Abstract
OBJECTIVE
Individuals with diabetes have an excess mortality compared with people without diabetes. This study used a national cohort of older Spanish adults to identify possible factors explaining the relation between diabetes and excess mortality.
RESEARCH DESIGN AND METHODS
A cohort of 4,008 people ≥60 years of age was selected in 2000–2001 and followed prospectively until 2008. At baseline, data were collected on diabetes and major risk factors for mortality: social network, diet, physical activity and other lifestyle factors, obesity, hypertension, dyslipidemia, and previous cardiovascular disease and cancer. Analyses were conducted with Cox regression with progressive adjustment for mortality risk factors.
RESULTS
In the study cohort, 667 people had diabetes. A total of 972 deaths occurred during follow-up. The hazard ratio (HR) and 95% CI for mortality in diabetic versus nondiabetic subjects, adjusted for age, marital status, education level, social class, medical consultation, and treatment with statins, angiotensin II antagonists, or aspirin, was 1.40 (1.11–1.76) in men and 1.70 (1.37–2.10) in women. Adjustment for additional risk factors produced little change in the HR. After adjustment for all risk factors, including cardiovascular disease and cancer, the mortality HR in diabetic versus nondiabetic individuals was 1.43 (1.12–1.82) in men and 1.67 (1.34–2.08) in women. The inclusion of lifestyles and diseases occurring during follow-up also produced little change in the relation between diabetes and mortality.
CONCLUSIONS
The excess risk of mortality in diabetic versus nondiabetic individuals cannot be explained by mortality risk factors or by the presence of cardiovascular disease or cancer.
Several investigations have demonstrated higher mortality in diabetic than in nondiabetic subjects (1–5). However, few such studies have examined the extent to which mortality risk factors are responsible for this difference (6). Some authors who have investigated this issue have concluded that aggressive intervention measures are needed in individuals with diabetes to reduce the frequency of risk factors that increase their risk of mortality in comparison with those without diabetes (7,8).
Interventions on risk factors may reduce the absolute risk of mortality in diabetic patients, as has been observed with the strict control of blood pressure in diabetic individuals with hypertension (9,10). However, such a recommendation does not take into account the findings in other population groups where it has been observed that the presence of some risk factors is not always associated with an increased risk of mortality. This is the case in some studies of the elderly, showing that obesity is associated with a reduced risk of mortality (11,12).
The objective of this study was to assess the association between diabetes and mortality over 8 years of follow-up in one of these cohorts of older adults and to identify possible mortality risk factors that explain this relation.
RESEARCH DESIGN AND METHODS
Study participants and design
A national sample of 4,008 people, representative of the noninstitutionalized Spanish population ≥60 years of age, was selected between 1 October 2000 and 31 March 2001 and was followed prospectively up to 31 October 2008. At baseline, subjects were selected using probabilistic sampling with multistage clusters. The clusters were obtained according to region of residence and size of municipality. Census sections were then chosen randomly within each cluster, and the households where information was finally obtained from the subjects were chosen within each section. Study participants were selected in age and sex strata. The study response rate was 71%. Baseline information was collected in the home through personal interviews and physical examination by trained and certified personnel. Full details of participants and measurements have been reported previously (13). Informed consent was obtained in writing from each study participant and from an accompanying family member. The study was approved by the Clinical Research Ethics Committee of La Paz University Hospital in Madrid, Spain.
Study variables
Mortality was obtained from the National Death Index, a computerized database with information on the vital status of all residents in Spain. Up to 31 October 2008, the vital status of 3,991 individuals (99.6% of the cohort) had been identified; 1,742 subjects were between 60 and 69 years of age, 1,451 were between 70 and 79 years of age, and 798 were ≥80 years of age. A total of 972 deaths occurred during this period.
At baseline, subjects were shown a list of various chronic diseases and were asked whether a physician had ever told them they had any of them; respondents replied yes or no for each disease. The questionnaire also included a question in which study participants were asked to show all the medications they were taking at the time. Subjects were considered to have diabetes if a physician had diagnosed them with diabetes or if they were on insulin or oral antidiabetic medications.
We collected baseline information on risk factors related to lifestyles shown to be associated with mortality in the literature. Included in the analysis were social network, lifestyles (smoking, alcohol consumption, physical activity, and diet), obesity, hypertension, and dyslipidemia. Other baseline variables used in the analyses were age, marital status, education, social class based on occupation, frequency of visits for medical consultation, and current treatment with several medications.
Social network was evaluated by the frequency with which the respondent saw family members or friends and was grouped into the following categories: daily or almost daily, once or twice a week, and less often. With regard to smoking, subjects were classified as never smokers, former smokers, or current smokers. Individuals were also asked to state which of the following alternatives best reflected their alcohol consumption frequency: never drinker, former drinker, occasional drinker, or regular drinker. For leisure-time physical activity, participants were classified into three categories: none, occasional, and regular. Subjects were also asked about their weekly intake of fruit, vegetables, and olive oil, each of which was grouped into three categories according to frequency of consumption: daily, one or more days per week, and less than once a week.
Information on obesity and hypertension was obtained by physical examination. BMI was calculated as weight divided by height squared. Participants were considered to be obese if they had a BMI ≥30 kg/m2, and to have abdominal obesity when waist circumference was >102 cm in men and >88 cm in women. They were deemed to be hypertensive when their systolic blood pressure was ≥140 mmHg or their diastolic blood pressure was ≥90 mmHg, or if they were on current antihypertensive drug treatment. Study participants were also asked if a physician had told them that they had high (blood) cholesterol. Subjects were considered to have dyslipidemia if they answered this question in the affirmative or if they were taking cholesterol-lowering medications. The presence of cardiovascular disease and cancer was also included in the analysis. Information on heart disease, stroke, and cancer was self-reported based on the above-mentioned list of chronic diseases.
Marital status was categorized as married, widowed, or single/divorced. Education level was grouped into three categories based on the highest education level attained: low (illiterate individuals and those who did not complete primary education), medium (completed primary education), and high (completed secondary or higher-level education). Occupational social class was grouped into three categories: nonmanual workers (professionals, managers, proprietors, and clerical workers), manual workers (skilled and unskilled), and farm workers. For women who never had paid employment, >75% of this cohort, the social class was estimated from their husband’s occupation.
The frequency of visits for medical consultation was grouped into two categories: at least once a month and less than once a month. We also considered whether or not subjects were currently being treated with statins, angiotensin II antagonists, or aspirin. Control of hypertension was also analyzed. Control was defined as pharmacological treatment of hypertension associated with systolic blood pressure <140 mmHg and diastolic blood pressure <90 mmHg.
Statistical analysis
Mortality analyses were conducted with Cox regression, and the main results were summarized with hazard ratios (HRs) and their 95% CIs. We first evaluated the association between risk factors and cardiovascular disease and 8-year mortality, in men and women. We then estimated the association between these risk factors and mortality in individuals with and without diabetes. Likelihood ratio tests were used to assess whether the results differed by sex or presence of diabetes. For this purpose, we used the change of deviance to assess the possibility of interaction between sex and each risk factor (or between diabetes and each risk factor), by comparing the model without interaction with a model containing the appropriate interaction term. We also assessed whether the associations in diabetic and nondiabetic people depend on sex.
We then evaluated the association between diabetes and mortality using Cox regression models. Basic Cox models were adjusted for age, marital status, education level, occupational social class, medical consultation, and current treatment with statins, angiotensin II antagonists, or aspirin. We subsequently adjusted for each of the following variables: social network, diet, other lifestyle risk factors, obesity, hypertension, dyslipidemia, heart disease, stroke, and cancer. Finally, models were adjusted for all covariates together.
In 2003, an attempt was made to contact the subjects again, and this was successful in 3,235 cases. Of the 3,235 individuals followed-up until 2003, the following were excluded from the analyses: 245 who died in the period 2001–2003 and 5 who failed to provide information. In the remaining 2,985 subjects, data on lifestyles in 2003 and chronic diseases diagnosed by the physician in the period 2001–2003 were collected by telephone interview conducted by trained staff. The association between diabetes and mortality was also evaluated in these subjects, and the information obtained during follow-up was incorporated into the models.
RESULTS
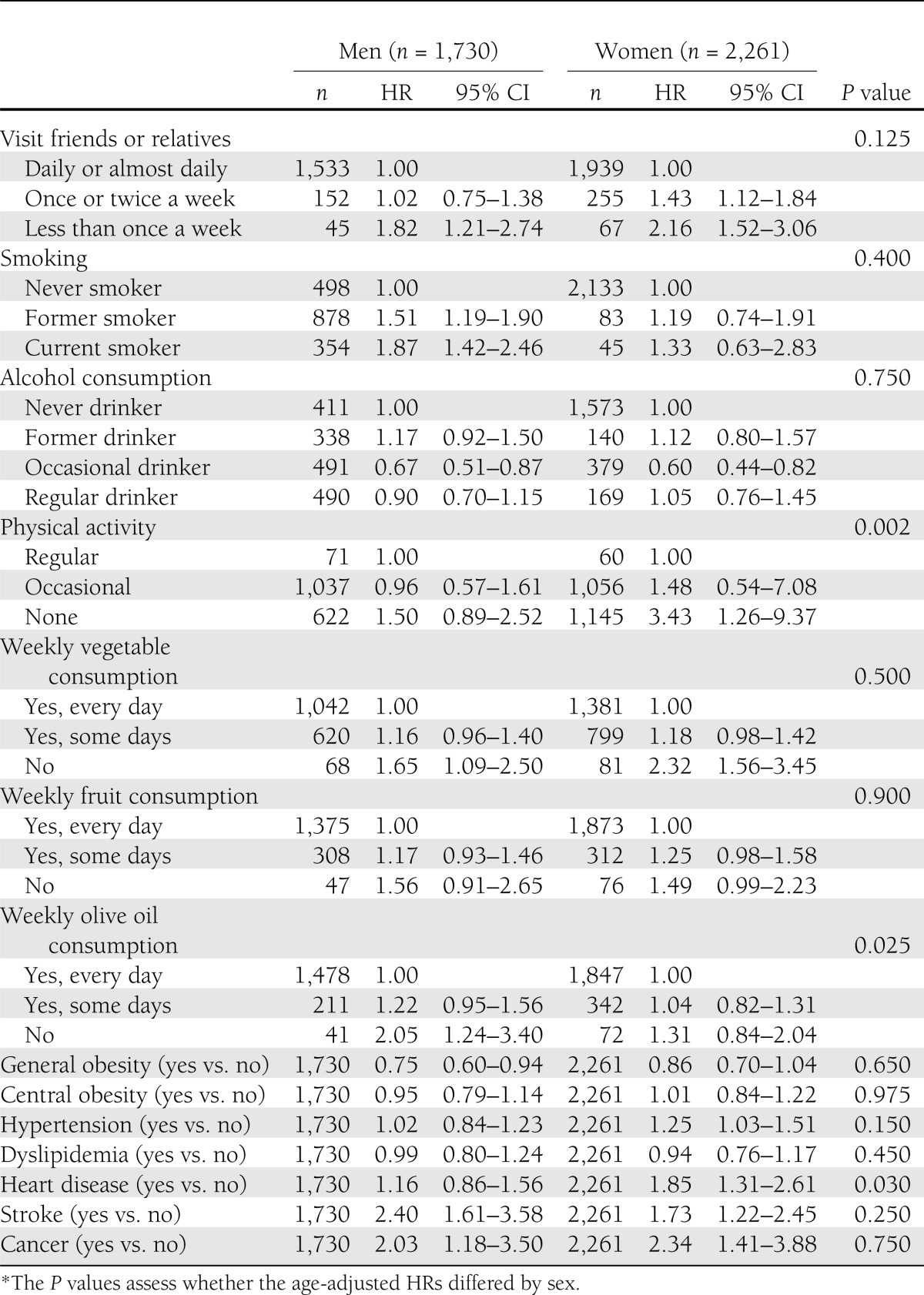
Table 1 shows the association between the risk factors and chronic diseases and mortality. A higher risk of mortality was observed, either in men, women, or both sexes, among those who less frequently saw family or friends, who were smokers or had ever been smokers, who were sedentary, who did not consume vegetables, fruit, or olive oil at least once a week, who had hypertension, or who had any of the chronic diseases investigated. Physical activity and heart disease were associated with mortality in women, but not in men, whereas olive oil consumption was associated with mortality in men, but not in women. Occasional drinking and general obesity were associated with a reduced risk of mortality in both sexes.
Table 1.
Age-adjusted HRs and 95% CIs for mortality according to risk factors and chronic diseases by sex and P values for the differences by sex
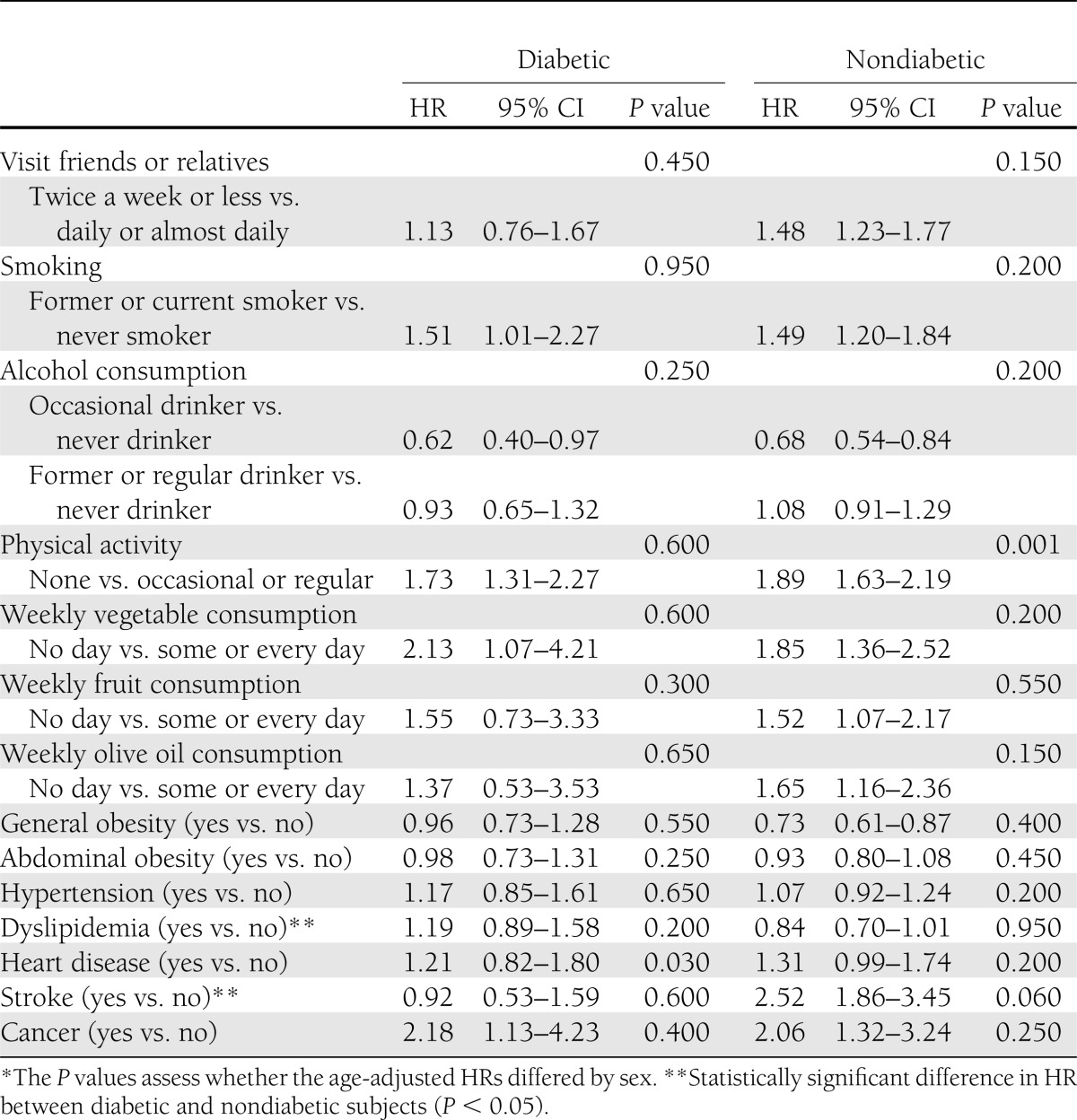
The association between the risk factors and chronic diseases investigated and mortality in people with and without diabetes is presented in Table 2. Due to the small number of subjects, the risk factor categories were collapsed. The mortality HRs for most risk factors and chronic diseases were similar in people with and without diabetes, but mortality HRs for dyslipidemia and for stroke were different in each group, with evidence of statistical interaction (P < 0.05). In both diabetic and nondiabetic individuals, mortality HRs for most risk factors were similar in men and women, with the exception of heart disease in individuals with diabetes and physical activity in those without this disease; in both of these cases, the association was stronger in women than in men.
Table 2.
Age-adjusted HRs and 95% CIs for mortality according to risk factors and chronic diseases in people with and without diabetes
There were statistically significant differences between diabetic and nondiabetic subjects in the frequency of medical consultation and in current treatment with statins and angiotensin II antagonists. About 53.1% of individuals with diabetes visited the physician at least once a month versus 35.0% of nondiabetic individuals. The frequency of treatment with statins and angiotensin II antagonists in diabetic patients was 19.2 and 10.1%, respectively, compared with 9.9 and 4.4% in those without diabetes. Statistically significant differences were also seen in adequate control of hypertension, which was 27.6% in diabetic versus 33.5% in nondiabetic individuals. In contrast, no statistically significant differences between those with and without diabetes were observed with respect to treatment with aspirin (16.7 and 15.0%, respectively).
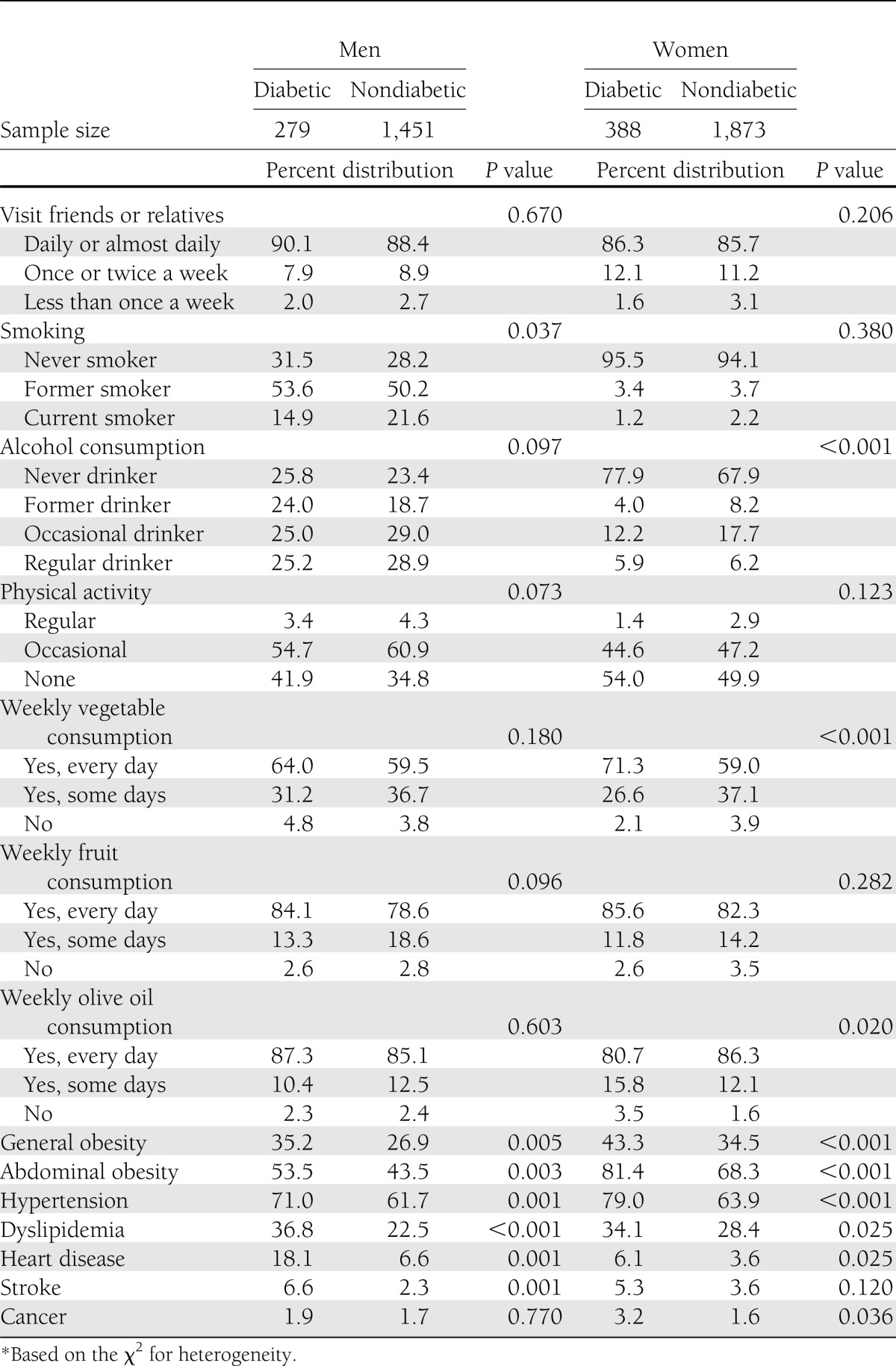
The distribution of risk factors and chronic diseases in individuals with and without diabetes is shown in Table 3. In men, the distribution of most of the risk factors at baseline did not differ significantly between the two groups (P > 0.05), except for smoking, obesity, hypertension, and dyslipidemia. In women, the risk factor distribution was significantly different for alcohol consumption, weekly vegetable consumption, weekly olive oil consumption, obesity, hypertension, and dyslipidemia. The prevalence of the chronic diseases investigated was higher in diabetic than in nondiabetic individuals, although the differences were not significant (P > 0.05) for cancer in men and for stroke in women.
Table 3.
Distribution of baseline characteristics of people with and without diabetes by sex
In men, the age-adjusted mortality rates per 100 person-years throughout the follow-up period was 5.7 in diabetic subjects and 3.3 in those without diabetes, whereas the comparable rates in women were 4.6 and 2.6, respectively.
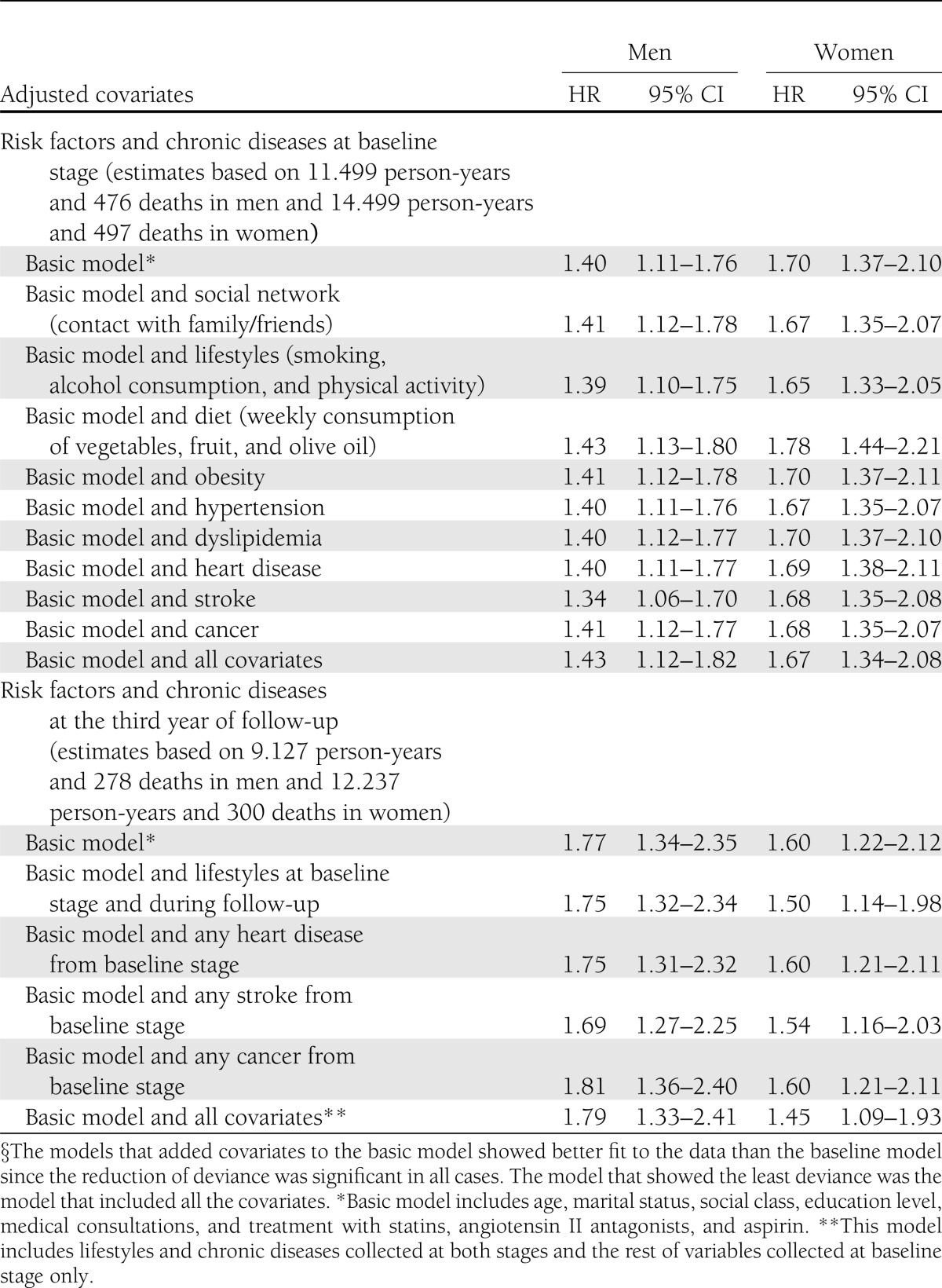
Table 4 presents the multivariable association between diabetes and mortality adjusted for the different risk factors and chronic diseases. The mortality HR in diabetic versus nondiabetic individuals in the basic model, adjusted for age, marital status, education level, occupational social class, medical consultation, and treatment with statins, angiotensin II antagonists, or aspirin, was 1.40 (95% CI 1.11–1.76) in men and 1.70 (1.37–2.10) in women. In men, the magnitude of the HR changed little or not at all with respect to those in the basic model, except after adjusting for stroke, when it decreased to 1.34. In women, the HR also changed little, except after adjusting for diet, when it increased to 1.78. The fully adjusted HR for mortality in diabetic versus nondiabetic subjects was 1.43 (1.12–1.82) in men and 1.67 (1.34–2.08) in women.
Table 4.
HRs and 95% CIs for mortality in diabetic vs. nondiabetic subjects adjusted for several risk factors and chronic diseases
Table 4 also includes the results of the multivariable association between diabetes and mortality in the 2,985 subjects for whom information was available in 2003. In men, the magnitude of the fully adjusted HR (1.79 [95% CI 1.33–2.41]) changed little with respect to the basic model (1.77 [1.34–2.35]). In contrast, in women, the magnitude of the fully adjusted HR (1.45 [1.09–1.93]) decreased with respect to the basic model (1.60 [1.22–2.12]).
CONCLUSIONS
In this national cohort of older adults in Spain, we found that the HR for mortality in diabetic versus nondiabetic subjects was 1.40 in men and 1.70 in women. Adjustment for all risk factors and for baseline cardiovascular disease and cancer produced little change in the magnitude of these HRs, which suggests that the excess mortality in individuals with diabetes cannot be explained by the risk factors and diseases studied. Visiting with friends or relatives, smoking, frequency of alcohol consumption, physical activity, frequency of consumption of vegetables, fruit, and olive oil, obesity, hypertension, heart disease, stroke, and cancer are predictors of the risk of mortality in both men and women. The association between risk factors and mortality was not significantly different between diabetic and nondiabetic individuals, except for dyslipidemia and stroke.
Various studies have found a higher risk of mortality in diabetic than in nondiabetic, older adults (2,3,14–17). Like the results observed in the entire cohort of our study, most, but not all, studies (3) have found that the excess mortality risk in diabetic subjects is higher in women than in men. The reasons for this are unknown, although some authors attribute this finding to a higher prevalence of mortality risk factors in diabetic women than men or to less aggressive medical management in diabetic women (1,18). Our findings do not support the explanation about the different prevalence of risk factors, because adjustment for mortality risk factors barely modifies the magnitude of the HR in either sex.
In the estimates for subjects who provided information in 2003, the excess mortality risk in diabetic men was higher than in diabetic women. This result can be attributed to the different proportion of people with diabetes who died before the new stage of data collection: 30% of men and 41% of women. Thus, the proportion of deaths in diabetic individuals in the remaining follow-up time was higher in men than in women.
Several studies have assessed the mortality risk associated with lifestyles and other health-related risk factors in cohorts of diabetic patients (2,19–23). The results of these investigations were unable to determine which factors are responsible for their excess mortality risk. The few studies conducted to identify these possible factors have yielded findings similar to ours; the risk factors do not explain the difference in mortality between diabetic and nondiabetic subjects (6–8,24,25). In our study, the greatest reduction in the magnitude of the HR was observed when we adjusted for lifestyles in women, but the reduction was little more than 7% (from 1.70 to 1.65) in the analysis of the entire cohort and 17% (from 1.60 to 1.50) in the analysis of the subjects who also provided information in 2003. This reduction was due to physical activity, since adjustment for smoking or for alcohol consumption barely changed the magnitude of the HR in the basic model (data not shown).
Also, the observed prevalence of risk factors is not always higher in diabetic than nondiabetic subjects (7,8,24,25). Similar to previous studies, we found that the prevalence of smoking does not differ between the two groups or is lower in diabetic individuals. Likewise, a previous study did not show differences between diabetic and nondiabetic individuals in dietary habits (8). In our study, people with diabetes show a more favorable risk profile with respect to dietary habits than those without the disease; consequently the HR did not decrease but rather increased slightly in men and especially in women after adjusting for diet.
Because the observed associations between risk factors and mortality do not differ significantly in people with and without diabetes, intervention measures to reduce mortality risk factors should not be more beneficial in relative terms in diabetic than in nondiabetic individuals. Some evidence in this regard has been observed in the case of hypertension control. Specifically, a meta-analysis showed that the reduction of mortality and cardiovascular events with strict control of blood pressure did not differ between diabetic and nondiabetic subjects (10). Something similar occurred in our study; even though diabetic subjects had poorer control of hypertension than those without diabetes, adjustment for the indicator of blood pressure control did not change the results (data not shown).
As expected, the prevalence of obesity was higher in diabetic subjects, but adjustment for obesity led to a slightly higher rather than lower mortality HR. This occurred because obesity was not associated with mortality in individuals with diabetes, but it was associated with a lower risk of mortality in nondiabetic individuals. These results are not surprising given the lack of clear evidence on the association between obesity and mortality (11) or between weight loss and mortality (26–30). This possible protective effect of obesity in nondiabetic Spanish elders has been found only for general obesity, also observed in other older populations (11), since in our study central obesity was not associated with mortality.
Likewise, some studies have shown that high levels of serum cholesterol in older people are associated with a reduced risk of mortality (31,32). In our study dyslipidemia was also associated with a lower risk of mortality in nondiabetic subjects. Although the prevalence of dyslipidemia was higher in subjects with diabetes, adjustment for dyslipidemia did not alter the magnitude of the HR in the analyses.
The interpretation of our results should take into account that our study deals with prevalent and not incident cases of diabetes. A systematic review of observational studies (15) reporting mortality in diabetic patients, diagnosed with type 2 diabetes over the age of 60, showed a lower association between diabetes and mortality than in the present study. Moreover, we cannot rule out a selective survival bias related to diabetes since diabetic patients who reach older ages may have better health than those who die prematurely. Accordingly, the magnitude of the HR obtained in this study may be underestimated.
In 2009, the participants were contacted again. Around 13% of subjects who did not have diabetes at baseline had developed diabetes. This circumstance probably contributed to an underestimate of the magnitude of the HR, since in the analysis, these subjects were considered not to have diabetes.
In our study, there might have been certain misclassification of diabetes, since it was based on reported information and not on an objective test of glycemia or oral glucose overload. Some patients may not have recognized their diabetic condition and may have been classified as nondiabetic. This misclassification would be presumably nondifferential with respect to mortality since the proportion of individuals misclassified on exposure (diabetic vs. nondiabetic subjects) is independent of future mortality risk. As a consequence, the mortality HR in diabetic versus nondiabetic individuals may have been underestimated because the latter group may contain diabetic subjects incorrectly identified as nondiabetic. In any case, it has been observed that self-reported diabetes is reasonably reliable as a surrogate for diagnosed diabetes (33,34).
On the other hand, an investigation that analyzed the information obtained in 97 prospective studies found an association between increased mortality and levels of fasting glucose and a substantial attenuation of the association between diabetes and mortality when adjusted for fasting glucose and markers of glycemia (6). The lack of information on these variables in our study is one of its limitations.
Several risk factors as well as the presence of disease were obtained from patient reports. Since we are unable to rule out the existence of information bias in the measurement of these variables, it is impossible to assure that all variables have been adequately controlled for confounding. It should also be noted that most risk factors were classified using broad categories and/or measuring only one aspect of the risk factor. As a result, the contribution of some risk factors to the explanation of the association between diabetes and mortality may have been underestimated. Nonetheless, when some measures, such as BMI, were disaggregated into various categories, the results were similar. Other measures, like visits with friends or relatives, could not be disaggregated, but it is unlikely that separating “daily” and “almost daily” would modify the findings.
In addition, it should be noted that Spain has one of the highest rates of physician consultations per person and per year with respect to the countries of Western Europe (35). Likewise, we have found a low frequency of treatment with statins and angiotensin II antagonists in diabetic patients. Spain is a Mediterranean country with low cardiovascular risk, and perhaps the Spanish physicians prescribe drugs based on the absolute risk reduction rather than on the relative risk reduction; although we must not exclude the possibility of a low market penetration of these drug treatments. In any case, the low levels of such treatments raise uncertainty in the generalization of our results to other populations.
We were unable to estimate the association between diabetes and mortality from specific causes of death because the National Death Index does not contain information on the cause of death. However, what is most important with regard to prognosis in diabetic patients is survival. Moreover, most deaths are due to cardiovascular diseases or cancer (1,4,15), and we have adjusted for important risk factors related to these diseases.
In conclusion, in older Spanish adults, diabetic individuals have a higher risk of mortality than those who do not have diabetes. This excess risk cannot be explained by mortality risk factors, cardiovascular disease, or cancer. This suggests that the excess mortality could not be explained by traditional risk factors alone.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
E.R. originated and designed the study and coordinated the writing of the manuscript. J.F. and F.R.-A. contributed to the analysis of this study and to the drafting of the manuscript. M.S., R.S., and S.A. contributed to the interpretation of the results and to the drafting of the manuscript. All authors contributed to, reviewed, and approved the final manuscript. E.R. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Geiss LS, Herman WH, Smith PJ. Mortality in non-insulin-dependent diabetics. In Diabetes in America. Harris MI, Bennet PH, Boyko EJ, Cowie CC, Eds. Washington, DC, U.S. Govt. Printing Office, 1995, p. 233–255 [Google Scholar]
- 2.Mulnier HE, Seaman HE, Raleigh VS, Soedamah-Muthu SS, Colhoun HM, Lawrenson RA. Mortality in people with type 2 diabetes in the UK. Diabet Med 2006;23:516–521 [DOI] [PubMed] [Google Scholar]
- 3.Oldridge NB, Stump TE, Nothwehr FK, Clark DO. Prevalence and outcomes of comorbid metabolic and cardiovascular conditions in middle- and older-age adults. J Clin Epidemiol 2001;54:928–934 [DOI] [PubMed] [Google Scholar]
- 4.Morgan CL, Currie CJ, Peters JR. Relationship between diabetes and mortality: a population study using record linkage. Diabetes Care 2000;23:1103–1107 [DOI] [PubMed] [Google Scholar]
- 5.Jansson SPO, Andersson DK, Svärdsudd K. Mortality trends in subjects with and without diabetes during 33 years of follow-up. Diabetes Care 2010;33:551–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seshasai SR, Kaptoge S, Thompson A, et al. Emerging Risk Factors Collaboration Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 2011;364:829–841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lotufo PA, Gaziano JM, Chae CU, et al. Diabetes and all-cause and coronary heart disease mortality among US male physicians. Arch Intern Med 2001;161:242–247 [DOI] [PubMed] [Google Scholar]
- 8.Hu FB, Stampfer MJ, Solomon CG, et al. The impact of diabetes mellitus on mortality from all causes and coronary heart disease in women: 20 years of follow-up. Arch Intern Med 2001;161:1717–1723 [DOI] [PubMed] [Google Scholar]
- 9.Katakura M, Naka M, Kondo T, et al. Prospective analysis of mortality, morbidity, and risk factors in elderly diabetic subjects: Nagano study. Diabetes Care 2003;26:638–644 [DOI] [PubMed] [Google Scholar]
- 10.Turnbull F, Neal B, Algert C, et al. Blood Pressure Lowering Treatment Trialists’ Collaboration Effects of different blood pressure-lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus: results of prospectively designed overviews of randomized trials. Arch Intern Med 2005;165:1410–1419 [DOI] [PubMed] [Google Scholar]
- 11.Janssen I, Mark AE. Elevated body mass index and mortality risk in the elderly. Obes Rev 2007;8:41–59 [DOI] [PubMed] [Google Scholar]
- 12.Guallar-Castillón P, Balboa-Castillo T, López-García E, et al. BMI, waist circumference, and mortality according to health status in the older adult population of Spain. Obesity (Silver Spring) 2009;17:2232–2238 [DOI] [PubMed] [Google Scholar]
- 13.Banegas JR, Rodríguez-Artalejo F, Ruilope LM, et al. Hypertension magnitude and management in the elderly population of Spain. J Hypertens 2002;20:2157–2164 [DOI] [PubMed] [Google Scholar]
- 14.Gu K, Cowie CC, Harris MI. Mortality in adults with and without diabetes in a national cohort of the U.S. population, 1971-1993. Diabetes Care 1998;21:1138–1145 [DOI] [PubMed] [Google Scholar]
- 15.Barnett KN, McMurdo ME, Ogston SA, Morris AD, Ewans JM. Mortality in people diagnosed with type 2 diabetes at an older age: a systematic review. Age Ageing 2006;35:463–468 [DOI] [PubMed] [Google Scholar]
- 16.Tan HH, McAlpine RR, James P, et al. DARTS/MEMO collaboration Diagnosis of type 2 diabetes at an older age: effect on mortality in men and women. Diabetes Care 2004;27:2797–2799 [DOI] [PubMed] [Google Scholar]
- 17.Bertoni AG, Krop JS, Anderson GF, Brancati FL. Diabetes-related morbidity and mortality in a national sample of U.S. elders. Diabetes Care 2002;25:471–475 [DOI] [PubMed] [Google Scholar]
- 18.Gregg EW, Gu Q, Cheng YJ, Narayan KM, Cowie CC. Mortality trends in men and women with diabetes, 1971 to 2000. Ann Intern Med 2007;147:149–155 [DOI] [PubMed] [Google Scholar]
- 19.Jarret J. Mortality in diabetes. Q J Med 1990;75:413–414 [PubMed] [Google Scholar]
- 20.Sprafka JM, Pankow J, McGovern PG, French LR. Mortality among type 2 diabetic individuals and associated risk factors: the Three City Study. Diabet Med 1993;10:627–632 [DOI] [PubMed] [Google Scholar]
- 21.Nöthlings U, Ford ES, Kröger J, Boeing H. Lifestyle factors and mortality among adults with diabetes: findings from the European Prospective Investigation into Cancer and Nutrition-Potsdam study. J Diabetes 2010;2:112–117 [DOI] [PubMed] [Google Scholar]
- 22.Ciechanowski P, Russo J, Katon WJ, et al. Relationship styles and mortality in patients with diabetes. Diabetes Care 2010;33:539–544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu L. Social connections, diabetes mellitus, and risk of mortality among white and African-American adults aged 70 and older: an eight-year follow-up study. Ann Epidemiol 2011;21:26–33 [DOI] [PubMed] [Google Scholar]
- 24.Rosengren A, Welin L, Tsipogianni A, Wilhelmsen L. Impact of cardiovascular risk factors on coronary heart disease and mortality among middle aged diabetic men: a general population study. BMJ 1989;299:1127–1131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ford ES, DeStefano F. Risk factors for mortality from all causes and from coronary heart disease among persons with diabetes. Findings from the National Health and Nutrition Examination Survey I Epidemiologic Follow-up Study. Am J Epidemiol 1991;133:1220–1230 [DOI] [PubMed] [Google Scholar]
- 26.Harrington M, Gibson S, Cottrell RC. A review and meta-analysis of the effect of weight loss on all-cause mortality risk. Nutr Res Rev 2009;22:93–108 [DOI] [PubMed] [Google Scholar]
- 27.Ingram DD, Mussolino ME. Weight loss from maximum body weight and mortality: the Third National Health and Nutrition Examination Survey Linked Mortality File. Int J Obes (Lond) 2010;34:1044–1050 [DOI] [PubMed] [Google Scholar]
- 28.Williamson DF. Weight loss and mortality in persons with type-2 diabetes mellitus: a review of the epidemiological evidence. Exp Clin Endocrinol Diabetes 1998;106(Suppl 2):14–21 [DOI] [PubMed] [Google Scholar]
- 29.Wedick NM, Barrett-Connor E, Knoke JD, Wingard DL. The relationship between weight loss and all-cause mortality in older men and women with and without diabetes mellitus: the Rancho Bernardo study. J Am Geriatr Soc 2002;50:1810–1815 [DOI] [PubMed] [Google Scholar]
- 30.Aucott L, Poobalan A, Smith WCS, et al. Weight loss in obese diabetic and non-diabetic individuals and long-term diabetes outcomes—a systematic review. Diabetes Obes Metab 2004;6:85–94 [DOI] [PubMed] [Google Scholar]
- 31.Weverling-Rijnsburger AW, Blauw GJ, Lagaay AM, Knook DL, Meinders AE, Westendorp RG. Total cholesterol and risk of mortality in the oldest old. Lancet 1997;350:1119–1123 [DOI] [PubMed] [Google Scholar]
- 32.Schatz IJ, Masaki K, Yano K, Chen R, Rodriguez BL, Curb JD. Cholesterol and all-cause mortality in elderly people from the Honolulu Heart Program: a cohort study. Lancet 2001;358:351–355 [DOI] [PubMed] [Google Scholar]
- 33.Heliövaara M, Aromaa A, Klaukka T, Knekt P, Joukamaa M, Impivaara O. Reliability and validity of interview data on chronic diseases. The Mini-Finland Health Survey. J Clin Epidemiol 1993;46:181–191 [DOI] [PubMed] [Google Scholar]
- 34.Van der Velden J, Abrahamse H, Donker G, Vand der Steen J, Van Sonsbeek J, Van den Bos G. What do health interview surveys tell us about the prevalences of somatic chronic diseases? Eur J Public Health 1998;8:52–58 [Google Scholar]
- 35.Organization for Economic Cooperation and Development. OECD.Stat extracts. Health care utilisation: consultations [Internet]. Available from https://portal.mspsi.es/http/stats.oecd.org/index.aspx Accessed 20 December 2011