normal ranges are shown in the shaded areas. The relationship is significant for liquid emptying (r = 0.82, P = 0.002) if one data point (circled; representing a type 1 diabetic patient) is removed.
Blood glucose concentrations (mean over 120 min) were lower at follow-up than baseline (12.8 ± 1.0 vs. 17.7 ± 1.1 mmol/L, P = 0.006), and HbA1c was nonsignificantly lower (7.2 ± 0.3 vs. 8.1 ± 0.7% [55 ± 3 vs. 65 ± 8 mmol/mol], P = 0.25). Plasma creatinine was unchanged between baseline and follow-up (0.085 ± 0.03 vs. 0.082 ± 0.03 mmol/L).
There was no difference in total (baseline 3 [4] vs. follow-up 3 [6], P = 0.17), gastric (P = 0.31), or esophageal (P = 0.73) symptom scores.
At follow-up, autonomic nerve function was not assessed in one patient with atrial fibrillation. Three of the 12 patients had definite autonomic neuropathy at baseline and 8 at follow-up; the total score was lower at baseline (1 [3] vs. 4 [2], P = 0.03).
CONCLUSIONS
This study represents the most prolonged longitudinal evaluation of gastric emptying in diabetes. After ∼25 years, there was no change in gastric emptying of solids and liquids, or symptom scores, whereas autonomic function deteriorated, but glycemic control improved. The latter is likely to reflect the increased attention given to optimizing glycemic control in diabetes. These observations are consistent with our previous longitudinal study (4) and suggest that both gastric emptying and gastrointestinal symptoms are usually stable over time in patients with diabetes. We acknowledge that the number of subjects studied was relatively small, but there was no trend for a change in either gastric emptying or symptoms. Selection bias cannot be excluded, but other than being younger, the baseline characteristics of those studied did not appear exceptional; many patients who declined or could not be contacted had simply moved, or were very elderly.
Delayed gastric emptying in diabetes is not invariably related to irreversible autonomic neuropathy, but rather has a complex and heterogeneous etiology, including loss/dysfunction of interstitial cells of Cajal, and deficient neurotransmission (8). Gastric emptying is also slowed during acute hyperglycemia (9,10). We observed lower blood glucose at follow-up, which might have ameliorated any progression in irreversible pathology.
Gastric emptying at baseline and follow-up were related, certainly for solids and probably also for liquids. Hitherto, there has been limited information about the “reproducibility” of gastric emptying in diabetes (11). Our observations suggest that, as in health (7), the interindividual variation in gastric emptying in diabetes is much greater than intraindividual variation.
In summary, this prospective study indicates that gastric emptying in patients with long-term diabetes is relatively stable over time.
Acknowledgments
This study was funded by a grant awarded by the National Health and Medical Research Council of Australia.
No potential conflicts of interest relevant to this article were reported.
J.C. conducted the study, including preparation of the protocol, subject recruitment, and data collection and analysis, and prepared the manuscript. A.R. assisted in performance of the study, including preparation of the protocol and analysis of gastric emptying data. M.B. assisted in performance of the study. C.K.R. supervised preparation of the protocol and critically reviewed the manuscript. K.L.J. supervised preparation of the protocol and analysis of gastric emptying data, and critically reviewed the manuscript. M.H. conceived the study, supervised preparation of the protocol, and was responsible for final content of the manuscript.
M.H. is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank Ms. Kylie Lange, Centre of Clinical Research Excellence in Nutritional Physiology, Interventions, and Outcomes, Adelaide, South Australia, Australia, who provided biostatistical advice.
References
- 1.Chang J, Rayner CK, Jones KL, Horowitz M. Diabetic gastroparesis-backwards and forwards. J Gastroenterol Hepatol 2011;26(Suppl 1):46–57 [DOI] [PubMed] [Google Scholar]
- 2.Kashyap P, Farrugia G. Diabetic gastroparesis: what we have learned and had to unlearn in the past 5 years. Gut 2010;59:1716–1726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kong MF, Horowitz M, Jones KL, Wishart JM, Harding PE. Natural history of diabetic gastroparesis. Diabetes Care 1999;22:503–507 [DOI] [PubMed] [Google Scholar]
- 4.Jones KL, Russo A, Berry MK, Stevens JE, Wishart JM, Horowitz M. A longitudinal study of gastric emptying and upper gastrointestinal symptoms in patients with diabetes mellitus. Am J Med 2002;113:449–455 [DOI] [PubMed] [Google Scholar]
- 5.Horowitz M, Harding PE, Maddox A, et al. Gastric and oesophageal emptying in insulin-dependent diabetes mellitus. J Gastroenterol Hepatol 1986;1:97–113 [Google Scholar]
- 6.Horowitz M, Maddox AF, Wishart JM, Harding PE, Chatterton BE, Shearman DJ. Relationships between oesophageal transit and solid and liquid gastric emptying in diabetes mellitus. Eur J Nucl Med 1991;18:229–234 [DOI] [PubMed] [Google Scholar]
- 7.Collins PJ, Horowitz M, Cook DJ, Harding PE, Shearman DJ. Gastric emptying in normal subjects—a reproducible technique using a single scintillation camera and computer system. Gut 1983;24:1117–1125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grover M, Farrugia G, Lurken MS, Bernard CE, Faussone-Pellegrini MS, Smyrk TC, Parkman HP, Abell TL, Snape WJ, Hasler WL, Unalp-Arida A, Nguyen L, Koch KL, Calles J, Lee L, Tonascia J, Hamilton FA, Pasricha PJ: Cellular changes in diabetic and idiopathic gastroparesis. Gastroenterology 2011;140:1575–1585 e1578 [DOI] [PMC free article] [PubMed]
- 9.Rayner CK, Samsom M, Jones KL, Horowitz M. Relationships of upper gastrointestinal motor and sensory function with glycemic control. Diabetes Care 2001;24:371–381 [DOI] [PubMed] [Google Scholar]
- 10.Schvarcz E, Palmér M, Aman J, Horowitz M, Stridsberg M, Berne C. Physiological hyperglycemia slows gastric emptying in normal subjects and patients with insulin-dependent diabetes mellitus. Gastroenterology 1997;113:60–66 [DOI] [PubMed] [Google Scholar]
- 11.Lartigue S, Bizais Y, Des Varannes SB, Murat A, Pouliquen B, Galmiche JP. Inter- and intrasubject variability of solid and liquid gastric emptying parameters. A scintigraphic study in healthy subjects and diabetic patients. Dig Dis Sci 1994;39:109–115 [DOI] [PubMed] [Google Scholar]