Abstract
OBJECTIVE
This systematic review and meta-analysis of randomized controlled trials (RCTs) assesses the effect of pharmacist care on cardiovascular disease (CVD) risk factors among outpatients with diabetes.
RESEARCH DESIGN AND METHODS
MEDLINE, EMBASE, CINAHL, and the Cochrane Central Register of Controlled Trials were searched. Pharmacist interventions were classified, and a meta-analysis of mean changes of blood pressure (BP), total cholesterol (TC), LDL cholesterol, HDL cholesterol, and BMI was performed using random-effects models.
RESULTS
The meta-analysis included 15 RCTs (9,111 outpatients) in which interventions were conducted exclusively by pharmacists in 8 studies and in collaboration with physicians, nurses, dietitians, or physical therapists in 7 studies. Pharmacist interventions included medication management, educational interventions, feedback to physicians, measurement of CVD risk factors, or patient-reminder systems. Compared with usual care, pharmacist care was associated with significant reductions for systolic BP (12 studies with 1,894 patients; −6.2 mmHg [95% CI −7.8 to −4.6]); diastolic BP (9 studies with 1,496 patients; −4.5 mmHg [−6.2 to −2.8]); TC (8 studies with 1,280 patients; −15.2 mg/dL [−24.7 to −5.7]); LDL cholesterol (9 studies with 8,084 patients; −11.7 mg/dL [−15.8 to −7.6]); and BMI (5 studies with 751 patients; −0.9 kg/m2 [−1.7 to −0.1]). Pharmacist care was not associated with a significant change in HDL cholesterol (6 studies with 826 patients; 0.2 mg/dL [−1.9 to 2.4]).
CONCLUSIONS
This meta-analysis supports pharmacist interventions—alone or in collaboration with other health care professionals—to improve major CVD risk factors among outpatients with diabetes.
Cardiovascular disease (CVD) is the major cause of death in patients with diabetes and is about two times more frequent in these patients compared with people without diabetes (1). Although studies have demonstrated that control of major CVD risk factors, such as hypertension or dyslipidemia, reduces the risk of cardiovascular complications among patients with diabetes (2–5), CVD risk factors remain poorly controlled in these patients (5–7). Therefore, effective interventions and new models of care are needed to improve management of CVD risk factors among patients with diabetes, particularly in light of the increase in health care costs and the increasing problems with access to primary care physicians in most health care systems (8). A recent systematic review evaluating the effect of pharmacists as team members on patient care in the United States has underlined the integration of pharmacists as a health care team member and provider of health services (9).
Pharmacists can therefore help fill the gap as primary care providers and can contribute to the control of CVD risk factors by their knowledge of medications, their easy accessibility for patients, and their collaborative practice with physicians (9–13). More specifically, pharmacists have the opportunity to provide medication instructions to patients at each prescription, to improve safe medication use, and to assist physicians in chronic care (12,14,15). In a recent meta-analysis, we showed that pharmacist care improves the management of outpatients with major modifiable CVD risk factors (15). However, studies conducted solely in outpatients with diabetes were not included in that meta-analysis. Other reviews have evaluated pharmacist interventions in the management of diabetes but focused solely on glycemic control (16), did not include only randomized controlled trials (RCTs), or did not pool data (17–19). Consequently, the objective of this systematic review and meta-analysis of RCTs is to assess the effect of pharmacist care on major CVD risk factors among outpatients with diabetes.
RESEARCH DESIGN AND METHODS
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement to conduct our systematic review (20).
Inclusion criteria and outcomes
We included studies that 1) had a RCT design; 2) evaluated the effect of pharmacist care delivered by a community, hospital, or clinical pharmacist; 3) among adults outpatients with diabetes (type 1 or 2) and with any modifiable major CVD risk factors (hypertension, dyslipidemia, smoking, or obesity); and 4) compared with a usual care group. Outcomes were systolic and diastolic BP, total cholesterol (TC), LDL cholesterol, HDL cholesterol, and BMI. We did not consider fasting blood glucose or glycosylated hemoglobin (A1C) as outcomes because they are not classical CVD risk factors and, in addition, were recently the subject of a systematic review assessing the effect of pharmacist care on metabolic control among patients with diabetes (16).
Search strategy
In collaboration with a research medical librarian (A.L.C.), electronic databases including MEDLINE via PubMed (1950 to March 2012), EMBASE (1980 to March 2012), CINAHL (1937 to March 2012), and the Cochrane Central Register of Controlled Trials (up to March 2012) were searched for randomized controlled studies of the impact of pharmacist care on major CVD risk factors among outpatients with diabetes, published in any language. Inclusion criteria and methods of analysis were specified in advance and documented in a protocol available upon request.
The PubMed search syntax served as the basis for all search strategies, using Medical Subject Headings (MeSH) and text terms with Boolean operators. The syntax consisted of three search themes intersected by the Boolean term “AND.” MeSH terms included cardiovascular disease-related terms (“Cardiovascular Diseases,” “Dyslipidemias,” “Diabetes Mellitus,” “Smoking,” “Overweight”) and pharmacist-related terms (“Pharmacists,” “Pharmaceutical Services,” “Pharmacy Service, Hospital,” “Pharmacies,” “Pharmacy”). The search was focused on randomized controlled studies using the Cochrane Highly Sensitive Search Strategy for identifying randomized trials in MEDLINE. The search strategy was then adapted for EMBASE, CINAHL, and the Cochrane Central Register of Controlled Trials. In addition to database searches, we also conducted a hand search of bibliographies of all relevant articles. The detailed search strategy used is described in the Supplementary Data online.
Methods of the review
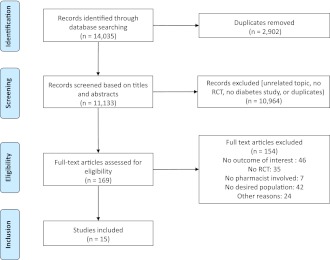
Two reviewers (V.S. and A.C.) independently screened all titles and abstracts and then examined the full text of each potentially eligible article using prespecified inclusion criteria (Fig. 1). Disagreements about study selection were resolved by discussion.
Figure 1.
Selection of studies for systematic review of pharmacist care interventions. (A high-quality color representation of this figure is available in the online issue.)
Data extraction
Two reviewers (V.S. and A.C.) independently extracted data using a standardized collection form. From each included study, the following characteristics were abstracted: 1) study authors and country and year of the publication; 2) study characteristics (study setting and design, duration of follow-up, sample size); 3) characteristics of participants (sex, age, CVD risk factors, medications); 4) characteristics of interventions (description and frequency of the pharmacist intervention); 5) characteristics of the usual care group; and 6) outcome measures (change in BP, TC, LDL cholesterol, HDL cholesterol, and BMI between baseline and follow-up).
Pharmacist interventions were classified using a priori–defined categories based on a recent systematic review of pharmacist care of patients with heart failure (21) as pharmacist-directed care (pharmacist initiated and managed interventions) and pharmacist collaborative care (pharmacist collaborated in interventions conducted by a multidisciplinary healthcare team).
Assessment of the methodological quality of individual studies
Using the Cochrane Risk of Bias Tool (22), two reviewers (V.S. and A.C.) independently assessed the quality (risk of bias) of each study regarding the following domains: adequacy of randomization, concealment of allocation, blinding of outcome assessors, completeness of data, selective outcome reporting, and “other bias.” As recommended, we rated each item as 1) “low risk of bias” if it is unlikely that a bias seriously alters the results; 2) “unclear” if it is plausible that a bias raises some doubt about the results; and 3) “high risk of bias” if it is plausible that a bias seriously weakens confidence in the results. Disagreements were resolved by discussion.
Statistical analysis
Statistical analyses were conducted following the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (22) and the PRISMA statement (20). Data were analyzed using STATA 11.0 software (StataCorp LP, College Station, TX). The meta-analysis was conducted using a random-effects model because of the a priori heterogeneity (15). Pooled intervention effect estimates are reported as weighted mean differences with 95% CI. We calculated SDs from SEs or CIs presented in the reports, if required. The χ2 and I2 statistics were used to assess statistical heterogeneity across studies, with I2 values of 50% or more indicating a substantial level of heterogeneity (22). Post hoc subgroup analyses were conducted according to the type of pharmacist care, the type and the number of interventions, and the setting of care. Funnel plots were drawn, and Egger tests were computed to explore a potential publication bias. Sensitivity analyses were conducted by excluding relatively small studies and restricting analysis to good-quality studies.
RESULTS
Results of the research and the included studies
Initially, 14,035 citations were identified (Fig. 1). After initial screening of titles and abstracts, 169 potentially relevant full-text articles were reviewed for eligibility. The review included 15 RCTs, all published in English, involving 9,111 participants.
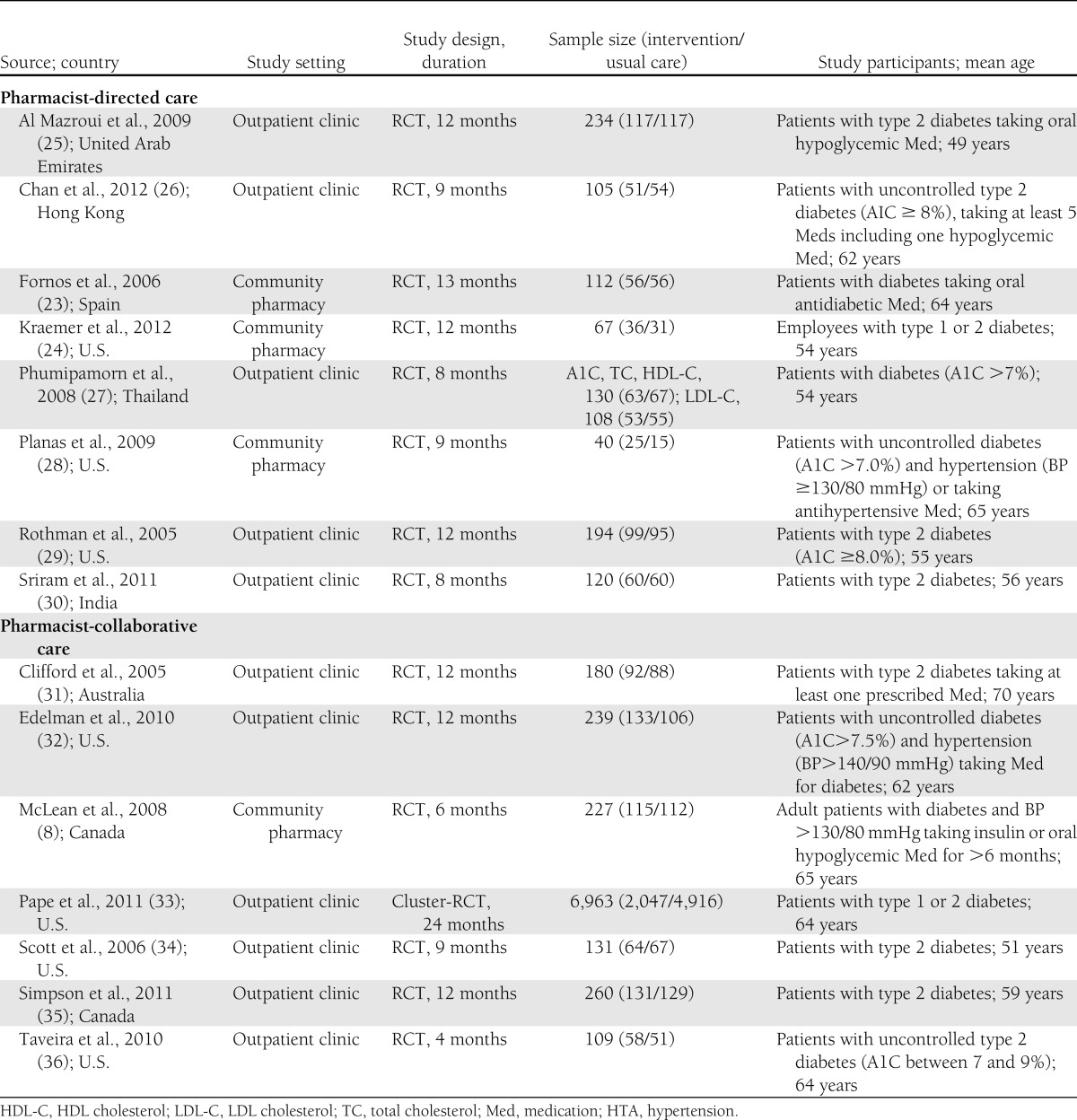
Details of the included studies, including the characteristics of the participants, the interventions of the pharmacist, and the outcome are given in Tables 1 and 2. The 9,111 participants (52% women) were a mean age of 63 years (range 49–70). The mean duration of follow-up was 11 months (range 4–24). Participants were most often followed up in outpatient clinics (12 studies); for example, Veterans Affairs Medical Centers or primary care clinics. Three studies were conducted in community pharmacies (8,23,24). Nine of the 15 studies were conducted in North America (7 in the U.S. and 2 in Canada), 4 in Asia (Thailand, China, United Arab Emirates, and India), 1 in Europe (Spain), and 1 in Australia.
Table 1.
Characteristics of the included studies: study setting and design, sample size, and study participants
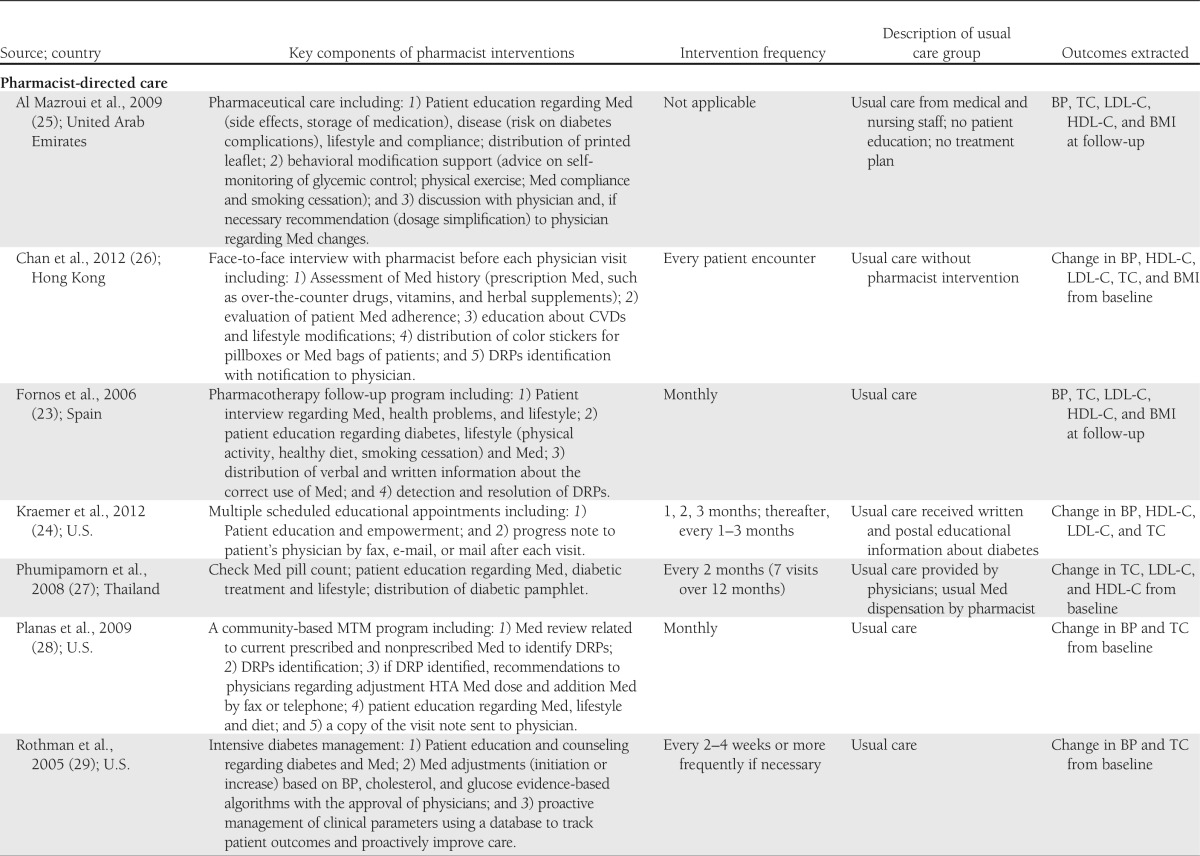
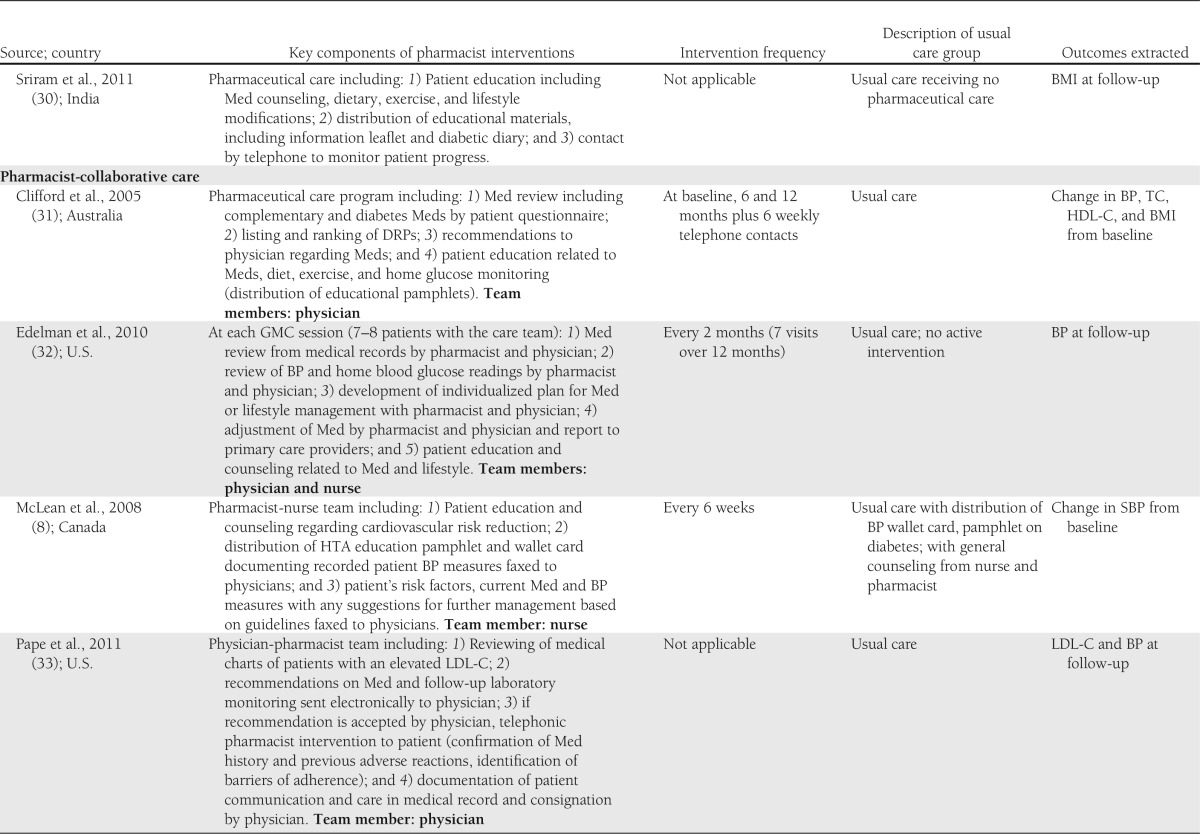
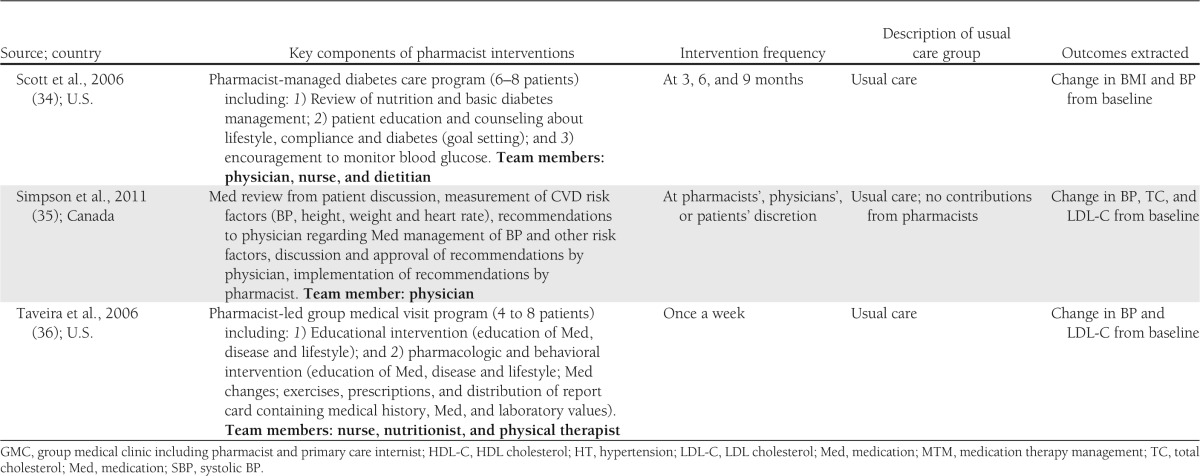
Table 2.
Characteristics of the included studies: key components of pharmacist interventions, intervention frequency, description of usual care group, and outcomes extracted
Types of pharmacist interventions
Eight studies were pharmacist-directed care (23–30) and seven were pharmacist collaborative care (8,31–36) (Tables 1 and 2). Pharmacist interventions were 1) medication management (monitoring of drug therapy such as adjustment and change of medications, medication review from patient interviews, or assessment of medication compliance) in 14 studies (8,23–29,31–36); 2) educational interventions to patients (education and counseling about medications, lifestyle and physical activity or about compliance; distribution or use of educational material; educational workshop) in 14 studies (8,23–34,36); 3) feedback to health care professional (drug-related problems [DRPs] identification, recommendation and discussion with physician regarding medication changes or problems of compliance, development of treatment plans) in 12 studies (8,23–26,28,29,31–35); 4) measurement of CVD risk factors (measurement of BP or review of laboratory data by the pharmacist during follow-up) in 3 studies (8,32,35); and 5) patient-reminder systems (telephone contact) in 5 studies (26,29,30,32,33).
Methodological quality of included studies
As assessed by the Cochrane Risk of Bias Tool (22), the quality of the 15 included studies varied (Supplementary Fig 1). Most studies adequately described randomization sequence generation, were free of selective outcome reporting, and were free of other bias (e.g., important baseline imbalance in patient characteristics). Allocation concealment and blinding to outcome assessors was not described in most studies. In all studies, participants were not blinded to pharmacist intervention.
Outcomes
The outcome was systolic BP in 12 studies (including 1,894 patients) (8,23–26,28,29,31,32,34–36), diastolic BP in 9 studies (1,496 patients) (23–26,29,31,32,35,36), TC in 8 studies (1,280 patients) (23–27,29,31,35), LDL cholesterol in 9 studies (8,084 patients) (23–27,33–36), HDL cholesterol in 6 studies (826 patients) (23–27,31), and BMI in 5 studies (751 patients) (23,25,26,30,31). No study reported smoking as an outcome.
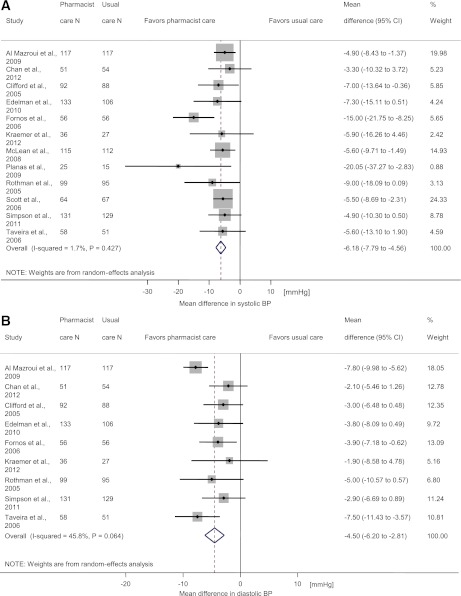
BP
Of the 12 studies reporting systolic BP (8,23–26,28,29,31,32,34–36), 7 demonstrated statistically significant reductions with pharmacist care. Of the nine studies reporting diastolic BP (23–26,29,31,32,35,36), three demonstrated statistically significant reductions with pharmacist care. Pooled analyses indicate that pharmacist care showed greater reductions in systolic BP (weighted mean difference −6.2 mmHg [−7.8 to −4.6], P < 0.001) and diastolic BP (weighted mean difference −4.5 mmHg [−6.2 to −2.8], P < 0.001) compared with usual care (Fig. 2A and B). Heterogeneity was negligible for systolic BP (I2 = 2%) but moderate for diastolic BP (I2 = 46%).
Figure 2.
Forest plots show the effect of pharmacist care on the mean difference in systolic BP (A) and in diastolic BP (B). Mean differences of less than 0 between pharmacist care and usual care groups indicate an effect in favor of pharmacist care. (A high-quality color representation of this figure is available in the online issue.)
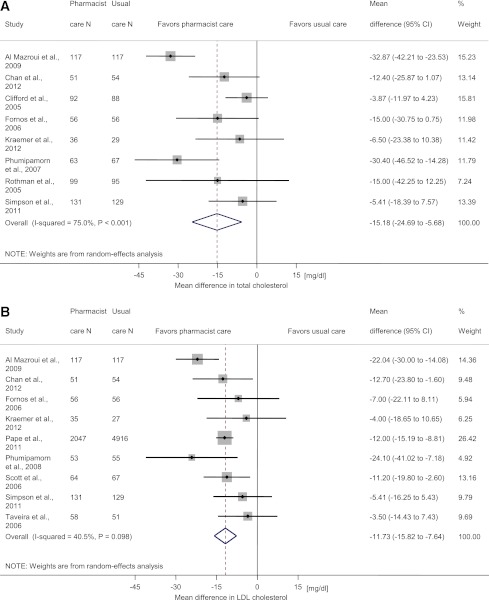
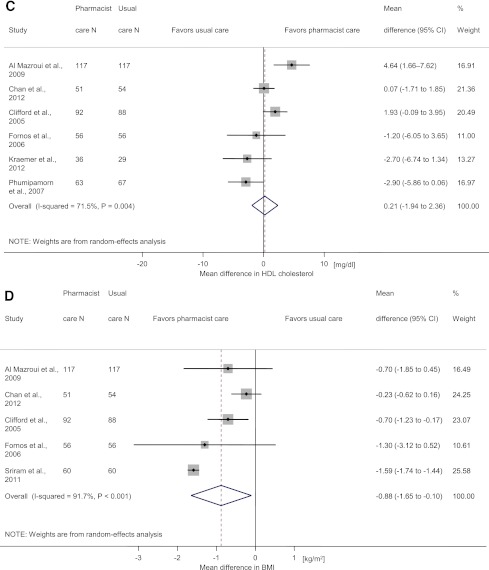
TC, LDL cholesterol, and HDL cholesterol
Two of the eight studies reporting TC demonstrated statistically significant reductions with pharmacist care (25,27), and the pooled estimate showed a significant reduction in TC (weighted mean difference −15.2 mg/dL [−24.7 to −5.7], P = 0.002; Fig. 3A). Five of the nine studies reporting LDL cholesterol demonstrated statistically significant reductions with pharmacist care (25–27,33,34), and the pooled estimate showed a significant reduction in LDL cholesterol (weighted mean difference −11.7 mg/dL [−15.8 to −7.6], P < 0.001; Fig. 3B). Six studies reported HDL cholesterol (Fig. 3C). The pooled estimate did not show a statistically significant change in HDL cholesterol (weighted mean difference 0.2 mg/dL [−1.9 to 2.36], P = 0.846). There was substantial heterogeneity for TC (I2 = 75%) and HDL cholesterol (I2 = 72%) and moderate heterogeneity for LDL cholesterol (I2 = 41%).
Figure 3.
Forest plots show the effect of pharmacist care on the mean difference in TC (A), LDL cholesterol (B), HDL cholesterol (C), and BMI (D). Mean differences of less than 0 between pharmacist and usual care groups indicate an effect in favor of pharmacist care. (A high-quality color representation of this figure is available in the online issue.)
BMI
Five studies reported BMI (Fig. 3D). Two studies (30,31) showed a statistically significant benefit of pharmacist care. The pooled estimate showed a significant reduction in BMI (weighted mean difference −0.9 kg/m2 [−1.7 to −0.1], P = 0.026) with a substantial heterogeneity between studies (I2 = 92%).
Subgroup analyses
We conducted post hoc subgroup analyses to explore the possible differences between studies according to the type of pharmacist care, the type and the number of interventions and the setting of care (Supplementary Table 1). These analyses, conducted only for the outcome systolic BP available in 12 studies, showed a statistically and clinically significant reduction in systolic BP for both pharmacist-directed care and pharmacist-collaborative care, with a tendency to a greater reduction in systolic BP for pharmacist-directed care compared with pharmacist-collaborative care (weighted mean difference −8.1 mmHg [−12.3 to −3.7] vs. −5.7 mmHg [−7.7 to −3.7]). Studies conducted in community pharmacies inclined to a greater reduction in systolic BP compared with other studies (weighted mean difference −10.0 mmHg [−16.4 to −3.7] vs. −5.5 mmHg [−7.3 to −3.7]). We found no major differences in systolic BP reductions according to the type and the number of interventions.
Publication bias
We explored the possibility of publication bias for the 12 studies in which the outcome was systolic BP. The funnel plot for the outcome systolic BP showed a slight asymmetry, with a borderline P value using the Egger test (P = 0.08), indicating a potential publication bias.
Sensitivity analyses
Because of a potential publication bias and to explore the impact of study quality on the effect estimates, we conducted two sensitivity analyses. After excluding the six smallest studies (8,25,29,31,32,35), with fewer than 80 participants per randomization group, the six remaining studies demonstrated a statistically significant reductions in systolic BP for pharmacist care compared with the usual care group (weighted mean difference −5.7 mmHg [−7.8 to −3.6], I2 = 0%) and of the same magnitude that was observed when all studies were included. The second sensitivity analysis was restricted to studies of “good quality.” Of 12 studies with the systolic BP outcome, 5 were of good quality, with a low risk of bias on at least 4 of 6 items using the Cochrane Risk of Bias Tool (22), and showed again statistically significant and similar reductions for the pharmacist care (weighted mean difference −5.6 mmHg [−8.2 to −2.9], I2 = 0%).
CONCLUSIONS
Our systematic review and meta-analysis supports the benefits of pharmacist interventions in the management of major CVD risk factors among outpatients with diabetes. Pharmacist interventions were associated with significant reductions in systolic and diastolic BP, TC, LDL cholesterol, and BMI compared with the usual care group. No significant change was observed with HDL cholesterol. The most frequent pharmacist interventions were medication management (monitoring of drug therapy such as adjustment and change of medications, medication review from patient interviews, or assessment of medication compliance), educational interventions to patients (education and counseling about medications, lifestyle and physical activity or about compliance; distribution or use of educational material; educational workshop), and feedback to another health care professional (DRPs identification; recommendation and discussion with physician regarding medication changes or problems of compliance; development of treatment plans).
Beyond the individual studies included in our review, no other systematic review has examined the efficacy of pharmacist interventions in the management of major CVD risk factors among patients with diabetes. Nevertheless, these beneficial results are consistent with our recent systematic review on the effect of pharmacist care in CVD care among outpatients (15) and extend this earlier work by including data from trials focusing specifically on pharmacist care among outpatients with diabetes.
The benefit of pharmacist interventions on CVD risk factors in patients with diabetes combined with the impact of pharmacist care on metabolic control (A1C and fasting blood glucose), as shown in a recent systematic review (16), could translate in substantial benefits on patient morbidity and mortality as well as on health care costs. Our review indicates that pharmacist care improves in a comprehensive manner all major CVD risk factors among outpatients with diabetes, except smoking, for which no study was identified. Because smoking amplifies the risk of CVD among patients with diabetes (37) and may have deleterious effect on diabetes control (38), studies are needed to assess the impact of pharmacist care to reduce the risk of smoking among patients with diabetes. The beneficial effect of pharmacist care on BMI that we observed is encouraging because, like smoking cessation, weight loss is difficult to achieve but of major importance among patients with diabetes to help reduce CVD risk and control blood glucose (39).
We could not identify which type of intervention was more potent to control CVD risk factors among patients with diabetes. Our subgroup analyses restricted to studies assessing systolic BP did not reveal clear differences in effect size according to the type of pharmacist care, the type and the number of interventions, or the setting of care. Moreover, we could not estimate from this review how much training the pharmacist needs, which elements of the intervention have a real impact, the frequency with which the pharmacist has to intervene, or if there is an impact on CVD risk factors beyond the period of intervention. Nevertheless, identification of the more potent intervention was hampered because pharmacist interventions varied among the identified studies and often included a combination of several interventions. Heterogeneity was found in the effect of interventions on diastolic BP, TC, LDL cholesterol, and HDL cholesterol and may be attributable to differences in terms of interventions, care setting, and co-interventions between studies (15).
Strengths and limitations
The strengths of our review include a comprehensive systematic review of the literature, the assessment of the impact of pharmacist interventions on all major CVD risk factors, and the inclusion of different types of pharmacist interventions. Limitations include the variation in pharmacist interventions between studies, preventing the definite identification of the most beneficial intervention, and the absence of direct evidence of the effect of pharmacist interventions on CVD events or death among patients with diabetes. Another limitation includes the absence in many studies of a detailed description of the intervention provided to the control group. In addition, we could not explain the observed heterogeneity between studies for some outcomes. We also identified a potential publication bias. However, our sensitivity analysis restricted to relatively large studies as well as our analyses restricted to good quality studies did not suggest any substantial bias in the estimation of the effect of pharmacist interventions. Finally, most studies were conducted in the U.S. and Canada, reflecting an advanced role of the pharmacist in these health care systems.
Summary and perspectives
Our review provides evidence that pharmacist interventions—conducted alone or in collaboration with other health care professionals—improve management of major CVD risk factors among outpatients with diabetes. However, our work also indicates that more research is needed to assess which pharmacist interventions are most effective, implementable, and less time-consuming in various types of health care systems or jurisdictions. Future research should also demonstrate cost-effectiveness of pharmacist interventions for patients with diabetes and CVD risk factors. There is also a significant need to develop and evaluate interprofessional education initiatives during pharmacy, medical, and nursing training to enhance future collaborative care among patients with diabetes.
Supplementary Material
Acknowledgments
This research was supported in part by the Canadian Institutes of Health Research (CIHR) from the Applied Public Health Research Chair in Chronic Disease Prevention to G.P. and by research and development funding from the Department of Community Medicine and Health, CHUV, Lausanne, Switzerland. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
No potential conflicts of interest relevant to this article were reported.
V.S. and A.C. contributed substantially to the conception and design of the study protocol, contributed to the acquisition and management of data, performed statistical analysis, were responsible for the analysis and interpretation of data, drafted the manuscript, revised the manuscript for important intellectual content, and gave final approval for the submitted version. G.P. and B.B. contributed substantially to the conception and design of the study protocol, were responsible for the analysis and interpretation of data, supervised the study, obtained funding, revised the manuscript for important intellectual content, and gave final approval for the submitted version. A.L.C. contributed to the acquisition and management of data, revised the manuscript for important intellectual content, and gave final approval for the submitted version. V.S. and A.C. are the guarantors of this work and, as such, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc12-0369/-/DC1.
References
- 1.Sarwar N, Gao P, Seshasai SR, et al. Emerging Risk Factors Collaboration Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 2010;375:2215–2222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 3.UK Prospective Diabetes Study Group Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703–713 [PMC free article] [PubMed] [Google Scholar]
- 4.Preis SR, Hwang SJ, Coady S, et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation 2009;119:1728–1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Resnick HE, Foster GL, Bardsley J, Ratner RE. Achievement of American Diabetes Association clinical practice recommendations among U.S. adults with diabetes, 1999-2002: the National Health and Nutrition Examination Survey. Diabetes Care 2006;29:531–537 [DOI] [PubMed] [Google Scholar]
- 6.McFarlane SI, Jacober SJ, Winer N, et al. Control of cardiovascular risk factors in patients with diabetes and hypertension at urban academic medical centers. Diabetes Care 2002;25:718–723 [DOI] [PubMed] [Google Scholar]
- 7.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA 2004;291:335–342 [DOI] [PubMed] [Google Scholar]
- 8.McLean DL, McAlister FA, Johnson JA, et al. SCRIP-HTN Investigators A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: study of cardiovascular risk intervention by pharmacists-hypertension (SCRIP-HTN). Arch Intern Med 2008;168:2355–2361 [DOI] [PubMed] [Google Scholar]
- 9.Chisholm-Burns MA, Kim Lee J, Spivey CA, et al. US pharmacists’ effect as team members on patient care: systematic review and meta-analyses. Med Care 2010;48:923–933 [DOI] [PubMed] [Google Scholar]
- 10.Fera T, Bluml BM, Ellis WM. Diabetes Ten City Challenge: final economic and clinical results. J Am Pharm Assoc (2003) 2009;49:383–391 [DOI] [PubMed] [Google Scholar]
- 11.Santschi V, Rodondi N, Bugnon O, Burnier M. Impact of electronic monitoring of drug adherence on blood pressure control in primary care: a cluster 12-month randomised controlled study. Eur J Intern Med 2008;19:427–434 [DOI] [PubMed] [Google Scholar]
- 12.Tsuyuki RT, Johnson JA, Teo KK, et al. A randomized trial of the effect of community pharmacist intervention on cholesterol risk management: the Study of Cardiovascular Risk Intervention by Pharmacists (SCRIP). Arch Intern Med 2002;162:1149–1155 [DOI] [PubMed] [Google Scholar]
- 13.Villeneuve J, Genest J, Blais L, et al. A cluster randomized controlled Trial to Evaluate an Ambulatory primary care Management program for patients with dyslipidemia: the TEAM study. CMAJ 2010;182:447–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bogden PE, Abbott RD, Williamson P, Onopa JK, Koontz LM. Comparing standard care with a physician and pharmacist team approach for uncontrolled hypertension. J Gen Intern Med 1998;13:740–745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santschi V, Chiolero A, Burnand B, Colosimo AL, Paradis G. Impact of pharmacist care in the management of cardiovascular disease risk factors: a systematic review and meta-analysis of randomized trials. Arch Intern Med 2011;171:1441–1453 [DOI] [PubMed] [Google Scholar]
- 16.Collins C, Limone BL, Scholle JM, Coleman CI. Effect of pharmacist intervention on glycemic control in diabetes. Diabetes Res Clin Pract 2011;92:145–152 [DOI] [PubMed] [Google Scholar]
- 17.Evans CD, Watson E, Eurich DT, et al. Diabetes and cardiovascular disease interventions by community pharmacists: a systematic review. Ann Pharmacother 2011;45:615–628 [DOI] [PubMed] [Google Scholar]
- 18.Machado M, Bajcar J, Guzzo GC, Einarson TR. Sensitivity of patient outcomes to pharmacist interventions. Part I: systematic review and meta-analysis in diabetes management. Ann Pharmacother 2007;41:1569–1582 [DOI] [PubMed] [Google Scholar]
- 19.Wubben DP, Vivian EM. Effects of pharmacist outpatient interventions on adults with diabetes mellitus: a systematic review. Pharmacotherapy 2008;28:421–436 [DOI] [PubMed] [Google Scholar]
- 20.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koshman SL, Charrois TL, Simpson SH, McAlister FA, Tsuyuki RT. Pharmacist care of patients with heart failure: a systematic review of randomized trials. Arch Intern Med 2008;168:687–694 [DOI] [PubMed] [Google Scholar]
- 22.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane-handbook.org [Google Scholar]
- 23.Fornos JA, Andrés NF, Andrés JC, Guerra MM, Egea B. A pharmacotherapy follow-up program in patients with type-2 diabetes in community pharmacies in Spain. Pharm World Sci 2006;28:65–72 [DOI] [PubMed] [Google Scholar]
- 24.Kraemer DF, Kradjan WA, Bianco TM, Low JA. A randomized study to assess the impact of pharmacist counseling of employer-based health plan beneficiaries with diabetes: the EMPOWER study. J Pharm Pract 2012;25:169–179 [DOI] [PubMed] [Google Scholar]
- 25.Al Mazroui NR, Kamal MM, Ghabash NM, Yacout TA, Kole PL, McElnay JC. Influence of pharmaceutical care on health outcomes in patients with type 2 diabetes mellitus. Br J Clin Pharmacol 2009;67:547–557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chan CW, Siu SC, Wong CK, Lee VW. A pharmacist care program: positive impact on cardiac risk in patients with type 2 diabetes. J Cardiovasc Pharmacol Ther 2012;17:57–64 [DOI] [PubMed] [Google Scholar]
- 27.Phumipamorn S, Pongwecharak J, Soorapan S, Pattharachayakul S. Effects of the pharmacist’s input on glycaemic control and cardiovascular risks in Muslim diabetes. Prim Care Diabetes 2008;2:31–37 [DOI] [PubMed] [Google Scholar]
- 28.Planas LG, Crosby KM, Mitchell KD, Farmer KC. Evaluation of a hypertension medication therapy management program in patients with diabetes. J Am Pharm Assoc (2003) 2009;49:164–170 [DOI] [PubMed] [Google Scholar]
- 29.Rothman RL, Malone R, Bryant B, et al. A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. Am J Med 2005;118:276–284 [DOI] [PubMed] [Google Scholar]
- 30.Sriram S, Chack LE, Ramasamy R, Ghasemi A, Ravi TK, Sabzghabaee AM. Impact of pharmaceutical care on quality of life in patients with type 2 diabetes mellitus. J Res Med Sci 2011;16(Suppl 1.):S412–S418 [PMC free article] [PubMed]
- 31.Clifford RM, Davis WA, Batty KT, Davis TM, Fremantle Diabetes Study Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care 2005;28:771–776 [DOI] [PubMed] [Google Scholar]
- 32.Edelman D, Fredrickson SK, Melnyk SD, et al. Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Ann Intern Med 2010;152:689–696 [DOI] [PubMed] [Google Scholar]
- 33.Pape GA, Hunt JS, Butler KL, et al. Team-based care approach to cholesterol management in diabetes mellitus: two-year cluster randomized controlled trial. Arch Intern Med 2011;171:1480–1486 [DOI] [PubMed] [Google Scholar]
- 34.Scott DM, Boyd ST, Stephan M, Augustine SC, Reardon TP. Outcomes of pharmacist-managed diabetes care services in a community health center. Am J Health Syst Pharm 2006;63:2116–2122 [DOI] [PubMed] [Google Scholar]
- 35.Simpson SH, Majumdar SR, Tsuyuki RT, Lewanczuk RZ, Spooner R, Johnson JA. Effect of adding pharmacists to primary care teams on blood pressure control in patients with type 2 diabetes: a randomized controlled trial. Diabetes Care 2011;34:20–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Taveira TH, Friedmann PD, Cohen LB, et al. Pharmacist-led group medical appointment model in type 2 diabetes. Diabetes Educ 2010;36:109–117 [DOI] [PubMed] [Google Scholar]
- 37.Fagard RH. Smoking amplifies cardiovascular risk in patients with hypertension and diabetes. Diabetes Care 2009;32(Suppl. 2):S429–S431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chiolero A, Faeh D, Paccaud F, Cornuz J. Consequences of smoking for body weight, body fat distribution, and insulin resistance. Am J Clin Nutr 2008;87:801–809 [DOI] [PubMed] [Google Scholar]
- 39.Fujioka K. Benefits of moderate weight loss in patients with type 2 diabetes. Diabetes Obes Metab 2010;12:186–194 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.