Abstract
Background
The aims of this study were to evaluate the associated injuries occurring with acute perilunate instability and to assess the clinical and radiographic outcomes of perilunate dislocations and fracture–dislocations treated with a combined dorsal and volar approach.
Methods
A total of 45 patients (46 wrist injuries) with perilunate dislocations and fracture–dislocations were prospectively evaluated. The size of the mid-carpal ligament tear, the location of the scapholunate ligament tear, and the presence of osteochondral fragments and of the dorsal radiocarpal ligament avulsions were recorded at injury. Final clinical and radiographic outcomes were evaluated in 25 cases (25 wrists) with a minimum of 6 months of follow-up.
Results
Intraoperative examination of the 46 cases with operative treatment showed the volar carpal ligament tear to be present 100 % of the time and to be an average length of 3.4 cm. Complete avulsion of the dorsal extrinsic radiocarpal ligaments was found in 65.2 % of cases. The scapholunate ligament was torn in 35 cases. Osteochondral fragments were found either volarly or dorsally in 74 % of the cases. The average flexion–extension arc was 82°, forearm rotation was 155°, and grip strength averaged 59 % of the uninjured hand. The average final scapholunate angle was 55° and the scapholunate gap was 2.2 mm.
Conclusion
Treatment of perilunate fracture–dislocations with a combined volar and dorsal approach results in reasonable and functional clinical results. The incidence of associated injuries with these carpal dislocations is high. Although the perilunate fracture–dislocations have a slightly better radiologic alignment than the dislocation group, the clinical outcome is similar.
Keywords: Perilunate, Fracture, Dislocation, Osteochondral, Carpal ligament
Introduction
Perilunate dislocations and fracture–dislocations of the carpus are among the most severe injuries sustained and are extremely challenging to treat. They are a subcategory of carpal instability complex which involves disruption of carpal bone alignment between both the same row and between the proximal and distal rows. The mechanism of injury characteristically involves forceful wrist hyperextension, ulnar deviation, and intercarpal supination, leading to a progressive and predictable spectrum of injury, also termed progressive perilunate instability [20]. These injuries commonly occur in young adults and result from high-energy injuries such as a fall from a height or a motor vehicle accident (MVA). They have also been seen as a result of extreme athletic activities [22]. As many as 25 % of these injuries are initially missed, leading to a possible delay in diagnosis and, subsequently, a poorer outcome [10].
Although closed treatment was historically advocated for these injuries, the trend has been toward anatomic reduction and repair of the ligamentous and osseous structures with early open reduction and internal fixation [4]. Several methods of open reduction and internal fixation have been proposed in the literature. Many authors have suggested a dorsal approach for its benefit of offering adequate exposure of the proximal carpal row and mid-carpal joint [6, 11, 16]. The volar approach suggested by Herbert and Fisher [9] allows access to distal scaphoid fractures and allows repair of the volar ligaments and capsular rent as well as the release of the carpal tunnel. Still others propose a combined dorsal and volar approach that takes advantage of the benefits of each individual approach [2, 24, 26].
Most of the previous studies on perilunate dislocations have mainly focused on the correlation of the preoperative radiologic indexes with the final clinical and radiologic outcomes in order to evaluate the proposed surgical technique. Likewise, we evaluated the outcomes of these injuries treated with a prospective standardized protocol using a combined dorsal and volar approach and rigid internal fixation. It has been proposed that the clinical outcome of these patients might be dependent on the initial injury and the extent of articular cartilage damage [12]. In order to evaluate this, we evaluated the intraoperative findings and their association with final follow-up outcomes.
Materials and Methods
Patients who were diagnosed and treated for perilunate dislocations and fracture-dislocations at our institution between January 2001 and June 2008 and who agreed to be part of this study made up the cohort for this study. The study was approved by our institutional review board. A total of 53 patients with 54 wrist injuries were identified. The patients included were those who presented with acute injuries, without any prior surgical intervention at another institution. This eliminated eight patients; thus, 45 patients with 46 wrist injuries met our inclusion criteria. The intraoperative findings of these patients were recorded, including the size of the mid-carpal ligament tear, the location of the scapholunate ligament tear, the presence of dorsal or volar osteochondral fragments, and the presence of a dorsal radiocarpal ligament avulsion.
For evaluation of postoperative clinical and radiographic outcomes, we excluded the patients with <6 months follow-up. Twenty-five cases met these criteria. The final outcome measures were assessed in the following manner. Wrist function (flexion–extension arc and pronation–supination arc) and elbow extension and flexion were measured using a handheld goniometer. Grip strength was measured using a Jamar (Lafayette Instrument Company, 3700 Sagamore Parkway Lafayette, IN 47904) dynamometer. These values were recorded in both absolute degrees and as a percentage of the value of the opposite extremity. To obtain a subjective assessment, a Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire was completed and the degree of pain, tenderness at the surgical site, unsightly scarring, and crepitus were also recorded.
Radiographs were evaluated immediately post-surgery and at the latest follow-up. The scapholunate, radiolunate, and capitolunate angles were measured on lateral views, while the scapholunate interval, scapholunate gap, and carpal height ratio were assessed posteroanteriorly (PA). A revised carpal height index was measured that assesses the amount of carpal collapse. This method, which has been used in previous studies, divides the carpal height length (distance from the base of the third metacarpal to the lunate facet) by the length of the capitate obtained on a PA radiograph (normal, 1.57 ± 0.06) [21]. These parameters were measured using the angle tool on a digital radiograph system (PACS, General Electric Company, 3000N, Grandview Blvd., Waukesha, WI 53188). In addition, radiographic evidence of arthritis was assessed according to the grading scale established by Knirk and Jupiter [15]. Avascular necrosis of the lunate was graded using plain radiographs and according to the classification of Lichtman et al. [18].
The characteristics of the 46 wrist injuries in 45 patients of the initial study group are as follows. The dominant hand was injured in 21 cases. There were 23 dorsal perilunate dislocations and 23 dorsal perilunate fracture–dislocations. The fracture–dislocations were transscaphoid (n = 17), radial transstyloid (n = 5), and transscaphoid–transcapitate (n = 1).
Complete clinical and radiographic evaluation at a minimum of 6 months (range, 6–126; average, 24.3 months) was obtained in 25 of the cases. Of this group, most cases were males (22 cases), the average age was 33.3 (20–55) years, and the dominant wrist was injured in 13 patients. The major mechanisms of injury were motor vehicle injury (12) and fall (10) followed by bike accident (1), pedestrian struck (1), and sports injury (1). Thirteen (52 %) of the cases had concomitant injuries including radius or ulna fractures (seven cases), acetabular fracture (one case), elbow dislocation (two cases), one case of ulnar nerve injury, two phalangeal fractures, and one metacarpal fracture. Of the 25 cases available for minimum 6 months of follow-up, the injuries were dorsal perilunate dislocations in 13 patients and dorsal perilunate fracture–dislocations in 12 patients. There were eight trans-scaphoid fracture–dislocations and four radial trans-styloid fracture–dislocation in the fracture–dislocation group.
The final wrist range of motion, grip strength, and radiologic indexes were compared between the perilunate dislocation and the fracture–dislocations groups. The change in the aforementioned radiologic indexes from postoperative time to the final follow-up was compared in each group using an unpaired t test. The correlations of the intraoperative findings and the final follow-up range of motion, grip strength, and radiologic indexes (lunate avascular necrosis (AVN), revised carpal height, radiolunate, and capitolunate angle) were also assessed using appropriate statistical tests (unpaired t tests). The analyses were done using SPSS, version16 (SPSS Inc., Chicago, IL). A p value of ≤0.05 was deemed statistically significant.
Surgical Management
All cases had the operative procedure performed under a general anesthetic. A combined dorsal and volar approach was used in all cases. The volar approach consists of a carpal tunnel incision extending proximal to the wrist crease and then curving ulnarly then proximally into the distal forearm. The carpal tunnel is decompressed and its contents examined. The interval between the carpal tunnel contents and the ulnar neurovascular bundle is utilized to evaluate the volar midcarpal ligament, assess the reduction of the carpus, as well as identify any osteochondral fragments. The lunate is reduced from this exposure if dislocated into the carpal canal.
A standard dorsal longitudinal incision was used in line with Lister’s tubercle. The extensor retinaculum was identified and incised in line with the third dorsal compartment. The extensor pollicis longus tendon is retracted radially and the second and fourth dorsal compartments elevated off the capsule. The dorsal capsule is then incised longitudinally. If the capsule is avulsed or torn, this area of injury is used as a starting point for the arthrotomy. The carpal bones are identified and the injuries noted. Kirschner (K)-wires are placed in the scaphoid and lunate to act as “joysticks” to facilitate reduction. The carpus is anatomically reduced and stabilized with K-wires through both the proximal carpal row and across the midcarpal joint. Osteochondral fractures, based on their size, are either fixed or excised. Associated scaphoid and radial styloid fractures are repaired if necessary, usually with cannulated screws.
The majority of scaphoid fractures were fixed using the dorsal approach (16 cases). In two cases, the volar approach was used for a very distal scaphoid fracture pattern. A headless screw was used in 16 cases, two small-headed screws in one case and smooth pins in one other case. The scapholunate and lunotriquetral ligaments were repaired as needed. The scapholunate (SL) ligaments were repaired in 33 cases and the lunotriquetral (LT) ligament was not repaired in any cases. The capsule was then closed. K-wires were placed under the skin in 28 cases and left out of the skin in 18 cases. All cases involved pinning of the mid-carpal joint, while the LT joint was pinned in 42 cases. Intraoperative fluoroscopy was utilized to evaluate the reduction and ensure proper alignment of the carpus. Lastly, the mid-carpal ligament tear was repaired using the volar approach.
The wrist was immobilized in a long-arm splint and finger range of motion exercises were started immediately. Sutures were removed at 10–14 days. Patients were changed into a long-arm cast to prevent forearm rotation for an additional 4 weeks. This immobilization was then converted to a short-arm cast for another 4 weeks. At approximately 10 weeks from surgical repair, the cast and the K-wires were removed. Formal physiotherapy is then initiated with intermittent off-the-shelf wrist immobilization.
Results
In the total of 45 patients, the intraoperative examination showed the volar carpal ligament tear to be present 100 % of the time and to be an average length of 3.4 cm. Complete avulsion of the dorsal extrinsic radiocarpal ligaments was found in 65.2 % of cases. The scapholunate ligament was torn in 35 cases, 25 from the lunate attachment, 8 from the scaphoid, and 2 mid-substance tears. Osteochondral fragments were found volarly in 17.4 % of cases, dorsally in 41.3 %, and both volarly and dorsally in 15.2 %. Preoperative median nerve compressive symptoms were found in 28 cases, with paresthesia being present. These symptoms were severe and progressed to acute carpal tunnel syndrome and required urgent release in 18 patients (39 %).
Complete clinical and radiographic evaluation at a minimum of 6 months was obtained in 25 of the cases. The operation was performed at an average time of 7 days (0–24 days) from the time of injury. Sixty-five percent of cases were done during the first 7 days following the injury. The final wrist clinical and radiologic indexes are demonstrated in Table 1. The digital range of motion was full in all cases, with composite flexion being possible into the distal palmar crease. Elbow range of motion showed full extension and an average flexion of 137°. Grip strength averaged 54 lbs, which represented a 59 % value as compared to the contralateral hand. Pain, tenderness at the surgical site, unsightly scarring, and crepitus are described in Table 2. Pain was absent or only mild in 91 % of the patients. At the final follow-up, 12 cases had no evidence of arthritis, 4 patients had grade 1 arthritis, 6 had grade 2, and 3 cases had grade 3 according to the classification of Knirk and Jupiter [15]. Of the three patients with grade 3 arthritis, two had a deep infection that required operative debridement. The other patient with a deep infection had grade 2 arthritis.
Table 1.
Clinical and radiologic outcomes at the final follow-up
| Final follow-up outcome | M ± SD | |
|---|---|---|
| Clinical | Flexion–extension | 82 ± 29° |
| Pronation–supination | 155 ± 33° | |
| Grip strength of injured hand/uninjured hand | 59 ± 23 % | |
| DASH score | 40 ± 16 | |
| Radiologic | Revised carpal height ratio | 1.5 ± 0.06 |
| Scapholunate gap | 2.2 ± 1.6 mm | |
| Scapholunate angle | 55 ± 9° | |
| Radiolunate angle | 8 ± 7° | |
| Capitolunate angle | −12 ± 6° |
Table 2.
Pain, tenderness at the surgical site, unsightly scarring, and crepitus at the final follow-up
| Clinical evaluation | Grade | Number (percentage) |
|---|---|---|
| Pain | None (0) | 9 (43) |
| Mild (1−3) | 9 (43) | |
| Moderate (4−6) | 2 (10) | |
| Severe (7−10) | 1 (4) | |
| Tenderness | None | 8 (50) |
| Mild | 8 (50) | |
| Moderate/severe | 0 (0) | |
| Unsightly scarring | None | 10 (77) |
| Mild | 2 (15) | |
| Moderate/severe | 1 (8) | |
| Crepitus | None | 8 (89) |
| Present | 1 (11) |
The perilunate dislocation patients were slightly older than the perilunate fracture–dislocation group (36 vs. 31 years, p = 0.26). Table 3 shows the radiologic indexes of these two groups. Both the fracture–dislocation and the dislocation-alone groups had a decrease in carpal height index from immediate postoperative to the final follow-up, demonstrating some mild carpal collapse. The scapholunate angle was seen to increase significantly in the dislocation group, from 45.2° to 53.0° (p = 0.03) at the final follow-up, while in the fracture–dislocation group, the change was not significant, but showed an increase from 50.5° to 57.4°. No significant differences were found in the SL, radiolunate, and capitolunate angles from postoperative to the final follow-up. The SL gap increased in both the dislocation group (1.59–2.35 mm) and in the fracture–dislocation group (2.01–2.03 mm). At the final follow-up, there was only 8 % lunate avascular necrosis in the fracture–dislocation cases, while the dislocation group showed 54 % avascular necrosis (p = 0.01). There were three grade II, three grade III, and two grade IV cases according to the classification of Lichtman et al. [18]. In the dislocation group, six of seven (86 %) patients with lunate AVN had grade 2 or higher arthrosis, while in the fracture–dislocation group, if AVN was not present, the incidence of no or minimal (grade 1) arthrosis was 91 %.
Table 3.
Comparison of immediate postoperative and follow-up radiologic indexes in both the dislocation and dislocation–fracture groups
| Perilunate dislocation group | Perilunate fracture–dislocation group | |||||
|---|---|---|---|---|---|---|
| Radiologic indexes | Postoperative (M ± SD) | Follow-up (M ± SD) | p value | Postoperative (M ± SD) | Follow-up (M ± SD) | p value |
| Revised carpal height | 1.53 ± 0.07 | 1.48 ± 0.05 | 0.05* | 1.5 ± 0.09 | 1.44 ± 0.07 | 0.04* |
| Scapholunate gap | 1.59 ± 0.91 | 2.35 ± 1.71 | 0.17 | 2.0 ± 0.79 | 2.03 ± 1.47 | 0.97 |
| Scapholunate angle | 45.21 ± 9.47 | 53.02 ± 7.08 | 0.03* | 50.51 ± 8.71 | 57.43 ± 9.91 | 0.08 |
| Radiolunate angle | 8.99 ± 9.19 | 8.84 ± 7.9 | 0.97 | 8.36 ± 4.77 | 6.58 ± 5.53 | 0.41 |
| Capitolunate angle | 14.1 ± 4.96 | 13.53 ± 6.25 | 0.81 | 8.52 ± 3.84 | 10.68 ± 4.78 | 0.26 |
*p ≤ 0.05
The final flexion–extension (fracture–dislocation, 78 ± 32°; dislocation, 86 ± 25°; p = 0.53) and pronation–supination arcs (fracture–dislocation, 166 ± 23°; dislocation, 145 ± 38°; p = 0.15) were statistically similar in the perilunate fracture–dislocations and the dislocation groups. The grip strength (fracture–dislocation, 64 ± 25 %; dislocation, 53 ± 20 %; p = 0.33) also did not show any significant difference. DASH scores were obtained at final follow-up in 13 patients; the score was 40 ± 16 points.
Fifty percent of the cases who fell had lunate avascular necrosis compared to 17 % (2/12) in the MVA group (p = 0.10). The two patients who developed lunate AVN in the MVA group were found to have evidence of grade 2 and 3 arthritis at the final follow-up. Comparing the patient outcomes of those with moderate or severe arthritis (≥2) vs. those with minimal or none (≤1) demonstrated some significant differences. Forearm rotation was significantly worse in the more arthritic group (118 ± 38° vs. 170 ± 14°, p < 0.01). Flexion–extension arch approached a significant difference (70° vs. 89°, p = 0.13), while grip strength was not significant (50 vs. 63 %, p = 0.31) between the two groups.
There were three cases of deep infection, all of which required irrigation and debridement in the operating room. There was one case of superficial infection that responded to oral antibiotics. The three cases of deep infection went on to arthritis, two with grade 3 and one with grade 2, while superficial infection resulted in grade 2 arthritis. In the deep infection group, two cases had the pins left out of the skin and one case had buried pins. The one case with buried pins was lost to appropriate follow-up and presented to the emergency room 13 weeks post-surgery with his original postoperative dressing and splint and evidence of an infection. The patient with a superficial infection had buried pins. In the final patient group, 22 % (2 of 9) of the cases with exposed pins resulted in deep infection, while only 1 case in 16 patients (7 %) with buried pins had a deep infection and one had a superficial infection. This comparison was not significant (p = 0.26). There was one case of scaphoid nonunion in the fracture–dislocation group. In this case, the scaphoid was fixed with a headless screw, but also with a supplementary percutaneous pin in the scaphoid that was left out of the skin. There was no clear infection of this case, but there was progressive loosening of the screw and non-healing of the scaphoid. One case of distal ulnar instability also occurred postoperatively.
Discussion
Perilunate dislocations and fracture–dislocations are complex injuries that require anatomic operative treatment in order to have reasonable clinical results. Even if proper operative treatment is performed, the outcomes can be guarded. This study examined the associated ligamentous and bony injuries seen with these carpal dislocations and examined the clinical and radiographic outcomes. Some differences were seen between the fracture–dislocation group and the dislocation-alone patient group.
Although the radiological outcome of the fracture–dislocation group was somewhat better maintained, the clinical outcome was similar to the dislocation group. In all cases, the delay from the time of injury to operation was <24 days, while 65 % of cases underwent operation in 7 days following the injury. Such operative delay did not appear to affect the clinical or radiologic outcome. However, an appropriately timed treatment is essential. Patients with acute carpal tunnel syndrome or irreducible dislocations require urgent operative repair.
Avascular necrosis of the lunate was higher in the fall group (50 %) compared to the MVA group (17 %). Thus, it can be concluded that the mechanism of injury plays a role in lunate AVN. The rate of AVN in pure dislocation (54 %) was significantly higher than in the fracture–dislocation (8 %) group. We theorize that this is due to the greater soft tissue stripping and complete avulsion of the SL and LT ligaments and possibly from the greater energy directly transmitted to the lunate in dislocations alone.
The size of the volar mid-carpal ligament tear and the presence of osteochondral fragments or dorsal radiocarpal ligament tear did not have any predictive value for the clinical and radiologic prognosis. However, these injuries were addressed and repaired anatomically. If these associated injuries are ignored with a single approach, the clinical results may be worse. It seems that instead of a single major contributor to the prognosis, a myriad of factors affect the outcome in these injuries. These seem to include the mechanism of injury; the magnitude of energy imparted; and the extent of bone, ligament, and cartilage damage. We feel that there is truly a spectrum of injury severity patterns within the perilunate injury classification. Those with a true “low-energy” injury seem to do better than the complex, “high-energy” injuries. However, we were not able to analyze this hypothesis in this study.
Table 4 shows a review of the studies on the combined volar–dorsal approach for perilunate dislocations and fracture–dislocations. Our study results were similar to the study of Hildebrand et al. [12] for functional outcome measures: flexion–extension, 82 ± 29° vs. 82 ± 40°; pronation–supination, 155 ± 33° vs. 150 ± 22°. Our series had a higher final DASH score (39 vs. 16) and less grip strength (59 vs. 73 %). Ten of our patients (43 %) had ipsilateral upper extremity fractures or dislocations compared to 5 of 22 (23 %) cases of such injuries in the study of Hildebrand et al. In addition, the DASH scores were not obtained on all of our patients. This might be the reason why the aforementioned indexes were higher than their study. In our series, the incidence of grade 2 and 3 arthritis was 36 % with an average follow-up of 24.3 months. In studies with an average follow-up of 2–2.5 years, the arthritis rate was 18−22 % [1, 13, 14, 24, 25], while studies with a follow-up period of 6–12 years showed the arthritis rate to be as high as 50–100 % [5, 10, 23]. A high percentage of these severe injuries, with chondral fractures and articular impaction, appears to progress to some degree of arthrosis over time. However, many of these patients may do well clinically.
Table 4.
Review of the studies on the combined volar–dorsal approach for perilunate dislocations and fracture–dislocations [1, 7, 12, 13, 17, 24]
| Author (year) | Follow-up | Perilunate dislocations, fracture–dislocations | Approach | Postoperative immobilization | Flexion–extension arc (deg) | Pronation–supination arc (deg) | DASH | Grip strength (kg) | Lunate AVN | Arthritis | Revised carpal height ratio |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Inoue and Imaeda (1996) | 24 months (11–90) | 28 patients with 29 fracture–dislocations | Palmar: 22 | A: 4 weeks (12) | A: 114 | Not reported | Not reported | A: 81 % | Not reported | Not reported | Not reported |
| Dorsal: 1 Combined: 6 | B: ≥5 weeks (16) | B: 96 | B: 80 % | ||||||||
| Sotereanos et al. (1997) | 30 months (12–69) | 11 | Combined | 8 weeks | 89 | Unrestricted | Not reported | 23 (77 %) | Not reported | 2 | 0.50 |
| Apergis et al. (1997) | 2 years (0.5–7) | 19 cases, 20 wrists | Dorsal: 10 | 6–8 weeks | |||||||
| Combined: 10 | |||||||||||
| Hildebrand et al. (2000) | 37 months (13–65) | Dislocation: 6 Fracture–dislocation: 17 | Combined | 10 weeks | 82 ± 40 | 150 ± 22 | 16 ± 13 | 35 ± 13 Normal: 48 ± 12 | 14 % | 50 % | 1.49 ± 0.12 |
| Komurcu et al. (2008) | 45 months (23–70) | 12 Fracture–dislocation: 6 acute (1st week) | Dorsal: 8 | 10 weeks | Early: 129.5 ± 20.42 | Not reported | Not reported | Early: 34 ± 12.8 | 0 | Early: 0 | Early: 1.51 |
| 6 delayed (1st to 5th week) | Combined: 4 | Delayed: 95.5 ± 18.08 | Delayed: 26.3 ± 13.5 | Delayed: 2 | Delayed: 1.45 | ||||||
| Normal: 43.8 ± 7.7 | |||||||||||
| Forli et al. (2010) | 13 years (10–23) | Dislocations: 11 | Dorsal: 11 | 5–13 weeks | 95 | Not reported | Not reported | 39 (87 %) | Not reported | 67 % | None |
| Fracture–dislocations: 7 | Volar: 3 | ||||||||||
| Combined: 4 |
The scapholunate angle for the dislocation and the fracture–dislocation groups were 53° and 58°, respectively, in our study, but there was a significant increase in the SL angle in the dislocation group from the initial postoperative to the final follow-up. This may be due to the reliability of bone healing as compared to the tendency of ligamentous healing to be inconsistent and also to elongate over time. Like the results of Hildebrand et al. (58°) [12] and Inoue and Kuwahata (61°) [14], our results were also within the normal range. In addition, the revised carpal height ratio of both the dislocation and the fracture–dislocation groups decreased significantly from the initial postoperative values to those at final follow-up. The presence of osteochondral fragments and the sizes of the mid-carpal ligament tear and dorsal radiocarpal tear were demonstrated in a high percentage of these patients. These injuries were repaired or excised and the carpus was reduced anatomically from both the dorsal and volar perspectives, which likely aided in providing favorable clinical outcomes.
The differences between perilunate dislocations and fracture–dislocations have been repeatedly discussed in the literature, with conflicting reports [12]. In our study, although perilunate dislocations had a greater increase in scapholunate angle compared to the fracture–dislocation group, the final hand range of motion and grip strength were similar. However, at a longer clinical follow-up, these patients may result in increased carpal deformity and subsequent decreased clinical outcomes. In the study of Hildebrand et al. [12], among all the final clinical and radiologic measures, the only difference between these two groups was in the revised carpal height ratio. The perilunate dislocation group had a higher revised carpal height ratio compared to the perilunate fracture–dislocation group (1.56 ± 0.06 vs. 1.46 ± 0.12). As was shown in the study of Komurcu et al. [17], the radiologic results may not always correlate with the clinical outcomes in these injuries. In the study of Forli et al. [7], even the presence of radiological arthritis and static carpal instability did not reduce the function at a minimum of 10 years of follow-up. We also showed that the development of arthritis did not impair the flexion–extension arch or grip strength; however, there was a significant correlation with forearm rotation and advanced arthritis.
In our series, the incidence of dislocations was similar to that of fracture–dislocations. In comparison, both Hildebrand et al. [12] and Herzberg et al. [10] reported the incidence of fracture–dislocation cases at two to three times higher than dislocations alone. Herzberg et al. performed a clinical and radiologic outcome study on 115 perilunate dislocations and fracture–dislocations with at least 1 year of follow-up. Treatment delay and the presence of an open injury had an adverse impact on the clinical results (clinical scoring system modified from [8] and [27]), while the anatomical type had less of an effect [10]. In the current study, the operation was performed within a maximum time period of 24 days (with the majority operated in 7 days) after the injury and did not affect the outcome. There was a wider range of operation delay in the series of Herzberg et al. [10] (up to 19 months) compared to ours. They showed that the outcome was better if cases were treated before the 45th day following the injury.
In perilunate dislocation or fracture–dislocations, all the involved bony and ligamentous structures should be addressed. Although previous studies have shown reasonable results using a single approach [16], we speculate that a combined dorsal/volar approach can provide the best exposure for repairing all structures and reducing the carpus anatomically. Scaphoid fractures should be rigidly stabilized, bony avulsions should be fixed to their corresponding origin, and the ligaments must be repaired [19]. Through the volar approach, the lunate can be reduced and the volar capsule repaired. The dorsal approach provides access to reduce the scapholunate and lunate-triquetral articulations and fix scaphoid fracture from an antegrade approach [24].
We immobilized the wrist for 10 weeks to assure satisfactory ligament healing [3]. Inoue and Imaeda [13] performed a study on 29 patients with trans-scaphoid perilunate dislocations who underwent open reduction and Herbert screw fixation. Twenty-four months of follow-up showed that a better range of wrist motion can be achieved if the patients are treated with cast immobilization for 4 weeks (114°, 90–135°) compared to 5 weeks or longer (96°, 50–130°, p < 0.05). However, the average grip strength and average wrist score were similar. Modification of our current postoperative protocol may improve eventual range of motion. However, currently, we have as our goal stability and ligamentous healing in order to obtain a functional range of motion.
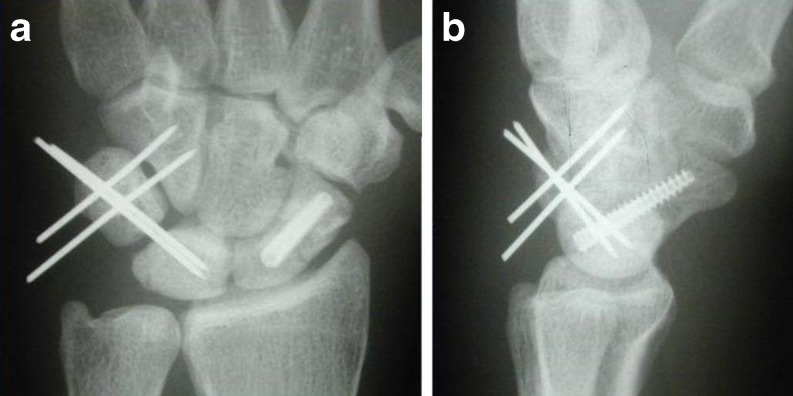
Temporary carpal fixation with Kirschner wires is necessary for a successful ligament healing. Since the injury is a combination of a dissociative injury within the proximal carpal row and a non-dissociative injury at the mid-carpal joint lunate, we feel that K-wire stabilization should be placed both within the proximal row and across the mid-carpal joint. Due to the need for prolonged immobilization and the possibility of deep infection, the K-wires should be cut short and left buried under the skin. Of our three deep infections, two of the cases had pins that were left out of the skin, emphasizing this point. We currently bury the pins below the skin in all cases of perilunar instability. Due to its high tendency for volar flexion, stable fixation of the scaphoid is required with either a screw for scaphoid fractures or a combination of scapholunate and scaphocapitate pins for ligamentous injuries alone. The lunotriquetral joint should be reduced anatomically and stabilized with one or two pins if unstable (Figs. 1, 2, and 3).
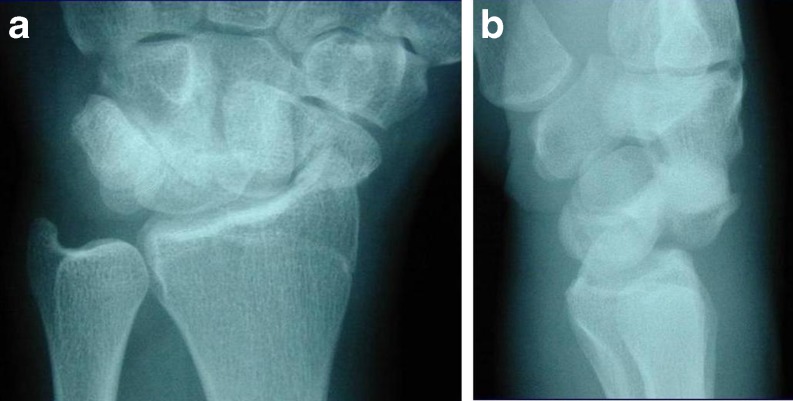
Fig. 1.
Posteroanterior (a) and lateral (b) views of perilunate fracture–dislocation with trans-scaphoid fracture
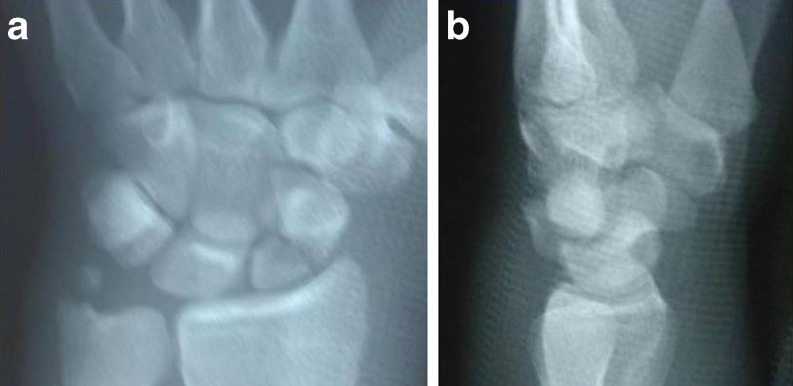
Fig. 2.
Posteroanterior (a) and lateral (b) views of closed reduction of the wrist
Fig. 3.
Posteroanterior (a) and lateral (b) views of the wrist. Antegrade fixation of the scaphoid using the dorsal approach, ligament repair, and a K-wire fixation of the triquetrum to the lunate and hamate
We did not evaluate the work status of these patients, and almost half of our original patients did not have more than 6 months of follow-up. This might be due to the fact that young active patients do not attend the follow-up clinic if adequate daily function is restored. Also, these cases were performed at an urban level 1 trauma center where patient follow-up is difficult. These patients do tend to have follow-up; however, if they are having problems, our institution typically is the only facility in the area that provides them with care.
Although perilunate fracture–dislocations in general had better radiologic parameters than the dislocation-alone group, the clinical outcome for both in our series was similar. A combination of a dorsal and volar approach, combined with anatomic repair of the injured structures, provides acceptable clinical results in these high-energy fracture–dislocations of the carpus. However, this study does not make a direct comparison of this technique with a single approach. If appropriate treatment is rendered, the incidence of arthrosis in these patients is still high. Fortunately, the final clinical outcome does not correlate with radiographic pattern, and a good clinical outcome can be seen even with mild arthrosis.
Acknowledgments
Conflict of Interest
The authors declare that they have no conflicts of interest, commercial associations, or intent of financial gain regarding this research.
Footnotes
Type of the study and the level of evidence: Prospective, Level II
References
- 1.Apergis E, Maris J, Theodoratos G, Pavlakis D, Antoniou N. Perilunate dislocations and fracture–dislocations. Closed and early open reduction compared in 28 cases. Acta Orthop Scand Suppl. 1997;275:55–59. [PubMed] [Google Scholar]
- 2.Blazar PE, Murray P. Treatment of perilunate dislocations by combined dorsal and palmar approaches. Tech Hand Up Extrem Surg. 2001;5:2–7. doi: 10.1097/00130911-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Boorman RS, Shrive NG, Frank CB. Immobilization increases the vulnerability of rabbit medial collateral ligament autografts to creep. J Orthop Res. 1998;16:682–689. doi: 10.1002/jor.1100160609. [DOI] [PubMed] [Google Scholar]
- 4.Campbell RD, Jr, Thompson TC, Lance EM, Adler JB. Indications for open reduction of lunate and perilunate dislocations of the carpal bones. J Bone Joint Surg Am. 1965;47:915–937. [PubMed] [Google Scholar]
- 5.Cooney WP, Bussey R, Dobyns JH, Linscheid RL. Difficult wrist fractures. Perilunate fracture–dislocations of the wrist. Clin Orthop Relat Res. 1987;214:136–147. [PubMed] [Google Scholar]
- 6.DiGiovanni B, Shaffer J. Treatment of perilunate and transscaphoid perilunate dislocations of the wrist. Am J Orthop (Belle Mead NJ) 1995;24:818–826. [PubMed] [Google Scholar]
- 7.Forli A, Courvoisier A, Wimsey S, Corcella D, Moutet F. Perilunate dislocations and transscaphoid perilunate fracture–dislocations: a retrospective study with minimum ten-year follow-up. J Hand Surg Am. 2010;35:62–68. doi: 10.1016/j.jhsa.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Green DP, O’Brien ET. Open reduction of carpal dislocations: indications and operative techniques. J Hand Surg Am. 1978;3:250–265. doi: 10.1016/s0363-5023(78)80089-6. [DOI] [PubMed] [Google Scholar]
- 9.Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984;66:114–123. doi: 10.1302/0301-620X.66B1.6693468. [DOI] [PubMed] [Google Scholar]
- 10.Herzberg G, Comtet JJ, Linscheid RL, Amadio PC, Cooney WP, Stalder J. Perilunate dislocations and fracture–dislocations: a multicenter study. J Hand Surg Am. 1993;18:768–779. doi: 10.1016/0363-5023(93)90041-Z. [DOI] [PubMed] [Google Scholar]
- 11.Herzberg G, Forissier D. Acute dorsal trans-scaphoid perilunate fracture–dislocations: medium-term results. J Hand Surg Br. 2002;27:498–502. doi: 10.1054/jhsb.2002.0774. [DOI] [PubMed] [Google Scholar]
- 12.Hildebrand KA, Ross DC, Patterson SD, Roth JH, MacDermid JC, King GJ. Dorsal perilunate dislocations and fracture–dislocations: questionnaire, clinical, and radiographic evaluation. J Hand Surg Am. 2000;25:1069–1079. doi: 10.1053/jhsu.2000.17868. [DOI] [PubMed] [Google Scholar]
- 13.Inoue G, Imaeda T. Management of trans-scaphoid perilunate dislocations. Herbert screw fixation, ligamentous repair and early wrist mobilization. Arch Orthop Trauma Surg. 1997;116:338–340. doi: 10.1007/BF00433985. [DOI] [PubMed] [Google Scholar]
- 14.Inoue G, Kuwahata Y. Management of acute perilunate dislocations without fracture of the scaphoid. J Hand Surg Br. 1997;22:647–652. doi: 10.1016/S0266-7681(97)80366-X. [DOI] [PubMed] [Google Scholar]
- 15.Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647–659. [PubMed] [Google Scholar]
- 16.Knoll VD, Allan C, Trumble TE. Trans-scaphoid perilunate fracture dislocations: results of screw fixation of the scaphoid and lunotriquetral repair with a dorsal approach. J Hand Surg Am. 2005;30:1145–1152. doi: 10.1016/j.jhsa.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Komurcu M, Kurklu M, Ozturan KE, Mahirogullari M, Basbozkurt M. Early and delayed treatment of dorsal transscaphoid perilunate fracture–dislocations. J Orthop Trauma. 2008;22:535–540. doi: 10.1097/BOT.0b013e318183eb23. [DOI] [PubMed] [Google Scholar]
- 18.Lichtman DM, Mack GR, MacDonlad RI, Gunther SF, Wilson JN. Kienböck’s disease: the role of silicone replacement arthroplasty. J Bone Joint Surg Am. 1977;7:899–908. [PubMed] [Google Scholar]
- 19.Lutz M, Arora R, Kammerlander C, Gabl M, Pechlaner S. Stabilization of perilunate and transscaphoid perilunate fracture–dislocations via a combined palmar and dorsal approach. Oper Orthop Traumatol. 2009;21:442–458. doi: 10.1007/s00064-009-1906-1. [DOI] [PubMed] [Google Scholar]
- 20.Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980;5:226–241. doi: 10.1016/s0363-5023(80)80007-4. [DOI] [PubMed] [Google Scholar]
- 21.Nattrass GR, King GJ, McMurtry RY, Brant RF. An alternative method for determination of the carpal height ratio. J Bone Joint Surg Am. 1994;76:88–94. doi: 10.2106/00004623-199401000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Raab DJ, Fischer DA, Quick DC. Lunate and perilunate dislocations in professional football players. A five-year retrospective analysis. Am J Sports Med. 1994;22:841–845. doi: 10.1177/036354659402200617. [DOI] [PubMed] [Google Scholar]
- 23.Schaller P, Grunert J. Late outcome after surgical treatment of perilunar dislocation and dislocation fractures. Handchir Mikrochir Plast Chir. 1998;30:298–302. [PubMed] [Google Scholar]
- 24.Sotereanos DG, Mitsionis GJ, Giannakopoulos PN, Tomaino MM, Herndon JH. Perilunate dislocation and fracture dislocation: a critical analysis of the volar–dorsal approach. J Hand Surg Am. 1997;22:49–56. doi: 10.1016/S0363-5023(05)80179-0. [DOI] [PubMed] [Google Scholar]
- 25.Su CJ, Chang MC, Liu Y, Lo WH. Lunate and perilunate dislocation. Zhonghua Yi Xue Za Zhi (Taipei) 1996;58:348–354. [PubMed] [Google Scholar]
- 26.Trumble T, Verheyden J. Treatment of isolated perilunate and lunate dislocations with combined dorsal and volar approach and intraosseous cerclage wire. J Hand Surg Am. 2004;29:412–417. doi: 10.1016/j.jhsa.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 27.Witvoet J, Allieu Y. Recent traumatic lesions of the semilunar bone. Rev Chir Orthop Reparatrice Appar Mot. 1973;59(Suppl 1):98–125. [PubMed] [Google Scholar]